Poster Presentation - Top Poster Award
Antibiotic Stewardship
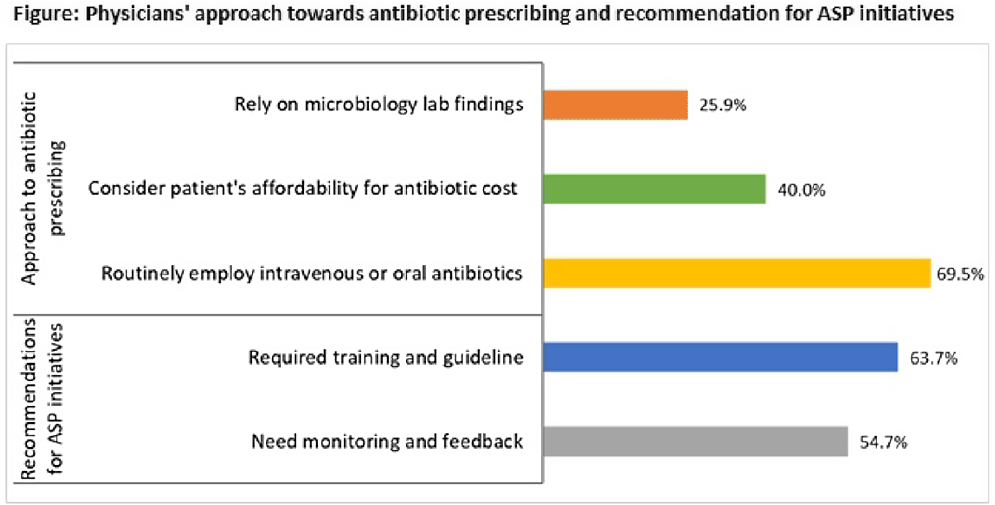
Perceptions toward and practices regarding antibiotic stewardship and use among physicians at tertiary-care public hospitals in Bangladesh
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s1
-
- Article
-
- You have access
- Open access
- Export citation
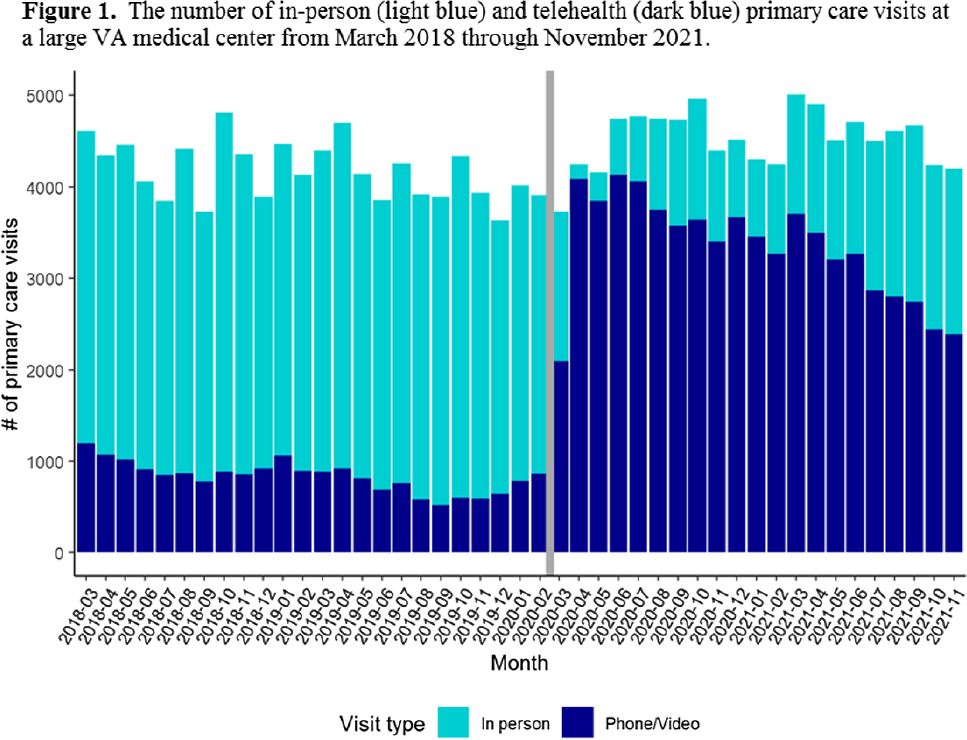
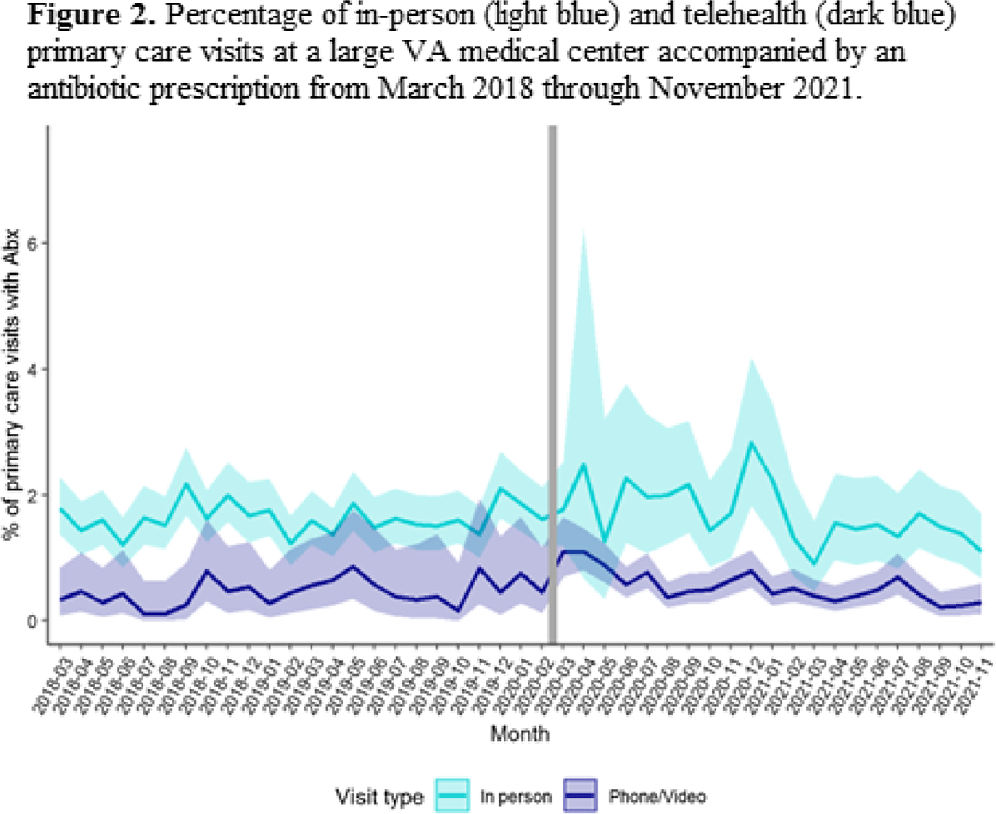
Outpatient antibiotic use for common infectious diagnoses: Patterns in telehealth during the emergence of COVID-19
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s1-s2
-
- Article
-
- You have access
- Open access
