Neurovascular compression syndrome (NVCS) is an abnormal intersection between a cranial nerve and blood vessel. Reference Haller, Etienne, Ko vari, Varoquaux, Urbach and Becker1 NVCS can be asymptomatic or symptomatic depending on cranial nerve involvement. Examples include trigeminal neuralgia, hemifacial spasm, vestibular paroxysmia, and glossopharyngeal neuralgia. Reference Haller, Etienne, Ko vari, Varoquaux, Urbach and Becker1 This series details the presentations of uncommon NVCS, specifically involving the anterior visual pathway. The optic nerve carries sensory information from the ganglion cells of the retina along the optic chiasm and tract before synapsing in the lateral geniculate nucleus. An artery with normal caliber or dolichoectasia (artery with dilatation or tortuous component) can cause a compression. Although often incidentally found, NVCS can lead to symptomatic vision loss in various patterns. Diagnosis is based on clinical and radiological evaluation. For any suspected nerve compression syndrome, magnetic resonance imaging (MRI) of the brain is diagnostic. Reference Baldauf, Rosenstengel and Schroeder2 Thorough investigation is required to rule out other causes of neurological deficits. The purpose of this case series is to study the effect of neurovascular compression syndrome involving the anterior visual pathway.
Individuals with NVCS involving the anterior visual pathway on diagnostic imaging were identified by one author (ANES) in their outpatient neuro-ophthalmology clinic between 2014 and 2020. Patients were included if a NVC was identified on imaging. Patients referred for atypical glaucoma were also followed by a glaucoma specialist. This case series is a retrospective analysis of their charts, including symptoms, visual acuities, relative afferent pupillary defects (RAPD); optic disk appearances including neuroretinal rims and cup-to-disk ratios, optical coherence tomography (OCT) images of the retinal nerve fiber layer (RNFL), Humphrey visual fields (HVF), and diagnostic images (MRI) if available. OCT images were collected in a subset of cases, and most patients were monitored with serial HVFs. Ganglion cell complex analysis was completed in some patients in the last three years.
