Introduction
Population ageing poses health-care challenges worldwide, since it increases the risk of physical health problems, as well as mental and neurological disorders, such as depression and dementia, in older adults (World Health Organization, 2017a). The increase in the number of individuals with dementia is becoming a global issue (World Health Organization, 2017b), and depression has been reported to have the highest relative risk (1.9) among the five main risk factors for dementia among those aged 65 years and above (Livingston et al., Reference Livingston, Sommerlad, Orgeta, Costafreda, Huntley, Ames, Ballard, Banerjee, Burns, Cohen-Mansfield, Cooper, Fox, Gitlin, Howard, Kales, Larson, Ritchie, Rockwood, Sampson, Samus, Schneider, Selbæk, Teri and Mukadam2017).
Today, reminiscence practice is gaining popularity as a psycho-social approach for mental health promotion in older adults (Westerhof et al., Reference Westerhof, Bohlmeijer and Webster2010; Zhou et al., Reference Zhou, He, Gao, Yuan, Feng and Zhang2012; Okuda et al., Reference Okuda, Hashimoto and Jikumaru2017). First proposed by Butler (Reference Butler1963), reminiscence practice has since been used by various professionals. Over the years, reports on the effectiveness of this practice in older adults with dementia (Charlesworth et al., Reference Charlesworth, Burnell, Crellin, Hoare, Hoe, Knapp, Russell, Wenborn, Woods and Orrell2016; Lök et al., Reference Lök, Bademli and Selçuk-Tosun2019) and community-dwelling older adults (Franck et al., Reference Franck, Molyneux and Parkinson2016) have been accumulating. Many of the reports have indicated that there are positive effects of reminiscence practice on the depression and cognitive function of older people with dementia, but further accumulation of efficacy studies is needed (Woods et al., Reference Woods, O'Philbin, Farrell, Spector and Orrell2018). Previous studies in community-dwelling older people have shown a reduction in depression (Zhou et al., Reference Zhou, He, Gao, Yuan, Feng and Zhang2012; Choy and Lou, Reference Choy and Lou2016), and the effectiveness of reminiscence practice for improving cognitive function (Jahanbin et al., Reference Jahanbin, Mohammadnejad and Sharif2014) is being investigated by randomised controlled trial design, but there are very few reports. In other words, examinations of its effects on depression in community-dwelling older adults remain inadequate (Tavares and Barbosa, Reference Tavares and Barbosa2018), and evidence of its effectiveness in dementia prevention is limited (Duru and Dutkun, Reference Duru and Dutkun2018). Further, in recent years, research has been conducted on psychological effect focusing on nostalgia (Routledge et al., Reference Routledge, Wildschut, Sedikides and Juhl2013; Ismail et al., Reference Ismail, Christopher, Dodd, Wildschut, Sedikides, Ingram, Jones, Noonan, Tingley and Cheston2018).
In this context, an effective approach involves the use of sensory elements, such as music, photographs and other stimuli, in addition to the initiation of conversations in group settings, to encourage reminiscence in older adults (Jopling and Mousley, Reference Jopling and Mousley2018). Although many attempts have been made to implement such a reminiscence practice, evidence on the use of sensory elements as reminiscence cues remains insufficient (Umemoto et al., Reference Umemoto, Shibata and Hayashi2016; Mahendran et al., Reference Mahendran, Rawtaer, Fam, Wong, Kumar, Gandhi, Xu Jing, Feng and Kua2017).
