Introduction
Overcoming care fragmentation remains among the key challenges facing health systems globally (Reference Nolte and McKeeNolte & McKee, 2008; Reference SainiSaini et al., 2017; Reference SchoenSchoen et al., 2011). This has become particularly acute against the background of a changing disease burden and the rising number of people with multiple health problems. Policy-makers have recognized this challenge and countries are exploring new approaches to health care delivery to enhance the coordination of care and so better meet the needs of those with chronic and multiple health problems and optimize service use (Nolte, Knai & Saltman, 2014; Reference WodchisWodchis et al., 2015; World Health Organization Regional Office for Europe, 2016). The focus has tended to be on the service provider side, with the introduction of innovative care models such as through strengthening multidisciplinary team work, the use of care coordinators or case managers, co-location of different providers, and shared pathways, among other developments (Reference Nolte and KnaiNolte & Knai, 2015). The need for involving the individual and their family is widely recognized, although more often than not the focus tends to be on educational elements emphasizing knowledge and adherence to expert advice.
Yet individuals have an important role to play in protecting and promoting their own health, deciding on appropriate approaches to maintain health and managing chronic conditions and the impacts they have on life and well-being (National Reference VoicesVoices, 2014). There is a range of ways by which people take an active role in their own care, including through shared decision-making, care planning and self-management (see Chapter 11). While conceptually different (Reference LhussierLhussier et al., 2015), the fundamental notion underpinning each is their aim to engage patients in decisions about their care (Reference Coulter and CollinsCoulter & Collins, 2011; Reference CoulterCoulter et al., 2015) and that service users and their carers should form an integral part of the care process (Health Reference FoundationFoundation, 2014). This is seen to be of particular relevance in the context of chronic disease, which confronts those affected with a spectrum of needs and requires them to manage the impact of the illness on physical, psychological and social functioning, to interact with health care providers and implement treatment regimens, to monitor their health status and make associated care decisions, to alter their behaviour and to engage in activities that promote physical and psychological well-being (Reference ClarkClark, 2003). Service users inevitably become a major caretaker and thus a core part of the ‘workforce’ in chronic care (Reference Dubois, Singh, Jiwani, Nolte and McKeeDubois, Singh & Jiwani, 2008).
This chapter focuses on self-management and self-management support, which are considered to be core components of person-centred care (International Alliance for Patients’ Organizations, 2006; National Reference VoicesVoices, 2014; Health Reference FoundationFoundation, 2014). Self-management support is seen to be key to enable service users to move from passive recipients to active partners in care (World Health Organization Regional Office for Europe, 2016). Most often conceptualized in the context of chronic, long-term health problems, it features as one of the four interacting components of the Chronic Care Model that are considered to be essential to providing high-quality care for those with chronic disease (Reference WagnerWagner, 1998). Many countries in Europe and elsewhere have included self-management support as an integral component of national, regional or local strategies, and approaches to service delivery that aim to better meet the needs of people with long-term health problems (Reference Nolte and KnaiNolte & Knai, 2015; Nolte, Knai & Saltman, 2014; World Health Organization Regional Office for Europe, 2016).
A range of expectations has been associated with self-management and support interventions and policies in this context. For example, it is anticipated that supporting service users recognizes their own knowledge and capacity, that it increases their confidence, strengthens preventive activities and ensures appropriate use of services, and will thus reduce costs and make service delivery more sustainable. There is also an expectation that it will improve service users’ experiences of health care, and give people more control over their lives, empower them as partners and improve health outcomes and well-being. Yet, as Reference MorganMorgan et al. (2016) argued, it remains unclear “how all these promising ideas hang together” (p. 2), or whether (and how) these ambitions can be achieved simultaneously (Reference Entwistle, Cribb and OwensEntwistle, Cribb & Owens, 2016). There is evidence that some forms of support for self-management can impact positively on some of these anticipated outcomes for some service user groups (Reference FranekFranek, 2013; Reference TaylorTaylor et al., 2014), but not all aims have been met. In particular, robust evidence that self-management efforts will reduce service utilization has so far been established for selected (hospital) services and selected conditions only (National Reference VoicesVoices, 2014; Reference TaylorTaylor et al., 2014). Reference Entwistle, Cribb and OwensEntwistle, Cribb & Owens (2016) also contended that practices seeking to support self-management can, at times, undermine rather than enhance people’s experiences of health care.
This chapter explores some of the key issues pertaining to contemporary policy and practice around self-management and support in the context of wider efforts to enhance care coordination in a move to more person-centred systems. It begins by summarizing common definitions of self-management and self-management support and a brief description of what we know about the availability of self-management support strategies in European settings. We then discuss key insights from the evidence base on the impact of self-management interventions. We examine in greater detail some of the challenges facing service users, practitioners and policy-makers in conceptualizing and implementing relevant strategies and discuss policy implications.
Defining self-management and self-management support
Reference KendallKendall et al. (2011) traced the emergence of self-management in the health field to the self-care and self-help movements that evolved from the 1970s in particular, although early accounts date at least to the 18th century. A focus has been on achieving equality between the provider and service user in terms of making decisions and the capacity to determine the direction of their own care. Mirroring the wider discussion around person-centredness (Chapter 2), interpretations of self-management have since developed in different ways, largely reflecting different disciplinary and professional perspectives and expectations in the context of a changing health care environment, which involves technological advances, the rising burden of chronic disease and the increasing need for cost-containment.
