Percutaneous device closure is a form of interventional cardiac catheterisation that may be used for the treatment of CHD. Reference Baumgartner, De Backer and Babu-Narayan1 This procedure is an attractive alternative to open-heart surgery because of its shorter hospital stay, faster return to daily life, better cosmetic outcomes, and fewer complications. Reference Quek, Hota, Tai, Mujumdar and Tok2
Percutaneous device closure is a form of interventional cardiac catheterisation that is the first-line treatment for most atrial septal defects because of its well-documented efficacy and minimal morbidity. Reference Mylonas, Ziogas and Evangeliou3 Percutaneous closure of an atrial septal defect is performed via the femoral vein under local anaesthesia in an alert state in adults. Reference Baumgartner, De Backer and Babu-Narayan1,Reference Mylonas, Ziogas and Evangeliou3
The fear of the interventional cardiac catheterisation itself, the discomfort caused by catheter insertion, and the unfamiliar environment of the cardiac catheterisation laboratory can act as stressors and cause anxiety. Reference Werner, El Louali, Fouilloux, Amedro and Ovaert4 Furthermore, during interventional cardiac catheterisation, patients undergoing the procedure in an awake state without sedation experience extreme stress, such as anxiety or fear, as they can hear various monitor sounds, communicate with the procedure team, and follow the progress of the procedure. Reference Jeong and Kang5
The anxiety caused by these factors alters the patient's hypothalamic–pituitary–adrenal axis and stimulates the autonomic nervous system, resulting in physiological responses in the body, including increased pulse, blood pressure, and secretion of stress hormones. Reference Lieber, Bose and Zhang6 Therefore, it is necessary to apply appropriate interventions to help patients undergo the procedure comfortably.
Relaxation therapies, such as music therapy, are commonly used as intervention methods to reduce anxiety associated with invasive procedures, such as interventional cardiac catheterisation. Reference Lieber, Bose and Zhang6,Reference Bradt and Dileo7 Music therapy – a low-cost therapy with relatively few side effects, can reduce anxiety, relieve tension, and activate the parasympathetic nervous system to lower stress responses. Reference Lieber, Bose and Zhang6,Reference Witte, Spruit, Hooren, Moonen and Stams8 Accordingly, music therapy for patients with heart disease in the setting of interventional cardiac catheterisation procedures could be clinically helpful in relieving anxiety and the effects of the autonomic nervous system. However, there is no consistent evidence. Reference Lieber, Bose and Zhang6,Reference Bradt and Dileo7 The effects of music therapy on physiologic variables are complex and may vary depending on the patient’s characteristics; thus, a closer examination is needed. Moreover, it is essential to verify that these variables modulate autonomic nervous system effects.
Therefore, music therapy was applied in this study during interventional cardiac catheterisation procedures in patients with atrial septal defects, to evaluate the effect of music therapy on the response to anxiety, heart rate variability, and stress hormone levels.
Materials and methods
Study design and participants
This study was a pre- and post-test randomised controlled trial. The participants were randomly divided into experimental and control groups. Outcome variables were assessed at baseline (pre-test), immediately before catheter insertion (mid-test), and at the end of the intervention (post-test).
A total of 131 patients who underwent percutaneous closure of an atrial septal defect during hospitalisation at the Samsung Medical Center were assessed for eligibility. Patients between the ages of 20 and 70 years who could communicate and had read and completed the consent form and questionnaire were included. Exclusion criteria were as follows: those with hearing impairment, significant cognitive impairment, anxiety, psychosis, or personality disorder in their medical record; those taking hypnotics or anxiolytics; and those taking drugs that affect the autonomic nervous system (β-blockers, diabetes drugs, etc.). Reference Jandackova, Scholes, Britton and Steptoe9
The randomisation sequence was created with the R software random number generator using the permuted block design at a 1:1 allocation ratio to the experimental or control group after admission for interventional cardiac catheterisation. Reference Rosenberger and Lachin10 The calculation of the sample size was based on a study by Park et al, Reference Park and Kim11 with the following assumptions concerning a repeated measure analysis of variance for the primary endpoint with G*power 3.1 software: estimated effect (f) 0.18, a significance level of 5%, and power of 95%. These assumptions resulted in a minimum sample size of 82 participants. Thus, considering dropouts, the target sample size was 94 participants; 47 participants were recruited for each group.
Measurements
State anxiety
State anxiety was measured using the short version of the State-Trait Anxiety Inventory, a 6-item questionnaire developed from the 20-item State-Trait Anxiety Inventory. Reference Marteau and Bekker12 The short State-Trait Anxiety Inventory has been psychometrically tested and found to be reliable with the 20-item state anxiety (r = 0.90–0.95). Reference Bayrampour, McDonald, Fung and Tough13 The total scores ranged from 6 to 24, and higher scores indicated a more severe level of anxiety. Reference Marteau and Bekker12 For this study, Cronbach’s α was 0.91.
