LEARNING OBJECTIVES
After reading this article you will be able to:
• understand the range of mental disorders encountered among detainees in police custody
• appreciate the evidence base and problems encountered when screening for mental disorders in this population
• recognise the need for a staged approach to screening and assessment of detainees.
Mental disorders are common among people within criminal justice, or correctional, systems but there is less worldwide literature on health and screening in police custody than in prisons, partly owing to methodological difficulties inherent in performing research in the former. Furthermore, what constitutes police custody varies significantly between geographical and jurisdictional entities, as does the organisation, funding, culture and accountability of police forces, making international comparisons difficult. Arrests rates in the USA and in England and Wales show a downward trend but the global picture is unclear as arrest rate data are not available from all jurisdictions.
Scholarly descriptions of mental disorders in police settings date back to the 1970s and 1980s in the USA (Steadman Reference Steadman, Deane and Borum2000) and in the UK (Rix Reference Rix1997). The health and screening of police detainees gained more attention in the 1990s (Robertson Reference Robertson, Pearson and Gibb1996) and there is now a growing international evidence base from the UK (McKinnon Reference McKinnon and Grubin2014; Brooker Reference Brooker, Tocque and Mitchell2018; Samele Reference Samele, McKinnon and Brown2021), France (Chariot Reference Chariot, Beaufrere and Denis2014; Lepresle Reference Lepresle, Vidal and Mairesse2017), Germany (Heide Reference Heide, Stiller and Lessig2012), The Netherlands (Ceelen Reference Ceelen, Dorn and Buster2012), Australia (Baksheev Reference Baksheev, Ogloff and Thomas2012), the USA (Kaba Reference Kaba, Solimo and Graves2015) and Canada (Hoffman Reference Hoffman, Hirdes and Brown2016). Despite methodological variations, studies consistently report a burden of health conditions considerably higher than that encountered in the general population.
In England and Wales in 2009, Lord Bradley published a wide-reaching review of access to services for people with mental health problems and intellectual disability who are in contact with the criminal justice system (the report uses the UK terminology ‘learning disability’ to describe people with intellectual disability) (Bradley Reference Bradley2009). In subsequent years, ‘liaison and diversion’ services have developed in police custody and the lower (magistrates’) courts, with the aim of screening for and addressing the psychiatric and psychological needs of offenders as early as possible in the criminal justice system pathway. This has been operationalised by embedding mental health professionals to screen and signpost detainees according to need (Forrester Reference Forrester and Hopkin2019).
There has also been increased interest in the identification and management of people with neurodevelopmental conditions and in the disproportionate presence of people from Black, Asian and minority ethnic (BAME) backgrounds among people arrested and coming into contact with the police, and how these relate to unmet need among these vulnerable and often hard to reach groups (Samele Reference Samele, McKinnon and Brown2021).
Screening and its relevance to police custody
The method of screening depends on the disease and outcome in question. Public interest in health screening has come to the fore recently in the context of the COVID-19 pandemic, which has highlighted long-held concerns that varying definitions of screening can lead to confusion as to its purpose.
Although mental health screening tools are long established, their utility in police custody where imminent risk is present is uncertain; in such circumstances immediate clinical assessment may be preferred (Hoffman Reference Hoffman, Hirdes and Brown2016; McKinnon Reference McKinnon and Finch2018). Furthermore, the emphasis and purpose of screening differs depending on the viewpoint of the person who is commissioning, performing, interpreting or receiving screening, and the outcomes of interest. Police custody therefore presents opportunities for screening with various aims:
• clinical aims:
◦ the identification of individuals with specific conditions so that they can be offered appropriate assessments and/or interventions
◦ the development of clinical pathways for particular groups of people or conditions
• service-based aims:
◦ needs assessments to inform the delivery of local services
◦ service planning or design
• research aims, such as:
◦ the measurement of the prevalence of specific conditions and their comorbidities
◦ ascertaining the validity and reliability of screening tools
• fulfilling statutory screening requirements (in some jurisdictions).
This article provides an overview of the rationale for screening for various domains of mental disorder within police custody. The bibliographic references pertaining to specific screening tools are contained in the supplementary material available online at https://dx.doi.org/10.1192/bja.2022.25.
