Introduction
Centuries ago, scientists first noticed the link between foods that were lacking in the diet and conditions or illnesses such as scurvy, pellagra and anaemia (Reference Murphy, Yates, Atkinson, Barr and Dwyer1, Reference Keusch2). Occurrences of illnesses were associated with the lack of specific and essential components in the overall diet (i.e. deficiency of nutrients) (Reference Murphy, Yates, Atkinson, Barr and Dwyer1, Reference Keusch2). In this way, some of the basic concepts which lay the foundations of the science of human nutrition were discovered – the need for adequate nutrition for the maintenance of body function and consequently good health (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Afshin, Sur and Fay4, Reference Kocarnik, Compton and Dean5). In more recent decades, human nutrition has evolved beyond mere avoidance of nutrient deficiency and developed so that we can aim to consume a diet that will support optimum health (Reference Forouhi and Unwin6, Reference Kirkpatrick, Vanderlee, Dias and Hanning7). Nutritional advice has broadened to include the prevention of lifestyle-related chronic diseases such as cardiovascular disease and type 2 diabetes and so has led to the concept of balanced nutrition for optimal health (Reference Pomerleau, McKee, Lobstein and Knai8). However, these modern-day afflictions of excess often co-exist alongside the immensely serious problem of undernutrition, which is still widespread in developing countries and among vulnerable groups of people living in developed countries (Reference Perez-Escamilla, Bermudez and Buccini9).
Adequate nutrition requires that all nutrients are consumed in adequate amounts and in the correct proportions. Adequate nutrition is required for functions such as growth and development in utero; physical growth in infancy, adolescence and other life stages; reproduction, pregnancy and lactation; repair of body tissues; and resistance to infection, among others (Reference Forouhi and Unwin6, Reference Kirkpatrick, Vanderlee, Dias and Hanning7). At birth, breast milk provides the perfect balance of nutrients. However, when we start to rely on a variety of foods, we require a balanced diet to maintain good health. In the following sections, we will consider important nutrients and other attributes within an optimal diet.
Energy
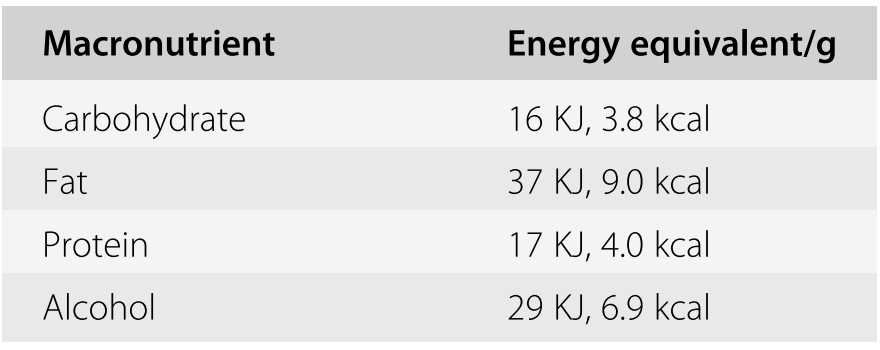
Energy is one of the most important things we obtain from food. In the body, energy consumed is used to support metabolic processes (digestion, absorption, excretion, growth) (Reference Shetty10, Reference Roberts, Heyman and Evans11). Energy intake is the sum of the energy content of macronutrients in the foods consumed – the total of carbohydrate, protein, fat and alcohol – with fat being the most energy dense (Table 1.1). When considering energy intake, it is important to ensure we consume enough for our specific requirements (Reference Shetty10, Reference Roberts, Heyman and Evans11). If we consume too much, we store excess energy for use in periods of energy deficit, leading to increased adiposity. To maintain a stable body weight, we need to balance intake and expenditure – this is known as energy balance.