With the goal of conducting further research to solve this problem, a reminiscence practice programme was developed to prevent depression and dementia. Hanaoka et al. (Reference Hanaoka, Muraki, Ede, Yamane and Okamura2016) demonstrated that olfactory stimulation is associated with cues that encourage reminiscence in older adults. It is also reported that reminiscence practice using raw materials as olfactory stimuli alleviates depression better than reminiscence practice through conversations alone (Hanaoka et al., Reference Hanaoka, Muraki, Ede, Yasuhara and Okamura2018). However, a problem pertaining to the complexity of using raw materials as odorous substances remained unaddressed. To use olfactory stimuli in a manner that requires less preparation, Hanaoka et al. (Reference Hanaoka, Muraki and Okamura2019) investigated the use of the 40 odorous substances from the Japanese version of the University of Pennsylvania Smell Identification Test (UPSIT-J; Ogihara et al., Reference Ogihara, Kobayashi, Nishida, Kitano and Takeuchi2011). It was found that more than 70 per cent of older adults had reminiscence experiences with 16 of these substances.
For olfactory stimuli and memory, the olfactory nervous system and amygdala are closely related (Herz, Reference Herz2004), and the olfactory sense is known to evoke emotionality and to be strongly associated with memory. The autobiographical memory recalled by olfactory cues has been reported to be clearer and more emotional than verbal labels (Chu and Downes, Reference Chu and Downes2002). For this reason, the possibility of application to reminiscence practice using olfactory cues that take advantage of the characteristics of olfactory stimuli is also mentioned (Yamamoto, Reference Yamamoto2015).
Based on this preliminary investigation (Hanaoka et al., Reference Hanaoka, Muraki, Ede, Yasuhara and Okamura2018, Reference Hanaoka, Muraki and Okamura2019), the current study evaluated the effects of simple reminiscence practice using olfactory stimuli on depression and cognitive function in community-dwelling older adults.
Materials and methods
Study design and participants
This study included a single-blind randomised controlled trial. The inclusion criteria for study participants were as follows: they were (a) natives of Japan, (b) 65 years or older, (c) living in a community, (d) capable of visiting the trial facilities, and (e) capable of providing written informed consent to participate. The exclusion criteria were: they (a) were receiving long-term care insurance benefits, (b) had documented olfactory disorders, and (c) experience communication impediments in daily life.
Participants were recruited from comprehensive community care centres after obtaining permission from the individuals implementing care prevention services in the community to hold briefings for those visiting the centres. The researchers held briefings at four community centres two weeks prior to the intervention to explain verbally the study's purpose and characteristics and obtain the participants’ complete written consent.
The sample size was calculated as 48 individuals using G*Power software (Faul et al., Reference Faul, Erdfelder, Lang and Buchner2007), and by assuming a medium effect size of 0.25, alpha of 0.05 and power of 0.80 to examine the interaction between two factors (time and group) using a repeated-measures analysis of variance (2 × 2 design). A 20 per cent dropout rate was predicted, and the targeted number of participants was 58 (29 each in the intervention and control groups).
Procedure
The individuals who consented to participate underwent questionnaire screening to confirm their eligibility (Figure 1). Participants who met the criteria were randomly assigned to either the intervention group or control group for each community centre using a computer program run by a third party that was not involved in the analysis.