- Export citation
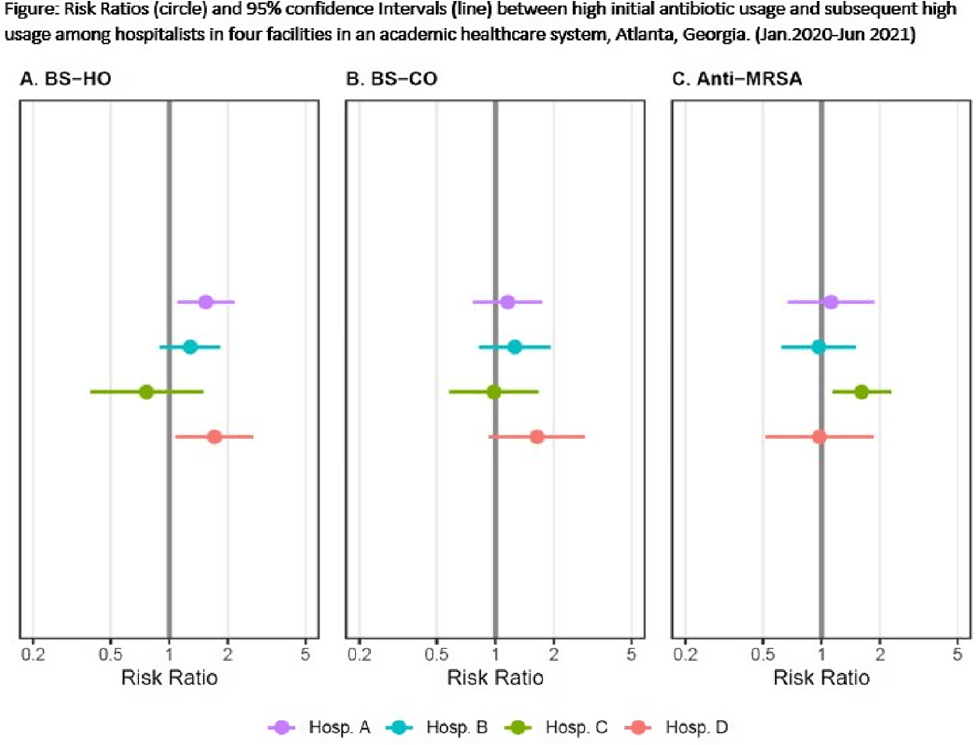
Do hospitalists who prescribe high (risk-adjusted) rates of antibiotics do so repeatedly?
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s2
-
- Article
-
- You have access
- Open access
- Export citation
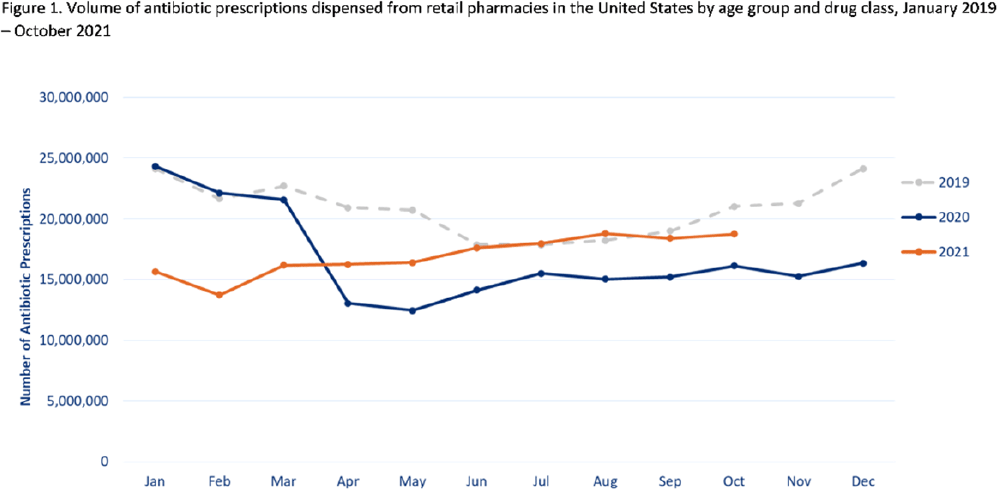
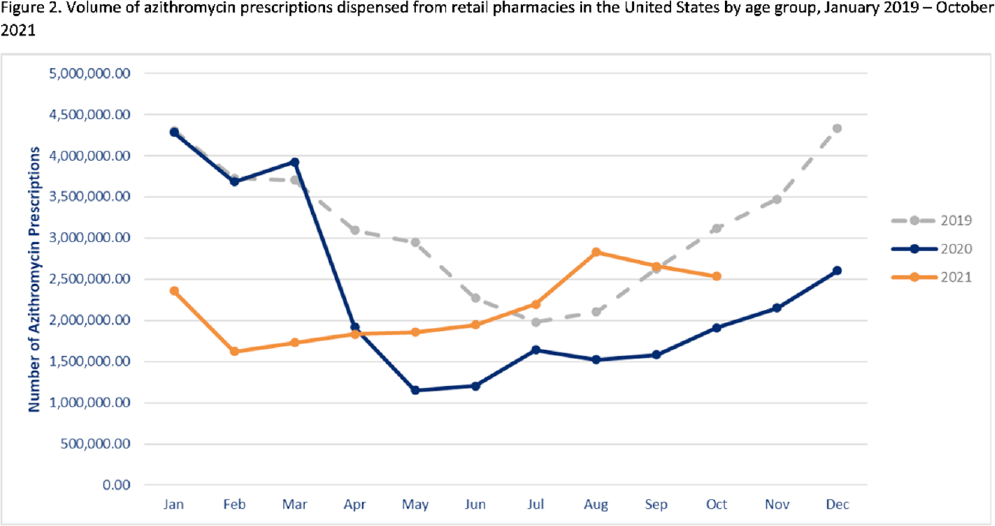
Outpatient antibiotic prescribing during the COVID-19 pandemic–United States, January 2019–October 2021
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s2-s3
-
- Article
-
- You have access
- Open access
- Export citation
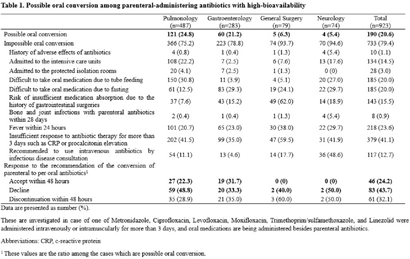
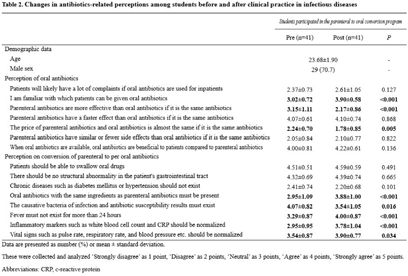
