Book contents
- Immunohistochemistry in Diagnostic Dermatopathology
- Immunohistochemistry in Diagnostic Dermatopathology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface and Acknowledgments
- Chapter 1 Introduction to Immunohistochemistry
- Chapter 2 Epithelial or Squamous Neoplasms
- Chapter 3 Neoplasms of Cutaneous Appendages
- Chapter 4 Inflammatory Dermatoses Mimicking Lymphomas
- Chapter 5 Cutaneous Lymphoid Neoplasms
- Chapter 6 Melanocytic neoplasms
- Chapter 7 Soft Tissue Neoplasms
- Chapter 8 Miscellaneous Tumors
- Chapter 9 Detection of Genetic Syndromes
- Chapter 10 Immunobullous Disorders
- Chapter 11 Cutaneous Infections
- Chapter 12 Therapeutic and Prognostic Applications
- Index
- References
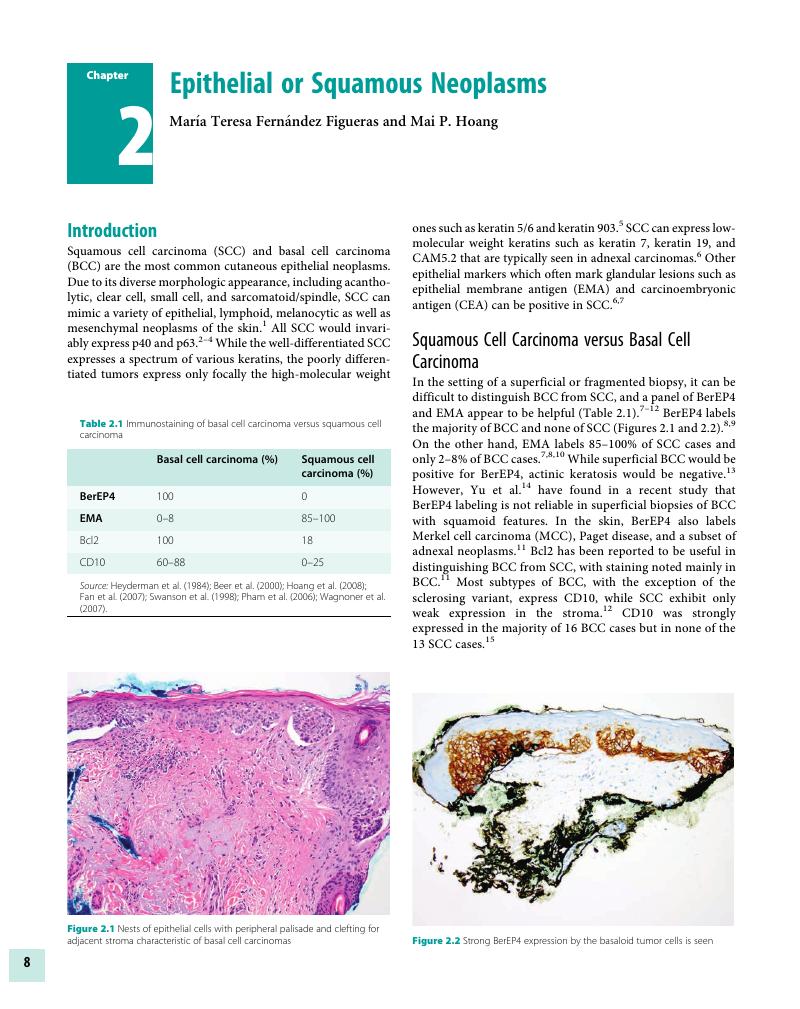
Chapter 2 - Epithelial or Squamous Neoplasms
Published online by Cambridge University Press: 04 November 2017
- Immunohistochemistry in Diagnostic Dermatopathology
- Immunohistochemistry in Diagnostic Dermatopathology
- Copyright page
- Dedication
- Contents
- Contributors
- Preface and Acknowledgments
- Chapter 1 Introduction to Immunohistochemistry
- Chapter 2 Epithelial or Squamous Neoplasms
- Chapter 3 Neoplasms of Cutaneous Appendages
- Chapter 4 Inflammatory Dermatoses Mimicking Lymphomas
- Chapter 5 Cutaneous Lymphoid Neoplasms
- Chapter 6 Melanocytic neoplasms
- Chapter 7 Soft Tissue Neoplasms
- Chapter 8 Miscellaneous Tumors
- Chapter 9 Detection of Genetic Syndromes
- Chapter 10 Immunobullous Disorders
- Chapter 11 Cutaneous Infections
- Chapter 12 Therapeutic and Prognostic Applications
- Index
- References
Summary
- Type
- Chapter
- Information
- Immunohistochemistry in Diagnostic Dermatopathology , pp. 8 - 26Publisher: Cambridge University PressPrint publication year: 2017