Against this background, it is not surprising that there is no single, universally accepted definition of self-management and self-management support, and the scope of what is considered varies. In an early review, Reference ClarkClark et al. (1991) distinguished between self-care and self-management, with the former referring to a wide range of preventive behaviours and actions taken by those who are healthy or are at risk of ill-health.
Self-management, in contrast, was interpreted in the context of chronic disease and was seen to refer more specifically to the active participation of people in their own treatment, undertaking related tasks and activities with the collaboration and guidance of the individual’s physician and other health care providers (Reference ClarkClark et al., 1991; Reference LorigLorig, 1993). However, although self-care and self-management (and indeed self-management support) form distinct multidimensional constructs (Reference JonesJones et al., 2011), boundaries between concepts have increasingly blurred and related terms are now often used interchangeably in health policy and research literature (Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt, 2014).
As noted, self-management is most often conceptualized in the context of chronic disease, and this is further illustrated by a widely used definition proposed by the Institute of Medicine. It describes self-management as “the tasks that individuals must undertake to live well with one or more chronic conditions. These tasks include having the confidence to deal with medical management, role management, and emotional management of their conditions” (Reference Adams, Greiner and CorriganAdams, Greiner & Corrigan, 2004, p. 57). One other widely cited definition is that proposed by Reference BarlowBarlow et al. (2002), suggesting a broader conceptualization that also takes account of the wider psychosocial context within which people live. Accordingly, self-management includes “the individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition” (p. 178). Reference VassilevVassilev et al. (2011) further highlighted the role of social networks in the management of long-term health problems.
Reference Corbin and StraussCorbin & Strauss (1985) identified, based on in-depth interviews with middle-aged and older couples in the USA, three types of ‘work’ that those with chronic illness have to undertake when managing their condition/s at home: illness work (medical management of the condition), everyday life work (maintaining, changing and creating new meaningful behaviours or life roles), and biographical work (managing the emotional impacts of having a chronic condition and its consequences). Building on this framework, Reference Lorig and HolmanLorig & Holman (2003) distinguished six core self-management skills: problem solving, decision-making, resource utilization, the formation of a patient–provider partnership, action planning and self-tailoring. These tasks form key components of the Chronic Disease Self-Management Programme (CDSMP) (Stanford Medical Reference SchoolSchool, 2017), developed by the same authors (Reference LorigLorig et al., 2001; Reference LorigLorig et al., 1999) and implemented widely since; we will discuss this programme below.
Self-management support has been defined as “the systematic provision of education and supportive interventions by health care staff to increase patients’ skills and confidence in managing their health problems, including regular assessment of progress and problems, goal setting, and problem-solving support” (Reference Adams, Greiner and CorriganAdams, Greiner & Corrigan, 2004, p. 57). This definition is reflective of the IOM’s more health-care-centred definition of self-management mentioned above. Yet support interventions and approaches extend further, as shown by Reference TaylorTaylor et al. (2014), who developed a taxonomy for self-management support. It considers four dimensions: (i) the recipient (patients, carers, health professionals, organizations); (ii) self-management components; (iii) modes of delivery (face to face, remote, telehealth care, web based); and (iv) people delivering the support (lay, professionals), with identified components summarized in Box 12.1.
Box 12.1 Taxonomy of self-management support as proposed by Reference TaylorTaylor et al. (2014)
Reviewing the evidence from 30 qualitative systematic reviews (covering 515 unique studies) and 102 quantitative systematic reviews (covering 969 RTCs), Reference TaylorTaylor et al. (2014) identified 14 types of component of self-management support, which may be directed at the patient or carer. These include: education about condition and management, information about available resources (financial, social), personalized action plan, regular clinical review, monitoring with feedback, practical support with adherence (medicine reviews, dosette boxes, prompts, reminder checklists), equipment, safety netting (e.g. specialist telephone advice), training to communicate with health professionals, training for activities of daily living (e.g. occupational therapy), training for practical self-management activities (e.g. inhaler technique instructions), training for psychological strategies (problem solving, action planning, goal setting, distraction, relaxation, etc.), social support (e.g. befriending, peer support or mentoring), and lifestyle advice and support (diet, physical activity, smoking cessation, handling life stresses).
Indirect components were those delivered to health professionals such as education and training (e.g. adult learning and communication skills), equipment (e.g. clinical information systems, protocols for disease assessment), prompts (e.g. reminders to discuss action plan), feedback and review (e.g. review from managers, on-site mentoring, monthly reports) and financial incentives, as well as those delivered at an organizational level such as training in implementing self-management, equipment including telehealth care tools, protocols for disease assessment, prompts incorporated into the clinical record system, audit and feedback at organizational level, and financial incentives.
What is happening across Europe?
Decision-makers across Europe have recognized the need for implementing policies and strategies to support self-management mainly in the context of chronic diseases (Reference ElissenElissen et al., 2013; Reference Nolte and KnaiNolte & Knai, 2015). Available overviews of best practice cases highlight that supporting the active participation of patients in their care is seen as a priority to optimally respond to patient needs and improve health outcomes (European Reference CommissionCommission, 2017; World Health Organization Regional Office for Europe, 2016).
However, approaches to self-management support vary widely between and within countries in terms of content, format, provider and availability (Reference ElissenElissen et al., 2013). For example, Reference KousoulisKousoulis et al. (2014) carried out a review of the literature on diabetes self-management arrangements in place in six European countries (Bulgaria, Greece, the Netherlands, Norway, Spain and the UK). Covering the period 2000–2013, the review included 56 studies that reported on 21 interventions and programmes for diabetes and chronic disease self-management. Two-thirds (n=13) of programmes and interventions were set in the UK, five in the Netherlands, one each in Norway, Spain and Bulgaria and none in Greece (where initial discussions and approaches had only started to emerge at the time of the study), typically located in primary care settings. The majority of approaches comprised educational or training programmes, typically, although not always, emphasizing behavioural change as an important goal while the mode and duration of related interventions varied. Other models included technological support tools, often web-based, that sought to strengthen self-monitoring abilities and individual responsibility, again with considerable variation in terms of focus and content.