The effect of a parenteral-to-oral conversion program for high-bioavailability antibiotics use
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s3-s4
-
- Article
-
- You have access
- Open access
- Export citation
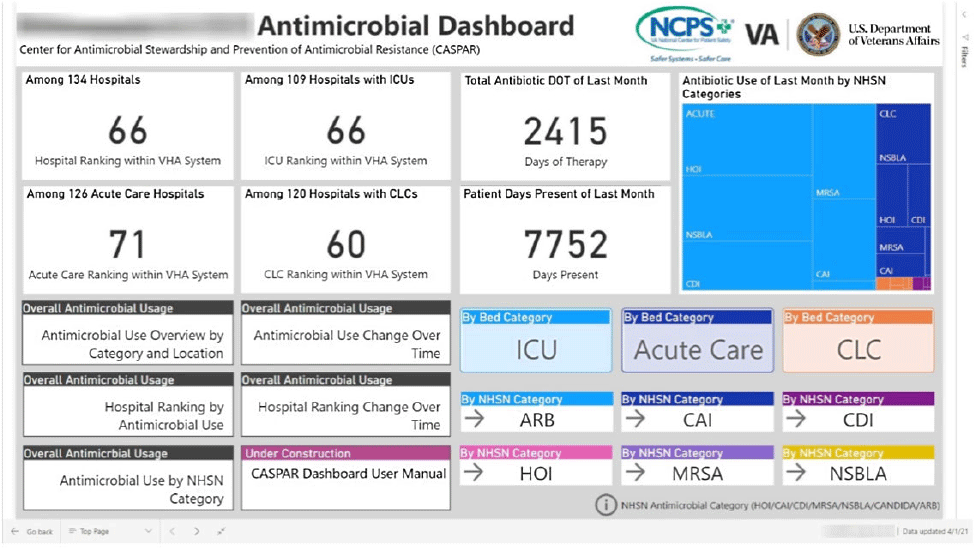
Qualitative Evaluation of an automated nationwide benchmarking antimicrobial utilization dashboard for the VHA
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s4
-
- Article
-
- You have access
- Open access
- Export citation
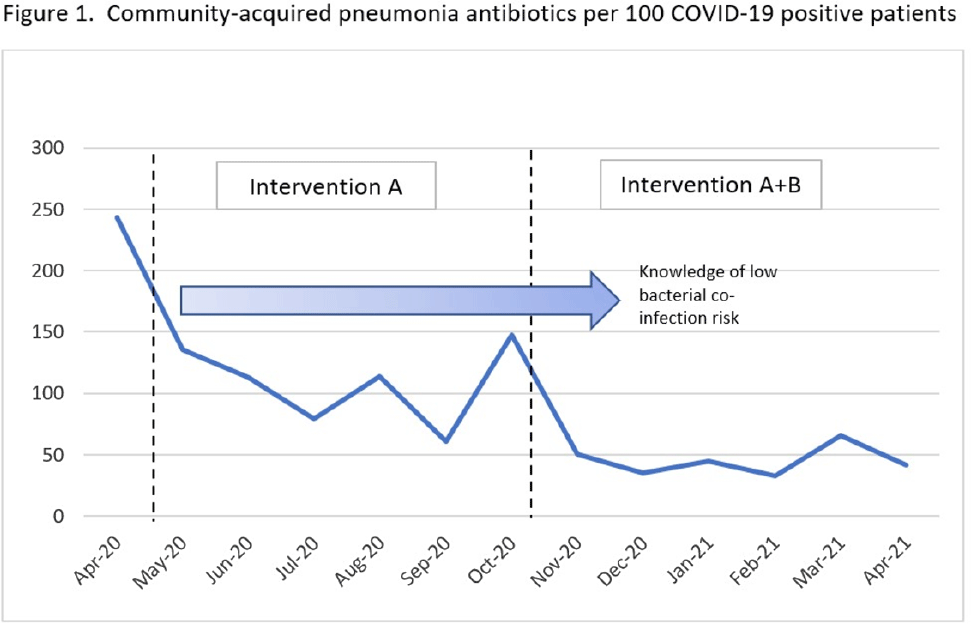
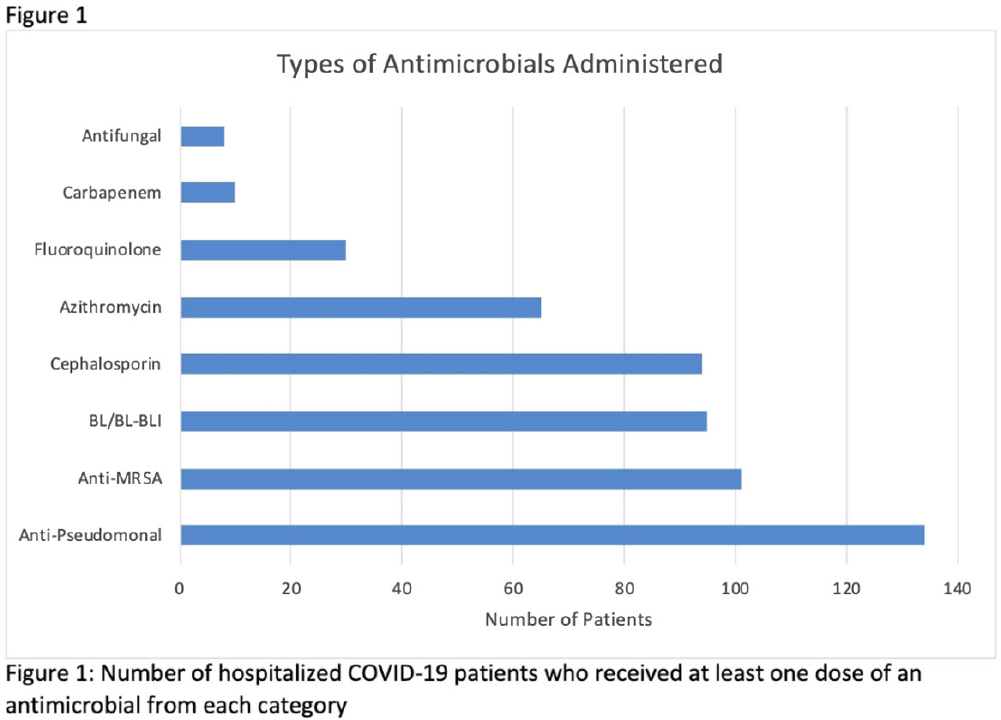
A little education goes a long way: Decreasing antibiotics for community-acquired pneumonia in COVID-19 patients