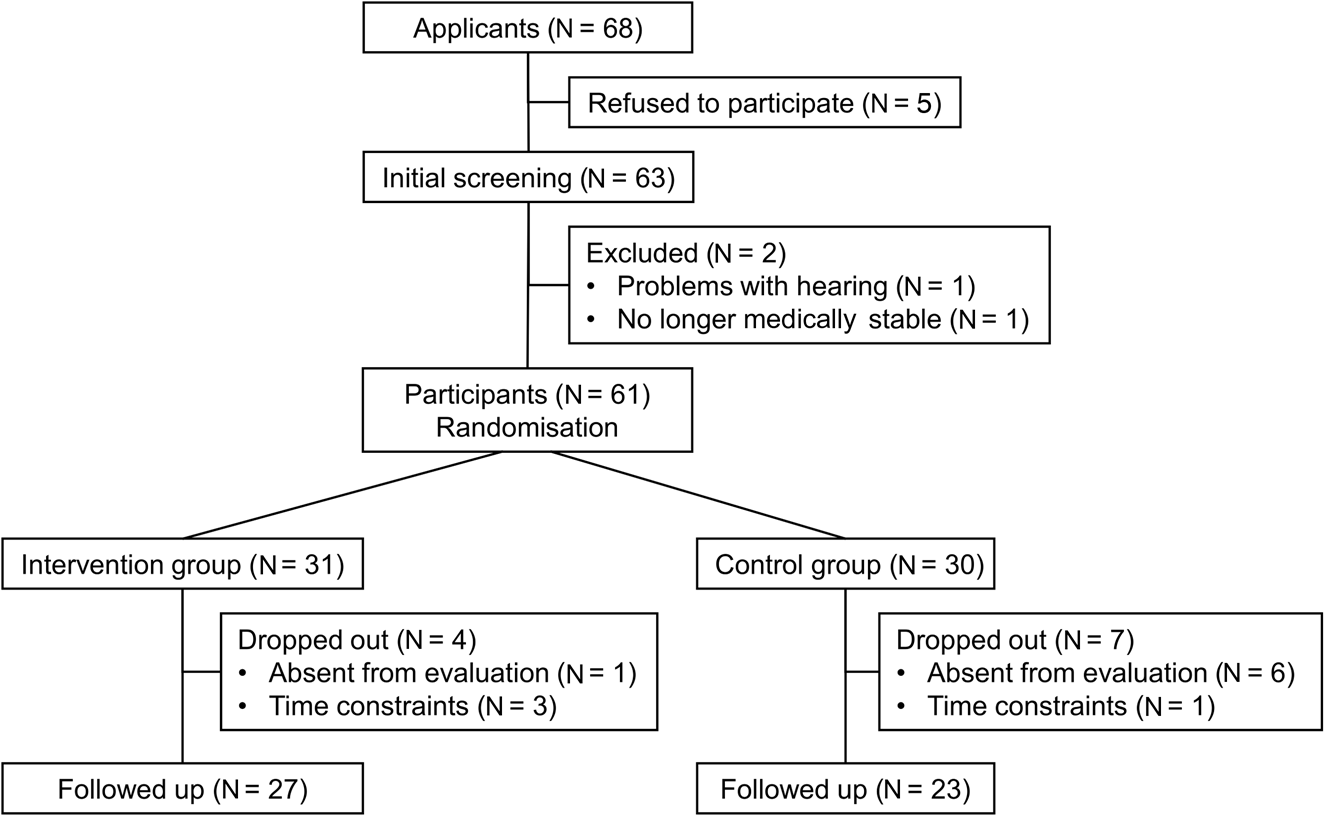
Figure 1. Study participation data.
The intervention and control groups underwent group reminiscence practice using olfactory and language cards, respectively. Each session included one group leader from the study team and approximately seven participants. The group leaders were occupational therapists who had previously attended a basic course (comprising two 60-minute sessions on reminiscence practice's history and significance, implementation methods, group-work techniques and points to consider during implementation) that was considered necessary for the group reminiscence practice by the lead author. Both groups were evaluated at the baseline and after the completion of all sessions (two time-points).
Reminiscence sessions
Intervention group
The study recruited older adults participating in calisthenics at the community centres as a once-weekly long-term care prevention service. Twelve group sessions were implemented, in which reminiscence was prompted using olfactory cards from the UPSIT-J (Ogihara et al., Reference Ogihara, Kobayashi, Nishida, Kitano and Takeuchi2011). Reminiscence practice was performed either immediately before or after calisthenics for approximately 40 minutes, to limit the participants’ burden. Unlike the conventional reminiscence practice, the sessions did not follow any theme. At the beginning of the session, one of the participants placed 12 numbered cards in a bag with numbers corresponding to 12 olfactory substances (sandalwood, yuzu fruit, fish, apple, smoke, wintergreen, soap, menthol, watermelon, grass, chocolate and peach), and one of the participants in the group took one card from the bag and chose the type of card to be used in each session. These olfactory substances (excluding those with gender differences) were found to have the highest percentage of recall experiences in our previous survey (Hanaoka et al., Reference Hanaoka, Muraki and Okamura2019). The leader passed the selected olfactory card to each participant, who rubbed the card's microencapsulated odorous part using a cotton swab and then sniffed the emitted smell for approximately 30 seconds. Subsequently, the leader asked the participants to state whether the smell reminded them of anything from their past and, if so, the memories or thoughts that were triggered by the smell.