Numerical rating scale for anxiety
Participants rated their anxiety levels on a numerical rating scale, which ranged from 0 (no anxiety) to 10 (severe anxiety) before and during the interventional cardiac catheterisation. The numerical rating scale for anxiety was psychometrically tested and found to be reliable (r = 0.60). Reference Williams, Morlock and Feltner14
Salivary cortisol level
All salivary cortisol samples were taken on the procedure day by a trained study manager under the supervision of a specialist in the laboratory. All samples were collected from 07:30 to 10:00 am. Salivary cortisol levels were measured using a commercial kit (ER HS Salivary Cortisol, Salimetrics; Carlsbad, CA, USA) according to the manufacturer’s protocol (including sampling step). 15 The mean values of duplicated data were used to represent the measured values. Sensitivity and intra- and inter-assay coefficients of variation were <0.007 µg/dL, 7%, and 9.3%, respectively. Reference Miller, Plessow, Rauh, Groschl and Kirschbaum16
Heart rate variability
Heart rate variability recordings were obtained for 5 min using an SA-3000P device (Medicore Co., Seoul, Korea). All participants attached electric patches to both wrists and their left ankles and remained in a relaxed supine position. We collected data on the day of the procedure between 07:30 and 10:00 a.m. to control for circadian changes in heart rate variability. The room temperature during data collection was 23–25°C. Heart rate variability analysis was performed using heart rate variability methodological standards. 17,Reference Shaffer and Ginsberg18
For the frequency domain heart rate variability indices, power within the 0.04–0.15 Hz range was considered the low-frequency band, whereas frequencies 0.15–0.4 Hz were defined as the high-frequency band. Reference Shaffer and Ginsberg18 The high-frequency component mainly reflected parasympathetic activity, whereas the ratio of low to high frequency reflected sympathetic activity and sympathovagal balance. Reference Shaffer and Ginsberg18 For time-domain analysis, we used the standard deviation of 2-minute means for all R-to-R intervals during the entire recording, root-mean-squares of differences between adjacent intervals, and percentage of successive RR-interval differences ≥50ms. These parameters were used to express parasympathetic activity. Reference Shaffer and Ginsberg18
Music intervention
Music that relaxes, such as Korean traditional music, classical music, new-age ballads, and religious music (e.g., Korean gospel hymns and Buddhist music), were stored in genre and selected according to the patient's preference.10 MP3 players and headsets were used for music therapy. Headsets were tested before the procedure to ensure that patients did not have problems following the medical personnel's instructions during the procedure, and noise levels ranged from 60 to 70 dB. Reference Witte, Spruit, Hooren, Moonen and Stams8,Reference Argstatter, Haberbosch and Bolay19 Music therapy was performed for 20 minutes in the waiting room before the procedure, and 60 minutes in the catheterisation room, from the start to the end of the procedure. This resulted in a period of approximately 80 minutes. A licensed music therapist performed music interventions for all patients to ensure consistent therapy.
The data collection procedures used in this study were as follows:
On the day of the interventional cardiac catheterisation, the experimental group arrived in the waiting room 20 minutes before the start of the procedure, and a pre-test was conducted. Next, the experimental group listened to the selected music while they waited. After 20 minutes, each patient was moved to the cardiac catheterisation laboratory in a treatment bed while listening to the music. Interventional cardiac catheterisation was initiated after the middle test. During catheterisation, the patients continued to listen to the music. Post-test measurements were assessed shortly after the interventional cardiac catheterisation was completed, and the catheter was removed (Fig 1).