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s4-s5
-
- Article
-
- You have access
- Open access
- Export citation
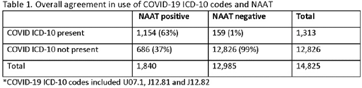
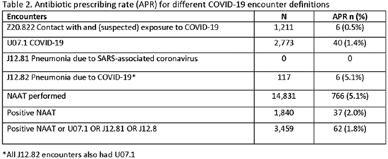
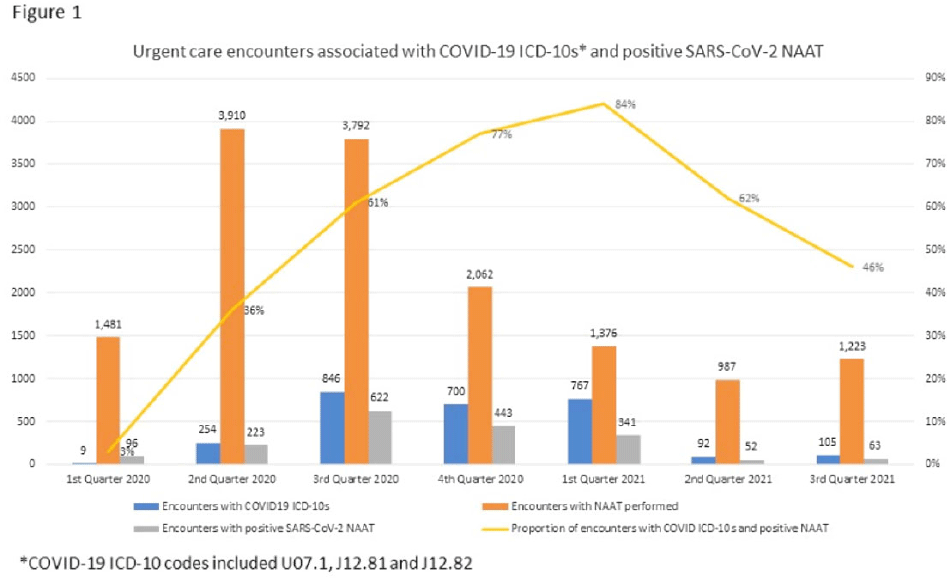
Impact of different COVID-19 encounter definitions on antibiotic prescribing rates in urgent care
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s5
-
- Article
-
- You have access
- Open access
- Export citation
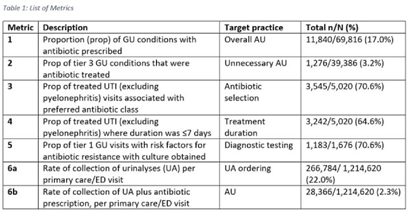
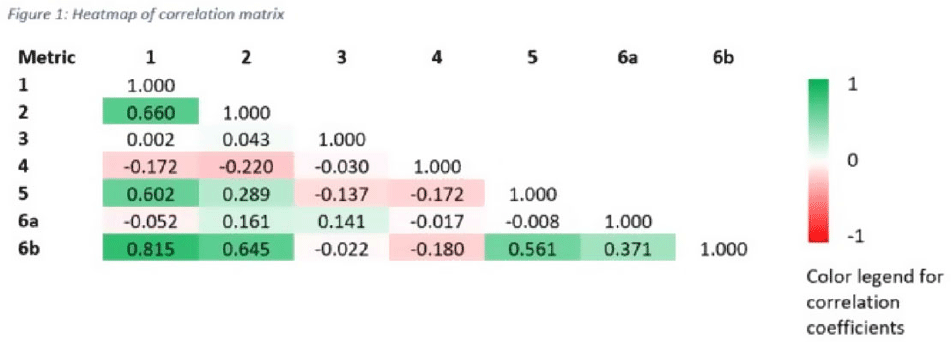
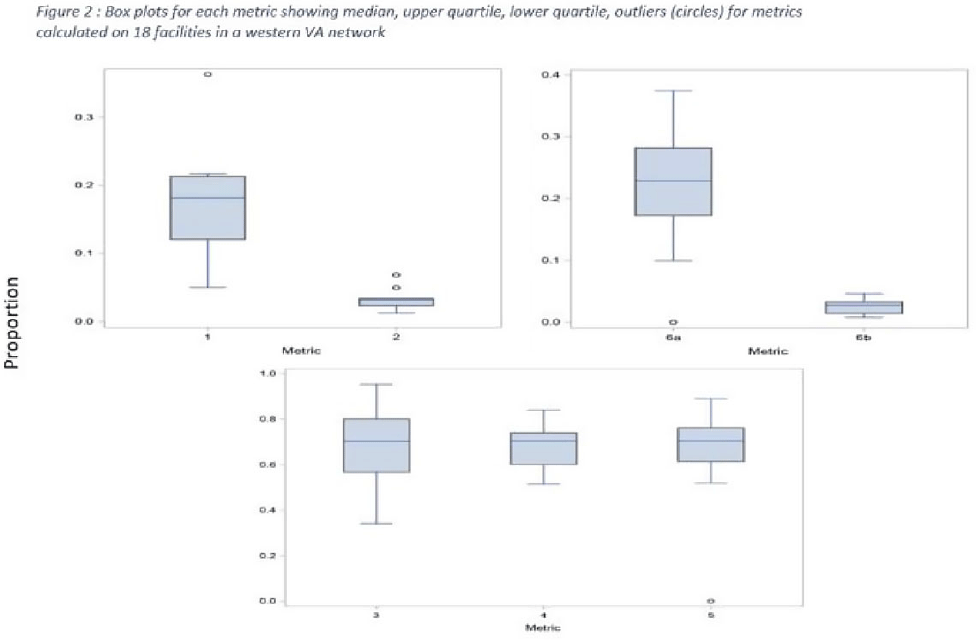