Opportunities for screening in police custody
Most screening research in police custody relates to a broad category of psychiatric and mental health-related illnesses and conditions (Wardrop Reference Wardrop, Ranse and Chaboyer2021). This is unsurprising, given that high prevalence rates have been observed in other parts of the criminal justice system, particularly prisons, and the existence of a bi-directional relationship between poor mental health and offending behaviour (Irwin Reference Irwin, Owen, Liebling and Maruna2005). There is also evidence that some police officers (Bell Reference Bell and Eski2016) and some custody healthcare staff (Hurley Reference Hurley, Linsley and Elvins2013) need further support and training to improve their understanding of the needs of detainees with mental disorders.
One criticism of research and policy in this area is that there is a tendency to focus on circumscribed ‘mental disorders’ which are neither homogeneous nor exist in isolation. This has led to calls for a more holistic concept of ‘mental vulnerability’ (Farrugia Reference Farrugia2021).
However, a key clinical aim of screening is to identify severe and life-threatening conditions, and screening that is not diagnosis- or disorder-focused would be likely to seriously limit the effectiveness of this process.
Psychiatric disorders
In Australia, Baksheev et al (Reference Baksheev, Ogloff and Thomas2012) evaluated the Brief Jail Mental Health Screen (BJMHS) and Jail Screening Assessment Tool (JSAT) to identify mental disorders among 150 custody detainees. Compared with a gold standard interview (Structured Clinical Interview for DSM-IV Axis I Disorders; SCID) both tools performed well in identifying serious mental illness (SMI) (with a sensitivity of 84% and 100% respectively) and any Axis I disorder (81% and 99%), but at the expense of high false-positive rates (specificity 60% and 56% respectively for SMI, and 64% for both tools regarding Axis I disorders). Standard custody ‘risk assessment forms’ completed by custody nurses had much lower sensitivity for depressed/suicidal detainees or those with any Axis I disorder.
In The Netherlands, Dorn et al (Reference Dorn, Ceelen and Buster2013) also administered the BJMHS to 248 police detainees and found that just under 40% screened positive, although no comparison was made with a gold standard. Screening positive correlated with having financial difficulties and no permanent address.
The referral of detainees to liaison and diversion services depends on the identification of the need by the police staff or healthcare professional within custody (see also the ‘Special circumstances’ section below). Noga et al (Reference Noga, Walsh and Shaw2015) describe a screening tool for use in police custody to identify those who need a diversionary pathway. The Police Mental Health Screening Questionnaire (PolQuest) has 14 items designed to identify detainees needing diversion to health and social services and its pathway design stratifies between urgent and routine referrals regardless of the availability of liaison and diversion services. PolQuest has not been validated against a gold standard clinical evaluation, but non-psychiatric disorders are outside its scope.
Developmental conditions
Intellectual disability
Some of the earliest research pertaining to mentally vulnerable detainees in police custody emanates from the UK. Clare & Gudjonsson (Reference Clare and Gudjonsson1992) devised questions for police custody officers in London to use in reception screening (risk assessments). The basis of this work was to identify ‘mental vulnerability’ in its broader sense, leading to further research in this field. Serious implications can also arise after an individual is charged in police custody then arrives at court, where issues such as effective participation in the court process and fitness to plead (competency to stand trial) may become relevant (Brown Reference Brown2019). Therefore, it is important to identify vulnerability as early as possible in the criminal justice system, to ensure appropriate healthcare intervention and that the person concerned can participate in a meaningful way.
An early evaluation of Clare & Gudjonsson's screening questions in police custody in Cambridge, UK, found that almost 12% of those screened had previously attended a ‘special needs school’, around half had attended ‘learning difficulties’ schools and the remainder had attended schools for young people with ‘emotional and behavioural’ difficulties (Lyall Reference Lyall, Holland and Collins1995). Regardless, the vast majority reported the need for help with communication problems. These screening questions had disappeared from the mandated risk assessment questions in London by 2008, but similar items were trialled during the piloting of the HELP-PC risk assessment in 2012, showing that they retained good discriminatory power between detainees with and without intellectual disability (McKinnon Reference Mckinnon, Thorp and Grubin2015).
The Hayes Ability Screening Index (HASI), which was developed to identify prisoners with intellectual disability in Australia, has the advantage of not relying solely on self-report. With sensitivity of 82% and specificity of 72%, its use in police custody has been advocated (Silva Reference Silva, Gough and Weeks2015), but an administration time of around 20 min may render it unfeasible for screening every detainee.