Twenty-nine patients (17 male, 12 female) with a mean age of 65.8 (standard deviation of 13.5) demonstrated various combinations of neurovascular compression syndrome (Table 1). Seven patients had multiple neurovascular compressions (24.1%) creating a total of 36 compressions (cases 1, 3, 9, 13, 15, 24, and 27). Both anterior and posterior circulations were involved, as well as all components of the anterior visual pathway. Specific neurovascular compressions are detailed in Table 1, (see column 4 for vessel and column 5 for nerve involved). Dolichoectasia was seen in five of the 29 patients (17.2%).
Table 1: Summary of patient demographics and clinical information
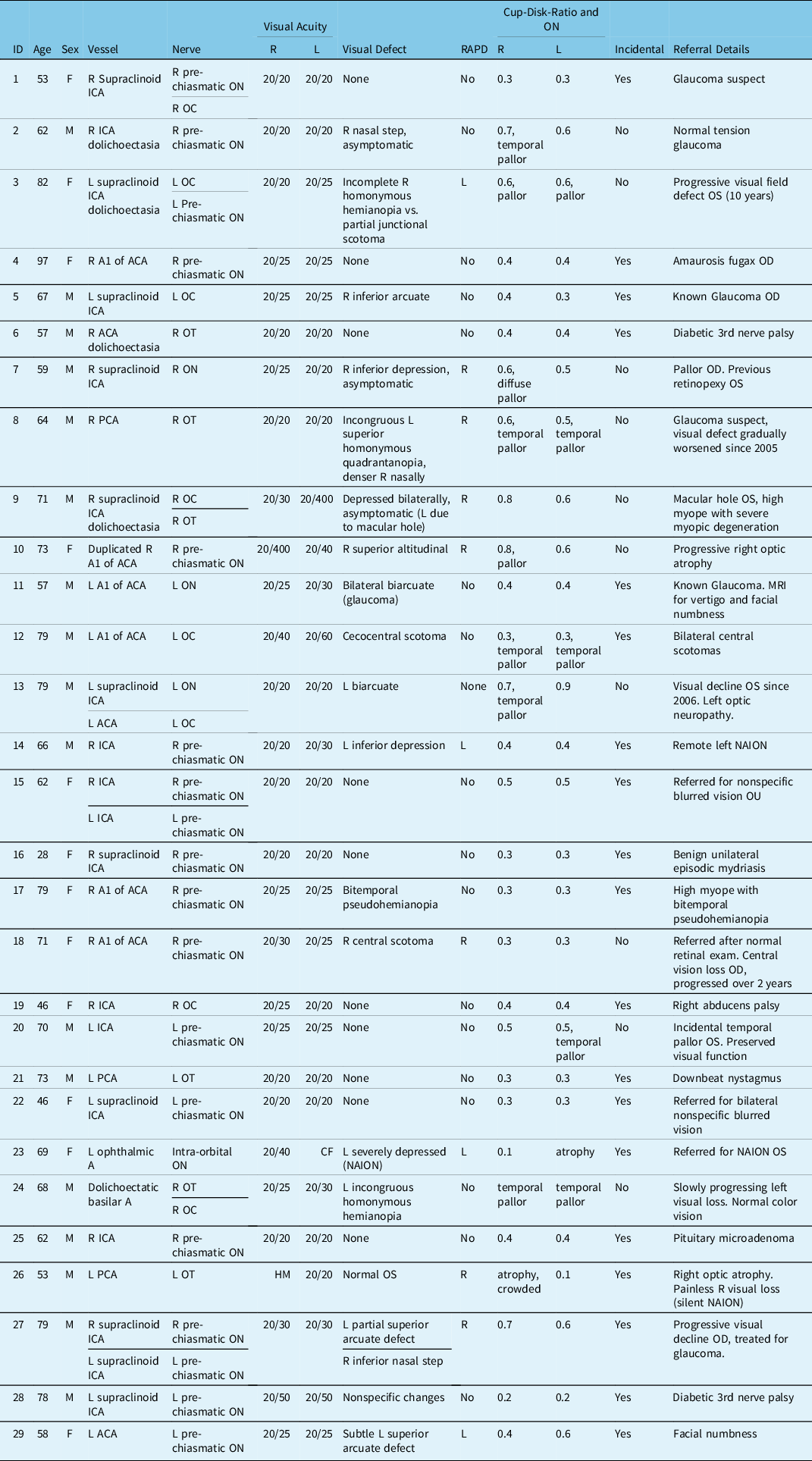
A = Artery; ACA = Anterior cerebral artery; CDR = Cup-to-disk ratio; HVF = Humphrey visual field; ICA = Internal cerebral artery; L = Left; LCA = Long circumferential artery; N = Nerve; NAION = Non-arteritic anterior ischemic optic neuropathy; NVC = Neurovascular conflict; OC = Optic chiasm; OD = Right eye; ON = Optic nerve; OS = Left eye; OT = Optic tract; PCA = Posterior cerebral artery; R = Right; RAPD = Relative afferent pupillary defect; VA = Visual acuity.
The most common NVCS (5/36, 13.8%) included the pre-chiasmatic optic nerve and supraclinoid internal cerebral artery. NVCS was an incidental finding in 19 patients (65.5%). These patients were imaged for other purposes such as oculomotor nerve palsy, nonarteritic anterior ischemic optic neuropathy, and downbeat nystagmus. They had no RAPD, optic disk changes, or visual defects secondary to the NVCS. 10/29 cases (34.5%) presented with visual field defects in variable patterns which localized to the NVCS site (cases 2, 3, 7–10, 13, 18, 20, and 24). OCTs were collected when available (72.4%, 21/29) (Table 2). When OCTs were obtained, RNFL atrophy was evident in many symptomatic cases of NVCS. Visual defects varied based on the site of the compression, which included retinal nerve fiber layer defects (such as nasal step, arcuate defects, and central scotomas), diffuse loss, incongruous homonymous hemianopia, and homonymous quadrantanopia. Eleven (37.9%) patients had normal visual fields. 31.0% (9/29) of patients (cases 1–3, 5, 8, 10, 11, 13, and 27) were referred to rule out non-glaucomatous pathology by glaucoma specialists. 55.5% (5/9) of these (cases 2, 3, 8, 10, and 13) patients were found to have visual field defects matching the NVCS, rather than normal tension glaucoma (NTG).
