Book contents
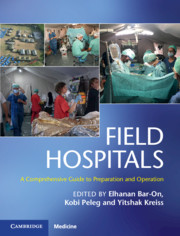
- Field Hospitals
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Chapter 25 - Infectious Diseases and Public Health in a Field Hospital
from Section 4 - Clinical Considerations
Published online by Cambridge University Press: 09 January 2020
- Field Hospitals
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Summary
Field hospitals can play a key role in the clinical treatment and public health management of infectious diseases during emergency situations, both in the setting of disasters primarily of an epidemic nature and of outbreaks that result secondarily in the midst of other crises. Planning and preparation are key components to successful operation in these settings and present unique issues compared to more routine field hospital scenarios absent a contagious threat. Special consideration needs to be given to site selection, the physical structure of a facility, infection prevention and control measures, personal protection, selection and training of staff, data collection and sharing, and clinical standard operating procedures. The mission of field hospitals can be expanded beyond clinical care to help stabilize epidemics through ensuring basic living conditions are available, including the provision of adequate food, clean water, sanitation, and shelter. The public health focused activities of a field hospital should include community-based prevention and health promotion activities, risk communication, and disease surveillance and control: all of which may provide invaluable contributions to broader public health response efforts during crisis.
Keywords
- Type
- Chapter
- Information
- Field HospitalsA Comprehensive Guide to Preparation and Operation, pp. 245 - 255Publisher: Cambridge University PressPrint publication year: 2020
References
- 1
- Cited by