A shorter seven-item tool, the Learning Disability Screening Questionnaire (LDSQ), was developed by and has been validated in community forensic, forensic in-patient and prison settings, with sensitivity and specificity both exceeding 80%. At 5–10 min per administration, it may be more promising for use in police custody settings; studies administering the LDSQ in such settings have estimated the prevalence of intellectual disability to be 3% (Middlemiss Reference Middlemiss2012), 7% (Young Reference Young, Goodwin and Sedgwick2013) and 4.5% (Samele Reference Samele, McKinnon and Brown2021). Nevertheless, the LDSQ has not yet been validated in police custody, although Silva et al (Reference Silva, Gough and Weeks2015) have also suggested its use by liaison and diversion teams.
The 15-item self-report Rapid Assessment of Potential Intellectual Disability (RAPID) screen has shown good positive predictive value in court attendees and police detainees, with all those screened positive found to have intellectual disability or borderline intellectual functioning on validation testing, although the extent of false-negative screens remains unclear.
Autism spectrum disorder
Methodological variations hamper estimates of the prevalence of autism spectrum disorder (ASD) within the criminal justice system. One systematic review reported wide prevalence rates (2–29%) among offender populations and found that the rate of offending among the ASD population varied between 2 and 26%, with little difference between types of offence between people who did and did not present with ASD (King Reference King and Murphy2014). From the perspective of police custody, detainees with ASD, regardless of any additional presence of intellectual disability, are of relevance because of concerns about cognitive processing and potential vulnerability during police interviews; people with ASD are more likely to have social communication problems, suggestibility, be overly compliant or display anxiety and rigidity, leading to poor performance in police interviews (Allely Reference Allely2015). There are therefore important reasons to attempt to identify people in police custody who present with ASD, but short tools for the identification of ASD in this setting, such as the Autism Spectrum Quotient (AQ-10), have not yet been evaluated in this population.
Hyperkinetic disorders
Young et al (Reference Young, Goodwin and Sedgwick2013) administered the Diagnostic Interview for ADHD in Adults (DIVA) to custody detainees and found that 23.5% had ‘current symptoms’. Recently, Samele et al (Reference Samele, McKinnon and Brown2021) estimated 11% of custody detainees to have attention-deficit hyperactivity disorder (ADHD) using the Adult ADHD Self-Report Scale (ASRS). This compares with studies investigating liaison and diversion referrals which did not use structured tools and reported rates of 2–3% (McKenna Reference McKenna, Murphy and Rosenbrier2019). Although it can be applied quickly, meaning that it is attractive for use in police custody settings, the ASRS may lack specificity, but may nonetheless facilitate referral to liaison and diversion teams.
Dementia
Given the relatively young average age of police custody detainees, dementia-related disorders are seen less commonly than among the general population. One Dutch study found no one with dementia among 1357 detainees (Dorn Reference Dorn, Ceelen and Buster2014) and only 8% of 50 detainees over 60 years of age in a much earlier English study were assessed as having ‘possible dementia’ (Needham-Bennett Reference Needham-Bennett, Parrott and MacDonald1996). Dementing disorders may not be recognised until a crisis takes place, which may be arrest. Norfolk & Stark (Reference Norfolk, Stark and Stark2005) recommended the use of the Mini-Mental State Examination (MMSE), particularly among older detainees. Although not validated in police custody settings, this may be a suitable tool for liaison and diversion services to apply to detainees over the age of 50, to allow them to be referred to appropriate primary care or specialist services, including memory protection services.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is common in the criminal justice system. One meta-analysis found a point prevalence of 6% among male and 21% among female prisoners, meaning that these conditions are between 5 and 8 times more common than in community samples (Baranyi Reference Baranyi, Cassidy and Fazel2018). One study in police custody in London found a point prevalence of 8% (Samele Reference Samele, McKinnon and Brown2021).
The Trauma Screening Questionnaire (TSQ-10) has a sensitivity of 86% and specificity of 93% against the Clinician-Administered PTSD Scale (CAPS). As a short questionnaire, it may be suitable for administration in police custody by non-healthcare professionals or by self-report in the custody suite, but further validation is required, as is a clinical service plan that describes what should be done if a detainee screens positive.
Substance misuse
Around half of all deaths in custody are identified as being caused by drugs and/or alcohol, and in around four out of five deaths drugs or alcohol were identified as associated factors (Lindon Reference Lindon and Row2017). Substance use disorders frequently accompany other mental disorders. There are, however, conceptual reasons to consider alcohol and drugs separately, as will be discussed.