The group sessions involved the following four stages: (a) reflection on the previous session; (b) an olfactory card's random selection by one participant and subsequent distribution by the leader; (c) participants individually smelling the card and talking about the memories or thoughts that were triggered, followed by a discussion; and (d) the leader asking the members about their impressions and briefly summarising the session.
Control group
The timing, frequency, how recall stimuli were selected and structure of sessions were the same for both the intervention and control groups; however, instead of olfactory cards, the control group used language cards to prompt reminiscence. The language cards used were pieces of A4 card paper on which were written the names of each of the same 12 odorous substances as those for the intervention group as reminiscence stimuli.
Measures
Participant characteristics
A questionnaire survey was conducted to obtain information on the participants, such as their age, gender, presence or absence of a spouse, education, financial situation and sense of health.
Olfactory visual analogue scale (VAS)
A VAS was used to evaluate olfactory function based on participants’ subjective assessments (McCormack et al., Reference McCormack, Horne and Sheather1988). The left end of the 10-centimetre scale bar depicted ‘no smell at all’, whereas the right end indicated a ‘perfectly obvious smell’. The participants made marks on the scale to indicate their olfactory function, and the degree of olfactory awareness was an approximation presented as a VAS score (percentage). Some reports indicated the assignment of a cut-off point of 47 per cent (Takebayashi et al., Reference Takebayashi, Tsuzuki, Oka, Fukazawa, Daimon and Sakagami2011); however, in the current study, with the exception of those who answered ‘no smell at all’, all participants with a score below the 47 per cent cut-off were included in the analysis.
Geriatric Depression Scale-15 (GDS-15)
The Geriatric Depression Scale is a 30-item self-administered tool that measures depression in older adults (Brink et al., Reference Brink, Yesavage, Lum, Heersema, Adey and Rose1982). A shortened version with 15 items (GDS-15), each of which can be answered either ‘yes’ or ‘no’, is commonly used. The score ranges from 0 to 15 points, and higher scores indicate higher levels of depression. Further, a Japanese version has been developed with confirmed reliability and validity (Yatomi, Reference Yatomi1994).
Five Cognitive Test
The Five Cognitive Test measures group cognitive function (Yatomi and Asada, Reference Yatomi and Asada2006). It can measure the cognitive level of healthy community-dwelling older adults and identifies mild cognitive impairment. It considers the Japanese cultural background and helps determine the effects of dementia prevention programmes on community-dwelling older adults (Shigematsu et al., Reference Shigematsu, Okura, Nakagaichi and Nakata2014).
The test includes five tasks: cued recall, character position referencing, animal name listing, clock drawing and analogy tests. The time required to complete all tasks is approximately 45 minutes. We used a particular version of the test in which only the cued recall and character position referencing tests are performed to shorten the time by 15 minutes and reduce the participants’ burden. The cued recall test involves the memorisation of 32 words together with categories serving as cues and measurement of memory ability by having the subjects recall the memorised words using the categories as hints (score range: 0–32). The character position referencing test requires subjects to circle the items where the Japanese characters for ‘top’, ‘middle’ and ‘bottom’ match the positions at which the characters are written, while simultaneously numbering these circled characters to measure attention ability (score range: 0–40).