Energy expenditure is made up of three components – basal metabolic rate (BMR), thermic effect of food (TEF) and physical activity (PA) (Reference Levine12). BMR refers to the energy required to maintain essential functions (e.g. heart rate and respiration). It is by far the largest component of energy requirements, accounting for approximately 70% of required energy. It varies by age, sex and body size. Alongside BMR, there is a specific component of energy associated with the digestion of food known as the TEF. This is caused by an increase in metabolic processes involved in the digestion, absorption and metabolism of foods that are consumed. This accounts for approximately 10% of our energy requirements. PA is used to describe physical movement, which includes movement during normal daily activities, as well as exercise. This can be the most variable aspect of energy expenditure, accounting for anywhere between 20% and 50% of our total energy requirements (Reference Levine12, Reference Donahoo, Levine and Melanson13). The recommended intake of energy will be discussed later, but it is important to note that excess energy consumed that is not utilised can be stored as fat (adipose tissue) or glycogen (muscles and liver). The adipose tissue is the largest energy store and, unlike glycogen, it has no limit and can continue to accumulate while the body is in positive energy balance. Excessive adiposity is known to cause increased risk of diseases such as type 2 diabetes and cardiovascular disease (Reference Franco, Ordunez and Caballero14).
Carbohydrate
Within the diet, the role of carbohydrates is to be a source of fuel, but overall carbohydrates are also part of energy stores, structural components of cell walls, part of nucleic acids (RNA and DNA) and part of many proteins and lipids (Reference Lanham-New, Hill, Gallagher and Vorster3). There are many different types of carbohydrates which differ by their basic structure. This difference in structure also affects how easily they are digested, with more complex structures taking longer to digest than simple carbohydrates, which are readily broken down during digestion (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Buttriss and Stokes15, Reference Seal16). Fibre is part of the carbohydrate family – and a very important but quite complex nutrient. The exact definition of fibre is often open to question. Generally, it is an indigestible complex carbohydrate found in plants. Fibre can either be classified as ‘soluble’ or ‘insoluble’ and ‘digestible’ or ‘indigestible’. Insoluble fibre is essentially a bulking agent which helps to prevent constipation and maintain gut health. A low fibre intake is known to be associated with constipation and gut disease (Reference Buttriss and Stokes15, Reference Seal16). The recommended intake for adults varies slightly according to different national guidelines but ranges between 18 g and 25 g per day (Reference Agostoni, Bresson and Fairweather Tait17). In the diet, the main sources of carbohydrate include starchy foods such as bread, cereal, potatoes, rice and pasta and foods and drinks containing sugars such as milk, fruits and confectionery. Carbohydrates are the most important form of energy in the diet, usually contributing between 40% and 60% of energy intake. Major sources of fibre are fruits, vegetables, pulses or legumes, wheat bran, seeds, brown rice and whole-grain products such as breads, cereals and pasta (Reference McGowan, O’Sullivan and Kehoe18, Reference McCarthy, Kehoe, Flynn and Walton19, Reference Kehoe, Walton, McNulty, Nugent and Flynn20).
Protein
Protein is the most abundant nitrogen-containing compound in the diet. It is a major functional and structural component of all body cells. Proteins consist of one or more chains of amino acids, with each protein having a unique sequence of amino acids. Amino acids have the same central structure with a carboxylic acid (COOH) and amino nitrogen (NH2) group. Proteins’ roles in the body include acting as enzymes and messengers/signallers (hormones), as well as having essential parts to play in growth, gene expression and immune function (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Young, Gersovitz, Munro, Moment, Adelman and Roth21, Reference Wu22). Protein requirements have been defined by the World Health Organization (WHO) as
the lowest level of dietary protein intake that will balance the losses of nitrogen from the body, and thus maintain the body protein mass, in persons at energy balance with modest levels of physical activity, plus, in children or in pregnant or lactating women, the needs associated with the deposition of tissues or the secretion of milk at rates consistent with good health. (23)
However, it is also important that protein intakes are considered in terms of both the amount and quality, with an appropriate consumption of required amino acids. Amino acids may be categorised as essential (they need to be provided in the diet as the body cannot synthesise them), conditionally essential (there is a measurable limitation to the rate at which they can be synthesised) or non-essential (they can be synthesised in adequate amounts in the body) (Table 1.2) (Reference Wu22).