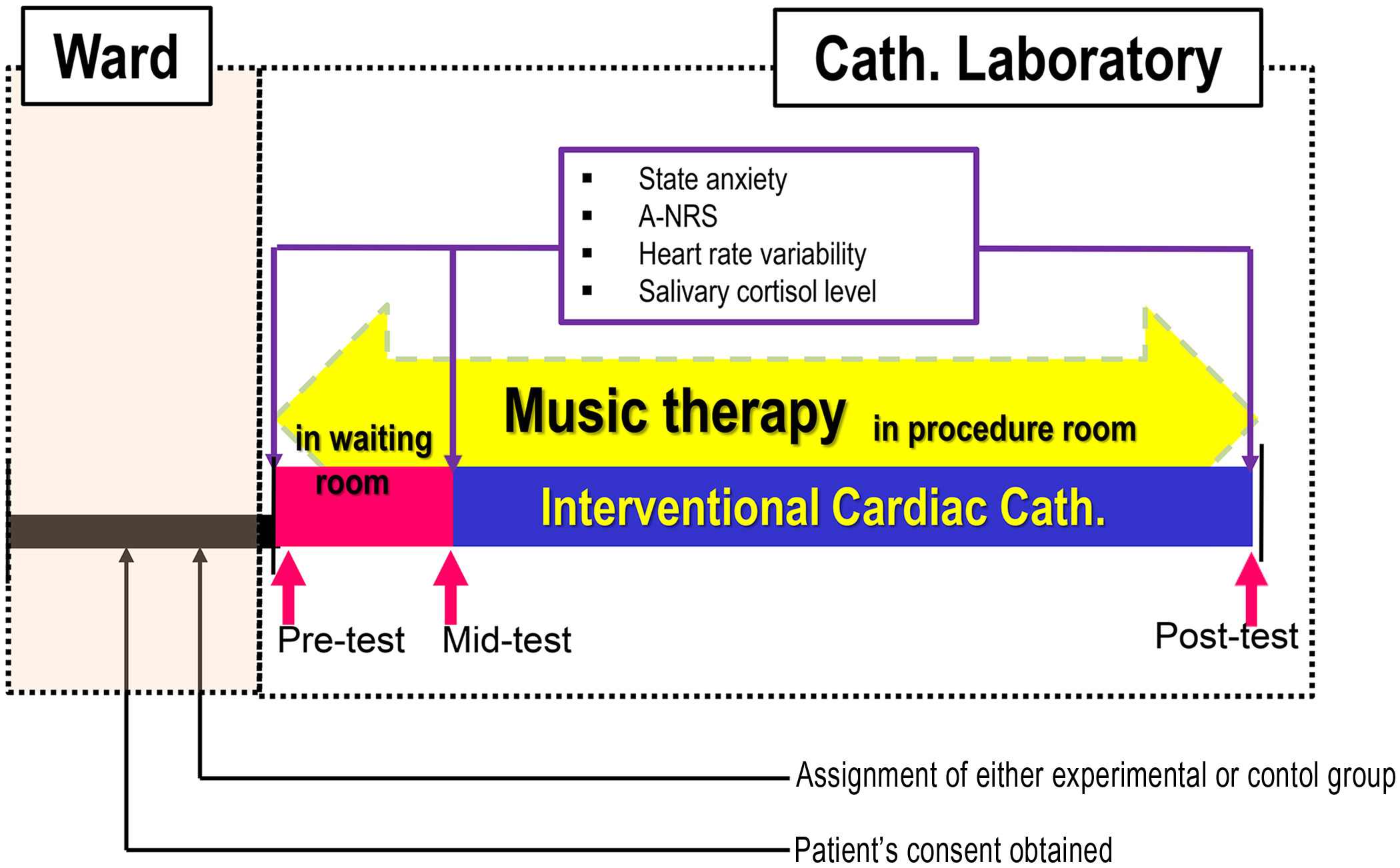
Figure 1. Procedures and data assessment. Cath.=catheterisation; A-NRS=anxiety-numerical rating scale.
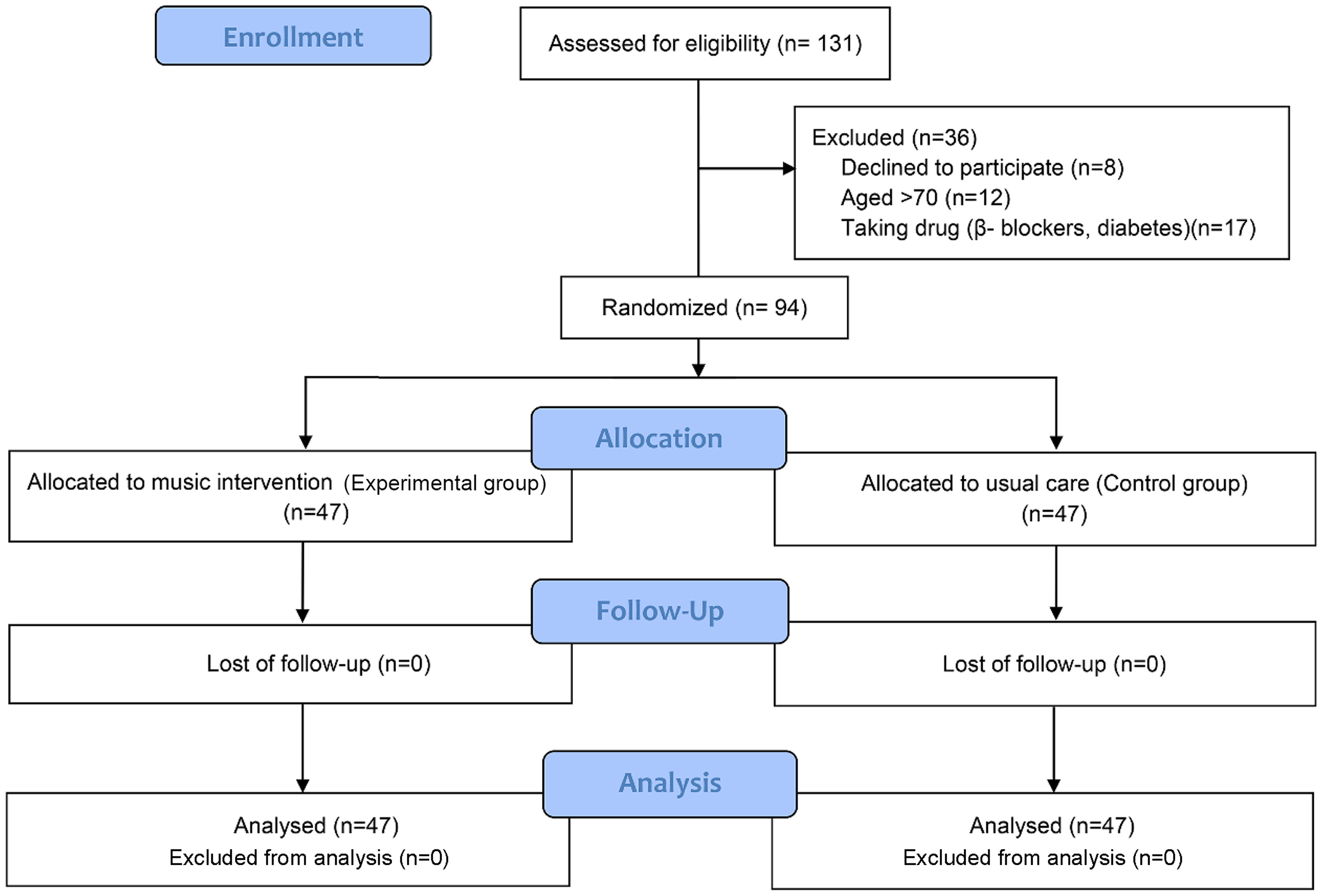
Figure 2. Flow chart showing the two-group progression through a randomised trial.
For the control group, music therapy was not applied, and pre-, mid-, and post-test evaluations were conducted at the same time as the experimental group. A trained nurse who worked in the cardiac catheterisation laboratory performed the pre-, mid-, and post-tests for all patients.
Statistical analysis
Data were analysed using IBM SPSS Statistics for Windows, version 27 (IBM Corp., Armonk, NY, USA). Group differences in the general and clinical characteristics were assessed using the chi-square test for categorical variables and the t-test or Mann–Whitney U-test for continuous variables. The reliability of the instrument was tested using Cronbach’s α. We used repeated-measures analysis of variance between participants (experimental versus control group) and within participants (pre-, mid-, and post-test), and controlled for age and sex as covariates. The Greenhouse–Geisser correction was used when Mauchly’s test of sphericity was violated. The level of significance was set at p < 0.05.
Results
Participant characteristics
Of the 131 patients who were admitted with the atrial septal defect for device closure, eight declined to participate in the study, 12 were over the age of 70, and 17 patients who took β-blockers or diabetic medicines were excluded. Using R software, 94 eligible patients were assigned to either the experimental (n = 47) or control (n = 47) groups. All 94 patients completed the study without dropping out. Figure 2 provides a detailed flow chart of the participants’ progress throughout the study.
The mean age of patients was 45.40 (±16.04) years in the experimental group and 47.26 (±13.83) years in the control group; 66% of the patients in each group were female. There were no statistically significant baseline differences between the two groups regarding demographic and clinical variables, levels of anxiety, cortisol levels, or heart rate variability measures (Table 1).