Tier-based antimicrobial stewardship metrics for genitourinary-related antibiotic use in Veterans’ Affairs outpatient settings
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s5-s6
-
- Article
-
- You have access
- Open access
- Export citation
COVID-19
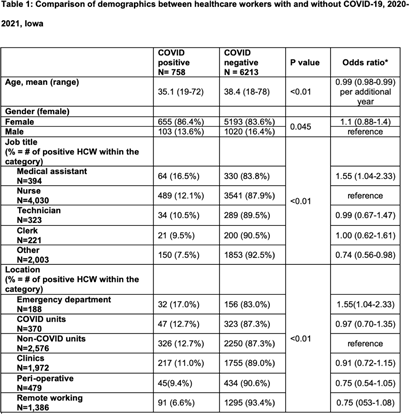
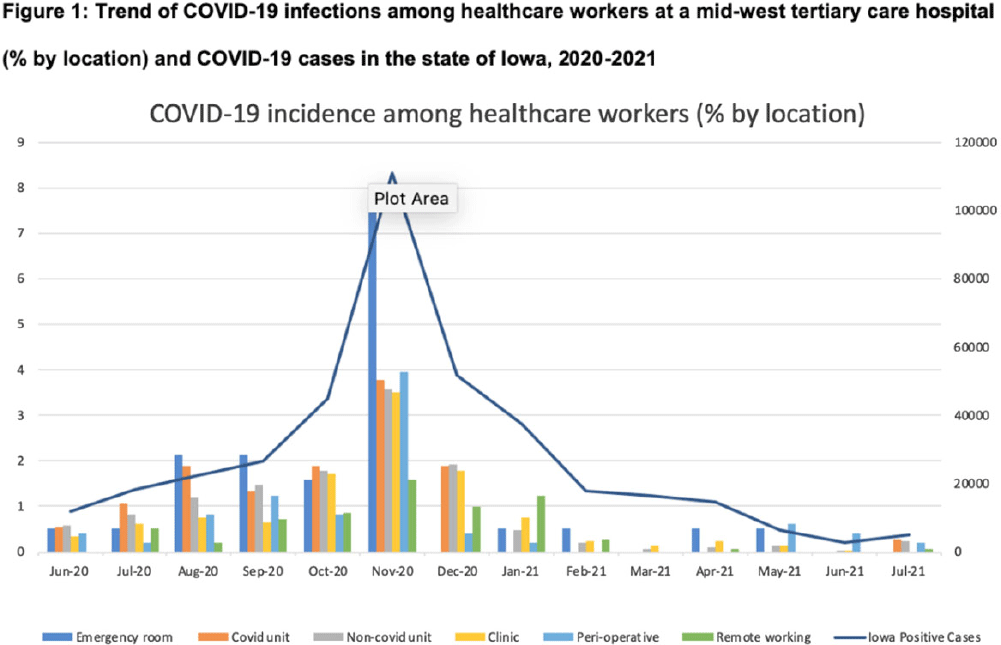
COVID-19 incidence among nonphysician healthcare workers at a tertiary care center–Iowa, 2020–2021
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s6-s7
-
- Article
-
- You have access
- Open access
- Export citation
Which nursing home workers were at highest risk for SARS-CoV-2 infection during the November 2020–February 2021 winter surge of COVID-1?