Similar variation in the levels of support provided was demonstrated by Nolte, Knai & Saltman (2014) in a review of some 50 coordinated care approaches across 13 countries in Europe. The large majority of these approaches provided some form of patient self-management support, typically involving education for self-management, frequently delivered in a group-based context or on a one-to-one basis and most often in the context of disease management programmes. Education offered within the reviewed approaches tended to focus on disease control through the provision of information about the disease, healthy behaviours and practical instructions concerning, for instance, blood glucose monitoring, foot examination or insulin injection. Most approaches also sought to involve patients in the development of a care or treatment plan and goal setting, and provided regular assessment of patient needs and problems. They typically used support materials in the form of information brochures to complement patient education programmes, with a smaller number using interactive web sites or telephone-based support services to provide patients with personalized information on how to manage their disease. In the majority of cases, self-management support was provided by health professionals including physicians, or, more frequently, by trained nurses within primary care settings. Self-management support programmes provided by others, including lay people, were uncommon, but one well-known example includes the Expert Patient Programme in England (see below). Overall, the review found that while approaches to patient support for self-management had moved beyond the mere distribution of information materials, approaches in place tend to reflect service-driven programmes aimed at disease control rather than more general support strategies targeting the wider social context within which people live and drawing on a wider potential support network including other patients, peers or volunteers, among others.
Clearly, reviews such as those presented here risk overlooking examples of innovative practices locally (World Health Organization Regional Office for Europe, 2016). At the same time, it is also clear, in particular in the context of chronic diseases, that while countries are exploring a range of novel approaches to enhance care coordination and integration, and transform service delivery more broadly, strategic programmes and initiatives to strengthen self-management support appear to have remained relatively underdeveloped. We will return to the challenges of systematically implementing self-management support strategies later in this chapter.
What is the evidence?
Reviews of self-management support interventions have described improvements in selected health outcomes among people with chronic disease, including health-related quality of life and healthy behaviours (Reference FranekFranek, 2013; Reference PanagiotiPanagioti et al., 2014). There is also some evidence for the potential of such interventions to reduce health service utilization without compromising patient health outcomes, but observed effects tend to be small and the evidence was found to be strongest for respiratory and cardiovascular problems (Reference PanagiotiPanagioti et al., 2014). Focusing specifically on self-monitoring as one component of self-management, Reference McBain, Shipley and NewmanMcBain, Shipley & Newman (2015) found, in a review of systematic reviews, evidence of significant reductions in hospitalizations and readmissions to hospital, specifically for heart failure and chronic obstructive pulmonary disease (COPD). At the same time, their review also reported evidence suggesting that observed reductions in (re-)admissions may lead to increases in service use elsewhere in the health care system.
Reference TaylorTaylor et al. (2014), based on a review of the qualitative and quantitative evidence (see also Box 12.1), concluded that “overall, there appears to be a great deal of evidence, much of it favourable, relating to self-management support across most of the [chronic conditions] studied, but it is clear that not everything works” (p. 418). The authors found no one component to be superior to any other and the most effective interventions were multifaceted and multidisciplinary. They identified a set of core components common to self-management support that are applicable to most chronic conditions, for example education and the provision of knowledge and information about the condition, while noting that interactive learning was likely to be more effective than passive education and education provided in isolation. Some selected components were associated with specific characteristics of a given condition, such as support for activities of daily living for those with disabling conditions (e.g. stroke, lower back pain, progressive neurological disorders, COPD), action plans for those with conditions that are at risk of marked exacerbations (e.g. asthma, COPD), or intensive disease-specific training to enable self-management of specific clinical tasks (e.g. type 1 diabetes, home dialysis for people with chronic kidney disease). Importantly, they found that supported self-management needed to be tailored to the individual, their culture and beliefs, as well as taking account of the natural progression of the condition in order to be effective.
A number of studies and reviews have specifically focused on the effectiveness of the aforementioned CDSMP (Reference LorigLorig et al., 2001) and related strategies and found the evidence to be somewhat mixed (Reference FosterFoster et al., 2007). For example, Reference BradyBrady et al. (2013) conducted a meta-analysis of 23 studies of the CDSMP delivered in small English-speaking group mode. They demonstrated small to moderate improvements in psychological health and selected health behaviours such as exercise and cognitive symptom management that remained after 12 months. But they did not find robust evidence that the programme reduced health care utilization. This latter finding was confirmed in two Canadian studies that were also unable to demonstrate robust evidence for CDSMP reducing health service use (Reference JaglalJaglal et al., 2014; Reference LiddyLiddy et al., 2015).
Reference KendallKendall et al. (2012) highlighted the importance of the group context within which the CDSMP is being delivered. Based on insights from a focus group study of participants and peer leaders in Australia, they found that positive impacts such as increased knowledge, which led to an increased sense of confidence, perceptions of greater control and a positive attitude to their disease, crucially depended on the “social aspect of the group” (p. 7). Noting that self-management is at its core a social concept, their work pointed to the role of social processes including social engagement, the development of a collective identity, collaborative coping and shared learning in determining the outcomes achieved through CDSMP courses. This observation of the key role of the group context is further supported by Reference BradyBrady et al. (2013), who found that alternative delivery modes of the CDSMP (e.g. internet) had fewer significant improvements than the small English-speaking group mode. A recent scoping review of evidence of benefits and challenges from participating in group-based patient education programmes by Reference StenbergStenberg et al. (2016) also supports this conclusion. However, that review was unable to disentangle the effects of different types of intervention and it remains unclear whether the nature of the intervention or its mode of delivery is more important in enhancing self-reported outcomes such as reduced symptom distress or improved self-management skills.
