Mental health services in the UK continue to develop. The pace and direction of recent changes has been heavily influenced by the publication of the NHS Plan (Department of Health, 2000). New services such as crisis resolution teams and assertive outreach teams are now part of the landscape of psychiatric services. The efficacy of these services has been demonstrated in Canada, the USA and Australia (Reference Joy, Adams and RiceJoy et al, 1998), and they have been shown to be as safe as standard hospital care in terms of suicide rates. However, scepticism has remained that the same would apply in the UK. Some of this scepticism centred on the use of hospital-based care as the comparator in trials, rather than standard community care such as provided by community mental health teams.
The NHS Plan states that crisis teams should produce a ‘30% reduction of pressure’ on acute in-patient services. Presumably this was to be achieved by reducing the rate and length of admissions. Certainly some of the early studies suggested crisis resolution teams could do both (Reference HoultHoult, 1986; Reference Dean, Phillips and GaddDean et al, 1993; Reference Marks, Connolly and MuijenMarks et al, 1994). A recent study in the UK has demonstrated that 24 h crisis teams focusing on home treatment can reduce admissions (Reference Johnson, Nolan and PillingJohnson et al, 2005). However, this mainly applied to patients with less-severe illness and not to those detained involuntarily (who were less likely to be included in the study). Data from Hospital Episode Statistics (Information Centre, 2006) show that those detained have longer lengths of stay. In addition, there are very limited data on the impact of these service developments on detentions under the Mental Health Act 1983.
A crisis service was established in Newcastle and North Tyneside in 2000. This operates 24 h per day, 7 days a week and provides assessment of psychiatric emergencies, home-based treatment as an alternative to hospital admission and gate-keeping of psychiatric beds. The model used is adapted from that described by Hoult (Reference Hoult1986). The assertive outreach service was established in the same year and covers the same population. The service operates extended hours, 09.00 h to 22.00 h Monday to Friday and 09.00 h to 22.00 h at weekends. A service is provided to patients who have severe psychotic illnesses and are difficult to engage, and have often had repeated admissions to hospital, frequently under compulsion. The model employed is that of the assertive community treatment services described by Stein & Test (Reference Stein and Test1980).
The aim of this study was to measure the impact of introducing a crisis team and an assertive outreach team in 2000, primarily to measure changes to the admission rate, diagnosis and length of stay of in-patients. The secondary aim was to measure changes to the numbers of involuntary admissions and the number of suicides in the population. Services that were not directly affected by redesign were used as a comparison group.
Method
Psychiatric services in Newcastle and North Tyneside formed the basis of this study. The total population is 450 000. Data were collected on psychiatric admissions from 1999 to 2004 to all acute adult psychiatric wards. In 1999 there were eight acute adult wards plus a pre-discharge ward. Routinely collected admission data from the hospital information technology department were used.
We decided to investigate the same 3-month period (1 April to 30 June) in each of the 5 years. A 3-month time frame was chosen to make the study more feasible. We accessed the data after at least 1 year had passed, thus allowing for the majority (99%) of admissions to have been completed. Admissions to three mental health of older adult wards were used as a comparison group. Data on diagnosis were collected from the same hospital system, which uses clinical coding forms to obtain primary and secondary diagnosis from the ward staff. These record and code diagnosis using ICD–10.
Data on suicides across the age span were obtained from the Newcastle Primary Care Trust and North Tyneside Primary Care Trust. These used data from the Office for National Statistics Public Health Mortality Files, ‘ mortality from intentional self-harm and injury undetermined whether accidentally or purposely inflicted (ICD–10 X60–X84, Y10–Y34 excluding Y33.9 equivalent to ICD–9 E950–E959 and E980–E989 excluding E988.8)’.
Data on involuntary admissions were collected from the local Mental Health Act Office. The total number of detentions under sections 2, 3, 5(2) and 5(4) on acute adult wards was collected for the years 1999–2004. Detentions to all other wards were used as a comparison group (elderly, rehabilitation, forensic, adolescent, neuropsychiatry, etc.). No details about individual patients were collected in relation to the Mental Health Act 1983.