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s7
-
- Article
-
- You have access
- Open access
- Export citation
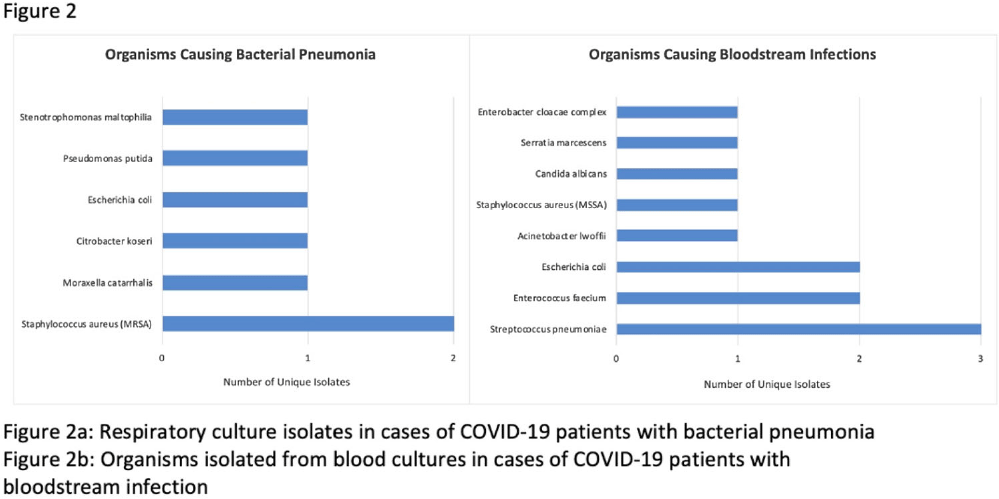
Coinfections in hospitalized COVID-19 patients are associated with high mortality: need for improved diagnostic tools
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s7-s8
-
- Article
-
- You have access
- Open access
- Export citation
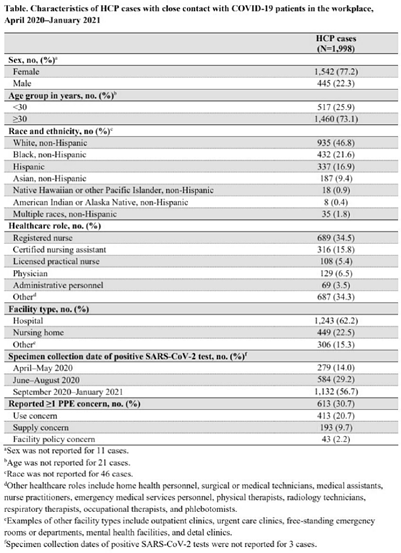
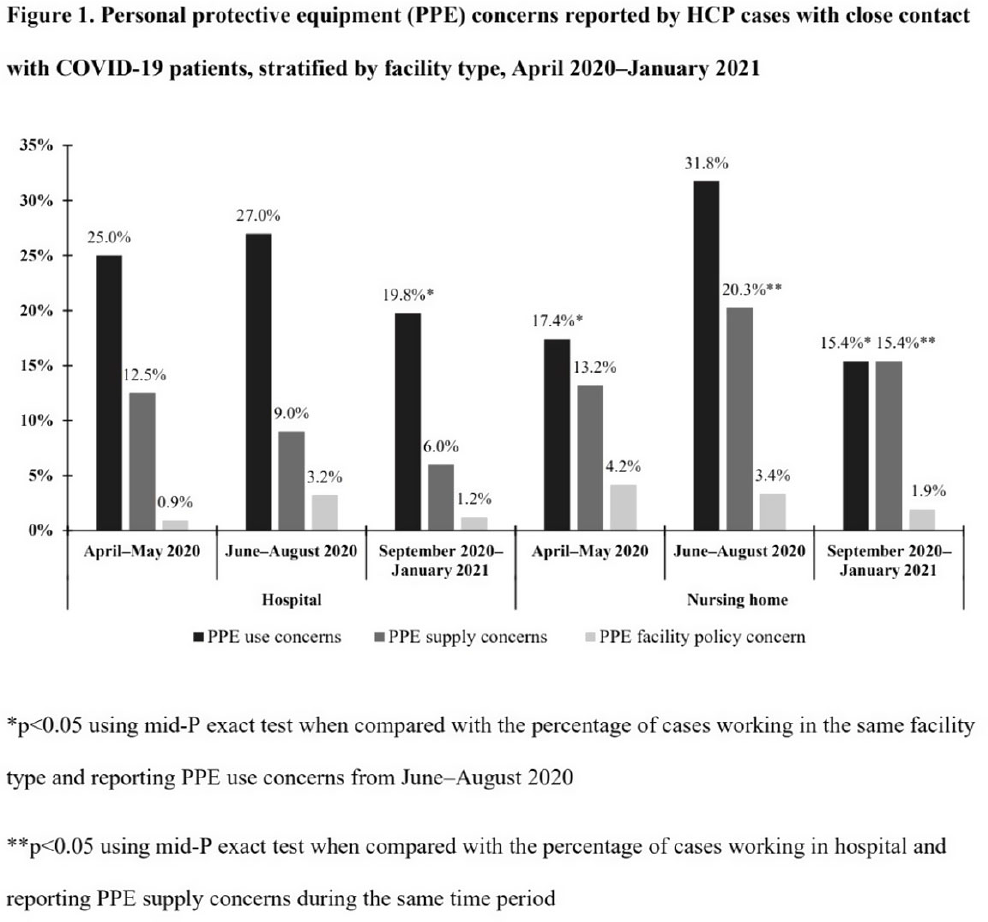
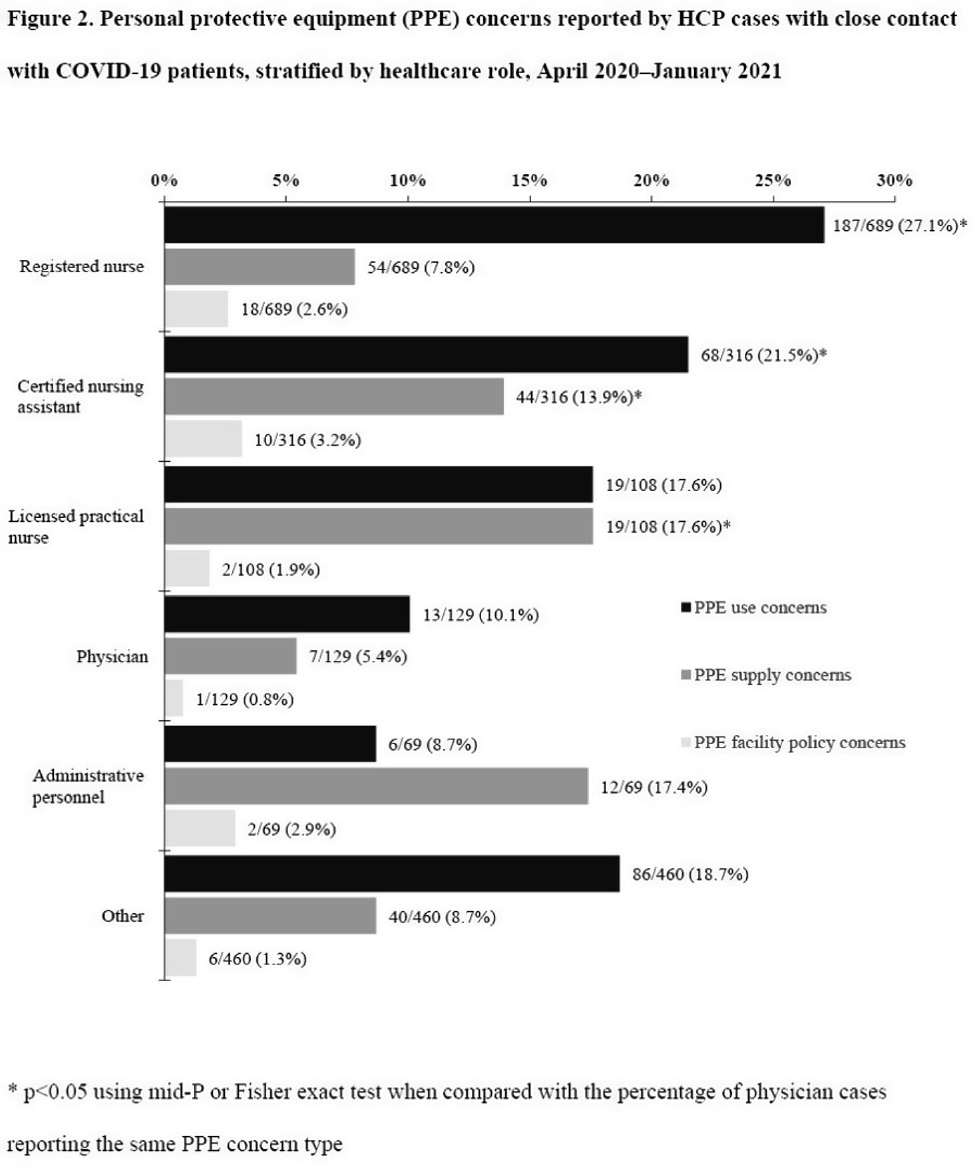
Characteristics of healthcare personnel who reported concerns related to PPE use during care of COVID-19 patients
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s8-s9
-
- Article
-
- You have access
- Open access
- Export citation
Improved assay for detecting SARS-CoV-2 from nonporous hospital surfaces using surrogate human coronavirus OC43
