Posterior interosseous neuropathy resulting from compression in the radial tunnel, also known as supinator syndrome, is usually diagnosed by clinical assessment and electrodiagnostic testing.Reference Cifu 1 , Reference Preston and Shapiro 2 In the past decade, high-resolution ultrasonography has been applied to aid the diagnosis of entrapment neuropathies such as carpal tunnel syndrome and cubital tunnel syndrome.Reference Kowalska 3 In this case report, we present how dynamic ultrasonography was used to assist in the diagnosis and treatment of supinator syndrome.
A 58-year-old right-handed man came to our clinic complaining of progressive left finger drop over the previous 3 to 4 months. He had no history of trauma or repetitive upper arm activities, nor did he have any neck, shoulder, or upper limb pain. His medical history included type 2 diabetes mellitus, hypertension, and dyslipidemia. Family history yielded no relevant details. On physical examination, he had full muscle strength for flexion in the left fingers and wrist; however, the muscle strength for extension of the left wrist was grade 4 with radial deviation and the muscle strengths for extension of the left second, third, fourth, and fifth fingers were grades 2, 2, 0, and 0, respectively. No obvious muscle atrophy or sensory impairment was found. The deep tendon reflexes of the biceps, brachioradialis, and triceps were normal. The Spurling test was negative.
Cervical spine X-ray and magnetic resonance imaging showed mild foraminal narrowing at the left C3/4 level, mild spinal stenosis at the C3-T1 levels without obvious root or cord compression, and imaging of the roots showed no signs of an inflammatory disorder. Electrodiagnostic testing revealed normal conduction velocity with low-amplitude compound muscle action potential without conduction block between forearm and elbow in a left radial motor study, and superficial radial sensory tests were normal. In addition, no evidence of conduction block was found in other arm nerves. A blood test showed normal liver and renal function, but the glycated hemoglobin level was 8.8%. The patient admitted that he did not take oral hypoglycemic agents regularly.
Ultrasonography was performed with an 18-MHz linear array transducer (Acuson S2000 Ultrasound System; Siemens, Munich, Germany). The probe was placed in parallel to the posterior interosseous nerve (PIN) and the PIN was examined with the forearm in the pronated and supinated positions, bilaterally, as shown in Figure 1. Compared with the right side, the left PIN showed marked compression and angulation by the superficial head of the supinator muscle in the supinated position. In-plane ultrasound-guided PIN hydrodissection was performed with a mixture of 0.5 ml 50% glucose water and 4.5 ml 1% xylocaine (Figure 2). The patient was also instructed to take oral hypoglycemic agents regularly and avoid strenuous or repetitive forearm activities.
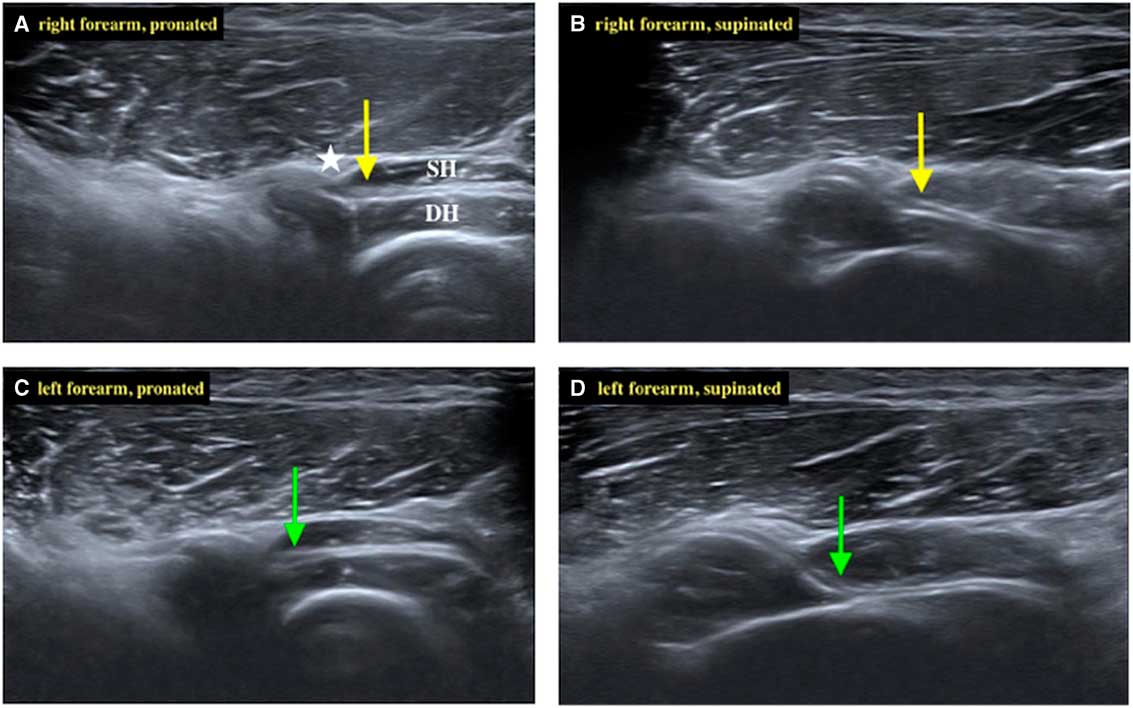
Figure 1 The posterior interosseous nerve (PIN; arrow) penetrated between the superficial head (SH) and deep head (DH) of the supinator muscle. The arcade of Fröhse (asterisk) was depicted clearly under ultrasound. (A) The right PIN (yellow arrow) of the forearm in the pronated position. (B) While the right forearm was supinated, the right PIN remained relatively straight. (C) The left PIN (green arrow) of the forearm in the pronated position. (D) While the left forearm was supinated gradually, the left PIN became compressed and angulated.
