Quality improvement (QI) has leapt up the agenda in healthcare over the past couple of decades, moving from relative obscurity to centre stage. In the UK, terrible events laid bare by Sir Robert Francis's inquiry into Mid Staffordshire hospital renewed focus on the need to improve quality and maximise safety (Reference FrancisFrancis 2013). This urgency was brought even closer to home for psychiatrists by the subsequent events at Winterbourne View Hospital (Department of Health 2012).
Healthcare leaders increasingly need to achieve ‘better value for patients from the resources available to the NHS’ (Reference Appleby, Ham and ImisonAppleby 2010). QI is a framework for realising this ambition, defined by Reference Batalden and DavidoffBatalden & Davidoff (2007) as the ‘combined and unceasing efforts of everyone – healthcare professionals, patients and their families, researchers, payers, planners and educators – to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development’.
Contemporary thinking about QI in healthcare draws heavily from other industries; the aeronautical and car manufacturing sectors are frequently cited as exemplars of safety and efficiency, respectively.
Many in healthcare focus on the rigorous safety measures in place in the airline industry that have transformed air travel over the years from a dangerous indulgence to one of the safest forms of transport (Reference DonaldsonDonaldson 2002). Internationally, there has been growing recognition of the importance of so-called human factors (Reference ReasonReason 1995). The Health and Safety Executive (1999) defines these as:
‘environmental, organisational and job factors, and human and individual characteristics, which influence behaviour at work in a way which can affect health and safety […] A simple way to view human factors is to think about three aspects: the job, the individual and the organisation and how they impact on people's health and safety-related behaviour’.
The World Health Organization (2009) outlines ten areas of safety in healthcare:
-
• organisational safety culture
-
• managers’ leadership
-
• communication
-
• team (structures and processes)
-
• team leadership (supervisors)
-
• situation awareness
-
• decision-making
-
• stress
-
• fatigue
-
• work environment.
These demonstrate the complex relationships between the job, the individual and the organisation; attention must be paid to each, as well as considering how they interact. Innovations such as critical incident reporting, the introduction of the European Working Time Directive and efforts to create a ‘no-blame’ culture to encourage people to speak out are all examples of safety improvement initiatives based on human factors concepts (Reference Lawton and ParkerLawton 2002; Reference Datta, Chatterjee and RolandDatta 2011). These mirror pre-existing changes in the airline industry, where all staff are encouraged to raise concerns and there are strict limits on working hours to ensure that key staff, such as pilots, are not compromised by fatigue.
The influence of industry on the evolution of modern approaches to QI in healthcare can be traced back to Walter Shewhart, a physicist, engineer and statistician who worked for the Bell Telephone Company in the 1920s. Shewhart developed statistical methods of understanding variation and used these to drive improvements in production processes, resulting in improved reliability of telephone transmission systems. He asserted that system performance data comprises two types of variation: that which is randomly occurring and normal within the system, and that which is not randomly occurring and so indicates that there is another cause. To find meaning within data, they must be understood in context.
This ability to analyse information about a system and use it to guide improvements influenced William Edwards Deming, who also studied with renowned statisticians Sir Ronald Fisher and Jerzy Neyman. Deming famously went on to influence the automotive industry in Japan in the 1950s and is widely credited as the inspiration for the Japanese post-war economic ‘miracle’.
Deming urged those wishing to make an improvement in any system to take a fourfold approach that he named the ‘system of profound knowledge’. This demands simultaneous appreciation of the system, understanding variation within that system, considering the psychology and behaviour of the people in the system and taking an epistemological perspective (Reference DemingDeming 2010). Several approaches that arose from this philosophy of using statistical techniques to streamline manufacturing process, such as Lean and Six Sigma, have subsequently been applied to healthcare (Reference DelliFraine, Langabeer and NembhardDelliFraine 2010).