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s9
-
- Article
-
- You have access
- Open access
- Export citation
Work system factors affecting COVID-19 PPE use: A human factors approach to analysis of video recordings of emergency department clinical work
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s9-s10
-
- Article
-
- You have access
- Open access
- Export citation
Work system barriers to & resilience strategies for COVID-19 PPE use in the emergency department: A qualitative interview study
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s10
-
- Article
-
- You have access
- Open access
- Export citation
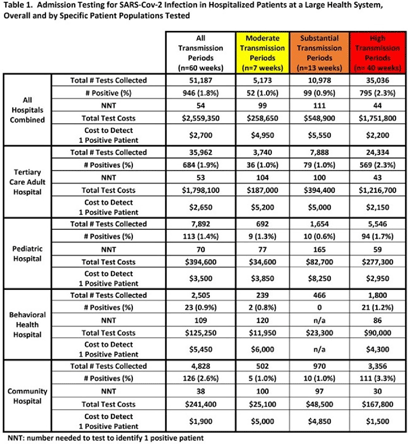
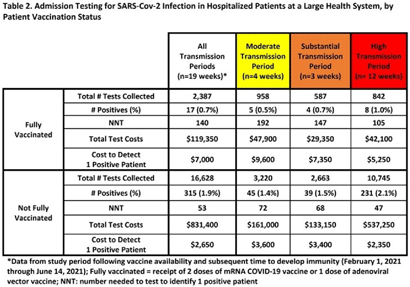
Analysis of Universal admission laboratory screening for SARS-CoV-2 asymptomatic infection across a large health system
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s10-s11
-
- Article