Length of stay was calculated by measuring number of bed days of discharged patients. However, in less than 1% of cases the admission was ongoing at the time of data collection. Most of these admissions were longer than a year and for these patients the most up-to-date length of stay was used. The distribution of length of stay to acute adult wards showed an exponential reduction; hence the median was used as a measure of central tendency. The mean was used to calculate bed use as follows:
The study was registered with the Clinical Governance Department of the Newcastle, North Tyneside and Northumberland Mental Health NHS Trust as a quality improvement study and approval was obtained from the Caldicott Guardian. Data were analysed using SPSS version 10 for Windows.
Results
The numbers of admissions to the acute adult wards for the 3-month period in the years 1999-2004 were 330, 319, 254, 225, 206 and 183 respectively. This represents a 45% reduction. Similarly the mean weekly admission rate fell from 24.5 (s.d.=4.0) in 2000 to 14.1 (s.d.=3.7) in 2004 (ANOVA, F=10.1, d.f.=4, P<0.0005). The number of admissions to the three wards for the elderly and the mean weekly admission rate did not change significantly (ANOVA, F=0.77, d.f.=4, P=0.55).
In 1999 bed occupancy was routinely over 100% and there were overspill acute adult admissions to private psychiatric wards and other NHS psychiatric units. However, following the changes in service delivery in 2000 the bed occupancy fell below 100% for the first time in many years. As a consequence a pre-discharge ward was closed in 2002 and one or two beds were closed on several of the acute adult wards. Thus the total number of beds was reduced by 30 (20%), from 149 in April 1999 to 119 in June 2004.
Data on length of stay are available from the year 2000. This shows that whereas the admission rate fell by 42% on acute adult wards between 2000 and 2004, the occupied bed days fell by only 22% (see Table 1). This was because the length of stay increased (median by 61% and mean by 35%). The median steadily increased from 15.5 days in 2000 to 25 days in 2004 (Kruskal—Wallis test, χ2=14.6, P=0.005). The reason for this increase was that the greatest reduction was seen in short admissions. Admissions lasting a week or less were reduced by 64% (ANOVA, F=8.7, d.f.=4, P<0.0005), those lasting between a week and a month fell by 45% (ANOVA, F=5.37, d.f.=4, P=0.001) and those longer than a month fell by 21% (ANOVA, F=0.77, d.f.=4, P=0.55).
Table 1. Number of admissions, mean length of stay and occupied bed days following reorganisation of adult mental health services for 2000–2004
| 2000 | 2001 | 2002 | 2003 | 2004 | |
|---|---|---|---|---|---|
| Male | |||||
| Admissions, n | 160 | 132 | 126 | 103 | 101 |
| Length of stay, mean | 37.5 | 46.9 | 39.0 | 57.0 | 59.1 |
| Bed days | 5995 | 6190 | 4914 | 5871 | 5969 |
| Female | |||||
| Admissions, n | 154 | 117 | 98 | 94 | 80 |
| Length of stay, mean | 40.3 | 48.0 | 46.4 | 38.4 | 44.3 |
| Bed days | 6188 | 5613 | 4539 | 3703 | 3551 |
| All | |||||
| Admissions, n | 314 | 249 | 224 | 197 | 181 |
| Length of stay, mean | 38.8 | 47.4 | 42.2 | 48.6 | 52.6 |
| Bed days | 12183 | 11803 | 9453 | 9574 | 9520 |
Overall there was a modest and non-significant change in the number of longer-stay patients on the wards. The numbers of patients admitted in the 3-month period in 2000–2004, whose admissions were longer than 90 days were 32, 32, 29, 26 and 26 respectively. For male patients the numbers were 13, 16, 13, 17 and 17. However, there was a steady and sustained fall in the number of long-stay female patients: 19, 16, 16, 9 and 9.