QI and audit in times of financial constraint
Clinical audit has long been seen as an essential cornerstone of clinical governance. Audit was introduced in to the National Health Service (NHS) by the government's white paper Working for Patients (Department of Health 1989). Audit is the process of setting explicit standards, then measuring practice against these standards and implementing the necessary change to improve patient care, thereby addressing any deviation from the standards (Reference PalmerPalmer 2002). It has been criticised as being overly focused on the process of data collection, with inadequate emphasis on bringing about the actual improvements (Reference Hillman and RouechéHillman 2011). When used to assess practice against minimum standards, audit becomes an exercise in quality assurance, focused on improving outcomes to meet a ‘good enough’ target, in contrast to continuous quality improvement, which seeks to achieve the ‘best possible’ outcomes through improved healthcare processes (Reference GoldstoneGoldstone 1998).
Clinical audit is not completely distinct from quality improvement; they share the repeated collection of data to inform change efforts, with a focus on improving patient outcomes and experience in a climate of financial restraint. Emphasising that healthcare is delivered within complex systems, Reference Langley, Moen and NolanLangley et al (2009) define systems as ‘interdependent group[s] of items, people, or processes working together toward a common purpose’ (p. 77). Audit generally involves staff in a discrete part of a system regularly accessing data within their local context to evaluate ‘what is happening in clinical practice against explicit criteria’ (Reference Hill and SmallHill 2006).
QI recognises that improved performance of individual parts cannot, on its own, maximise the effectiveness of the system as a whole (Reference Langley, Moen and NolanLangley 2009). It moves beyond clinical audit to multidisciplinary scrutiny of a system, emphasises integration, uses open-ended questions and seeks qualitative as well as quantitative data. QI seeks to bring about better outcomes while either reducing expenditure or, if this is not possible, ensuring that the best possible value is achieved for the investment made (Reference PorterPorter 2010). The process of improvement itself can bring about substantial savings by eliminating unnecessary activity, reducing costly harms and increasing efficiency. An intervention in a psychiatric inpatient unit designed to reduce violence has the potential to save money in a number of ways, as observed by Reference Brown, Fawzi and McCarthyBrown et al (2015), who conducted a financial analysis of their work to reduce physical violence on three older adults’ wards and observed a reduction in direct costs of £58 612, balanced against the £2000 required to fund environmental improvements.
The Model for Improvement
Developing knowledge of QI principles and methodology requires dedicated study and the opportunity to apply learning in an experiential environment. There are several different approaches, with their own perspectives for understanding and influencing positive change. By way of an example, the Model for Improvement (Fig. 1) provides an accessible framework to accelerate improvement efforts, posing three fundamental questions that are combined with Deming's structure for iteratively testing changes, the plan–do–study–act (PDSA) cycle (Reference DemingDeming 2010).
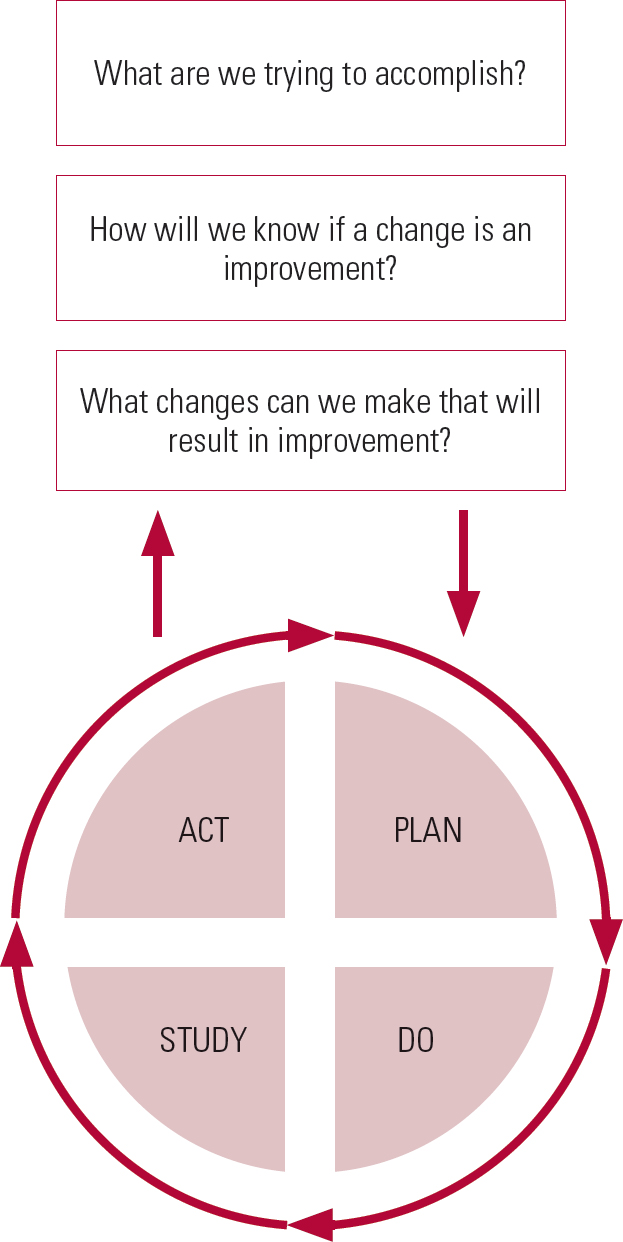
FIG 1 The Model for Improvement, developed by Associates in Process Improvement. Redrawn with permission from Reference Langley, Moen and NolanLangley et al (2009).