Table 2: Summary of most recent available OCT results
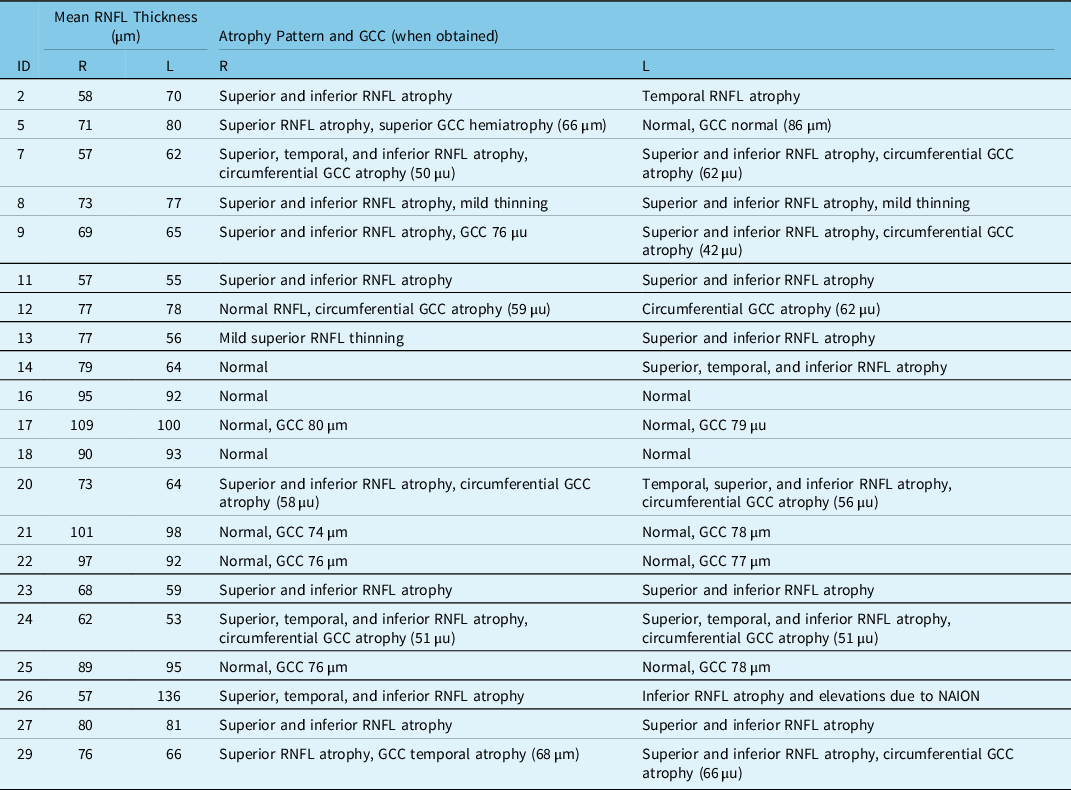
GCC = Ganglion cell complex; L = Left; R = Right; RNFL = Retinal nerve fiber layer.
96.5% (28/29) of patients remained stable from the visual perspective during follow-up visits. Figure 1 details HVFs for patients 8, 13, and 24. Figure 2 includes details on T2-weighted MRI images for these patients. Two among the five patients with optic tract compression showed matching homonymous visual field defects (cases 9 and 24). Case 24 presented with significant compression on optic tract and optic chiasm by dolichoectatic basilar artery and showed progression of homonymous quadrantanopia to incongruous homonymous hemianopia. All other patients have remained stable without worsening of vision or visual fields.