This test can be simultaneously performed on a group of up to 100 individuals by using a DVD and projecting the tasks on to a screen. After providing the necessary information on a prepared test sheet, participants are presented each task in accordance with the audio and video and are required to supply their answers. Higher scores indicate higher level of cognitive function for each task. The test's reliability and validity have been confirmed (Sugiyama et al., Reference Sugiyama, Mutsuo, Sakuma, Miyamae, Ito, Ura, Inagaki, Okamura, Yatomi, Yamaguchi, Fujiwara, Takahashi and Awata2015).
Statistical analysis
First, after checking the normality of the variables (age, olfactory VAS score, GDS-15 score, cued recall score, character position referencing score) at baseline using the Shapiro–Wilk test, participants’ basic characteristics and olfactory VAS scores at baseline were compared between the two groups using the t-test, chi-squared test or Fisher's exact test. Subsequently, to examine the effectiveness of group reminiscence therapy using olfactory stimuli, a repeated-measures analysis of covariance was conducted with time (baseline and post-intervention) and group (intervention and control groups) as independent variables, and depression and cognitive function as dependent variables. Variables showing significant inter-group differences in baseline comparison were used as covariates. For significant interactions between time and group, paired t-tests were conducted to compare baseline and post-intervention scores for both intervention and control groups.
Finally, to examine the factors associated with changes in depression and cognitive function scores, an evaluation was performed using Pearson's product-moment correlation coefficient or a t-test, with changes in depression and cognitive function scores (baseline to post-intervention) as the dependent variables, and basic characteristics, olfactory VAS scores, and depression and cognitive function baseline scores as the explanatory variables. In all the tests, p-values were two-sided, and p < 0.05 indicated statistical significance. All statistical analyses were performed using SPSS version 24.0.
Results
Study participation
Among the individuals who consented to participate and underwent initial screening, 61 satisfied the eligibility criteria and were randomised into one of the two groups. The intervention group recorded four dropouts: one participant who was absent from the evaluation and three who did not participate in a sufficient number of sessions. Meanwhile, the control group had seven dropouts: six participants who were absent from the evaluation and one who did not participate in a sufficient number of sessions. The final sample for analysis included 27 and 23 participants in the intervention and control groups (Figure 1).
Baseline comparison
Table 1 depicts the results of a baseline comparison of basic characteristics between the intervention (N = 31) and control (N = 30) groups. The mean ages were 77.2 (standard deviation (SD) = 5.3) and 80.4 (SD = 6.0) in the intervention and control groups, respectively. Apart from age, no other significant differences were found between the two groups. Further, both the groups included more female participants than male, and approximately 30 per cent of the participants in both the groups had a spouse.
Table 1. Basic characteristics and olfactory function of study participants at baseline
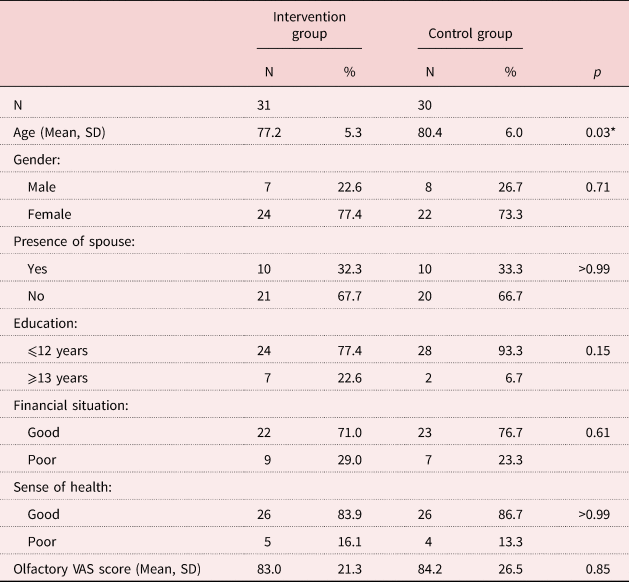
Notes: SD: standard deviation. VAS: visual analogue scale.
Significance level: * p < 0.05.