Table 1. Participants’ characteristics (n = 94)
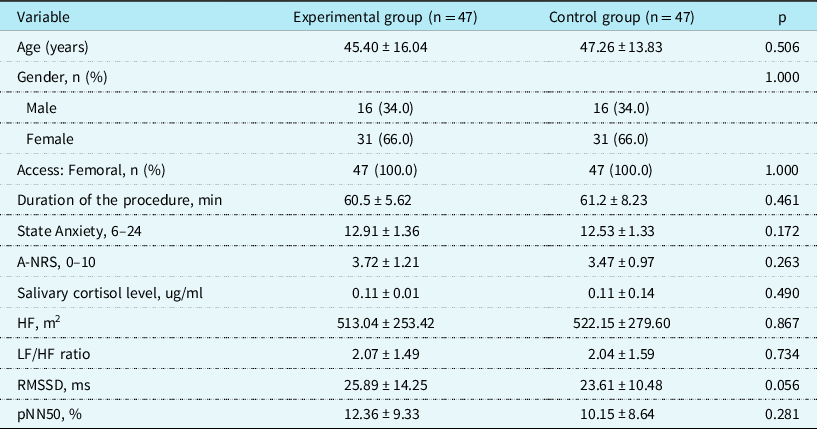
Data are expressed as mean ± standard deviation; A-NRS, anxiety-numerical rating scale; HRV, heart rate variability; LF, low-frequency component; HF, high-frequency component; RMSSD, root-mean-square of successive NN intervals; pNN50, proportion of successive RR intervals ≥ 50 ms in relation to the total RR intervals.
Anxiety
Regarding the state anxiety score, statistically significant differences were observed between the groups (F = 7.17, p < 0.001), time (F = 10.25, p = 0.002), and group-by-time interaction (F = 31.42, p < 0.001). Both groups had significantly lower state anxiety scores in the pre-test compared to the mid-test assessment (experimental group 12.91 ± 1.36 versus 13.92 ± 1.93, p < 0.001; control group 12.53 ± 1.33 versus 15.06 ± 2.08, p < 0.001). Both groups also had significantly lower post-test scores compared to mid-test scores (experimental group 11.89 ± 2.09 versus 13.92 ± 1.93, p < 0.001; control group 13.53 ± 1.53 versus 15.06 ± 2.08, p < 0.001). However, the state anxiety scores in the experimental group were significantly lower than those of the control group at the mid-test (13.92 ± 1.93 versus 15.06 ± 2.08, p < 0.001) and post-test (11.89 ± 2.09 versus 13.53 ± 1.53, p < 0.001) (Table 2).
Table 2. Comparison of anxiety, salivary cortisol level, and heart rate variability between the two groups (n = 94)
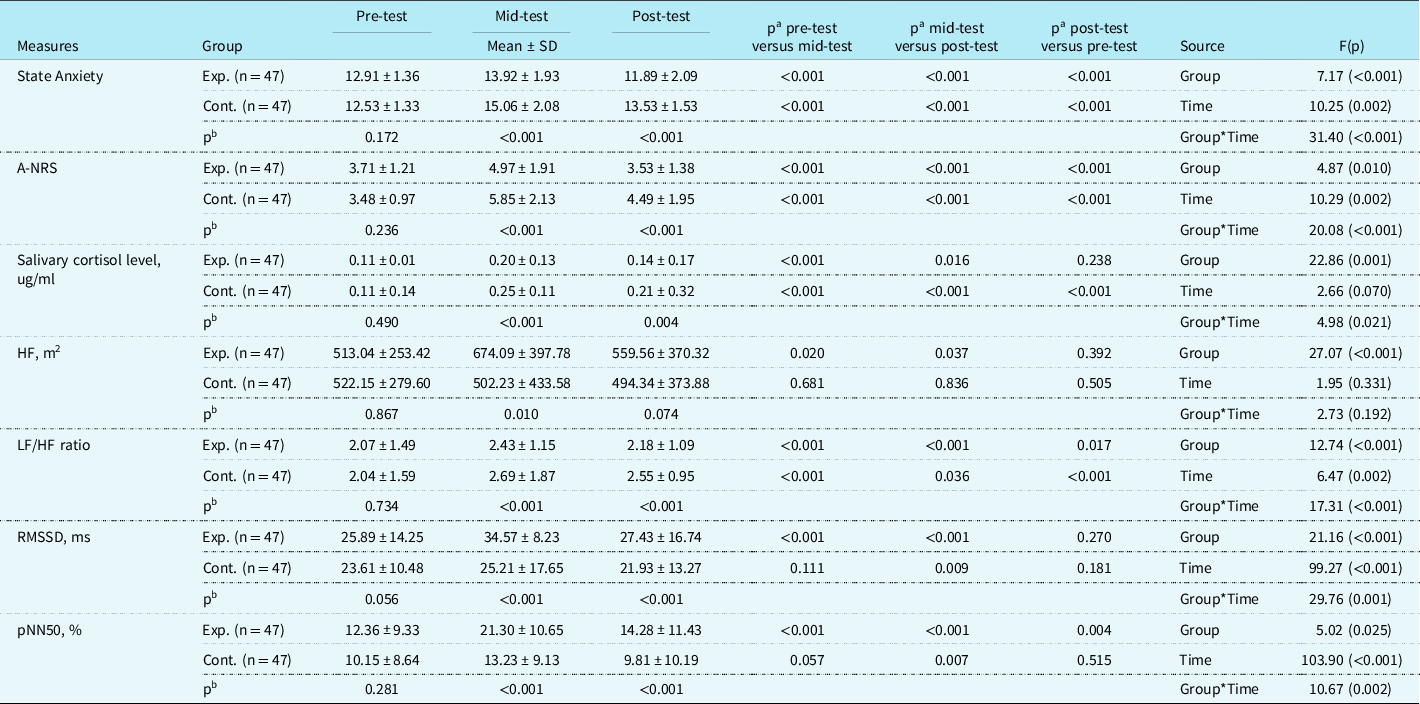
Data are expressed as mean ± SD, standard deviation; vs., versus; pa, value for time effect; pb, value for group effect; Exp., experimental group; Cont., control group; A-NRS, anxiety-numerical rating scale; HF, high-frequency component; LF, low-frequency component; RMSSD, root-mean-square of successive NN intervals; pNN50, proportion of successive RR intervals ≥ 50 ms in relation to the total RR intervals.