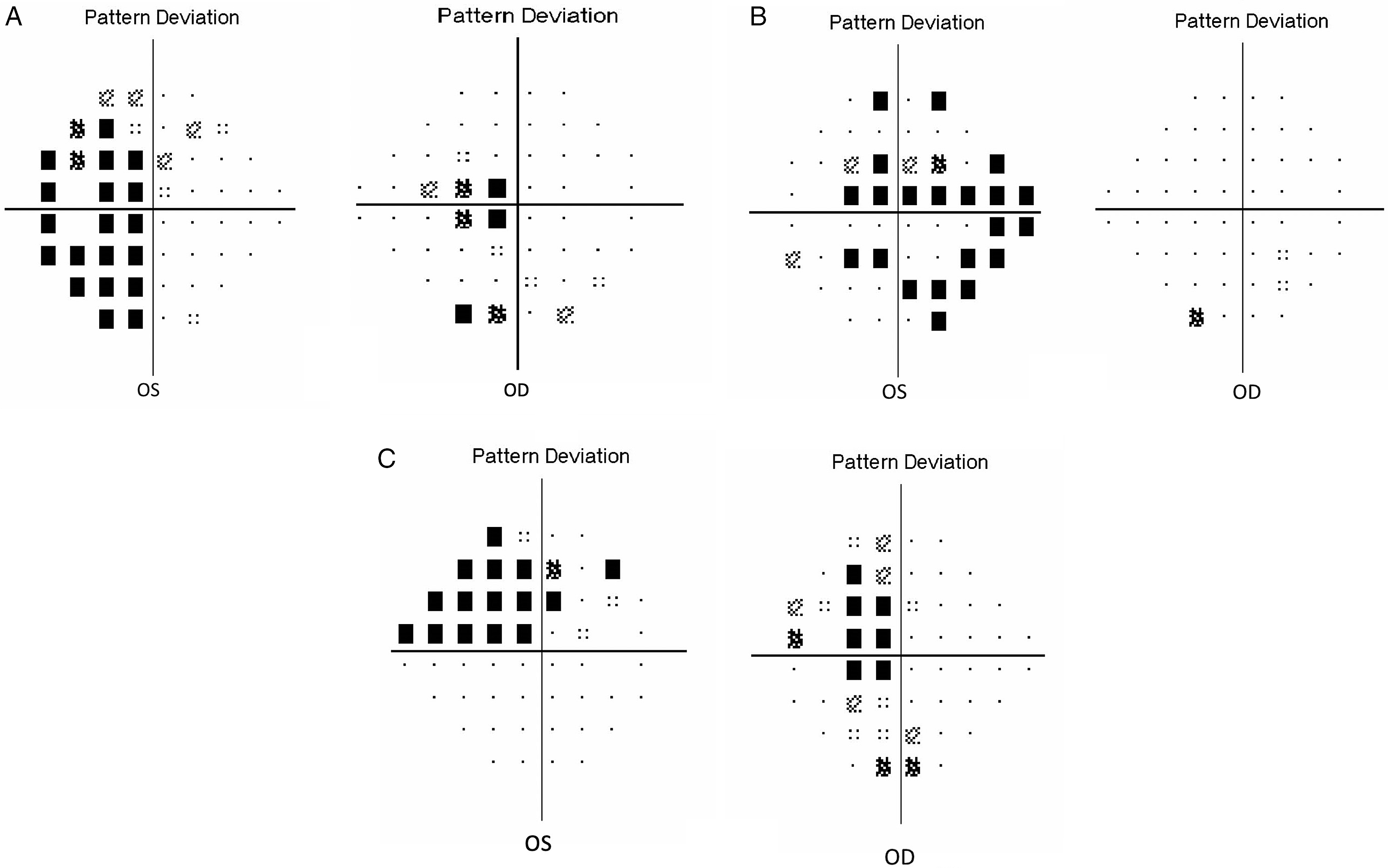
Figure 1: 24–2 SITA Humphrey visual fields. (A) Patient # 24. Incongruous left homonymous hemianopia. Neurovascular compression: Right optic tract and dolichoectatic basilar artery. (B) Patient # 13. Left biarcuate defect. Neurovascular compression: Left pre-chiasmatic optic nerve and left ACA. (C) Patient #8. Incongruous left homonymous quadrantanopia. Neurovascular compression: Right optic tract and right ACA.