Table 1.2 Amino acid classification
| Essential | Non-essential | Conditionally essential |
|---|---|---|
| Leucine, isoleucine, valine, phenylalanine, tryptophan, methionine, lysine, histidine, threonine | Tyrosine, cysteine, arginine, glutamine, glycine, proline | Selenocysteine, glutamate, aspartate, asparagine, alanine, serine |
Protein can also provide energy and typically provides 10–15% of dietary energy. Food sources are generally split into proteins of animal origin and proteins of plant origin. Good dietary sources of animal protein are meat, cheese, eggs and fish. Good dietary sources of plant protein are beans, pulses, nuts and cereal products (Reference Hone, Nugent, Walton, McNulty and Egan24).
Fat
Fats, also known as lipids, are composed of a carbon skeleton with hydrogen and oxygen substitutions. They can be classified into four categories, namely simple (e.g. triacylglycerol or cholesterol esters vitamin A and D), complex (e.g. phospholipids or lipoproteins), derived (e.g. fatty acids) and miscellaneous (e.g. carotenoids and vitamins E and K) (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Hayes25, Reference Foster, Williamson and Lunn26). With respect to diet, the main components of dietary fat are fatty acids (FAs). FAs are defined by the number of carbon atoms, the number of double bonds and the position of the first double-bond acids. How we name FAs is quite complex, with both common names and structured naming systems applied. The basic rule is that there are three parts: first, the number of carbons; second, the number of double bonds; and finally, the position of the first double bond (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Foster, Williamson and Lunn26). For example, the common dietary saturated FA stearate is C18:0 because it has 18 carbons and no double bonds. FAs can be both saturated (all single bonds) and unsaturated (one or more double bonds). The presence of double bonds leads to a change in the structure of the FAs. FAs with a single double bond are known as monounsaturated FAs, and two or more double bonds are known as polyunsaturated FAs. Lipids have three major functions – structural, storage and metabolic. Structural fat can include lipids associated with cell membranes (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Hayes25, Reference Foster, Williamson and Lunn26). These consist of a continuous double layer of lipid molecules into which proteins are embedded. There are three major classes of lipids in cell membranes – phospholipids, cholesterol and glycolipids, with phospholipids being the most common. Dietary fat is predominantly stored in the form of triacylglycerols (TAGs). TAGs are formed by linking FAs with an ester linkage to three alcohol groups in glycerol. These are the form in which fat is stored in adipose tissue and can be used as a fuel source during lipolysis, where fat stores are broken down. An example of a lipid with metabolic functions would be as a precursor to hormones such as steroids and eicosanoids (Reference Lanham-New, Hill, Gallagher and Vorster3). Fats in the diet are found in meat, in processed cooking fats such as oils, butter and spreads and in dairy products such as milk, cheese and cream. The average daily energy derived from fat in a typical diet ranges between 35% and 40% of total energy and consists mainly of triglycerides. The recommended intake of fat is between 20% and 35% of total energy intake (Reference Feeney, Nugent and McNulty27, Reference Li, McNulty and Tiernery28, Reference Linseisen, Welch and Ocke29). The intake of saturated fats is recommended to be less than 10% of total dietary energy (Reference Jacobson, Maki and Orringer30, Reference Eckel, Jakicic and Ard31, 32). However, recent evidence has opened a debate on the intake of saturated fat in particular (Reference De Souza, Mente and Maroleanu33). In a large review and meta-analysis, de Souza examined associations between intake of total fat and saturated fat with all-cause mortality and morbidities. From their analysis, they suggested that saturated fat intake was not associated with all-cause mortality or other metabolic diseases (Reference De Souza, Mente and Maroleanu33). Others have also examined this relationship by specific food groups, with similar findings (Reference Drouin-Chartier, Brassard and Tessier-Grenier34, Reference Alexander, Bylsma and Vargas35). Despite these more recent findings, the most recent review of published literature by the UK Scientific Advisory Committee on Nutrition (SACN), the body who provides independent scientific evidence for the development of public health guidelines in the UK, concluded that there is a significant body of evidence demonstrating a relationship between intake of saturated fats and cardiovascular disease and coronary heart disease events (36). They noted that, irrespective of the lack of evidence for an effect on mortality, non-fatal cardiovascular disease and coronary heart disease events have a serious adverse impact on health and quality of life, and that existing public health recommendations for saturated fat, at <10% total energy, are to be maintained (36).