What are the challenges?
We have seen above that there is evidence that some forms of support for self-management have impacted positively on some outcomes for some service user groups, but overall the evidence remains inconsistent. In particular, robust evidence that self-management efforts will reduce service utilization, and thus health care costs, remains weak. There are a number of reasons why this might be the case. For example, Reference PanagiotiPanagioti et al. (2014) suggested that strategies for self-management support vary in the way in which they explicitly seek to reduce service use, for example those specifically targeting the control of exacerbations in COPD. Others might aim to enhance patient empowerment more broadly, and the outcomes are therefore likely to vary. Targeting service use implicitly assumes that utilization is always user-led, which may, however, not be the case. Also, many self-management interventions have fairly limited impacts, and there is little robust data on long-term outcomes (Reference TaylorTaylor et al., 2014).
Reference Nolte and OsborneNolte & Osborne (2013) noted that part of the challenge lies in the use of outcome measures that do not adequately capture the intended impacts of self-management interventions, and measures are frequently developed without appropriate service user input (Reference BogerBoger et al., 2015). Others have highlighted concerns around the appropriateness of certain interventions, poor design or theoretical assumptions (or lack thereof) underlying the intervention. For example, a strong focus has so far been on psychological mechanisms around concepts such as self-efficacy and patient activation (Reference HibbardHibbard et al., 2004; Reference Lorig and HolmanLorig & Holman, 2003), which is also reflected in the frequency by which these mechanisms are represented in the literature (Reference Lu, Li and ArthurLu, Li & Arthur, 2014), while socioeconomic considerations have been incorporated less frequently. Interventions that are solely based on psychological models of self-management have been criticized “for their individualistic, biomedical and prescriptive focus on disease management” (Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt, 2014, p. 2). Such an approach, it is argued, failed to address lay understandings of self-management and the social context within which people live and which in turn shapes self-management practices (Reference OngOng et al., 2014). Reference Pickard and RogersPickard & Rogers (2012) also noted that programmes based on the CDSMP, such as the aforementioned Expert Patient Programme in England and similar approaches elsewhere (Reference LiddyLiddy et al., 2015; Reference HaslbeckHaslbeck et al., 2015; Reference ContelContel et al., 2015; Expert Patients Programme, 2012), aimed to train an “ideal typical, late-modern patient: responsible, self-directed and managing her own health” (p. 102). Such an approach, it is contended, involved an implicit shift in responsibility from the professional to the (lay) service user with regard to managing the disease and its psychosocial impacts (Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt, 2014). Related programmes are thus likely to benefit only that part of the population that is capable of taking up these roles, which, in turn, might increase health inequities (Reference KendallKendall et al., 2011).
Health care providers are increasingly encouraged to support people with chronic conditions to learn self-management skills. Indeed, education and training of health professionals in implementing self-management has been identified as an important component of self-management support interventions (Reference TaylorTaylor et al., 2014). Yet, as argued by Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014), such an approach implies a shared understanding of self-management between service users and providers, and this may not be a given. Using a systematic review and narrative synthesis of qualitative studies (n=55), the authors found important differences between lay and health professionals’ understandings of self-management. They also showed that these understandings differed from the dominant model of self-management that draws on the concept of self-efficacy underpinning approaches such as the CDSMP or the Expert Patients Programme. For example, health professionals tended to interpret self-management as a tool to promote compliance with expert advice and treatment, to monitor and control symptoms and engage in healthy behaviours, or what Reference MorganMorgan et al. (2016) referred to as ‘narrow approaches’ to self-management support (Box 12.2).
Box 12.2 Managing conditions well vs. managing (or living) well with conditions
Based on a synthesis of the evidence on health and social care professionals’ approaches to self-management support for people with chronic disease, Reference MorganMorgan et al. (2016) distinguished those which focus on supporting people to manage their condition(s) well in biomedical or disease-control terms (narrow approaches) from those that emphasize supporting people to managing well (or living well) with their condition(s) (broad approaches). In this interpretation, narrow approaches tend to focus on improving the control of symptoms and to reduce the risk of disease progression, exacerbations or complications. Forms of support are often limited to didactic education and motivation, and success is typically assessed using biomedical indicators, such as blood sugar levels in people with diabetes, or intermediate indicators such as behaviour change that will lead to changes in the biomedical indicators. Narrow approaches might take account of emotional issues, but this mostly seeks to encourage behaviour change to achieve disease control rather than to engage with patients’ lived experiences.
Conversely, the broader approach to self-management support was seen to be oriented towards supporting people to achieve a better quality of life, while also supporting the development of patients’ autonomy and self-determination. Measures of ‘success’ tend to consider progress in different domains such as people’s ability to adapt to and cope with their condition(s), their sense of control, and their ability to develop their own solutions to health-related problems. Forms of support are often characterized by a considerable degree of flexibility on the part of the practitioner, seeking to incorporate individuals’ circumstances and lived experiences, and creating scope for individuals to shape the agenda for discussion and action with their practitioners. The approach tends to be characterized by more “equitable and mutually respectful professional–patient relations” (p. 8) whereas the narrow approach was seen to underpin the more (traditional) hierarchical practitioner–patient model of communication.