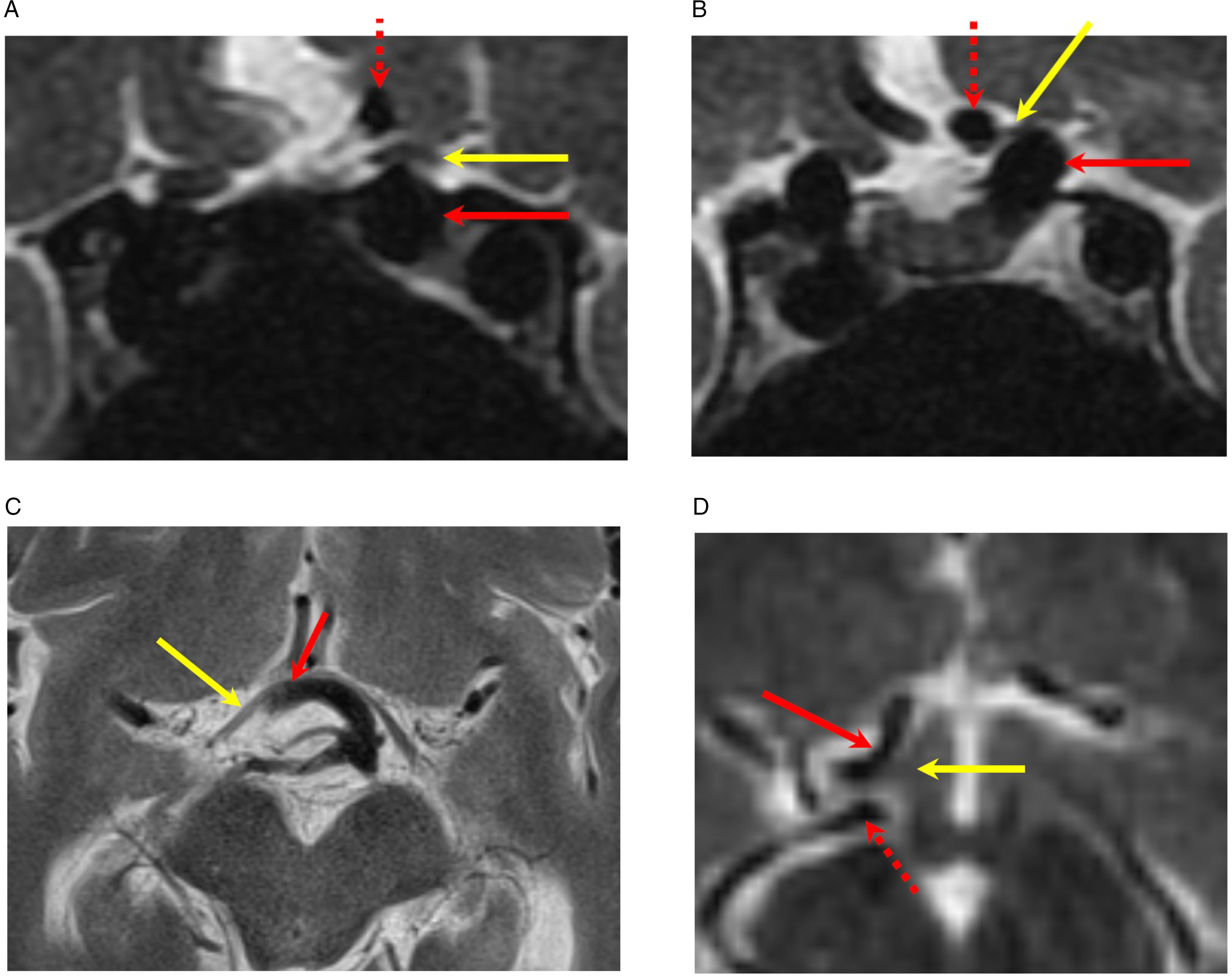
Figure 2: MR images. (A and B) Coronal T2-weighted images demonstrate compression of pre-chiasmatic left optic nerve (yellow arrow) by distal cavernous and paraclinoid left internal carotid artery (solid red arrow). The dashed red arrow is the left anterior cerebral artery (patient 13). (C) Axial T2-weighted image demonstrates compression of the right optic tract (yellow arrow) by the dolichoectatic basilar artery (red arrow) (patient 24). (D) Axial T2-weighted image demonstrates compression of the right optic tract (yellow arrow) by the right anterior cerebral artery (solid red arrow). The dashed red arrow is the right posterior cerebral artery. (Patient 8).