This model encourages those who would like to bring about change to engage with other stakeholders across the system and systematically plan changes they believe will be beneficial. Couched in the plural, the approach emphasises that sustainable change in a complex system necessitates joint working by people with multiple perspectives, across disciplines, professions and even organisations.
Having identified an area for improvement and outlined the scope and time frame of the work, the team need to determine what they must measure in order to find out whether a change being tested does indeed lead to improvement. The group agree in advance what evidence will be required to justify either further scrutiny or continued investment of effort with regard to a particular intervention. They then generate ideas about what could be tested and decide by consensus which change ideas will be prioritised for testing.
During testing, the PDSA cycle is used to refine and improve the change being attempted until the group of stakeholders is confident about the effectiveness of the change. Having proposed what will be done (plan), a change is carried out (do) and then reflected upon using relevant qualitative and quantitative information as appropriate, which is compared against the team's predictions (study). The learning from this informs the decision made by the team about how to proceed (act), and the next test of change is planned. This cyclical process helps the team to continuously build knowledge using an evidence base that is accumulated through their own practice. It is used to test changes on a small scale at first – even as small as a single patient interaction, for example – thereby reducing the potential risk involved in doing something differently. Reference Langley, Moen and NolanLangley et al (2009) assert that this sequential ‘trial-and-learning’ approach, although it appears counterintuitive, is a more effective way of making improvements in large or complex systems than ‘spending time in a conference room trying to perfect a change and then trying to “install” it’ (Reference Langley, Moen and NolanLangley 2009: p. 102).
The collected data can be analysed using statistical methods designed to understand variation over time. These are routinely used in manufacturing industries but have now been adapted and transposed to healthcare settings, allowing clinicians to consider information in new ways. Unlike traditional methods that aggregate data into quarterly or annual summaries to understand past performance against a ‘quality’ standard, statistical process charts track variation in a way that corresponds with clinically meaningful segments of time. This is determined by the needs of the system, and might be by the hour, week or month, or it might track time between rare events. Maintaining real-time relationships between data and events that accompany them preserves the richness of information being generated, permitting associations between changes and outcomes to be postulated and allowing future system performance to be predicted. This permits improved planning of resources, helps teams to guide patients’ expectations of the service – for example, waiting times – and supports managers to identify which improvements to quality outcomes will require system redesign.
Adaptive v. technical challenges
Identifying aspects of work where applying QI methodology can add value is an important consideration for anybody planning an initiative to improve quality. Reference Heifetz and LinskyHeifetz & Linsky (2002) draw a distinction between two different types of challenge: technical and adaptive.
Technical challenges are those where the problem and its likely solution are understood, requiring internal expertise to reach resolution. An example might be the challenge to improve compliance with mandatory staff training using line management processes. Adaptive problems are different; they are not linear and indeed it may not even be possible to resolve them, for example avoiding pressure ulcers in vulnerable patients. Typically, attempts to tackle adaptive problems will increase understanding of the problem and require the system to change in a sustainable manner if change is to be accomplished. Development of new attitudes, values and behaviours is essential to this process, and success may be understood in terms of the system moving in the right direction.