Alcohol
Alcohol use among people detained in police custody varies between 25 and 40% (McKinnon Reference McKinnon and Grubin2013a; Samele Reference Samele, McKinnon and Brown2021), which can pose serious risks associated with its short- and long-term effects in this setting.
Intoxication and fitness for detention
The characteristics of intoxication (e.g. slurred speech, incoordination and disinhibition) are mostly temporary. Intoxicated detainees, and those at risk of alcohol withdrawal, are likely to be unfit for interview and could be at greater risk of false confession. Severe intoxication can lead to death by respiratory failure, by issues associated with loss of consciousness (e.g. aspiration leading to respiratory arrest) or by the presence of hidden problems such as unidentified head injuries. Intoxication by any cause should result in the attention of a healthcare professional, but specific screening for alcohol dependence is important when considering risk of alcohol withdrawal (see in the following). The Glasgow Coma Scale (GCS) has been recommended as a minimum screen by the Royal College of Physicians’ Faculty of Forensic and Legal Medicine (Payne-James Reference Payne-James and Marks2019). The Alert, Voice, Pain, Unresponsive (AVPU) scale commonly used in intensive care settings correlates with the GCS and is shorter but has not yet been evaluated in police custody.
Dependence
Detention in police custody may be the first presentation of an alcohol use disorder and is an opportunity to deliver brief interventions to promote abstinence or reduction once sober and prior to release, especially given the long-term health effects of persistent alcohol misuse (Addison Reference Addison, McGovern and Angus2018). The most widely used screening tool is the Alcohol Use Disorders Identification Test (AUDIT), although a shorter version, the Fast Alcohol Screening Test (FAST), has been recommended for use in custody owing to its brevity.
Withdrawal and delirium tremens
Of immediate concern is the sudden cessation or reduction of alcohol intake in a dependent person, which may trigger alcohol withdrawal syndrome. Alcohol withdrawal syndrome manifests 3–12 h following the reduction, with withdrawal seizures potentially occurring 12–48 h after cessation of drinking. This is a medical emergency. Delirium tremens (DTs) is a state of severe withdrawal and often presents 3–4 days following cessation of alcohol, with vivid hallucinations, confusion, agitation, tremor and insomnia. With mortality of around 5%, identifying alcohol withdrawal syndrome is critical. The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar) is used in hospital settings to quantify withdrawal symptoms and signs and guide treatment. A score of over 15 indicates an increased seizure risk and is recommended as a cut-off for transfer to hospital for in-patient detoxification (Stark Reference Stark and Holmes2014). Its use in police custody has not yet been evaluated, but it may prove to be a valuable tool to minimise risk in detainees with a history of problematic alcohol use.
Drugs and illicit substances
Detainees in police custody unsurprisingly present with substantial levels of drug use (Payne-James Reference Payne-James, Wall and Bailey2005) along with poor physical or mental health. The Royal College of Psychiatrists and Faculty of Forensic and Legal Medicine (2020) guidelines for the management of substance use disorders do not recommend specific screening tools for detainees in police custody, but a close relative of the AUDIT, the Drug Use Disorders Identification Test (DUDIT), has been validated in criminal justice system settings with a sensitivity of 90%. As with alcohol, custody may present an opportune moment for brief interventions relating to illicit substances.
Head injuries
Acute phase
In the acute phase, head injury can substantially impair a detainee's capacity to participate in an investigative interview as well as pose significant risk of harm if not identified. Guidance from the College of Policing's Authorised Professional Practice recommends that ‘detainees who have suffered a head injury should be immediately transported to hospital for medical assessment and monitoring’ (College of Policing 2013). Carter & Mayhew (Reference Carter and Mayhew2010) found that head injuries accounted for 14% of all transfers from police custody to hospital. In the absence of an adequate account of injury or signs of trauma, recognising that a person has sustained a head injury is not straightforward, especially when masked by substance use. However, half of all traumatic brain injuries occur under the influence of alcohol, and since both may render an individual incoherent, uncooperative and aggressive, intoxication may mask undiagnosed head injuries. As research suggests that alcohol intoxication does not significantly impair a person's performance on the Glasgow Coma Scale (GCS), change in GCS score could be a sensitive indicator of head injury and lead to appropriate health intervention (Stuke Reference Stuke, Diaz-Arrastia and Gentilello2007).