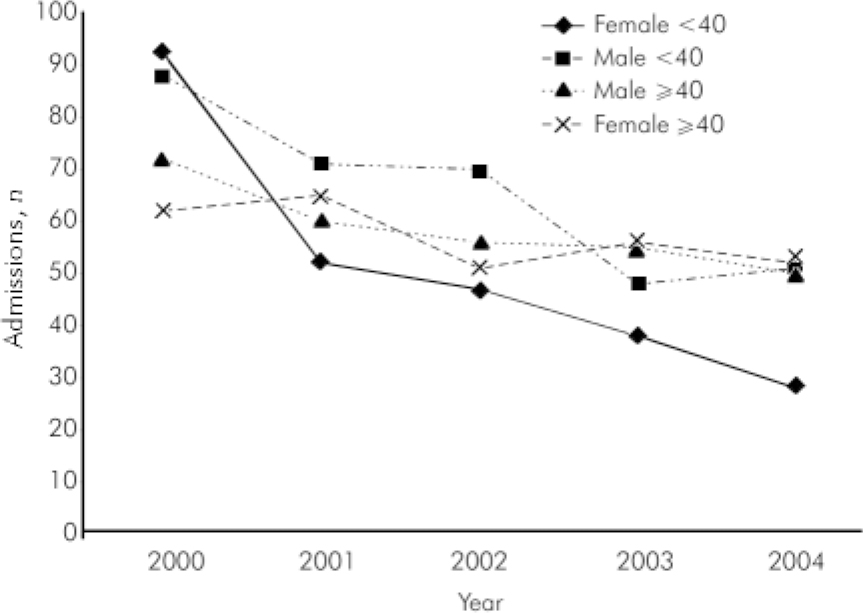
Fig. 1. Reduction in psychiatric admissions to acute adult wards from 2000 to 2004 according to age and gender.
Total occupied bed days fell by 22% from 12183 in 2000 to 9520 in 2004 for admissions during the 3-month period. However, this was only seen among female patients where occupied bed days fell from 6188 to 3551, a reduction of 43%. Surprisingly the occupied bed days remained roughly the same among male patients, 5995 in 2000 and 5969 in 2004. The reason for this was that male patients had a smaller fall in admissions (37%) but a large increase in the mean length of stay (58%), whereas female patients had a larger fall in admissions (48%) and virtually no change in length of stay.
The mean age of in-patients was 40.2 (s.d.=13) years. This increased from 38 years in 2000 to 42 years in 2004 (ANOVA, F=3.17, d.f.=3, P=0.013). The reason for the increase in age is shown in Fig. 1. There was a greater reduction in admissions of younger adults. This was most marked in women where there was a 70% reduction in those under 40 years. As a result the mean age of female patients increased from 37.6 years in 2000 to 44.2 years in 2004.
The completeness of information regarding diagnosis changed during the study period: in 2000 80% of admissions had a diagnosis recorded; by 2004 the figure was 45%. The data that we do have suggest that there was a reduction in admissions in all diagnostic categories, but the greatest reduction was in non-psychotic disorders. Consequently the proportion of admissions with psychotic disorders (schizophrenia, schizoaffective disorder, delusional disorder, bipolar affective disorder and psychotic depression) increased from 44% in 2000 to 60% in 2004 (χ2=16.3, d.f.=4, P=0.003). The length of stay remained constant over time within the psychotic/non-psychotic categories, with admissions for psychotic disorders being significantly longer than admissions for other diagnostic categories (median 27 v. 12 days, Mann–Whitney U-Test, Z=8.35, P<0.0005) (see Table 2).