The authors highlighted that broader approaches tend to be less evident in practice, which they linked, in part, to the challenges of implementing them within existing service delivery frameworks. Importantly, a considerable proportion of reviewed studies had concerned diabetes (~ 40%) and this could have impacted the wider focus on ‘narrower’ approaches to self-management support interventions in practice. This is mainly because in diabetes, disease-control measures (such as diet, exercise, monitoring and medication management) are particularly relevant in terms of their impact on the longer-term trajectory of the condition (complications such as blindness, neuropathy and vascular problems) and thus quality of life. These efforts are more easily measured through biomedical indicators such as HbA1 c and they incentivize a narrow approach (or disincentivize a move away from it). Such a focus will be less suitable for other conditions such as, for example, cancers or dementias where people can do less to control the disease and its progression.
According to Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014), such a ‘narrow’ view was at times also taken by lay people, in particular among those with certain characteristics such as emotional difficulties, low educational attainment or cultural beliefs that place trust in professional expertise and knowledge. Health professionals tended to expect that patients take increased responsibility to manage their own health, but this view was not necessarily shared by all service users. Importantly, lay views about self-management placed particular value on the quality of the relationship between the professional and the service user, seeing self-management as a collaborative partnership. But this understanding was less commonly expressed by providers. Overall, self-management appeared to form part of what Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014) described as “lay construction of illness narratives” (p. 15) that enabled people to make sense of and cope with their condition(s), and adapt to them in their everyday lives as a ‘social practice’, which involves the ability to mobilize social support from family and friends. These themes again tended to be less commonly reflected upon by health professionals.
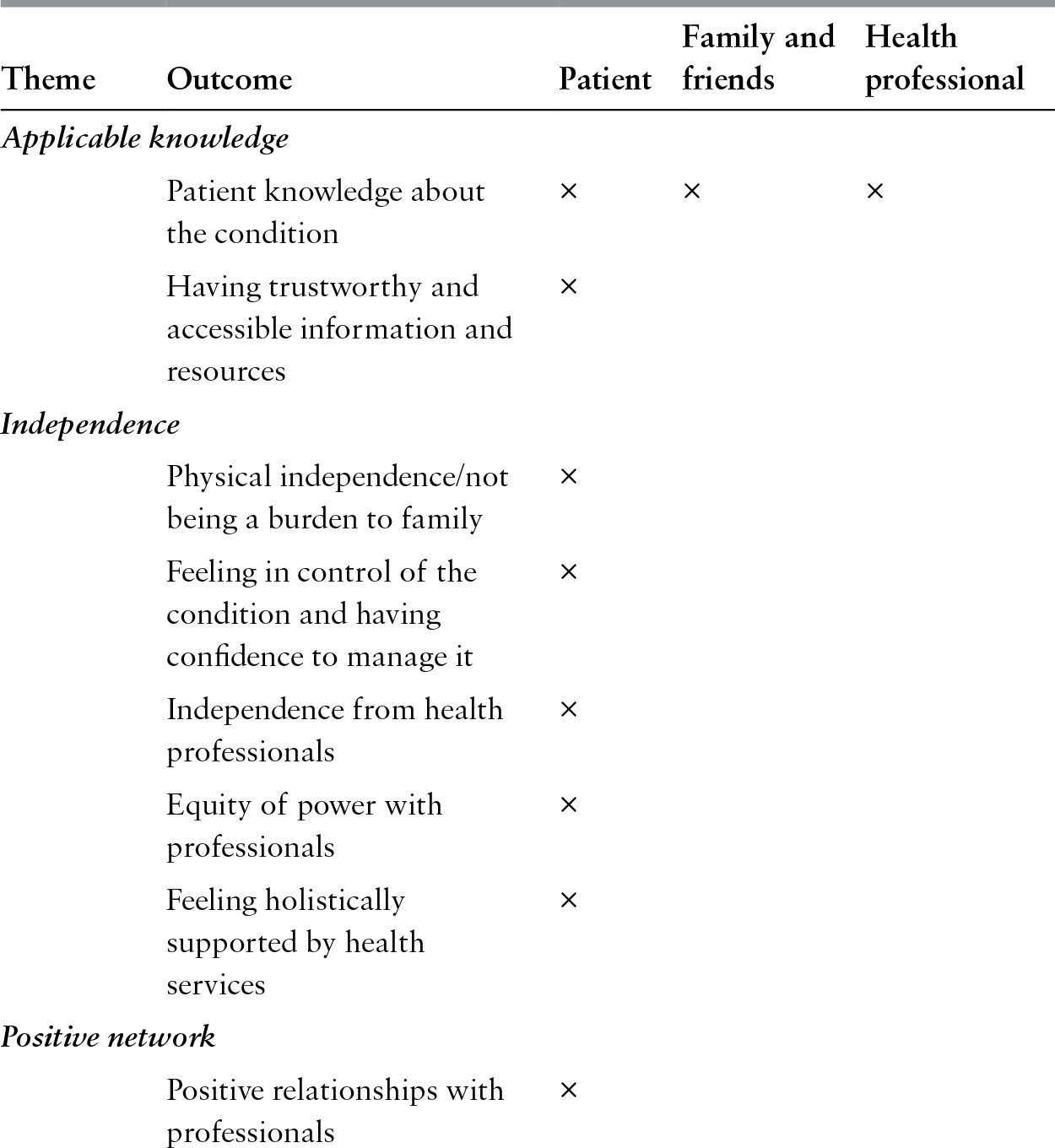
This apparent disjoint between service users’ and health professionals’ understandings of self-management is further illustrated by Reference BogerBoger et al. (2015), who synthesized the evidence of different stakeholders’ views on self-management outcomes, including patients, their families, health professionals, purchasers of services and policy-makers. Focusing on three exemplar conditions (diabetes, stroke, colorectal cancer), the review found that much of the evidence was from studies of the experience of self-management rather than actual views on desired outcomes. Importantly, several themes that were identified to be relevant by patients were not mentioned by health professionals, such as maintaining independence and a desire that the condition or illness should not define people’s lives (‘being me’) (Table 12.1).