The numerical rating scale for anxiety scores also showed trends similar to state anxiety scores. There were significant differences between the groups (F = 4.87, p = 0.010), time (F = 10.29, p = 0.002), and group-by-time interaction (F = 20.08, p < 0.001). In the numerical rating scale for anxiety scores, both groups had significantly higher scores in the mid-test compared to the pre-test assessment (experimental group 4.97 ± 1.91 versus 3.71 ± 1.21, p < 0.001; control group 5.85 ± 2.13 versus 3.48 ± 0.97, p < 0.001). Both groups also had significantly lower post-test scores compared to mid-test scores (experimental group 3.53 ± 1.38 versus 4.97 ± 1.91, p < 0.001; control group 4.49 ± 1.95 versus 5.85 ± 2.13, p < 0.001). Similarly, the scores of the experimental group were significantly lower than those of the control group at the mid-test (4.97 ± 1.91 versus 5.85 ± 2.13, p < 0.001) and post-test (3.53 ± 1.38 versus 4.49 ± 1.95, p < 0.001) (Table 2).
Salivary cortisol level
Statistically significant differences were observed in salivary cortisol levels between the groups (F = 22.86; p < 0.001) and group-by-time interaction (F = 4.98, p = 0.021), although there was no significant difference over time (F = 2.66, p = 0.070). Both groups had significantly lower cortisol levels in the pre-test compared to the mid-test assessment (experimental group 0.11 ± 0.01 versus 0.20 ± 0.13, p < 0.001; control group 0.11 ± 0.14 versus 0.25 ± 0.11, p < 0.001). Both groups also had significantly lower post-test cortisol levels compared to those at the mid-test (experimental group 0.14 ± 0.17 versus 0.20 ± 0.13, p = 0.016; control group 0.21 ± 0.32 versus 0.25 ± 0.11, p < 0.001). However, the experimental group had significantly lower cortisol levels than those of the control group at mid-test (0.20 ± 0.13 versus 0.25 ± 0.11, p < 0.001) and post-test (0.14 ± 0.17 versus 0.21 ± 0.32, p = 0.004) (Table 2).