Traditional management strategies have developed to deal with technical problems, and they can exacerbate problems if implemented with adaptive challenges (Reference HeifetzHeifetz 1994). QI offers an alternative way of dealing with the complex problems we so often face in healthcare systems, and the potential to make changes that lead to ‘improvement beyond what has been seen before’ (Reference Langley, Moen and NolanLangley 2009: p. 16). Any theory of change or logic model to tackle a complex adaptive problem will inevitably involve some technical aspects. QI often includes testing and learning about areas where existing knowledge and experience are weak, and facilitates shorter testing cycles with accelerated implementation in technical areas.
Factors that influence success in QI
The context in which QI is used within healthcare to attempt improvements has been recognised as an important determinant of success, and work is ongoing to establish which contextual factors are sufficiently modifiable to warrant investment at different stages of QI (Reference Fulop and RobertFulop 2015). Reference Kaplan, Provost and FroehleKaplan et al (2011) have explored contextual factors as they relate to QI in healthcare using a systematic review of the literature and structured input from a diverse group of QI experts. Having defined success for a QI project as ‘the implementation of system and process changes and associated outcome improvements’, they identified 25 factors they believed were likely to influence success and created a conceptual model applicable to QI in healthcare. The resulting Model for Understanding Success in Quality (MUSIQ) organises these into several themes: the environment external to the organisation in which QI work is being done; the organisation itself; local QI support and capacity; the team working on the project; and the microsystem in which the team functions (Fig. 2). A related MUSIQ tool allows projects to be scored in each domain, highlighting areas where contextual factors may be supporting or failing to support improvement efforts.

FIG 2 Contextual factors and the level of the healthcare system in which they operate, according to the Model for Understanding Success in Quality (MUSIQ) developed by Reference Kaplan, Provost and FroehleKaplan et al (2011). QI, quality improvement.
Case study: East London NHS Foundation Trust
East London NHS Foundation Trust (ELFT) is one of the UK's largest specialist healthcare providers, delivering mental health services to a population of 750 000 people in east London and, since April 2015, a further 630 000 people in Bedfordshire and Luton. Other provisions in London include community health services in Newham, psychological therapy services in Richmond, and children and young people's speech and language therapy services in Barnet. Services operate from over 100 community and inpatient sites, with over 735 general and specialist in-patient beds, 5000 permanent employees and an annual income exceeding £350 million.
ELFT's organisational mission is to provide the highest quality mental health and community care in England. A large-scale QI programme was launched in February 2014 to help the organisation achieve this. The QI programme is designed to support teams to continuously improve care and to change organisational culture so as to shift power and decision-making to the front line. It encourages teams and patients to drive change, collaborating to creatively tackle some of the trust's most complex quality issues. Two initial ‘stretch’ goals, clearly communicating that maintaining the status quo is not an option, were set: to reduce harm by 30% every year; and to ensure that every patient receives the right care, in the right place at the right time (Fig. 3). Two years after the QI programme was introduced at ELFT, improvement efforts have grown in scale and breadth to over 150 active projects across all areas of the organisation, including corporate services, all clinical services and the Council of Governors (ELFT 2015).
