No CrossRef data available.
Article contents
Low function and frequent readmission in nursing home patients with persistent resistant gram-negative bacterial colonization
Published online by Cambridge University Press: 16 May 2022
Abstract
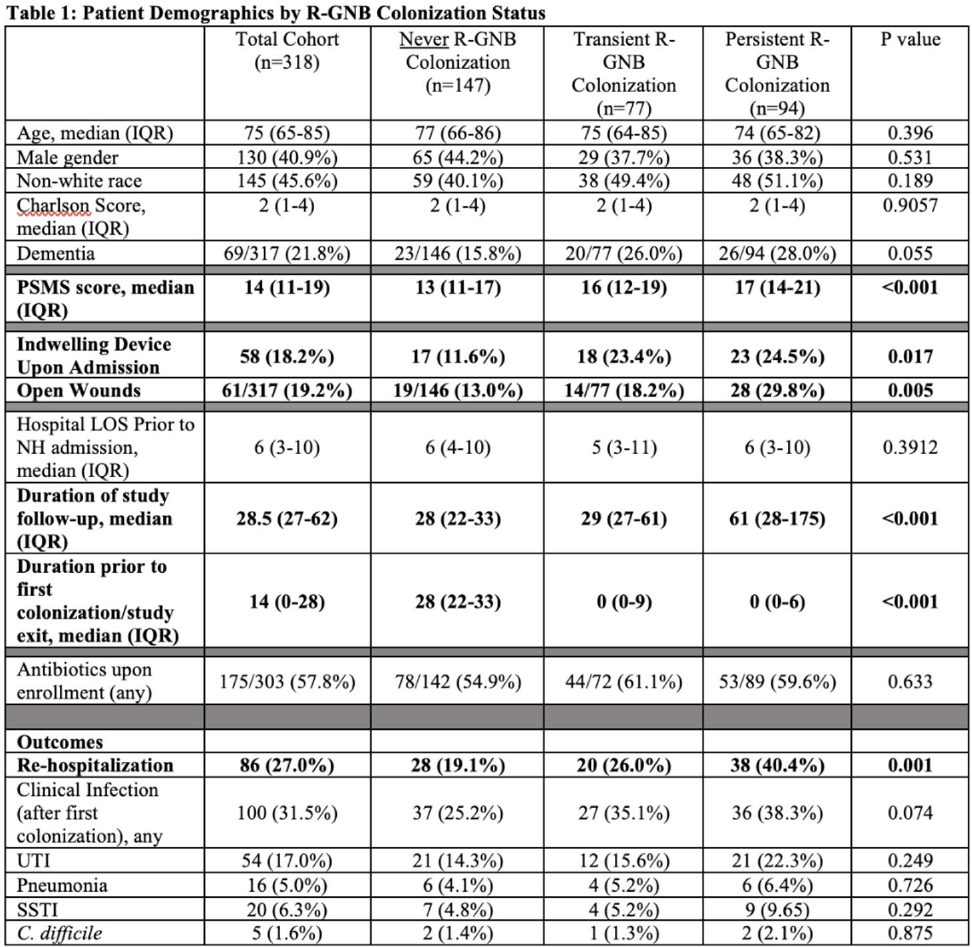
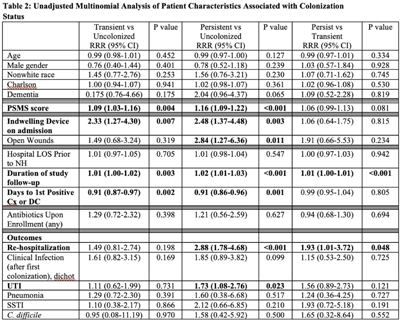
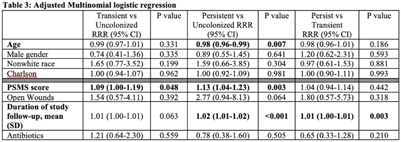
Background: Persistent colonization with resistant gram-negative bacteria (R-GNB) increases risk of clinical infection and intra-facility transmission among nursing home (NH) patients. Limited data exist on the roles of age and function on duration of R-GNB colonization. Methods: Secondary data analysis was performed from a cohort study of patients admitted to 6 Michigan NHs between November 2013 and May 2018. Swabs obtained upon enrollment, day 14, day 30, then monthly until NH discharge from 6 anatomical sites were cultured for GNB. R-GNB were defined as resistant to ciprofloxacin, ceftazidime, or imipenem. Positive R-GNB culture from a single visit followed by negative cultures for the same organism from ≥2 subsequent visits were defined as transient R-GNB colonization. All other patients with positive R-GNB cultures from multiple visits were considered persistently colonized. Demographic data, antibiotic use, device use, and physical self-maintenance scales (PSMSs) were obtained upon enrollment. Characteristics were compared between patients with transient versus persistent R-GNB and uncolonized patients using multinomial logistic regression. Results: We recruited 896 patients (median age, 75 years; 41% male; 46% nonwhite) and followed them for 2,437 total visits. Of 896 patients, 407 (45.4%) were colonized with ≥1 R-GNB during their stay. Of 171 patients with ≥ 2 follow-up visits after R-GNB detection, 94 (55%) remained persistently colonized with the same R-GNB (Table 1). Escherichia coli (30%) and Proteus mirabilis (22%) were the most frequently identified R-GNB. The most common anatomical colonization sites were perirectal (368 [24.3%] of 1,147) groin (340 [14.3%] of 2,046), and hands (115 [4.8%] of 2283). Compared to uncolonized patients, patients with persistent (1.09; 95% CI, 1.00–1.19, P = .048) and transient R-GNB colonization (1.13; 95% CI, 1.04–1.23; P = .003) had lower PSMS (Tables 2 and 3). Compared to uncolonized and transiently colonized patients, patients with persistent R-GNB colonization had prolonged lengths of NH stay (1.01; 95% CI, 1.00–1.01; P = .003). Conclusions: R-GNB colonization in vulnerable NH patients is common (407 [45.5%] of 896 and often persistent (94 [55%] of 171 patients with sufficient follow-up to assess persistence). Patients with persistent R-GNB had lower functional status, longer LOS, and higher readmission rates than those without. R-GNB decolonization should be investigated as a strategy to potentially improve outcomes among NH patients.
Funding: None
Disclosures: None
- Type
- MDR GNR
- Information
- Antimicrobial Stewardship & Healthcare Epidemiology , Volume 2 , Issue S1: SHEA Spring 2022 Abstracts , July 2022 , pp. s53 - s54
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2022. Published by Cambridge University Press on behalf of The Society for Healthcare Epidemiology of America