Comparison of score changes among groups
To examine the differences between the two groups in terms of changes in depression and cognitive function scores from the baseline to post-intervention, an analysis of covariance was conducted with age as the covariate, since this variable showed a significant difference in the baseline comparison of the groups’ basic characteristics. A significant interaction between time and group was found only for the GDS-15 scores (p = 0.04; Table 2). Subsequently, paired t-tests were performed to compare the GDS-15 scores at baseline and post-intervention among the groups, which revealed a significant change in the intervention group alone (p = 0.01).
Table 2. Scores on the Geriatric Depression Scale-15 (GDS-15) and cued recall and character position referencing tests for the intervention and control groups

Notes: N = 27 (intervention group) and N = 23 (control group). 1. F-statistic in repeated-measures analysis of covariance, with age as the covariate. SD: standard deviation.
Significance level: * p < 0.05.
Factors associated with changes in GDS-15 scores
An examination of the associations between the change in GDS-15 scores in the intervention group and basic characteristics, olfactory VAS scores and baseline GDS scores revealed a significant negative association with baseline GDS-15 scores alone (γ = −0.406, p = 0.04; Table 3).
Table 3. Factors associated with changes in Geriatric Depression Scale-15 (GDS-15) score in the intervention group
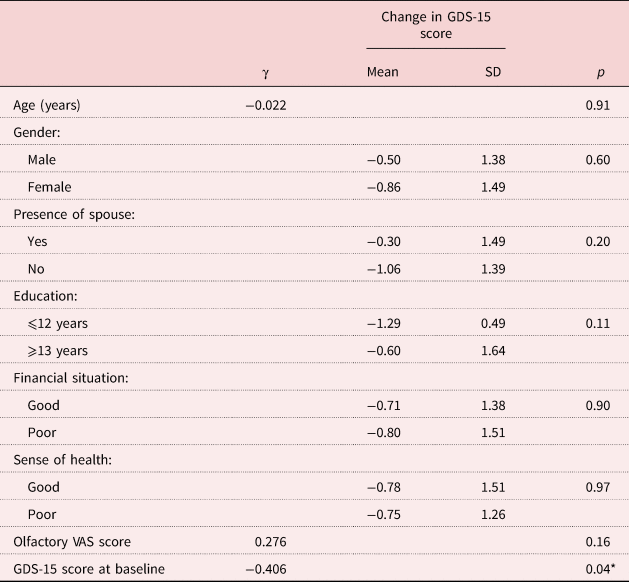
Notes: N = 27. SD: standard deviation. VAS: visual analogue scale.
Significance level: * p < 0.05.
Discussion
This study assessed a reminiscence practice programme that could easily be implemented for community-dwelling older adults. Reminiscence practice was performed using olfactory cards from the UPSIT-J, and the results revealed that this practice could alleviate depression to a higher extent than the practice of using language cards. This finding is consistent with the result of Hanaoka et al. (Reference Hanaoka, Muraki, Ede, Yasuhara and Okamura2018), who found a tendency towards depression alleviation in community-dwelling older adults who underwent group reminiscence practice using raw material smell stimuli tailored to various themes.
Willander and Larsson (Reference Willander and Larsson2007) compared memories of earlier personal events triggered by three cues – a smell cue alone, a language label cue alone and a smell plus language label cue – and found that autobiographical memories were the most emotional with a smell cue alone. Similarly, Herz (Reference Herz2004) compared smell, vision and hearing cues that trigger autobiographical memories and reported that smell was accompanied by the most emotional sensations, which felt like reliving the experience. Willander and Larsson (Reference Willander and Larsson2006) reported that smells evoke older memories than do language or vision, and that these memories include many events from before the age of 10 years.