Table 12.1 Self-management outcomes described as important by stakeholder group
Where there were overlaps, different stakeholder groups tended to conceptualize related outcomes in different ways. For example, while applicable knowledge was seen to be important, health professionals tended to interpret this outcome as knowledge about the disease process (‘knowing that’) while patients and their families focused on knowledge that was personally relevant and tailored to their specific situation (‘knowing how’; see Reference GreenhalghGreenhalgh et al. (2011)). Similarly, patients and professionals considered gaining self-management skills to be important, yet only health professionals identified motivation or goal-setting as core outcomes while patients emphasized managing emotions and stress (Table 12.1). Reflecting the findings by Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014), Reference BogerBoger et al. (2015) also highlighted the importance that patients attached to the quality of the relationship with the health professional (see Box 12.3), an issue that was not brought up by health professionals. Reference BogerBoger et al. (2015) were unable to identify evidence about how purchasers of services or policy-makers conceptualize self-management and desired outcomes, an issue also highlighted by Reference HarveyHarvey et al. (2015), and which we will return to later in this chapter.
Box 12.3 The value of different aspects of self-management support
Of course, identifying the range of outcomes different stakeholders view as relevant does not necessarily mean that all outcomes are valued as equally important. Reference BurtonBurton et al. (2017) demonstrated in a study of preferences of people with chronic pain or with breathlessness because of chronic respiratory disease that respondents consistently placed a high value on support services that take account of their personal situation and that were oriented to what matters to them for living well. Conversely, more personally relevant information was valued less highly while a friendly and communicative style was valued least. At the same time, respondents varied in the value they placed on different aspects, with a substantial minority rating the provision of personally relevant information highest, and these differences were not associated with broader social or demographic characteristics. Overall these findings suggest that a ‘one-size-fits-all’ approach to self-management is unlikely to meet people’s diverse needs, and strategies need to take account of this diversity.
As noted, differing interpretations of outcomes by different stakeholders likely reflect diversity in conceptualizations of self-management and self-management support, which further influence, or are influenced by, understandings of responsibility for self-management, along with what would be seen to qualify as ‘good’ self-management. For example, from a service perspective ‘goodness’ may be more closely linked to strict adherence to advice from health professionals, while from a user perspective it may mean adapting advice and modifying adherence in order to live well (Reference BogerBoger et al., 2015). Differing views on ‘goodness’ can create tensions between service users and health professionals, especially where user wants and preferences do not align with what the professional considers as the ‘right’ course of action (Reference CarrCarr et al., 2014), or where user choices are associated with increased costs to the system (Reference HarveyHarvey et al., 2015).
The notion of ‘responsibility’ in and for self-management was further explored by Reference Mudge, Kayes and McPhersonMudge, Kayes & McPherson (2016), who carried out a metasynthesis of 14 qualitative studies of clinicians’ (nurses, physicians, allied health professionals) views on their role in delivering self-management approaches. The theme of ‘control’ dominated reported perceptions: exercising authority over the patient (clinician control) (mainly) through education and instruction to help patients to control their condition (disease control) by adopting appropriate behaviours (patient control). This view concurs with what Reference MorganMorgan et al. (2016) described as a narrow approach to self-management support (see Box 12.2), which relies to a great extent on clinical markers to monitor progress; those not successfully managing their condition were often labelled as non-compliant (shifting responsibility to the patient). Reference Mudge, Kayes and McPhersonMudge, Kayes & McPherson (2016) highlighted that there appeared to be an (implicit) assumption that clinicians owned the control and would ‘grant’ it to patients to take on control themselves. At the same time, their review also showed that (some) clinicians recognized a paradigm shift away from the traditional expert-dominated, paternalistic relationship to one that values patient expertise and input, and that acknowledged patients’ lived experiences. Those experiencing the shift highlighted the challenges involved, such as sharing or ‘letting go’ of control. They also reiterated the tensions that are inherent in accepting the patients’ expertise as a legitimate input, and which might override the clinician’s perspective on a given issue and required professionals to reflect on their role as ‘experts’ (Reference CarrCarr et al., 2014).
Specifically focusing on patients’ accounts of formal and informal self-management support for type 2 diabetes, Reference FossFoss et al. (2016), based on a metasynthesis of the qualitative evidence (29 studies set in European countries), confirmed that, among people with diabetes, perceptions of self-management go beyond compliance and control. Indeed, self-management practices were seen to be the result of a range of interrelated factors that operate at micro and macro levels and “that exist not as part of the lives of patients but as actually founding or constituting their lives” (p. 681). Understandings of self-management centred around a sense of agency and identity and how environmental factors were connected to everyday lives and behaviours; a desire to achieve minimal disruption of everyday life; the significance and meaning of social networks both influencing and constituting self-management; the role of economic hardship in negotiating priorities in self-management; the challenges created by an emphasis on individual responsibility in encounters with the health service but also at the wider societal level as expressed by a need to ‘keep up appearances’, and feelings of guilt and shame when failing to comply with treatments or advice; and structural influences of the (primary) care system such as lack of adequate support structures including information, competencies and knowledge, alongside perceived lack of communication and collaboration, and of biopsychosocial approaches in practice.