Heart rate variability
Statistically significant differences were observed between the groups (F = 27.07, p < 0.001) in the high-frequency component, but none between the time (F = 1.95, p = 0. 331) and group-by-time interaction (F = 2.73, p = 0.192) (Table 2). In the experimental group, the high-frequency component significantly increased from the pre-test scores (513.04 ± 253.42) to the mid-test scores (674.09 ± 397.78) (p < 0.020) and decreased to the post-test scores (559.56 ± 370.32) (p = 0.037). Contrastingly, the control group had decreased from the pre-test (522.15 ± 279.60) to post-test scores (502.23 ± 433.58) (p = 0.681) and decreased to the post-test scores (494.34 ± 373.88) (p = 0.505). Furthermore, the scores in the experimental group were higher than those in the control group at mid-test (674.09 ± 397.78 versus 502.23 ± 433.58, p < 0.010) and post-test (559.56 ± 370.32 versus 494.34 ± 373.88, p = 0.074) (Table 2). There were significant differences in the low-and high-frequency component ratios between the groups (F = 12.74, p < 0.001), time (F = 6.47, p = 0.002), and group-by-time interaction (F = 17.31, p < 0.001). Both groups had significantly lower scores in the low-/high-frequency component ratio in the pre-test than in the mid-test assessment (experimental group 2.07 ± 1.49 versus 2.43 ± 1.15, p < 0.001; control group 2.04 ± 1.59 versus 2.69 ± 1.87, p < 0.001). Both groups also had significantly lower post-test scores compared to mid-test scores (experimental group 2.18 ± 1.09 versus 2.43 ± 1.15, p < 0.001; control group 2.55 ± 0.95 versus 2.69 ± 1.87, p = 0.036). However, the ratio scores in the experimental group were significantly lower than those of the control group at the mid-test (2.43 ± 1.15 versus 2.69 ± 1.87, p < 0.001) and post-test (2.18 ± 1.09 versus 2.55 ± 0.95, p < 0.001) (Table 2). The root-mean-squares of differences between adjacent intervals demonstrated significant differences between the groups (F = 21.16, p < 0.001), time (F = 99.27, p < 0.001), and group-by-time interaction (F = 27.76, p < 0.001). Both groups had higher scores in the root-mean-squares of differences between adjacent intervals in the mid-test compared to the pre-test assessment (experimental group 25.89 ± 1.49 versus 34.57 ± 8.23, p < 0.001; control group 23.61 ± 10.48 versus 25.21 ± 17.65, p = 0.111). However, both groups had significantly lower post-test scores compared to mid-test scores (experimental group 34.57 ± 8.23 versus 27.43 ± 16.74, p < 0.001; control group 25.21 ± 17.62 versus 21.93 ± 13.27, p = 0.009). The scores in the experimental group were significantly higher than those in the control group at mid-test (35.57 ± 8.23 versus 25.21 ± 17.65, p < 0.001) and post-test (27.43 ± 16.74 versus 21.93 ± 13.27, p < 0.001) (Table 2). There were significant differences in the percentage of successive RR-interval differences ≥50ms between the groups (F = 5.02, p = 0.025), time (F = 103.90, p < 0.001), and group-by-time interaction (F = 10.67, p = 0.002). Both groups had a significantly higher percentage of successive RR-interval differences ≥50ms in the mid-test compared to the pre-test assessment (experimental group 12.36 ± 9.33 versus 21.30 ± 10.65, p < 0.001; control group 10.15 ± 8.64 versus 13.23 ± 9.13, p = 0.057). However, both groups had significantly lower post-test scores compared to mid-test scores (experimental group 21.30 ± 10.65 versus 14.28 ± 11.43, p < 0.001; control group 13.23 ± 9.13 versus 9.81 ± 10.19, p = 0.007). Additionally, the percentage in the experimental group was significantly higher than that of the control group at mid-test (21.30 ± 10.65 versus 13.23 ± 9.13%, p < 0.001) and post-test (14.28 ± 11.43 versus 9.81 ± 10.19%, p < 0.001) (Table 2).
Discussion
The results of this study showed that both groups had worsened mid-test anxiety compared to the pre-test measurements. The experimental group had less overall anxiety at the post-test compared to the control group, suggesting that this relaxation intervention may have reduced anxiety by the end of the procedure. These results were consistent with findings demonstrating a significant reduction in anxiety scores when music therapy was applied to coronary angiogram patients Reference Park and Kim11 and patients under spinal anaesthesia during surgery. Reference Jeong and Kang5 Another study by Nilsson showed no significant reduction in anxiety in cardiac surgery patients who were allowed to listen to music selected in advance by the researchers, Reference Nilsson20 which contradicts our results. However, the results of the study by Nilsson Reference Nilsson21 indicated that the music was selected by the researchers, rather than by the patients; therefore, it may have been considered as noise, which may have made patients more nervous and led to increased psychological discomfort. Considering these results, more effective music interventions can be provided when a patient’s preferred music is played. Reference Witte, Spruit, Hooren, Moonen and Stams8,Reference McCrary and Altenmuller22
The salivary cortisol level was highest at the mid-test and decreased at post-test; however, the difference was not statistically significant. Moreover, the salivary cortisol levels at the mid-test and post-test were significantly lower in the experimental group than in the control group. These results were partially consistent with those reported by Nilsson et al. Reference Nilsson20 and with the findings of a study on patients undergoing surgery under spinal anaesthesia. Reference Jeong and Kang5 It can thus be inferred that the experimental group experienced less stress than the control group while listening to music.