This case series is a clinical summary of 29 patients with NVCS involving the anterior visual pathway. Although uncommon, NVCS can be asymptomatic, and discovered incidentally on routine imaging, or cause progressive visual loss evident on HVF. Reference Jacobson3,Reference Fargen and Blackburn4 Because of the nature of visual defects and the number of patients referred for glaucoma, it is important to consider NVCS in the differential diagnosis of NTG, Reference Jacobson3 While NTG results in four characteristic patterns, defects in NVCS have not been well characterized. Reference Kitazawa and Yamamoto5 This is particularly important when the field changes are progressive despite adequate diurnal intraocular pressure control, or when the changes are asymmetric in the setting of similar bilateral intraocular pressures. Visual loss occurs from direct compression by the vessel, although vascular pulsations have also been hypothesized to be an etiological factor. Reference Fargen and Blackburn4,Reference McLaughlin and Bojanowski6
Decompression surgery is usually reserved for patients with progressive visual loss. There have been a few isolated case reports and case series with successful decompression surgeries and visual improvement. Reference Fargen and Blackburn4,Reference McLaughlin and Bojanowski6–Reference Nonaka, Uede, Ohtaki, Tanabe and Hashi9 but there are no randomized studies given the rarity of this condition. Currently, the role of surgical decompression is not as well established as in other types of NVCS such as trigeminal neuralgia. Failure of early diagnosis has been postulated for unsatisfactory postoperative visual outcome. Reference Nonaka, Uede, Ohtaki, Tanabe and Hashi9
A case series published by Jacobson (1994) discussed the clinical features of 18 patients with optic nerve compression by the supraclinoid carotid artery. Reference Jacobson3 All patients had optic neuropathy (6 bilateral, 12 unilateral). Similar to our cases, they reported a variety of visual field defects with abnormal disks (pallor, atrophy, and cupping). In a previous case series of 10 cases, only one patient had progressive visual loss that required decompression. Reference Purvin, Kawasaki and Zeldes10 Compared to these previous reports, ours is the largest cohort studied.
In patients with trigeminal neuralgia who have similar pathomechanism resulting in compressive neuropathy, it has been noted that a neurovascular contact alone is not enough for diagnosis of NVCS. Reference Maurya, Sreedhar, Khera, Bhatia and Sharma11 It is important to radiologically identify nerve thinning, arterial imprint or grooving, or distortion of the course of the nerve, which may lead to the symptomatic presentations. Reference Maurya, Sreedhar, Khera, Bhatia and Sharma11 Arterial imprint or grooving is focal thinning of the nerve at the neurovascular compression site. Intraoperative histopathological study in patients with trigeminal neuralgia secondary to NVCS has shown demyelination and axonal loss. Reference Devor, Govrin-Lippmann and Rappaport12 A combination of high-resolution T2-weighted images, MR angiogram, and volumetric gadolinium-based contrast-enhanced T1-weighted image is recommended for detection of NVCS. Reference Haller, Etienne, Ko vari, Varoquaux, Urbach and Becker1 In terms of NVCS of optic pathways, the culprit arteries are large enough that they can be easily visualized as vascular flow voids on high-resolution T2-weighted images, and therefore, there may not be a need for contrast-enhanced MR angiogram in these cases.
Although mostly asymptomatic, NVCS can cause compressive optic neuropathy leading to significant visual disturbances. The majority NVCS is found incidentally and do not progress to this point. Decompression has been successful in isolated cases of progressive visual loss; however, there are no controlled studies. Patients are diagnosed using MRI imaging. It is important to include neurovascular compression syndrome in the differential diagnosis for normal tension glaucoma, especially with progressive visual field loss despite treatment. Patients with progressive visual field loss may require decompression surgery.
Disclosures
MJG: None. PJM: None. LC: None. CB: Leadership or Fiduciary Role: Glaucoma research society of Canada, and University of Toronto Medical Alumni Association; stock or stock options: Premark, Allysta. ANES: None.
Statement of Authorship
MJG: conceptualization and methodology, data curation and analysis, visualization, and writing (initial draft); PJM: conceptualization and methodology, visualization, and writing (review and editing); LC: conceptualization and methodology, visualization, and writing (review and editing); CB: conceptualization and methodology, visualization, and writing (review and editing); ANES: conceptualization and methodology, resources, data curation and analysis, writing (review and editing), and supervision.