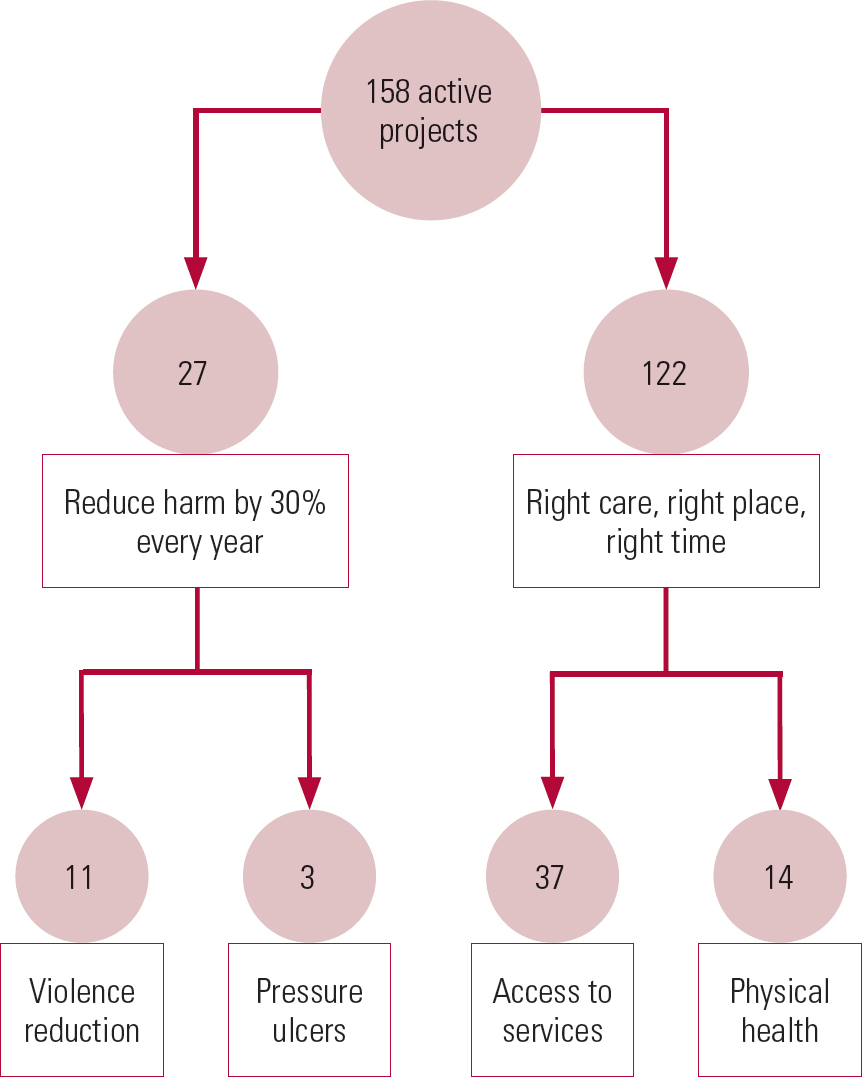
FIG 3 Number of active quality improvement projects and teams testing changes in East London NHS Foundation Trust. Two ‘stretch’ goals are divided into four key priority areas.
Programme design
A key strategic decision to partner with the Institute for Healthcare Improvement (IHI) has enabled ELFT to benefit from their wealth of experience of large-scale QI in healthcare.
Building the will
A multi-faceted campaign has helped build engagement among front-line and senior management staff, as well as patients and stakeholders. This has included launch events, roadshows and conferences, a bespoke QI microsite, regular digital and paper-based internal and external newsletters, and the use of social media.
The need to create space for QI was acknowledged through the trust's ‘Stopping Work of Lower Value’ drive. Teams are encouraged to identify and, where possible, discontinue activities that provide little value to patients and staff.
Building capability
Developing attitudes, knowledge and skills about QI is vital to the process of embedding improvement practice in the organisation. A small central team with expertise in improvement methodology co-ordinates the programme, designs and delivers teaching, builds internal learning communities and supports front-line improvement projects.
During the first 2 years of the programme, 500 people participated in 4 offerings of a 6-month Improvement Science in Action course. These participants include multidisciplinary clinicians of various grades, as well as non-clinical staff who are leading QI projects, patients, executive directors and local commissioners.
In 2015–2016, 30 staff members across all directorates in the trust completed a further 6-month improvement coaching course, cultivating local ambassadors for QI with ring-fenced time to engage with local staff and patients, facilitate discussions about improvement opportunities and act as a knowledge resource for teams. A second cohort of QI coaches was developed in 2016. Fifty senior members of staff linked to management structures in the directorates serve as named QI sponsors, leading QI within each part of the organisation, setting priorities, helping manage allocation of resources to QI and tackling barriers to change.