Relevance to offending
Understanding the link between brain injury and offending is important as it has implications for planning interventions, reducing long-term risks of reoffending and minimising associated disability in the individual. A large proportion of prisoners have a history of serious head injury: meta-analysis by Farrer & Hedges (Reference Farrer and Hedges2011) showed significantly higher rates of traumatic brain injury among incarcerated groups compared with the general population; this finding was supported by the work of McMillan et al (Reference McMillan, Graham and Pell2019), who reported lifetime prevalence rates of 24.7% for head injury among under-35-year-olds in Scottish prisons, compared with 18.2% in a matched general population. Head injury may result in increased impulsivity, aggression and impaired executive function, all of which can be precursors to increased offending behaviour. There are also correlates with detainees who present with other vulnerabilities, such as developmental disorders.
The Ohio State University Traumatic Brain Injury Identification Method (OSU TBI-ID) is an easy to administer three-step questionnaire requiring little formal training. It is brief to administer in a custody setting, although it relies on the detainee's accurate recollection of events. Generally, people tend to remember incidents where they have sustained head injury, but often cannot provide further details to determine the severity.
The Brain Injury Screening Index (BISI) is a self-report questionnaire to identify history of acquired brain injury. Evaluation of the tool in a custody setting showed poor to moderate interrater reliability, but moderate to good test–retest reliability, and its performance compared with medical records suggests its utility as an initial tool to triage those needing further neuropsychological assessment (Ramos Reference Ramos, Liddement and Addicott2020).
Deaths in custody
Aasebø et al (Reference Aasebø, Orskaug and Erikssen2016) compiled rates for deaths in police cells across mainly high-income countries. Rates varied from 0.14 deaths per year per million population in Germany to 4.46 deaths per year per million in South Africa. The authors also reported intoxication, intracranial bleeding and suicide as major causes of death. In England and Wales, the Independent Office for Police Conduct (IOPC) reported that the majority of deaths relate to the effects of intoxication or the involvement of restraint and that death by suicide within custody suites has become a rare event (Independent Office for Police Conduct 2020). However, death by suicide in the period immediately following police custody remains a significant concern: 40–70 such deaths occurred per year over the past 15 years, and many of those who died were accused of sexual offences. Figures from England and Wales suggest that although BAME detainees are not overrepresented among all-cause deaths during or following custody, a disproportionate number die following the use of force (INQUEST 2021).
Since the themes relating to deaths in and following police custody remain consistent, they provide areas in which the potential for screening in police custody can be further developed.
Screening for risk of suicide and self-harm
As already mentioned, although suicides represent a small number of deaths in custody, more people die by apparent suicide following release from custody. There has been little empirical evidence looking at suicide risk in police custody. In studies conducted in London, the Mini-International Neuropsychiatric Interview (MINI) identified 18% of custody detainees as being at risk of suicide (Samele Reference Samele, McKinnon and Brown2021) and the Beck Scale for Suicidal Ideation (BSSI) found suicidal ideation in 11% of screened detainees (McKinnon Reference McKinnon, Srivastava and Kaler2013b).
An important point of note is that screening tools used in isolation are not clinically effective to assess suicide risk; in the UK they are not recommended for clinical decision-making (National Institute for Health and Care Excellence 2011) and a clinical assessment should be undertaken.
Special circumstances
Statutory screening in police custody
Legal statutes in the UK jurisdictions of England and Wales and of Northern Ireland mandate the screening (known in police circles as ‘risk assessment’) of every detainee who is arrested and taken into police custody. In Scotland this is covered by standard operating procedures (Police Scotland 2018). ‘Risk assessment’ takes place on arrival at the custody suite and is carried out by a police custody officer (usually of sergeant rank) who has overall responsibility for the welfare of detainees. The legal ownership of risk assessment screening by the police in custody leads to a conceptual problem about the purpose of screening. There has been a temptation to emphasise the prevention of serious outcomes such as deaths in custody, which are reported annually by the IOPC in England and Wales, rather than using the risk assessment screening as an opportunity to intervene in health problems and promote health where an intervention could prevent reoffending related to the health issue. Recently, Stoneman et al (Reference Stoneman, Jackson and Dunnett2019) described a lack of standardisation across police forces, with not all risk assessment processes meeting standards laid out in the College of Policing's Authorised Professional Practice (College of Policing 2013). The HELP-PC project identified that risk assessments contained within police IT systems can be deficient compared with a structured clinical history and examination (McKinnon Reference McKinnon and Grubin2013a) and that the effectiveness of these assessments can be improved by the introduction of adapted evidence-based screening tools (McKinnon Reference McKinnon and Grubin2014).