Table 2. Diagnostic mix of in-patients following the reorganisation of an adult mental health service and corresponding median lengths of stay.
| In-patients, % | Median length of stay, days | ||||||
|---|---|---|---|---|---|---|---|
| Diagnosis (ICD—10) | 2000 | 2001 | 2002 | 2003 | 2004 | 2000-2004 | National data1 |
| Organic disorders (F 00-09) | 1 | 1 | 3 | 1 | 3 | 34 | 15 |
| Drug and alcohol disorders (F 10-19) | 10 | 9 | 13 | 8 | 7 | 9 | 10 |
| Schizophrenia and other psychotic disorders (F 20-29) | 29 | 35 | 33 | 38 | 39 | 28 | 28 |
| Mania and bipolar affective disorder (F 30-31) | 13 | 14 | 17 | 22 | 20 | 26 | 27 |
| Depression and other affective disorders (F 32-39) | 22 | 17 | 24 | 19 | 19 | 18 | 14 |
| Anxiety disorders and behavioural disorders (F 40-59) | 9 | 8 | 3 | 6 | 8 | 14 | |
| Personality disorders (F 60-69) | 11 | 13 | 9 | 7 | 7 | 9 | 10 |
| Other | 7 | 1 | 4 | 5 | 1 | 8 | |
The yearly number of suicides between 1999 and 2004 were 65, 51, 53, 63, 50 and 61 respectively. The majority of those dying by suicide were aged between 15 and 64 years (88% in 1999, 84% in 2004) and the male/female ratio was 5:1. Figure 2 shows the number of those dying by suicide aged 15–64 years and demonstrates that this remained stable in all groups, including younger, female adults (the group with the 70% reduction in admissions).
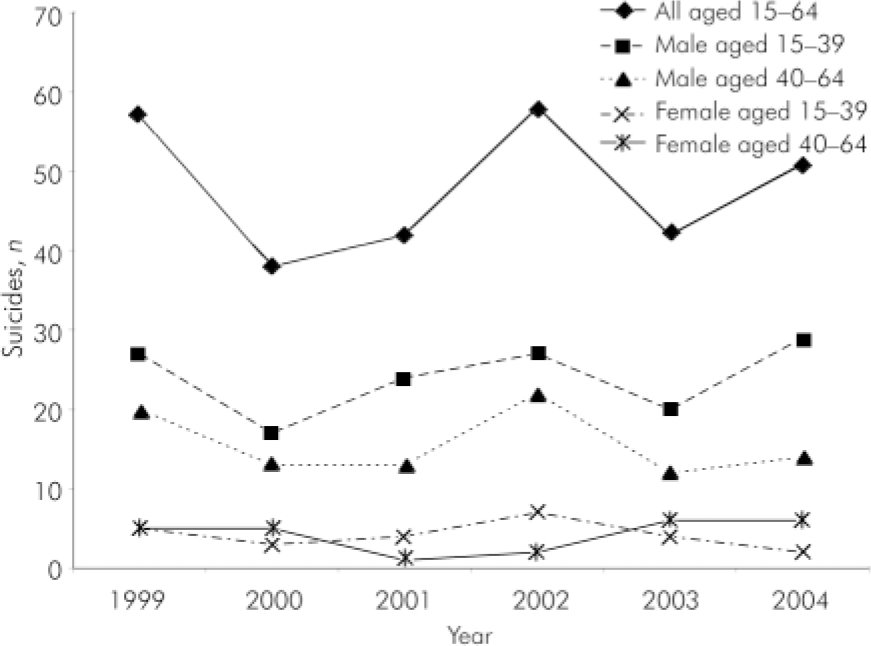
Fig. 2. Those dying by suicide aged 15–64 years in Newcastle and North Tyneside between 1999 and 2000.