A modular introduction to QI called ‘Pocket QI’ was introduced in October 2015, with 250 people having completed the four modules by August 2016. The IHI Open School online training course has been made available, with over 250 users to date, and bespoke learning events have resulted in 70 patients and carers receiving training.
Alignment
The trust has been reviewing and redesigning corporate systems to support improvement work. This has included reviewing the clinical audit programme; refreshing the induction process; making data over time available to all staff; and ensuring that QI is embedded within all internal training and development.
Reducing violence
The most frequently reported safety incident in the trust is physical violence, which has therefore been a priority area for improvement and provides an illustration of a learning system being developed across multiple units.
QI methodology was used on the acute adult mental health in-patient ward with the highest frequency of violence to test a number of change ideas, resulting in an increased average time between incidents of physical violence from 5 days to 11 days. The learning from this ward was scaled up to all six in-patient wards in the Tower Hamlets directorate using a collaborative learning approach. The teams meet every 6 weeks to discuss their tests of change and review data. Since the beginning of the project, Tower Hamlets has seen a 40% decrease in incidents of physical violence in its six in-patient mental health wards (Fig. 4), with the four acute adult wards seeing a 57% reduction (Fig. 5).

FIG 4 Rates of incidents of physical violence across all six in-patient mental health wards in Tower Hamlets. LCL, lower control limit; OBD, occupied bed-day; PDSA, plan–do–study–act; UCL, upper control limit. Adapted with permission from Reference Taylor-Watt, Cruickshank and InnesTaylor-Watt et al (2017).

FIG 5 Rates of incidents of physical violence across in-patient mental health wards in Tower Hamlets: the top chart relates to acute wards and the bottom chart relates to intensive care wards. LCL, lower control limit; OBD, occupied bed-day; PDSA, plan–do–study–act; UCL, upper control limit. Adapted with permission from Reference Taylor-Watt, Cruickshank and InnesTaylor-Watt et al (2017).
Across ELFT, a range of ideas have been tested in different settings, including older adult wards, adult mental health wards, intensive care wards and secure forensic wards. The ideas being tested come from both the limited evidence base in this field and the knowledge and experience of our staff and patients. The changes being tested and implemented are diverse and include the use of safety huddles, providing more meaningful activities throughout the week, and sensory stimulation.
Evaluation
Formal evaluations assist in recognising the nature of challenges in the slow process of securing system-wide improvement and can inform efforts to address obstacles (Reference Dixon-Woods, McNicol and MartinDixon-Woods 2012). Annual evaluation has been built into the work at ELFT to ensure that the QI programme continuously adapts to changing needs and environments. This mixed-method evaluation includes compiling existing data, repeating baseline surveys and supplementing these data with new information, primarily qualitative data drawn from interviews, focus groups and additional surveys.
The evaluation in 2015 identified three themes that were felt to help in the implementation of the QI programme: positive front-line engagement, QI team support and strong leadership (ELFT 2015). Conversely, three themes were identified as hindering programme implementation: unclear expectations regarding the QI programme, lack of support structures for staff, and communication problems. QI training was identified as both a helping and hindering factor. It was perceived to be helping because it offered a formal yet creative programme that provided QI projects a lifeline. It was perceived as hindering because there were issues with accessibility and flexibility of training options at the time, which have subsequently been addressed by an expanded range and capacity of learning opportunities.
Learning and sharing
To date, the QI programme has focused on four areas: engaging people across the organisation to use QI approaches to tackle something that matters to their team; enhancing people's knowledge and skills in QI; supporting teams working on QI projects; and ensuring that QI work is embedded into ‘business as usual’, including integration into operational structures. QI project teams now have access to local support systems – including connections with sponsors, coaches and local learning forums – enabling their work to flourish.