The findings by Reference FossFoss et al. (2016) echo those by Reference BurtonBurton et al. (2017), Reference MorganMorgan et al. (2016) and Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014) in that the lay or service user perspectives on self-management and support go beyond those constructed in contemporary policy and practice. The authors note how their review “paints a picture of individuals struggling with social, emotional and economic challenges” (p. 681). They found that people would feel supported by the health service at times, but that this encounter was periodically experienced as ‘yet another demand in their lives’ and that personal circumstances could stand in the way of ‘doing the right thing’ (p. 681). Based on these observations, and in line with other accounts (Reference Entwistle, Cribb and OwensEntwistle, Cribb & Owens, 2016; Reference KendallKendall et al., 2011; Reference Mudge, Kayes and McPhersonMudge, Kayes & McPherson, 2016; Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt, 2014; Reference VassilevVassilev et al., 2011), the authors suggest that the contemporary conceptualization of self-management as an ‘individual ability’ misses the reality of patients’ experiences of and capacity for self-management that is shaped by their social and material resources and the local context within which they live. Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt (2014) further emphasized the need for self-management support strategies to be based on social models to address differences in lay expectations and abilities to take responsibility in terms of learning self-management skills and to tailor professional support accordingly. This suggests that self-management support efforts should be targeted at all levels, from the individual (micro) to the societal (macro) level in order to be effective (Reference Hinder and GreenhalghHinder & Greenhalgh, 2012; Reference RogersRogers et al., 2015).
There is also a need to address the broader societal understanding of chronic conditions and of presenting a ‘public story’ that can positively impact people’s help-seeking behaviour and public perceptions of need (Reference TaylorTaylor et al., 2014). Particular issues arise for those where there is little public understanding of the nature of the health problem and the potential for being stigmatized and seen as ‘half a person’ because of loss of capacity, the (apparent) failure to take responsibility, or being seen as posing a burden to society (Reference BratzkeBratzke et al., 2015; Reference RogersRogers et al., 2015; Reference VassilevVassilev et al., 2016). Reference RogersRogers et al. (2015) further highlighted the importance of creating supportive social and policy environments that help people to better self-manage. In the context of diabetes, they draw attention to the role of, for example, the media in reinforcing negative stereotypes in relation to individual responsibility for the development of diabetes through poor lifestyle choices, alongside wider food policies that may (implicitly) promote diabetogenic environments and the production of unhealthy foods. Context matters, however, with people in different countries experiencing different challenges, as shown in a comparative study of people with diabetes in Bulgaria and the UK (Reference VassilevVassilev et al., 2016). This demonstrated how respondents in Bulgaria faced actual lack of resources, access to good quality food and medicines to enable self-management of their condition, pointing to the need for policy solutions that take account of local context.
Moving forward
Reference MorganMorgan et al. (2016) proposed that self-management support should “enable people to live (and die) well with their long-term condition(s)” (p. 11), suggesting that approaches to self-management support that draw on concepts such as empowerment and involvement should prompt questions about the scope of what people are actually empowered to do. Living with long-term health problems challenges individuals on many levels, of which interacting with the health service is only one, if an important one (Reference MayMay et al., 2014). This chapter has explored some of the key issues pertaining to contemporary policy and practice around self-management and support and how existing approaches that focus on care coordination may fall short of taking account of the wider social context within which people live. There may be a risk that strategies and approaches continue to emphasize the ‘narrow’ focus as exemplified by a recent analysis by Reference JonkmanJonkman et al. (2016), who proposed a ‘new operational definition’ of self-management interventions, which stresses individual responsibility for management and behavioural change “in order to function optimally” (p. 34). Indeed, observations from the review of support efforts in Europe described above suggest a continued focus on medical and behavioural management (Reference ElissenElissen et al., 2013), whereas less emphasis appears to be placed on the wider social context within which people live.
This may, in part, reflect a wider political context that emphasizes individual responsibility over more collective and regulatory efforts, for example promoting behavioural change interventions over structural solutions to create the necessary physical and social infrastructure (for example, transport) (Reference RogersRogers et al., 2015). However, it also highlights the challenges involved in taking a comprehensive, system-wide approach in devising policies to address the rising burden of chronic disease more broadly, which requires the capacity for multi- and intersectoral collaboration that extends beyond the immediate health sector (Reference Richardson, Zaletel and NolteRichardson, Zaletel & Nolte, 2016) and the ability (and willingness) to confront stakeholders that prioritize the interests of business and industry that run counter to wider public health goals.
The chapter has explored the challenges facing service users and health care providers in conceptualizing and implementing relevant strategies. There is so far little robust evidence about how managers and policy-makers view self-management in terms of strategies and desired outcomes (Reference BogerBoger et al., 2015; Reference HarveyHarvey et al., 2015). Yet given their role in developing and funding services that support self-management, and in promoting a move of health systems towards supporting self-management more broadly, it will be important to better understand how their priorities map with the stakeholders they aim to support (Reference BogerBoger et al., 2015). There is a particular need to understand the aims and objectives policy-makers seek to achieve in pursuing self-management support strategies to help inform the nature and scope of relevant interventions and approaches and their likelihood of success. Reference KendallKendall et al. (2011), in a review of policy documents and interview data in Australia, noted that one conception of self-management saw it as a cost-cutting mechanism that ‘works’ through reducing risk behaviour and improving health and thus reduces the use of costly health services. Yet as we have seen, the available evidence that existing approaches to self-management support will indeed reduce utilization (and health care costs) has so far remained weak (Reference PanagiotiPanagioti et al., 2014). This highlights the need for a better understanding of the causal pathways by which such (intermediary) goals can be realistically achieved in practice.