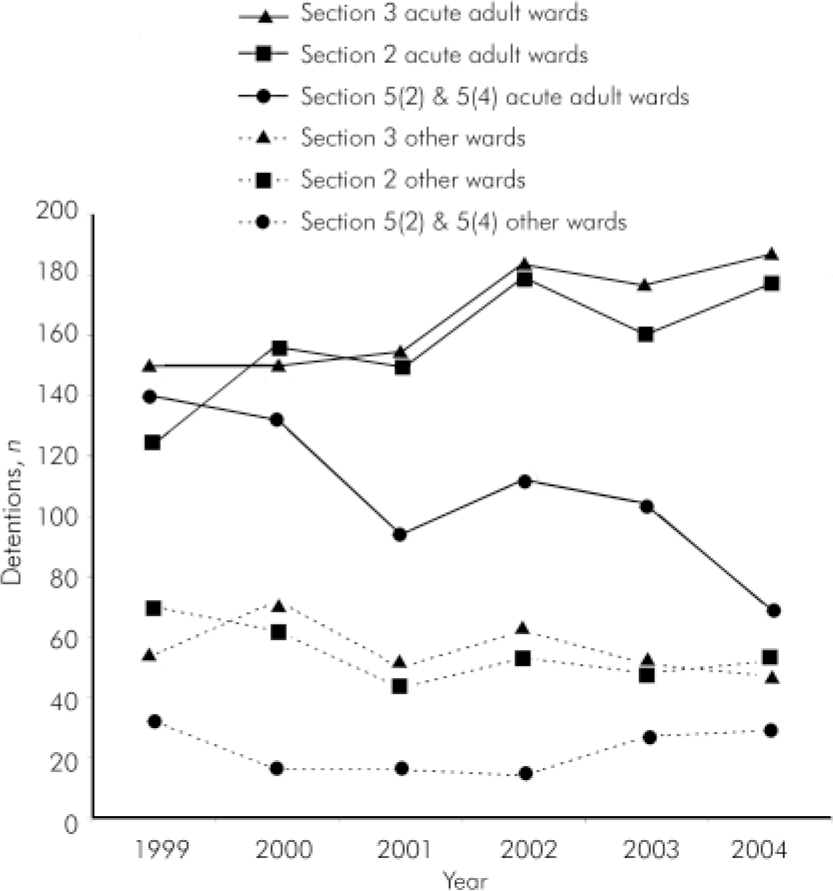
Fig. 3. Detentions under sections 2, 3, 5(2) and 5(4) in Newcastle and North Tyneside between 1999 and 2004. Detentions on acute adult wards are compared with all other wards.
Significant changes in the pattern of detentions under the Mental Health Act 1983 were evident (see Fig. 3). Detentions under section 2 increased 43% between 1999 and 2004 on acute adult wards. This was a significant change compared with similar detentions on other wards (χ2=14.69, d.f.=5, P=0.01). The increase in detentions under section 3 occurred later and was more modest, a 25% increase (χ2=11.64, d.f.=5, P=0.04). In contrast, there was a 46% fall in the use of section 5(2) and a 64% fall in section 5(4) on acute adult wards (χ2=19.63, d.f.=5, P=0.001).
There was a correlation between the falling number of admissions in the 3-month period of each year and the annual number of detentions under the Mental Health Act 1983. The correlation was negative for detentions under section 2 (r=–0.75, P=0.09, n=6) and section 3 (r=–0.88, P=0.02, n=6); positive for detentions under section 5 (2) (r=+0.89, P=0.02, n=6) and section 5 (4) (r=+0.77, P=0.07, n=6).
Discussion
This study investigates the impact of reorganising adult mental health services. The main part of this reorganisation was the introduction of a crisis resolution home treatment service and an assertive outreach service in 2000. The main findings are that admissions were reduced by approximately 45%, bed occupancy fell by 22%, the pattern of detentions under the Mental Health Act 1983 changed and there was no change in the number of suicides. Some of these impacts were anticipated, such as the reduction in admissions, whereas others were unexpected.
Limitations of this study include use of routinely collected data, particularly in relation to diagnosis. However, for bias to be present one would have to argue that as the rate of recording of diagnosis went down, this affected different diagnostic groups disproportionately. A 3-month sample was utilised to simplify data collection and we do not feel this has introduced bias across the sample period. The comparison groups for in-patient bed use and for Mental Health Act 1983 activity are not ideal, but represent services that did not undergo such dramatic change during the study period.