Vitamins and Minerals
Vitamins and minerals are essential components of the diet. There are a number of known vitamins, which can be broadly split into water-soluble vitamins and fat-soluble vitamins. B vitamins, vitamin C, biotin, folic acid, niacin and pantothenic acid are water soluble (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Dattola, Silvestri and Bennardo37). Vitamins A, D, E and K are fat soluble (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Dattola, Silvestri and Bennardo37, Reference Maqbool, Aslam, Akbar and Iqbal38). This solubility has a significant influence on the metabolism, storage and functioning of the vitamin. If we do not consume enough of each of these vitamins, we can become deficient in that vitamin, which means that whatever function it is supposed to do in the body is neglected (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Dattola, Silvestri and Bennardo37, Reference Maqbool, Aslam, Akbar and Iqbal38). For example, vitamin C is an essential cofactor in numerous enzymatic reactions such as the biosynthesis of collagen and the regulation of gene expression. Severe vitamin C deficiency has been known for many centuries as scurvy (Reference Carr and Rowe39). By the late 1700s, it was commonly known that scurvy could be cured by eating oranges or lemons, even though vitamin C was not isolated until much later, in the 1930s (Reference Carr and Rowe39).
Non-nutrients
Regular consumption of fruits, vegetables, whole grains and other plant foods has been shown to have an inverse relationship with the risk of developing chronic diseases, and these foods provide not only a range of vitamins, minerals and fibre but also a range of different bioactive compounds, including phytochemicals (Reference Mitra, Tareq and Das40, Reference XTruzzi, Tibaldi, Zhang, Dinelli and D′ Amen41). There are over 5,000 different phytochemicals identified to date and they each have specific roles in plant reproduction, growth, metabolism and defence, as well as contributing to plant colour (Reference Mitra, Tareq and Das40, Reference XTruzzi, Tibaldi, Zhang, Dinelli and D′ Amen41). Taking polyphenols as an example, polyphenol intake is hard to estimate because of large variations in plants influenced by season, harvesting conditions, processing and many more factors. While there is limited data on the consumption of phytochemicals overall, there has been a huge amount of research on the relationship of polyphenols to health outcomes, and emerging research suggests that consuming a diverse range of phytochemicals from fruits, vegetables, pulses and whole grains is beneficial for health (Reference Tomas-Barberan and Andres-Lacueva42, Reference Rajha, Paule and Aragonès43). Therefore, consumers should obtain their nutrients, antioxidants, bioactive compounds and phytochemicals from a balanced diet with a wide variety of fruits, vegetables, whole grains and other plant foods for optimal nutrition, health and well-being.
Nutrient Requirements
Establishing nutrient requirements was and still is considered one of the major steps in the derivation of food-based dietary guidelines (FBDGs). Nutrient requirements are quantitative nutrient intake goals or targets, known as recommended daily allowances (RDAs) or dietary reference values (DRVs), set to meet the needs of the majority of the population (Reference Barr44). During the 1950s, research in nutrition led to the emergence of the concept of the role of diet in health promotion, as opposed to mere prevention of nutrient deficiency. This in turn led to the recognition that guidance was needed on consumption of energy and some macronutrients (total and saturated fat), as well as components in the diet such as sugar, salt and fibre. This led to the idea of dietary guidelines advising populations to reduce fat, salt or sugar. In more recent decades, research focussing on the role of other nutrients (including vitamins and minerals) in health promotion and prevention of chronic conditions such as obesity, cardiovascular disease, type 2 diabetes, osteoporosis and some cancers has led to increasing recognition that even micronutrients may be required in optimal amounts (Reference Barr44, Reference Murphy, Yates, Atkinson, Barr and Dwyer45, 46, Reference Jensen and Binkley47). Therefore, although RDAs were originally designed to help protect against deficiency of nutrients, the association of nutrition with the development of chronic disease led to them also defining optimal levels of intake (Reference Barr44, Reference Murphy, Yates, Atkinson, Barr and Dwyer45, 46, Reference Jensen and Binkley47).