-
- You have access
- Open access
- Export citation
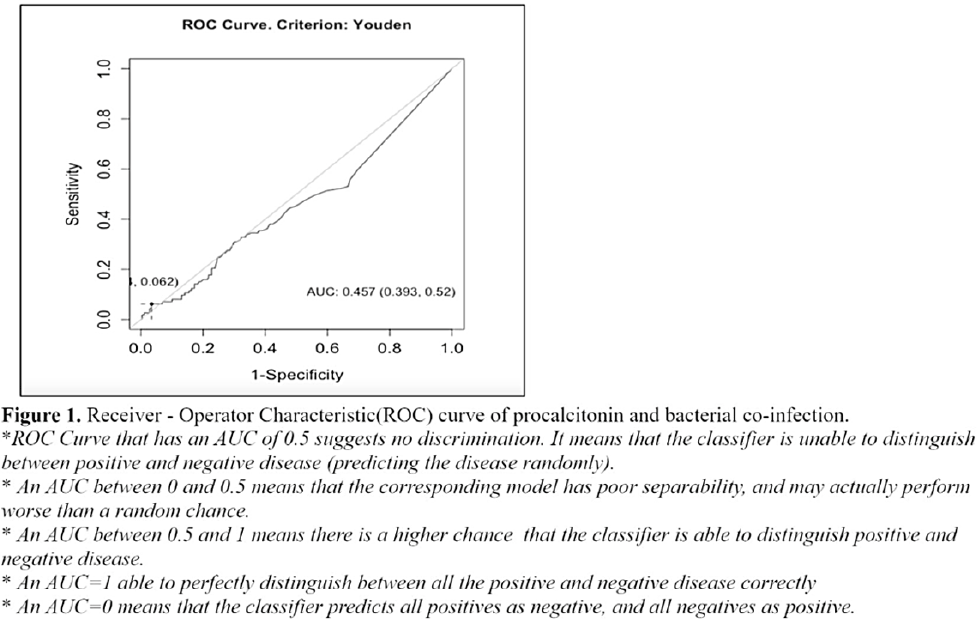
Procalcitonin as marker for bacterial coinfection among adult COVID-19 patients in a tertiary-care hospital in the Philippines
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s11
-
- Article
-
- You have access
- Open access
- Export citation
Prioritizing SARS-CoV-2 testing in a highly immunosuppressed patient population
-
- Published online by Cambridge University Press:
- 16 May 2022, pp. s11-s12
-
- Article
-
- You have access
- Open access
- Export citation
Diagnostic/Microbiology
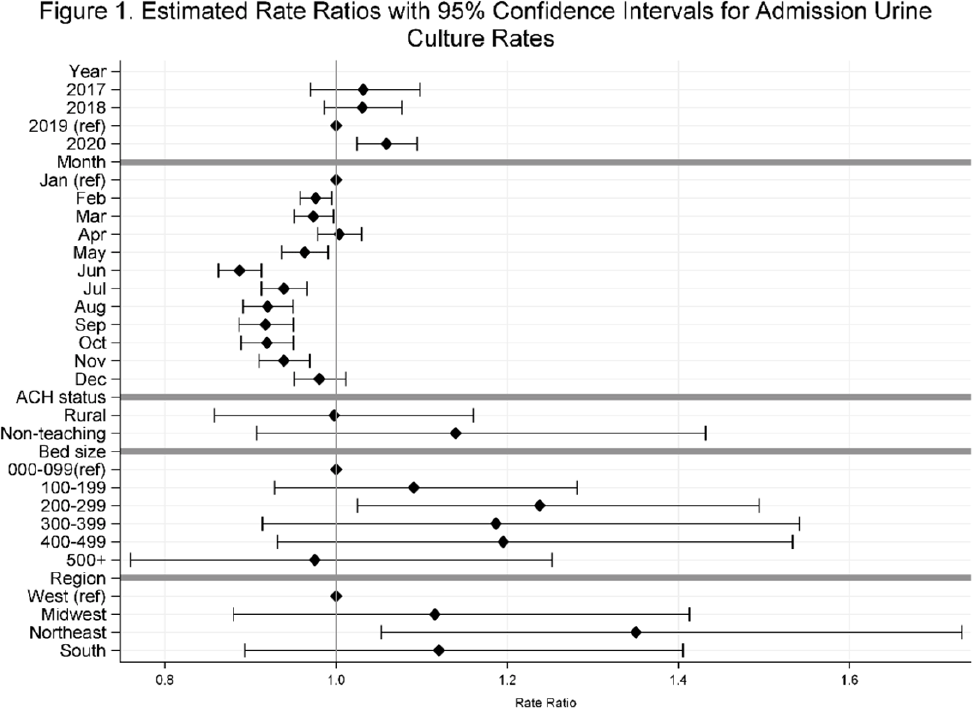
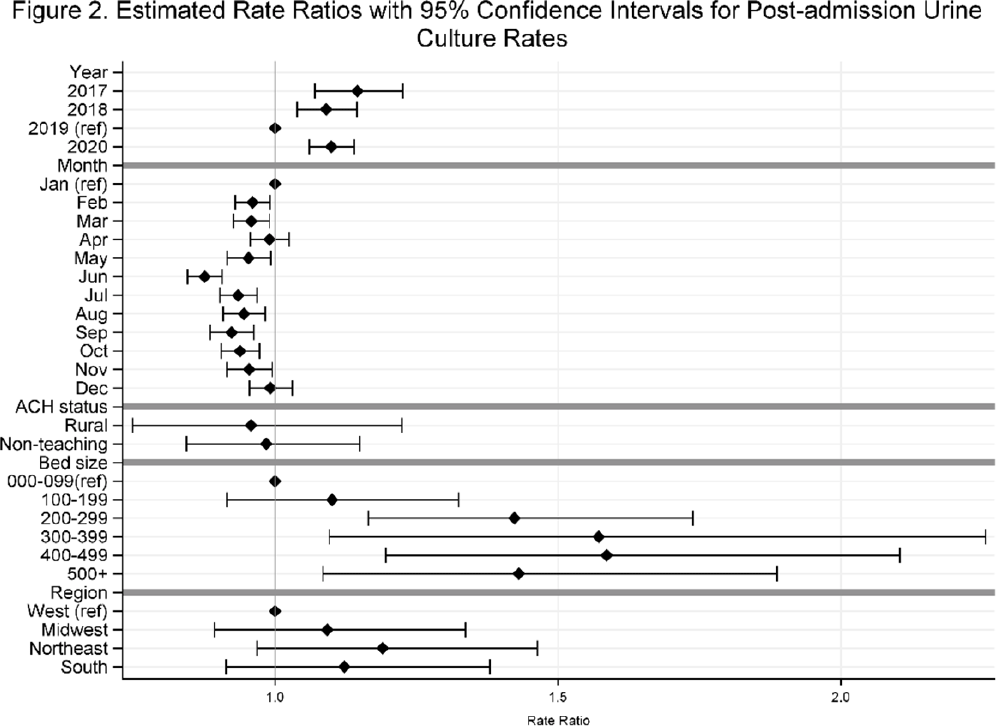
Temporal trends in urine-culture rates in the US acute-care hospitals, 2017–2020
-
- Published online by Cambridge University Press:
- 16 May 2022, p. s12
-
- Article
-
- You have access
- Open access
- Export citation