The participants talked about the details that were triggered by the reminiscence cues without being bound by a theme. In such sessions, the other participants and group leader empathised with the recounted details and thoughts. Although the intervention and control groups did not differ in terms of the recall method, except for the method of providing recall clues, the intervention group depicted a stronger tendency for depression alleviation. Hence, reminiscence therapy using smells was found to be better at making participants’ reminiscences more emotional. Moreover, childhood was the period recalled by most of the participants, and these recollections comprised relatively pleasant memories. In addition, although there was a significant difference in age between the intervention group and the control group at baseline, it was a difference of approximately three years and was considered to have had little effect on the contents of the recall. However, it is necessary to examine whether the recall card used this time was an olfactory element that is easily connected to the recall, and whether there is a possibility of a difference in recall depending on the participant characteristics.
A survey of the emotions that accompany autobiographical memories triggered by smell cues from an anatomical perspective revealed a connection between the sense of smell and the amygdala (Masaoka et al., Reference Masaoka, Sugiyama, Katayama, Kashiwagi and Homma2012). The following studies used functional magnetic resonance imaging to examine participants’ brain activity at the time they recalled autobiographical memories using smell cues. Herz (Reference Herz2004) reported that such recalled autobiographical memories are more emotional, and the amygdala and hippocampus are more activated by smell cues than visual cues. Furthermore, Arshamian et al. (Reference Arshamian, Iannilli, Gerber, Willander, Persson, Seo, Hummel and Larsson2013) reported that the brain's emotional regions, such as the amygdala, are more activated by smell cues than language cues. Hence, the current study's results are consistent with those of brain-imaging studies.
Regarding the effects on cognitive function, an examination of the changes in scores on the Five Cognitive Test (Yatomi, Reference Yatomi1994), which was developed to detect mild cognitive impairment, revealed no significant interactions. Hence, we could not confirm that the use of olfactory cards as reminiscence cues is more effective in developing participants’ memory ability and attention than that of language cards in reminiscence practice.
Umemoto et al. (Reference Umemoto, Shibata and Hayashi2016) examined the effects of reminiscence practice using smell cues on cognitive function in community-dwelling older adults. Their results suggested a potential improvement in memory ability, which is inconsistent with the current study's findings. Umemoto et al. (Reference Umemoto, Shibata and Hayashi2016) simultaneously evaluated the effects of reminiscence practice and smell cues using a one-group pre–post design. This is different from the current study's design, which examined the effects of the presence or absence of smell cues on cognitive function. This difference may explain the inconsistent results. Another reason for the inconsistency may be the difference in presentation of the smell cues. To simplify the smell cues, the current study used odorous substances from the UPSIT-J and distributed a single olfactory card to the participants in each session; however, in the study by Umemoto et al. (Reference Umemoto, Shibata and Hayashi2016), multiple essential oil and raw material smells were presented in each session in accordance with a theme. With the presentation of multiple odorous substances, the recognised smells were more frequently transmitted to the hippocampus, which controls memory. This created a situation where older adults with various experiences may have easily made connections with the different memories recalled by each participant, which may have affected the improvement effect on memory ability.
Other approaches, besides reminiscence practice, that focus on the sense of smell to improve cognitive function are also being commenced. Birte-Antina et al. (Reference Birte-Antina, Ilona, Antje and Thomas2018) examined the effects of olfactory stimuli on cognitive function by administering five months of olfactory training to subjects aged 50–84 years, who were asked to smell four different odorous substances twice a day: once in the morning and once in the evening. They, however, reported no effects on memory ability or attention. Meanwhile, a study that examined the effects of olfactory stimuli on the cognitive function of older people with dementia by performing aromatherapy for 28 days using essential oils for two hours at a time – in the morning and before falling asleep – did not mention memory ability and attention but did demonstrate improvement in cognitive function (Jimbo et al., Reference Jimbo, Kimura, Taniguchi, Inoue and Urakami2009). In such interventional studies focusing on sense of smell, differences are seen in various aspects including the duration, frequency and timing of olfactory stimuli application, as well as the participants involved. Results for the effects on cognitive function are, therefore, inconsistent. Previous studies of cognitive function with reminiscence practice have used the Mini-Mental State Examination for a screening assessment (Jahanbin et al., Reference Jahanbin, Mohammadnejad and Sharif2013), and it is not clear, to date, whether they work on memory. It is necessary to examine further if the combined use of olfactory stimulus leads to the improvement of memory as a synergistic effect when the recall method is carried out.