Other jurisdictions have different approaches to the reception screening of custody detainees. In Canada, although there is no statutory requirement to screen people for health conditions when they are taken into police custody, provincial governments have developed policies setting out police officer duties to recognise medical emergencies requiring transfer to an emergency department (R. Hoffman, personal communication, 2021). Most Australian states have their own police custody policies and procedures, although the Australian Federal Police, has issued national guidelines on persons police custody settings (Australian Federal Police 2012). This guidance sets out the responsibilities of the police officer in the light of a detainee requiring medical attention, but there is no requirement to screen or risk assess each detainee formally. In France, a custody detainee has a right to be examined by a physician within 3 h, but there is no clear process of screening for this purpose (Hodgson Reference Hodgson2004). Reports from Germany suggest that a lack of standardisation means that medical opinions are frequently not requested by police officers when they should be (Heide Reference Heide, Stiller and Lessig2012).
A hitherto under-researched area is screening at the point of release from custody, or so called ‘pre-release risk assessment’. It is unclear how effective such screening is, and there is variation across UK police forces. However, this is a potential opportunity for the development of tools to assist decision makers to aggregate important clinical and risk assessment information before releasing detainees with a defensible plan to meet needs relating to mental disorder (Lyall Reference Lyall, Austin and Alder2022).
Possible harms of screening
Screening is not without its problems, and there can be harms in certain circumstances. False-negative results miss true cases, leading to missed diagnoses. False-positive results can lead to unnecessary interventions such as surgery for benign conditions or limitations on activity due to false-positive cardiac screening. In a recent systematic search of Cochrane reviews of screening interventions, Johansson et al (Reference Johansson, Borys and Peterson2021) found that only one-third of reviews reported on false-positive or false-negative outcomes. As outlined in the Special Circumstances section above, routinely used screening in police custody is inaccurate. Although there may be concerns that screening-in too many individuals may overwhelm healthcare professionals, if full-time healthcare and specialist liaison and diversion services are embedded in custody, the screening balance should arguably be weighted towards overinclusion.
Conclusions
Police custody is a complex setting in which people are often held following stressful circumstances and are likely to be distressed by the fact of their arrest and detention. In addition, they may be intoxicated with, or withdrawing from, drugs or alcohol, or present with other physical health problems, including long-standing conditions (e.g. asthma or hypertension) or recent injuries (e.g. minor injuries/soft tissue injuries or more serious head injuries). These presentations complicate the process of screening and assessment for mental health conditions in police custody, and when this is combined with the prioritisation of police processes (e.g. formal arrest and questioning) and the legislative time constraints that apply in custody, further limitations become apparent. Nevertheless, given the high levels of psychiatric morbidity apparent in this population, it is incumbent on services to do their best to identify people and subsequently ensure that they receive the best available treatment, particularly in cases in which it is urgently needed. Yet despite this, although relevant screening tools are available, most were developed for use in the general population and few have been validated for use in police custody.
An evidence-based screening protocol
As screening tools have been developed, the literature has described a tension between concepts of diagnosis, vulnerability and risk, leading some to advocate for a ‘whole person approach’ to screening and intervention, as opposed to a diagnostic approach (Farrugia Reference Farrugia2021; Wardrop Reference Wardrop, Ranse and Chaboyer2021). However, although this argument may be useful from the perspective of research or service-planning, it has serious limitations in clinical practice, particularly as regards the identification of serious or life-threatening medical and psychiatric conditions that require immediate intervention. Clinical pathways and treatments vary between conditions, and it can be a significant challenge for non-experts in mental disorders to identify individual elements thereof to make sense of complex behavioural presentations; it is known that police officers often have difficulties in this role (McKinnon Reference McKinnon and Finch2018). Instead, a more pragmatic approach is needed, such as that laid out in Fig. 1. In accordance with this evidence-based protocol, an initial battery of screening tools is used to triage detainees for referral to a second stage in which specialist assessment takes place. During this second stage, a more holistic and nuanced clinical approach can then be applied by trained and experienced specialist clinicians.