We have also seen that different interpretations of self-management by different stakeholders may create tensions, such as between service users and health professionals in terms of judging the appropriateness of a particular course of self-management activity (Reference CarrCarr et al., 2014; Reference HarveyHarvey et al., 2015). There may also be tensions between service users and their families and wider social networks, which could constrain efforts to self-manage effectively (Reference FossFoss et al., 2016; Reference Sadler, Wolfe and McKevittSadler, Wolfe & McKevitt, 2014). Tensions may further arise within and between health professionals tasked with actively engaging patients in their own care although Reference Mudge, Kayes and McPhersonMudge, Kayes & McPherson (2016), in their analysis of clinicians’ views on their role in self-management, did not identify substantive evidence that there would be important differences in the clinicians’ views in this respect. Instead, what appeared to be more important was the challenges clinicians faced when actively incorporating self-management into their daily practice, requiring them to ‘let go’ of being the expert, ‘holding back’ and talking less and listening more.
Reference HarveyHarvey et al. (2015) suggested that there will likely be tensions between professionals and managers or decision-makers also. For example, as part of a wider move to evidence-based practice, there may be a requirement for standardization of care processes at the organizational level. Yet, as Reference TaylorTaylor et al. (2014) have shown, for self-management support to be effective, practitioners need to tailor their practice to individual service users’ needs and preferences, and this may run counter to standardized approaches. Challenges will also arise from the wider health care policy environment, for example as it relates to the provision of sustainable funding for self-management support interventions to enable firm embedding of relevant programmes in daily practice. This can be especially challenging in resource-constrained settings (Reference RogersRogers et al., 2015). But even where the wider policy context is supportive in principle, tensions may arise where national or macro-level priorities are not aligned and other (potentially competing) goals dominate service delivery priorities locally. This can be illustrated by evidence from England, which found that implementation of comprehensive self-management support strategies at local level was hampered by a continued emphasis on a biomedical model of chronic disease management, with measurement and payment linked to biomedical outcomes, most prominently within the system-wide pay-for-performance scheme in primary care (Reference KennedyKennedy et al., 2014; Reference ReidyReidy et al., 2016) (see also Box 12.4). Reinforcement of a focus on the biomedical model was also noted in other system contexts where pharmaceutical companies have taken a greater role in the funding and delivery of self-management support programmes in the absence of national funding sources (Reference RogersRogers et al., 2015).
Box 12.4 Implementing self-management support at the local level in the English NHS
In England, Clinical Commissioning Groups (CCGs; the purchasers of most health care in the English NHS) are encouraged to use a ‘House of Care’ model to service provision, which focuses on the integration of service users’ experiences and resources (NHS Reference EnglandEngland, 2017). Building on experiences in the UK and the Chronic Care Model developed by Wagner and colleagues in the United States, it considers four core interdependent components to realize person-centred coordinated care (Reference Coulter, Roberts and DixonCoulter, Roberts & Dixon, 2013). These are: engaged, informed individuals and carers (left wall of the house); health and care professionals committed to partnership working (right wall); commissioning including ‘more than medicine’ (floor); and organizational and supporting processes (roof). Self-management support is seen to be among the core strategies commissioners are asked to consider for supporting the delivery of person-centred care (Coalition for Collaborative Care and NHS England, 2016).
Reference ReidyReidy et al. (2016) examined the way CCGs consider and conceptualize self-management support and the extent to which this was reflected in the strategic planning and commissioning of services. Drawing on an analysis of planning documents of nine CCGs and interviews, the authors found that commissioners’ conceptualization of self-management support tended to reflect the national agenda or ‘official terminology’, which focused on support strategies as a means to reduce service utilization against the need for cost containment. While self-management support was generally seen to form an important component of culture change in service delivery, the operationalization of relevant strategies in practice was seen to be challenging unless guided by a top-down initiative. There was a reported lack of capacity to engage with the public for developing and implementing self-management support strategies, where these were not linked to traditional, nationally driven outcome measures and payments relating to biomedical outcomes.
Conclusions
The evidence presented in this chapter highlights that there is still a long way to go for health systems that seek to strengthen self-management support as part of a wider strategy of moving towards more coordinated, person-centred health systems. We have seen that any such strategy needs to consider the wider context within which people live and efforts should be targeted at the micro, that is the individual level, the organizational level and the macro or system level. Strategies also need to go beyond the immediate health care context in order to take full account of the broader influences that impact self-management activities at the individual level, of which the encounter with service providers is only one, albeit key, factor. Rather than supporting people to manage their condition(s) well in biomedical or disease-control terms (narrow approaches), the emphasis should be on supporting people to manage well (or live well) with their condition(s) (broad approaches). There are implications for the training of health and care professionals and how this needs to be adapted to enable providers engaging in a true partnership with the individual service user that provides the support appropriate to the individual’s preferences and needs. Managers need to consider approaches of how to best support their staff in providing self-management support, which will involve making relevant activities a priority, and which in turn requires the ability of organizations to do so against the background of demands placed upon them by the wider system context. This also highlights the need for the wider policy framework to be alert to the potential tensions and unintended consequences of policies that are not consistent, and to create a policy environment that provides the means for those who are asked to implement change to acquire the actual capacity and competence to do so, which will be critical for success.