To more fully understand what is meant by optimal levels of intake, it is important to consider the levels of nutrient adequacy (Reference Meyers, Hellwig and Otten48). For most nutrients, a stepwise understanding of nutrient adequacy can be established, ranging from optimisation of body stores or status to prevention of clinical deficiency (Figure 1.1). When considering body stores, we can store some nutrients within cells and organs within our body. When we have fluctuating intakes, we use these stores. If we have no intake, the stores go down – like a petrol tank. If you do not put the petrol in, the light comes on saying petrol is low, and eventually there is none left. Our body has biochemical measures that act similarly to the petrol light to tell us we are low but still have some petrol/nutrient in the tank. If not repleted, body stores will continue reducing and the function associated with that nutrient cannot be completed. Keeping with the car analogies, if we run out of petrol, we cannot drive; if we run out of water to clean our windscreen, we cannot clean it. Both are separate; each has a specific function which cannot be completed without the petrol/water. In the case of the water, the car/body can still function (because it has petrol) but it is not working at its best. With each nutrient, before we see signs of deficiency there are mild/undetectable symptoms, and these are the symptoms that begin to appear when stores are low and the body is not working as well as it should (Reference Barr44, Reference Murphy, Yates, Atkinson, Barr and Dwyer45, 46, Reference Jensen and Binkley47, Reference Meyers, Hellwig and Otten48) (Figure 1.1). For example, when our body is low in iron, say, we could feel tired and sluggish before we show overt signs of anaemia. Understanding this pathway for each nutrient allows for the development of dietary reference values, which aim for optimal levels of a nutrient for each population group (Reference Meyers, Hellwig and Otten48).

Figure 1.1 Stages in nutrient deficiency.
DRVs are the complete set of quantitative nutrient reference values for nutrients, indicating the specific amount of a nutrient that healthy people need depending on their age and sex (Reference Barr44, Reference Murphy, Yates, Atkinson, Barr and Dwyer45). DRVs include recommendations for average, upper and lower levels of intake (Table 1.3). Recommendations are given by nutrients, not foods. Instead of recommending portions of meat, fish or eggs, DRVs recommend a certain amount of protein intake in grams or recommended intake of folate in µg. It is also important to note that DRVs should not be viewed as recommendations for individuals. Rather, they are reference intakes for a population average (Reference Barr44, Reference Murphy, Yates, Atkinson, Barr and Dwyer45).
Table 1.3 Dietary reference value definitions and nomenclature
Recommendations about nutrient intakes are based on data and the distribution of the specific variable in a population (Reference Murphy, Yates, Atkinson, Barr and Dwyer45, Reference Jensen and Binkley47, 49). A combination of random genetic and environmental factors causes individuals to cluster near the average for many traits we measure, with fewer at extremes away from the average. Plotting this information for any given trait in a population results in a curve known as a normal distribution curve (Gaussian distribution). We use this concept of normal distribution curves in determining nutrient requirements, where the peak of the curve is equal to the average requirement for that population, with half of the population having requirements above and half of them having requirements below this point. This is normal for many measurements in a population – each individual will vary so that some require more, some less. Statistical calculations calculate the mean (or average) and the statistical variation around that average, called the standard deviation (SD). The mean of a normal distribution plus two standard deviations means that 97.5% of the population’s requirements or needs are met, so only the top 2.5% fall outside this. Using this approach, the statistical distribution of each individual nutrient can be calculated. As shown in Figure 1.2, the average requirement is set at the mean, with the PRI at the mean plus two standard deviations – so the requirements for 97.5% of the population will be met. The lowest threshold is set at the mean minus two standard deviations and the tolerable upper limit, which is above the PRI (Reference Murphy, Yates, Atkinson, Barr and Dwyer45, Reference Jensen and Binkley47, 49).