Further, we examined the baseline factors’ effects on changes in GDS-15 scores in the intervention group, that is, the factors that should be considered in an intervention involving reminiscence practice using olfactory stimuli. No association was found between the changes in GDS-15 scores and basic characteristics or olfactory function; however, there was a significant association with baseline GDS-15 scores, similar to an earlier study's results (Hanaoka and Okamura, Reference Hanaoka and Okamura2004). This suggests that depression can be more easily alleviated in people with higher depression levels than lower levels; therefore, this intervention programme can help maintain and improve the mental health of community-dwelling older adults.
Finally, olfactory function was measured using an olfactory VAS prior to the intervention to examine its effect on the intervention outcome; however, no significant effect was identified. One possible reason for this lack of association is that only three of the 27 participants (approximately 10%) in the intervention group scored below the VAS cut-off of 47 per cent, that is, the number of participants with suspected olfactory disorder was low. Furthermore, unlike the participants of conventional olfactory tests, the participants of the current study could smell the olfactory cards several times to confirm the smell during the group sessions, which may have compensated for the effects of any olfactory disorder. The third possible reason is that an olfactory VAS is an imprecise measure, as pointed out by some researchers (Mori et al., Reference Mori, Matsuwaki, Mitsuyama, Yamazaki, Okushi and Moriyama2011), and the participants’ olfactory function was inadequately captured. Therefore, simple and reliable olfactory-function evaluation methods and eligibility criteria are required to implement effective reminiscence practice programmes that use smell cues based on a high level of evidence.
Limitations
This study has several limitations. First, there were many dropouts, especially in the control group, which may have resulted in less than the adequate sample size required for analysis. Second, the mean age of the control group was significantly older than the intervention group at baseline. Finally, in recent years, research focusing on the nostalgic olfactory has been carried out; however, in this study, it was not possible to examine the olfactory stimuli about which the participants felt nostalgic.
In the future, it is necessary to make efforts to secure the necessary number of cases in which dropouts are assumed, and to encourage participants during the intervention in order to avoid dropouts. Further, when reminiscence practice is carried out using the olfactory stimulus, examining the effect of the brittleness and the effect on cognitive function and other variables is a problem.
Conclusions
This study could not demonstrate whether reminiscence practice using olfactory cards as olfactory stimuli affected cognitive function in older adults; however, this practice was found to alleviate depression among participants. To meet the needs of older adults, whose ageing progresses over the years, programmes that are practical, easy to implement during community activities and can be conveniently attended should be developed. The results of the current study suggest the significance of implementing effective reminiscence practice as an initiative to help maintain mental health, which is considered a risk factor for dementia.
Acknowledgements
We thank all participants and the associated personnel who co-operated in this study. We would also like to thank Editage (www.editage.com) for English-language editing.
Author contributions
The author contributions were as follows: conceptualisation – HH, TM and HO; methodology – HH, TM and HO; analysis – HH and TM; investigation – HH, FK and SY; resources – HH, FK and SY; data curation – HH and FK; writing original draft – HH and TM; writing, review and editing – all authors; and supervision – HO.
Financial support
This work was supported by JSPS KAKENHI (grant number JP 16K01506). The funding source had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
This research was approved by the Ethical Committee for Clinical Research of Hiroshima University (C-236) and all study procedures were performed in accordance with the Declaration of Helsinki. In addition, only individuals who gave their written consent to participate after receiving a full explanation were included in the study. The process can be found at https://cimr.hiroshima-u.ac.jp/rinsho/rinsho-research/start.