Results from the 2015 and 2016 NHS staff surveys are encouraging, with overall staff engagement, job satisfaction, perceived ability to contribute to improvements at work, clinical safety reporting mechanisms, and motivation at work all increasing consistently over the 4 years since this approach to improvement began to be discussed and developed (NHS 2015). Senior leaders in ELFT believe that the QI programme is a significant contributor to this improvement. The recent Care Quality Commission inspection of the trust also noted the impact of the QI approach on encouraging innovation, improving outcomes and experience for patients, and supporting deeper staff engagement. Some fairly unique aspects to the way this programme is being delivered, such as the emphasis on improvement priorities and change ideas being developed at the edge of the organisation by front-line teams together with patients, appear to be critical to the engagement and successes noted at this early stage in the improvement journey. The trust is committed to transparency and shares a great deal of information relating to quality improvement and outcomes openly on the website, as well as holding regular open mornings and an annual QI conference.
The future medical workforce
Improvement requires a progressive accrual of knowledge, skills, values and behaviours; any QI curriculum needs to reflect this. QI learning in the healthcare workforce needs start as early as possible in practitioners’ careers if it is to be embedded in practice. Psychiatrists in training should have the opportunity to develop a basic understanding and engage in practical experience of QI during medical school and foundation training. Examples of effective partnerships between education and health organisations are emerging, for example, collaboration between City University and ELFT, and Stirling University's adapted IHI practicum. These education initiatives are supported by mentors, managers and other clinical staff and provide undergraduate nursing students with structured teaching while aligning them with practice of QI.
The Academy of Medical Royal Colleges’ (AoMRC's) Joint Academy Training Forum commissioned a ‘task and finish’ group to consider this issue as it relates to the medical profession. The group involved key stakeholders from all four UK countries, the aim being to create an increased capacity across the workforce in order to allow healthcare teams to have a positive impact on the delivery of safe and effective patient care.
The final report, Quality Improvement – Training for Better Outcomes, recognises that trainees have generally been expected to focus on audit, which can be a token exercise in data collection, and makes recommendations designed to align efforts to implement QI training as a core component of every doctor's development (AoMRC 2016a). The group's recommendations (Box 1) are designed to provide a robust framework for embedding improvement methodology as a core competence for all doctors.
BOX 1 Key recommendations from the Academy of Medical Royal Colleges
-
• A progressive curriculum in quality improvement activity should underpin all training stages of a doctor, building capability and leadership, and a foundation for ongoing lifelong learning and implementation
-
• Quality improvement should be integral to all clinical and non-clinical job descriptions and appraisal, and career recognition given for quality improvement achievements
-
• Patient involvement should be advocated and included at every level with recognition that this may be achieved in a variety of ways
-
• All trainees, and their trainers and multi-professional teams with which they work, should have access to quality improvement training
-
• Quality improvement activity should be supported at all levels, locally, regionally and by Royal Colleges and specialist societies in the form of enabling ‘core’ quality improvement support aligned with existing educational structures to permit expert facilitation, coaching, mentoring and interprofessional learning, with protected time to undertake it
-
• Health and social care executives and non-executives should model best practice quality improvement approaches and create an open culture with the focus on learning, ownership and accountability rather than reprimand, as this facilitates a quality improvement culture
-
• A repository of quality improvement activity should be established to empower learning and sharing
-
• A stakeholder group should be established under the auspices of a national body such as the Academy of Medical Royal Colleges to align planning in quality improvement activity by key stakeholders and topic experts for the long-term, that is applicable to everybody, and to contribute to improving patient outcomes through education, training, research and collaboration
(Academy of Medical Royal Colleges 2016: pp. 8–9)
This learning will be augmented throughout core and higher training in preparation for senior leadership of QI work as consultants. Current consultants who are trainers should familiarise themselves with the expectations for students and trainees at different stages in order to provide appropriate support. This may also involve trainers undertaking additional training in order to feel confident in providing such support.
The report also suggests that each organisation in healthcare should have a local leader responsible for quality who would lead efforts to build capability and capacity. This would need to take account of the training environment and adapt existing learning opportunities to include an element of QI training. There is also a need to incorporate improvement education into the research agenda, building on the work of the Institute of Medicine (2001). It will be essential to involve patients and carers at every stage of the process, as they have a significant and diverse contribution to make.
One aim of the Academy's work has been to share best practice and map the resources that are available to clinicians to develop QI competencies. These have been gathered together on an informative, although not exhaustive, interactive map (AoMRC 2016b). They also developed a series of illustrative case studies (AoMRC 2016c).