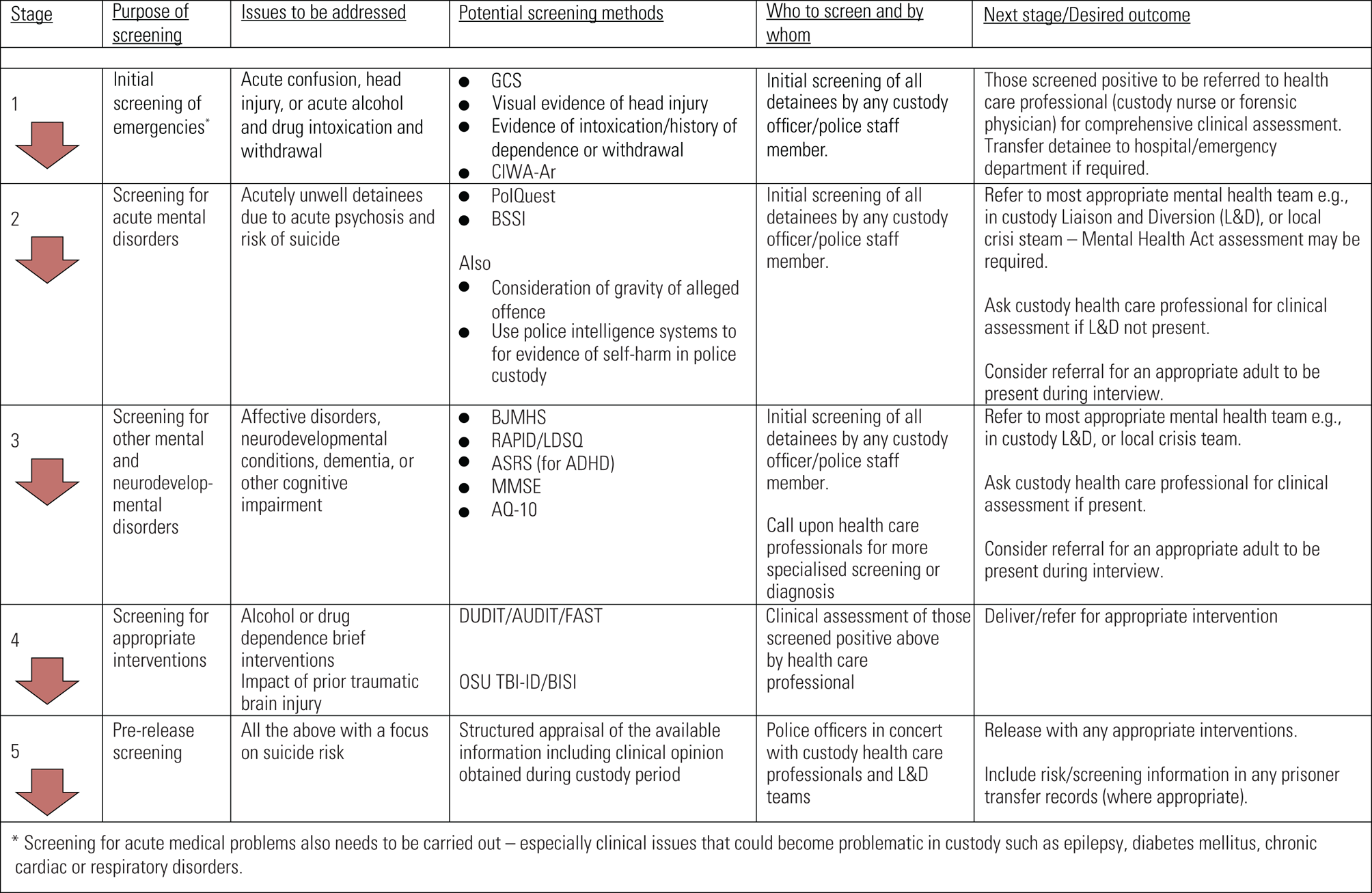
FIG 1 Proposed stages of clinical screening for mental disorders in people who have been arrested and taken into police custody. GCS, Glasgow Coma Score; CIWA-Ar, Clinical Institute Withdrawal Assessment for Alcohol scale; PolQuest, Police Mental Health Screening Questionnaire; BSSI, Beck Scale for Suicidal Ideation; BJMHS, Brief Jail Mental Health Screen; RAPID, Rapid Assessment of Potential Intellectual Disability; LDSQ, Learning Disability Screening Questionnaire; ASRS, Adult ADHD Self-Report Scale; ADHD, attention-deficit hyperactivity disorder; MMSE, Mini-Mental State Examination; AQ-10, Autism Spectrum Quotient; DUDIT, Drug Use Disorders Identification Test; AUDIT, Alcohol Use Disorders Identification Test; FAST, Fast Alcohol Screening Test; OSU TBI-ID, Ohio State University Traumatic Brain Injury Identification Method; BISI, Brain Injury Screening Index.