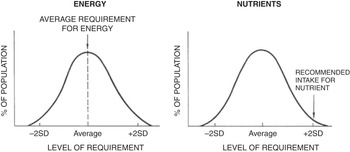
Figure 1.2 Nutrient and energy distribution curve.
Consumption of most nutrients greater than requirements is generally not harmful (except for energy) (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Shetty10, Reference Roberts, Heyman and Evans11). For energy, we do not recommend intakes at the mean plus two standard deviations as this would mean that 97.5% of population needs are being met, but many people are consuming more than they need. Therefore, if we set the energy needs for the population near to the highest requirement, we would be asking most of the population to be consuming above their requirements, resulting in weight gain. Over time, small imbalances in energy intake (EI) to energy expenditure (EE), where EI is greater than EE, can lead to overweight and obesity (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Shetty10, Reference Roberts, Heyman and Evans11). Energy recommendations are therefore given at the average for the population and we use the estimated average requirement (EAR) (Reference Lanham-New, Hill, Gallagher and Vorster3, Reference Shetty10, Reference Roberts, Heyman and Evans11) (Figure 1.2).
RDAs are set for healthy populations and are not applicable to those who have different illnesses or conditions as their nutrient requirements are completely different (Reference Murphy, Yates, Atkinson, Barr and Dwyer45, Reference Jensen and Binkley47, 49). Nutrient requirements vary with age, sex and physiological condition because of differences in growth for younger age groups and age-related changes in nutrient absorption and body functions and/or functional capacity. For this reason, DRVs are developed for different life stages and sex groups (Reference Murphy, Yates, Atkinson, Barr and Dwyer45, Reference Jensen and Binkley47, 49). Separate reference values are also established for pregnant and lactating women, taking into account the additional nutrient requirement for the formation of new tissues or to compensate for the nutrients lost to the body in the form of human milk, respectively, and considering the physiological adaptations that occur during these conditions. The European Food Safety Authority (EFSA) provides ongoing scientific opinions on DRVs to ensure they are underpinned by the latest available knowledge. In 2020, EFSA launched an interactive tool called the DRV Finder that searches by population group or nutrient based on their published opinions (Reference Herforth, Arimond and Álvarez-Sánchez50).
Food-Based Dietary Guidelines
While we accurately derive and set specific population nutrient requirements, people eat food, not nutrients – yet it is the combination of nutrients in food that determines the health of the individual. Nutritionists think of the foods that we eat in terms of the nutrients they provide. A balanced diet must provide the following basic nutrients: proteins, fats, carbohydrates (including fibre), vitamins, minerals and water, but the difficulty is that all of these nutrients are necessary in different quantities. So, how do nutritionists communicate the concept of good nutrition to the public? It is ironic that this most fundamental cornerstone in human nutrition simultaneously remains one of the most challenging areas for nutrition scientists. The translation of nutrient requirements for good health into the foods that people should eat is a complex and indeed sometimes contentious process. FBDGs are the translation of nutrients to food and are often referred to as ‘healthy eating guidelines’ or ‘healthy eating advice’. The nutrients needed for health are translated into the amounts and types of foods that are required to achieve a balanced diet. Government organisations and nutrition scientists are usually responsible for formulating and conveying these recommendations for healthy eating to the population (Reference Smitasiri and Uauy51, Reference Erve, Tulen and Jansen52, Reference Turrini, Leclercq and D’Amicis53, 54).