For all of this work to happen there needs to be organisational support at every level, including strategic direction from a slew of national bodies. Psychiatrists will have a pivotal role in ensuring that this is translated from policy into practice within mental health services, so that the next generation of psychiatrists has the necessary tools to be active improvers.
In modern healthcare, it is essential for psychiatrists to supplement specialist medical expertise, applicable to one-to-one interactions between clinicians and patients, with knowledge and skills to improve the quality of care and to work safely and effectively both within a team and across the healthcare system (Reference Jones and WoodheadJones 2015). Learning resources about QI are increasingly being made available through the workplace, with numerous additional offerings available free or at low cost (Box 2).
BOX 2 Resources
1000 Lives Plus (www.1000livesplus.wales.nhs.uk)
The national improvement service for NHS Wales, helping organisations and individuals to deliver high-quality and safe healthcare; offers free online QI resources, and educators can access QI education programmes.
BMJ Quality (www.quality.bmj.com)
Offers tools to help users become involved in QI; the full platform is accessible on subscription. Subscribers may submit their initiatives in the open-access journal BMJ Quality Improvement Reports.
East London NHS Foundation Trust (qi.elft.nhs.uk)
Information, educational materials and tools are freely available on its QI microsite.
Health Foundation (www.health.org.uk)
An independent charity whose focus is improving health and healthcare the UK; its website includes articles relevant to QI, as well as guides summarising key principles.
Institute for Healthcare Improvement (IHI) (www.ihi.org)
An independent, not-for-profit organisation that seeks to improve health and healthcare around the world. Its Open School encourages the development of local face-to-face networks (‘chapters’) where interprofessional groups learn about and undertake QI work in their institutions. The IHI site hosts free learning materials, and Open School learning modules accessible to subscribers.
King's Fund (www.thekingsfund.org.uk)
An independent charity working to improve health and care in England, the King's Fund provides access to materials about QI, including articles, briefings and reports relevant to the NHS.
NHS England Sustainable Improvement Team (www.nhsiq.nhs.uk)
Formerly NHS Improving Quality, this is a department of NHS England supporting improvement across the organisation. Resources have been created to share improvement and change expertise.
NHS Scotland Quality Improvement Hub (www.qihub.scot.nhs.uk)
Supports healthcare workers in Scotland to develop their improvement knowledge and skills; learning resources, including learning modules aimed at clinical staff, are available in the website's ‘Knowledge Centre’.
MCQs
Select the single best option for each question stem
-
1 In the 1920s, methods of understanding variation to drive improvements in industry were developed by:
-
a Jerzy Neyman
-
b William Deming
-
c Walter Shewhart
-
d Ronald Fisher
-
e Donald Berwick.
-
-
2 Regarding clinical audit and quality improvement (QI):
-
a QI and audit rely on repeated collection of system performance data
-
b clinical audit involves making changes to deliver improvements
-
c QI involves making changes to deliver improvements
-
d QI involves staff in a discrete part of the system
-
e clinical audit involves staff in a discrete part of the system.
-
-
3 In a typical technical challenge:
-
a skills to tackle the challenge exist within the system
-
b resolution is difficult to define
-
c further challenges are revealed when solutions are attempted
-
d attitudes, values and behaviours need to adapt
-
e those involved in the work develop solutions.
-
-
4 The Model for Improvement does not involve:
-
a determining what should be accomplished
-
b deciding how improvements will be recognised
-
c generating change ideas that can be tested
-
d establishing effectiveness using aggregated data retrospectively
-
e making predictions based on real-time data.
-
-
5 The MUSIQ tool is likely to be least effective when used by:
-
a a QI mentor, working with a project team
-
b project team, identifying their own needs
-
c clinical leader, deciding what QI support is needed for an initiative
-
d non-clinical manager, deciding what support needed for a QI initiative
-
e an organisation, determining their QI capability.
-
MCQ answers
| 1 | c | 2 | e | 3 | a | 4 | d | 5 | e |








eLetters
No eLetters have been published for this article.