It is vital that screening undertaken within police custody should prioritise life-threatening issues, such as alcohol withdrawal syndrome or confusion arising from head injury, before considering the management of other less urgent but nonetheless important mental and physical health conditions. Although the full consideration of physical health problems in police custody – including, for example, epilepsy or diabetes – is beyond the scope of this article, they also need to be factored into health screening and assessment processes.
There is a literature that indicates that police detainees with cognitive difficulties, and not only those with established intellectual and developmental disabilities or ASD, may benefit from symbol-based communication to ensure effective participation in the process, and risk assessment (Parsons Reference Parsons and Sherwood2016). Additionally, given the nature of police detention, it is necessary to factor in the possibility that detainees provide unreliable responses to screening tools if they are intoxicated or feeling defensive or argumentative on arrival. Therefore, if a comprehensive holistic screening process is to be developed, given the time limitations in police custody, a pragmatic approach needs to be taken. Police custody detainees and service users have first-hand experience of screening, and these views need to be acknowledged as a core part of developing and refining screening tools (Noga Reference Noga, Walsh and Shaw2015; McKinnon Reference McKinnon and Finch2018).
Finally, we have not addressed the issue of screening for personality disorder in police custody. Its prevalence among prisoners and some limited data suggesting it is present in large numbers of police custody detainees (Samele Reference Samele, McKinnon and Brown2021) merit further investigation. There is likely to be substantial comorbidity with mental disorders, causing vulnerability as outlined above, but we do not recommend a role for isolated personality disorder screening in police custody, although it may become more relevant at a later stage during court proceedings.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bja.2022.25.
Acknowledgements
I.M. would like to thank Professor Ron Hoffman, Nipissing University, Ontario, Canada, for his insights into Canadian police custody procedures.
Author contributions
All authors contributed to the drafting, review and approval of this article.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
I.M. currently holds Economic and Social Research Council (ESRC) funding to investigate healthcare provision in police custody settings. He has also held a National Institute for Health and Care Research (NIHR) Doctoral Fellowship to investigate health and screening of police custody detainees. A.F. has recently held a grant from Guy's and St Thomas’ Charity, London, entitled ‘Early assessment and intervention of intellectual disabilities and autism in court’, culminating in a publication on which A.F. and I.M. were co-authors.
MCQs
Select the single best option for each question stem
1 Morbidity in police custody:
a is substantial across the domains of physical health, mental health and substance misuse
b mainly relates to alcohol withdrawal and risk of head injury
c is presently managed effectively using internationally agreed pathways
d is less than that presenting in prison settings
e bears little relationship to morbidity detected in court samples.
2 Vulnerable groups in police custody:
a are effectively identified and managed using healthcare screens
b come under the remit of liaison and diversion services internationally
c include people with neurodevelopmental conditions
d are always considered suggestible
e should not be questioned under any circumstances.
3 Health screening in police custody:
a is an exact science
b should replace clinical judgement
c is a field that has been well-research and defined
d often relies on screening instruments that have been validated for use in other populations
e should not be recommended.
4 Conditions requiring an emergency response in police custody include:
a eczema
b hypertension
c bruising arising from recent assault
d psychosis
e alcohol withdrawal.
5 As regards health screening in police custody:
a this is a field in which there is the highest quality evidence, including many randomised controlled trials
b we are fortunate that there is widespread international cooperation in this field, with an international consensus approach describing a way forward
c healthcare teams working in police custody always use health screens
d before intervening in an emergency, it is important to engage the individual in a comprehensive screening process
e screening should be seen as an adjunct to clinical examination, rather than a replacement for it.
MCQ answers
1 a 2 c 3 d 4 e 5 e





eLetters
No eLetters have been published for this article.