FBDGs are to be used by governments as part of their national health strategies for health promotion. In 1992, the United Nations Food and Agricultural Organization (FAO) and the WHO identified that one major strategy to improve the nutritional status of populations was to call upon governments to provide quantitative and qualitative dietary advice to the public for different age groups and lifestyles. Later in 1995, the WHO/FAO jointly organised an expert consultation titled ‘Preparation and use of food-based dietary guidelines’, where it was concluded that FBDGs needed to take account of factors such as current dietary practices and habits and prevailing public health problems rather than nutrient requirements alone (55). The resulting WHO/FAO expert consultation report highlighted the rationale for FBDGs. There was established evidence for nutrition in health and disease prevention and complex science needed to be translated into practical guidance for people. The original concept of FBDGs took into account both the scientific evidence and epidemiological data linking specific food consumption patterns with low incidence of certain diseases, while not requiring a complete understanding of the underlying biological mechanisms. This report noted some important points that form the basis of the development of FBDGs (55). Foods make up diets but foods are more than just a collection of nutrients. There is already good evidence from studies (animal, clinical and epidemiological) that specific dietary patterns are associated with a reduced risk of specific diseases. For certain micronutrients, evidence suggests that intake higher than present nutritional recommendations may help to lower the risk of non-communicable diseases. However, scientific evidence has not yet identified the potential health outcomes of some non-nutrient food components (55).
More recently, in 2010, an expert panel of EFSA issued specific recommendations to be followed for a stepwise approach for the derivation of FBDGs (Reference Flynn, O’Brien, Ross, Flynn and Burke56). In the European Union, there are 27 member nations with very diverse populations. Therefore, each government needs to identify their priorities in terms of public health issues. The diet–disease relationships that exist in a particular country or region need to be established and FBDGs need to be developed that are in line with other existing policies relevant to health promotion. For example, there may be physical activity or alcohol policies already in existence and FBDGs need to be integrated where possible with these. The inclusion of stakeholders early on in the development of the guidelines is an important step in ensuring that the final outcome is acceptable (Reference Flynn, O’Brien, Ross, Flynn and Burke56). The final result should be a food guide that is consistent, easily understood and memorable. The key recommendations of this report were as follows:
1 Identify diet–health relationships relevant to a particular nation
2 Identify nutrients of public health importance
3 Identify foods relevant to FBDGs
4 Identify food consumption patterns
5 Test/optimise FBDGs
6 Consider graphic representation of FBDGs
7 Implement and monitor FBDGs’ impact
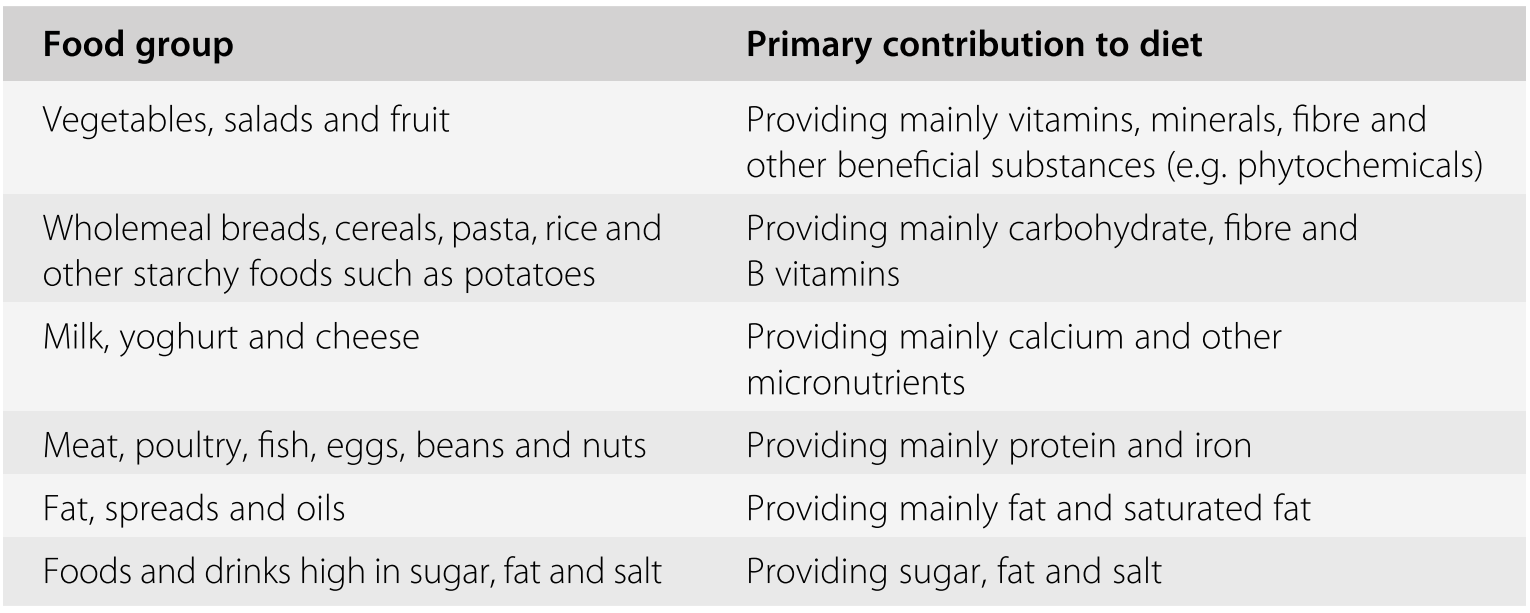