Our opinion is that this study supports the notion that in routine clinical practice in the NHS crisis resolution home treatment teams can be effective in reducing psychiatric admissions. Shortly after the introduction of this crisis team bed occupancy fell below 100% and out-of-area admissions stopped. This enabled the closure of an NHS psychiatric ward in 2002 and was the main reason for the closure of the only private adult psychiatric in-patient ward in the area in 2004. However, in October 2004 a further NHS ward was closed in Newcastle and overspill admissions returned.
The crisis team appeared to be particularly successful at reducing short admissions for both men and women. Longer admissions were only reduced in women, particularly young women. As a result the length of stay went up. Hence the reduction in bed occupancy was much more modest than the reduction in admissions. During this study period a large proportion of the assertive outreach team case-load continued to spend long periods in hospital. This mirrors other research that the introduction of an assertive outreach service in inner city populations in the UK does not have an impact on in-patient usage (Reference Killaspy, Bebbington and BlizardKillaspy et al, 2006). However, we are not able to fully investigate these influences in this study.
One explanation may be that home-based treatment is a more suitable alternative for what would have turned out to be short admissions. Another may be that the gate-keeping role is important, especially out of hours when this was previously carried out by senior house officers on call. The gender and age differences are interesting and may reflect the fact that some younger women have more support in the community, making home-based treatment a more viable option, or that they may have more reasons to stay out of hospital, such as responsibility for children.
Importantly, as with any service innovation, it is reassuring to note that there was no significant increase in the number of suicides over the study period. With the widespread implementation of crisis resolution home treatment teams, concern has been expressed regarding the risks and safety of managing acutely ill patients at home. These data suggest that the service changes described are a safe alternative to hospital admission in terms of suicide.
Mental Health Act 1983 statistics show a reduction in the use of section 5(2) and 5(4), an increase in section 2 and a delayed increase in section 3. Some of these changes may be explained by the use of home-based treatment for a group of patients who initially agree to informal treatment but gradually deteriorate and require detention under the Mental Health Act 1983. Previously they would have been in hospital and detained under section 5(2) or 5(4), but now are home treated and are detained under section 2 or 3. According to data published by the Health and Social Care Information Centre (2007) approximately 30–40% of detentions under section 5(2) revert to informal admissions. Another factor may be that the assertive outreach team has identified and remained in contact with patients who have difficult to manage illnesses. Ultimately some of these are detained, so increasing the pool of patients in contact with services. It is worth noting that the crisis team was not routinely involved in Mental Health Act 1983 assessments.
The knock-on effect of the reorganisation on the acute in-patient wards has been substantial. The increase in the relative number of patients staying for longer periods, detained, and with psychotic disorders has clear implications for in-patient staff, the therapeutic environment and most importantly the experience of patients. The change in length of stay has implications for the number of beds required, but it also points to other parts of the service. Length of stay can also be increased by a lack of suitable supported housing, hostels and rehabilitation services. If a range of such placements were available then it might be possible to reduce length of stay on acute in-patient units. We could then be more certain that the most expensive part of the service was being used most effectively.
In summary, a pattern appears to be emerging across the UK: a crisis resolution home treatment service is established with model fidelity (Reference Niemiec, Tacchi and KennedyNiemiec & Tacchi, 2003); psychiatric admissions reduce; morale increases as bed occupancy falls below 100%; efficiency rises; and some beds can be closed. These changes enable inpatient units to focus their delivery of care and marginally increase the staff to patient ratio. However, there is a risk that the significant financial pressures on mental health trusts can result in too many bed closures, particularly if decisions about bed closures are based on the reduction in admissions rather than the reduction in bed occupancy. Before closing beds the differing needs of those with short-term and those with longer-term conditions need to be considered. Otherwise the bed closures combined with the increased length of stay can result in occupancy levels returning to 100% but with greater levels of disturbance on the wards. This is to be avoided if the full benefits of this important development in community mental healthcare are to be maintained.
Declaration of interest
None.
Acknowledgements
We thank Valerie Maddison, Information Manager at the IT Department of the North Tyneside Primary Care Trust for providing the raw data on suicides.








eLetters
No eLetters have been published for this article.