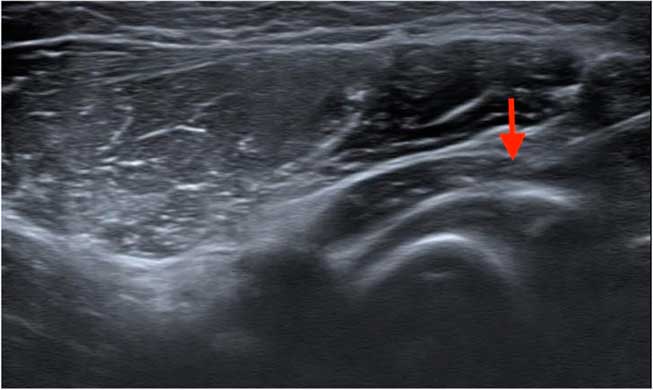
Figure 2 Hydrodissection was performed by placing a solution surrounding the left posterior interosseous nerve through the needle tip (red arrow).
After treatment, the patient went abroad; hence, follow-up was carried out a month and a half later. He received no further treatment during this period. On manual muscle test, the extension strengths of the left second and third fingers had improved by at least one grade and trace movement was noted in the left fourth and fifth fingers.
For many years, clinical assessment and electrodiagnostic testing formed the diagnostic basis for peripheral entrapment neuropathies.Reference Cifu 1 However, most cases of supinator syndrome constitute pure axonal loss lesions with no demonstrable conduction block between the forearm and elbow sites, as in this case.Reference Preston and Shapiro 2 Even if a conduction block exists, this does not indicate the exact site of entrapment.
Recently, high-resolution ultrasonography has been gaining popularity in assessing peripheral entrapment neuropathies. It has been reported that when PINs are found to be compressed at the arcade of Fröhse, they show a proximal swelling to up to 2 to 3.3 mm, compared with 1.1 to 1.3 mm in healthy subjects.Reference Bodner, Harpf, Meirer, Gardetto, Kovacs and Gruber 4 , Reference Djurdjevic, Loizides, Löscher, Gruber, Plaikner and Peer 5 However, considerable statistical error exists while measuring PIN diameter because of its small size and its normally tapering shape.Reference Dong, Jamadar and Robertson 6 In our case, the PIN did not show marked swelling, but there was obvious compression and angulation by the superficial head of the supinator muscle. Similar findings were reported by Kowalska et al.Reference Kowalska 3 We agree with the authors that PIN angulation might be a better ultrasound diagnostic criterion instead of PIN proximal swelling for diagnosing supinator syndrome.
Although the most common site of entrapment in supinator syndrome is the arcade of Fröhse, there are actually as many as five possible sites of compression in a short distance of the radial tunnel: (1) the fibrous bands of the anterior radiocapitellar joint between the brachialis and brachioradialis; (2) the recurrent radial vessels that fan out at the radial neck, also called the “leash of Henry”; (3) the leading edge of the extensor carpi radialis brevis; (4) the arcade of Fröhse; and (5) the supinator muscle itself.Reference Dang and Rodner 7 Ultrasonography may assist in localizing the exact site of compression and excluding external compression by secondary causes.Reference Djurdjevic, Loizides, Löscher, Gruber, Plaikner and Peer 5 Furthermore, real-time hydrodissection can be performed accurately to relieve the compression.
Although limited high-quality data exist, most of the current research favors the effectiveness of hydrodissection in treating carpal tunnel syndrome, ulnar neuropathy at the elbow and wrist, and meralgia paresthetica. Regarding complications, the most common complication of hydrodissection is inadvertent intraneural injection. Two studies indicated 16% to 17% intraneural injection rates with ultrasound guidance when performing presurgical brachial plexus block and sciatic nerve block. Nevertheless, none of the patients showed residual postoperative motor or sensory deficit, indicating the safety of the procedure.Reference Cass 8 Therefore, we believe that ultrasound-guided hydrodissection for supinator syndrome may be a safe and likely effective alternative to invasive surgery. Further research is needed to verify this postulation.
In conclusion, adding dynamic high-resolution ultrasonography examination to clinical assessment and electrodiagnostic testing can offer valuable information regarding diagnosis, intervention, and further activity modification for supinator syndrome.
Disclosures
The authors have nothing to disclose.