While the science has evolved, the rationale for the development of FBDGs remains the same. Most importantly, FBDGs need to be underpinned by strong scientific evidence written or produced in a very simple, easy-to-understand format. In practice, when considering food-based recommendations, foods that are similar are grouped into food groups. This means we can give recommendations based on food groups rather than a mix of individual foods. Each food group provides specific nutrients or has a specific function in the body. The major food groups often depicted or considered in FBDGs include the specific food groups, or variations of these, depending on the source. The key attributes and nutrients associated with each food group are also listed (see Table 1.4) (Reference Flynn, O’Brien, Ross, Flynn and Burke56).
Table 1.4 Food groups used in food-based dietary guidelines
Food items providing energy but few nutrients are grouped into the food group ‘Foods and drinks high in sugar, fat and salt’ – these include foods such as confectionery, cakes, biscuits, chocolate, crisps, savoury snacks and so on. Recommended intakes of these food groups are given as portions per food group and often depicted in a visual way to help the consumer understand which food groups to eat more or less. On this basis, using a pyramid as a visual, the food group ‘Vegetables, salads and fruit’ would be depicted at the bottom, with the greatest recommended intake of portions, and the food group ‘Foods and drinks high in sugar, fat and salt’ depicted as the smallest food group at the top (Reference Flynn, O’Brien, Ross, Flynn and Burke56).
The types of foods eaten in different countries are influenced by factors such as ethnicity, culture, dietary habits, food preferences, intake patterns and food availability, and so the classifications and types of foods contained in the major food groups can vary somewhat from country to country (Reference Smitasiri and Uauy51). For example, in Ireland and the UK, potatoes are consumed as a major staple, contributing mainly to carbohydrate intake, and so are included in the group ‘Wholemeal breads, cereals, pasta, rice and other starchy foods’. However, in other countries, where they are eaten less frequently, they may be considered only in the group ‘Vegetables, salads and fruit’ (Reference Flynn, O’Brien, Ross, Flynn and Burke56). Similarly, the number of food groups used may differ in different national food guides. For instance, the USA and Canada split their ‘Vegetables, salads and fruit’ group into one food group for ‘Fruit’ and a separate food group for ‘Vegetables’. The pictorial display of the guidelines varies from country to country and can be in the form of a plate (UK), a pyramid (USA, Ireland), a rainbow (Canada), a pagoda (China, Korea) or a circle (Australia, Germany, Sweden) (Reference Smitasiri and Uauy51).
Conclusion
The basic principle of nutrition is the provision of adequate nutrients for populations or groups within populations. Recommendations for nutrient intakes are based on scientific evidence, using a variety of information to determine recommended intake, as well as higher and lower levels. Each nutrient’s recommended intake is linked to its function and specific requirements in the body. While these are precise and specific, they lack relevance for the general public, and as such are translated into FBDGs. These aim to provide consumer-friendly food recommendations for people to achieve a nutritionally adequate balanced diet for optimal health and reduced risk of disease.