The high-frequency, root-mean-square of successive NN intervals, and proportion of successive RR intervals≥50ms, components reflecting cardiac parasympathetic activity in heart rate variability, were all highest at mid-test rather than at pre-test and then decreased at post-test. Moreover, the root-mean-square of successive NN intervals and the proportion of successive RR intervals ≥ 50 ms in the mid-test and post-test were significantly higher in the experimental group than in the control group. The low-/high-frequency component ratio was also highest at the mid-test rather than at the pre-test and then significantly decreased at post-test. However, the low-frequency component/high-frequency component ratios in the mid-test and post-test were significantly lower in the experimental group than in the control group. Thus, there appeared to be an increase in parasympathetic activity and a decrease in sympathetic activity in the experimental group compared to the control group, which represented an effective reduction of the stress response. 17 These findings were consistent with the results of increased parasympathetic tone after music therapy in various disease groups such as mothers of preterm infants, Reference Ribeiro, Alcântara-Silva and Oliveira23 hospitalised women with high-risk pregnancies, Reference Teckenberg-Jansson, Turunen and Pölkki24 combined cerebrovascular disease and dementia. Reference Kurita, Takase and Okada25 From these findings, music therapy demonstrated an ability to modulate autonomic tone, Reference McCrary and Altenmuller22 which may be a critical central mechanism influencing physical and mental health benefits. Reference McCrary and Altenmuller22 However, these mechanisms are complex and not yet clear. Furthermore, the results of Kume et al., Reference Kume, Nishimura and Mizuno26 which showed no significant difference in autonomic tone after music therapy in normal participants, contradicted the results of this study. Different results of previous studies can be derived depending on the study design, the characteristics of the subjects, and the characteristics of music therapy (frequency, intensity, time, and type). In addition, the parasympathetic tone was significantly increased in the mid-test not only in the experimental group but also control group in this study. This may be a self-regulation activity to balance autonomic tone in extreme stress situations, Reference McCrary and Altenmuller22 but the evidence is also unclear. Therefore, well-designed repeated randomised controlled studies according to subject characteristics may help to further clarify presently different outcomes.
Despite positive outcomes, this study has several limitations. Since the participants in this study were limited to adults recruited from a single tertiary centre, discretion should be exercised when generalising the results to all patients. Furthermore, atrial septal defects are more common in women than in men. Reference Jang, Seo and Moon27 There was a gender imbalance in this study, as 66% of patients were women. This may have affected the results of the study, even though gender was considered as a covariate in the statistical analysis. Third, because this study used patient-selected music and the researchers required informed consent before the study, patients knew that they were going to be evaluated for their anxiety and stress levels and, as such, could have behaved in a particular manner. Known as the Hawthorne effect, it could be a threat to the external validity of qualitative studies because patients could report responses depending on what the researchers were looking for rather than what the patient was experiencing. Reference Trowbridge and Horstman28 Therefore, a double-blinded study that adjusts for the Hawthorne effect is suggested.
Finally, our study did not consider the cost-effectiveness aspect. Furthermore, we tested the short-term or direct stress-reducing effects of music therapy in this study, but not the long-term outcomes. Notably, Gallagher et al. discussed that stress responses in patient undergoing percutaneous coronary intervention put these patients at risk, specifically for increased thrombosis, greater myocardial oxygen demand in a setting with partially compromised oxygen delivery and worse health-related quality of life after the procedure. Reference Gallagher, Trotter and Donoghue29 This is a significant near-term and long-term risk to the patient and patient outcomes. Although patients with atrial septal defects differ from these, they may also be negatively affected by the stress response. At the behavioural level, anxious patients undergoing percutaneous closure of atrial septal defects may adhere to poorer health behaviours, such as lower physical activity, cigarette smoking, and excessive alcohol consumption, which subsequently increases their cardiovascular risk. Reference Karlsen, Matejschek, Saksvik-Lehouillier and Langvik30 Their anxiety may also alter the autonomic nervous system through excessive activation of the hypothalamic–pituitary–adrenal axis and sympathetic nervous system, which may increase the occurrence of atrial tachycardia, atrial tachyarrhythmias, and atrial fibrillation. Reference Carnagarin, Kiuchi, Ho, Matthew and Schlaich31 This is an area that requires further investigation. Therefore, future studies are needed to better understand the specific mechanism(s) of action of music therapy in reducing anxiety and stress and to evaluate its overall role and benefit in medical procedures.
Conclusion
This study provided practical evidence of a reduction in anxiety and stress responses from listening to music preceding interventional cardiac catheterisation. The differences between the groups were sufficient to suggest that listening to music during a cardiac catheterisation may be beneficial.
Acknowledgements
We would like to thank Patricia Moon for English language editing.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation (Lov om medisinsk og helsefaglig forskning), with the Helsinki Declaration of 1975 (as revised in 2008), and have been approved by the institutional committees (Regional Committee for Medical and Health Research Ethics in Samsung Medical Center).







