Case report
A 39-week infant was born via Caesarean section for failure to progress at 2.87 kg at our institution. He had a prenatal cardiac diagnosis of double outlet right ventricle with a large subpulmonic ventricular septal defect, normally related great arteries and aortic atresia with a diminutive ascending and transverse aorta. He additionally had a genetic diagnosis of 22q11.2 deletion. Upon delivery he required intubation for hypoxaemia and poor respiratory effort. He was stabilised and initiated on a prostaglandin infusion for ductal dependent systemic blood flow. A postnatal echocardiogram, followed by a cardiac CT angiogram (Figure 1), again demonstrated the aortic valve atresia as well as a type C interrupted aortic arch with retrograde filling of his ascending aorta via the right common carotid artery through intracranial collateralisation and a presumed intact circle of Willis. He was taken to the operating room at 4 days of life where he underwent a complete biventricular repair with Yasui and type C interrupted aortic arch repair via median sternotomy.
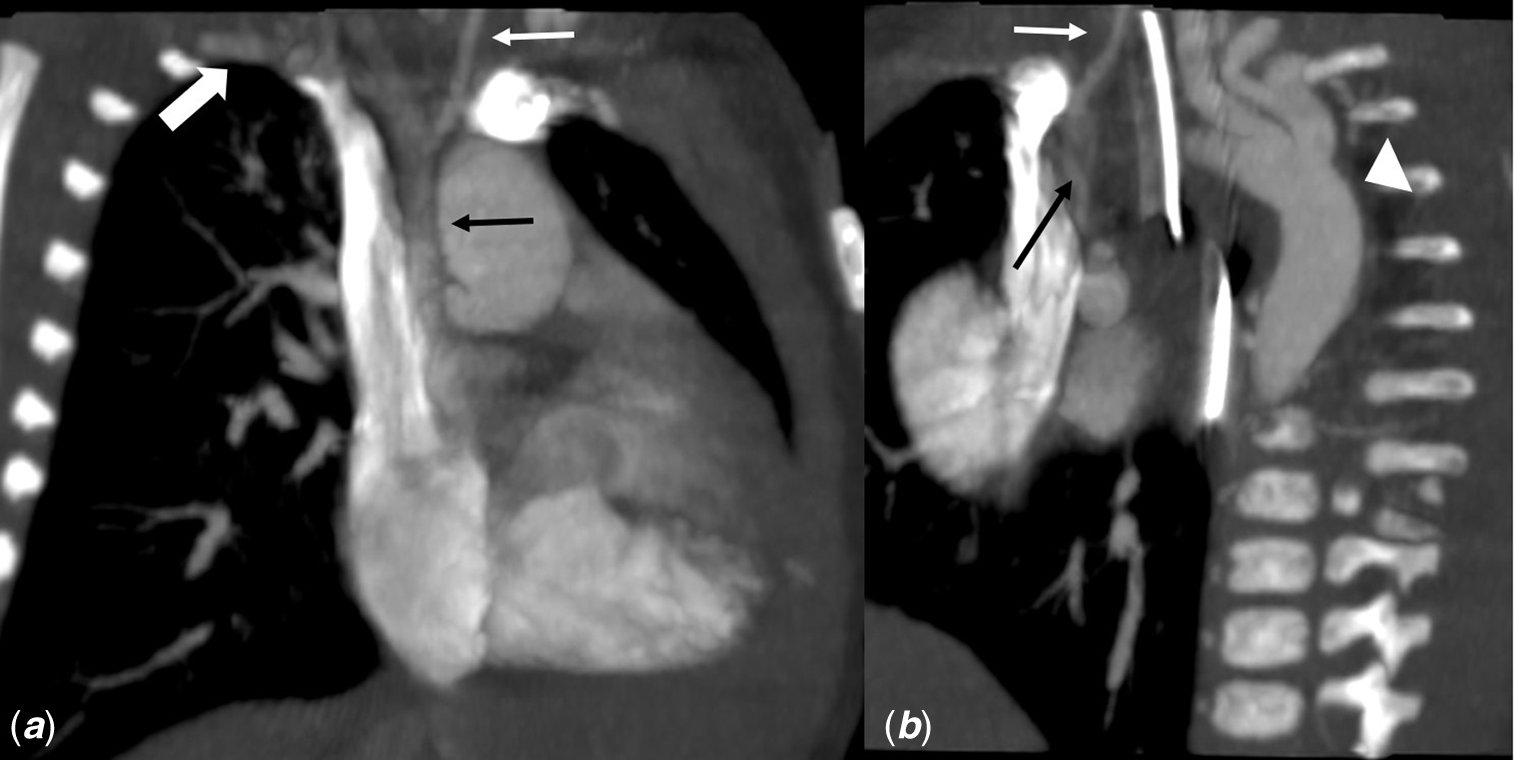
Figure 1. CT angiogram images showing the interrupted aortic arch with retrograde filling. Coronal ( a ) and sagittal ( b ) reformatted contrast-enhanced CT angiogram depicting retrograde opacification of the ascending aorta (black arrow) via right subclavian artery (bold white arrow) as well as right common carotid and inferior thyroid arteries (white arrow). Note the caliber difference and difference in opacification of the ascending aorta compared to the descending aorta (white arrow head).
After careful dissection and visualisation of anatomy, he was cannulated for cardiopulmonary bypass and cooled to 24°C. Standard venous cannulae were placed. For arterial cannulation, an aorta cannula was first placed in the distal ductus arteriosus, directed towards the descending aorta, and the patient was placed on bypass. On bypass, the surgeons cannulated the right subclavian artery, thus establishing separate flows for the systemic circulation and for the coronary and right-sided cerebral circulations. The heart was retracted and the descending aorta cannulated directly, at which time the ductal cannula was removed.
On beating heart bypass, the descending aorta was clamped and the patent ductus arteriosus was ligated and divided. The transverse aortic arch and proximal descending aorta were augmented via a large pulmonary homograft patch. The aorta was then cross-clamped and cardioplegia administered. The patch augmented arch was anastomosed to a lateral incision made in the distal ascending aorta, and a Damus-Kaye-Stansel was performed. A right atriotomy and right ventriculotomy were performed with baffling from the left ventricle across the ventricular septal defect to the pulmonary valve using polytetrafluoroethylene patch. A 10-mm aortic homograft with a 10-mm PTFE tube extension was obtained and placed between the right ventricle and branch pulmonary arteries. The atrial septal defect was downsized, leaving a residual 3–4 mm defect as a pop-off. The total bypass and cross-clamp times were 261 and 124 minutes, respectively.
The bypass wean was uneventful and there were no concerns on post-operative transesophageal echocardiogram. The patient was returned intubated with an open chest to the paediatric ICU for post-operative management. He was able to undergo chest closure on post-operative day 2. His post-operative course was significant for multiple failed extubation attempts with eventual tracheostomy placement for bilateral vocal cord paresis and subglottic stenosis. This was thought to be congenital given severity of paresis and failed extubation attempts in the pre-operative period as well as post-operatively, though we cannot rule-out an operative injury. He also underwent a gastrostomy tube placement at the time of tracheostomy. He was discharged home on post-operative day 40. An echocardiogram obtained 6 months after repair demonstrated a small residual ventricular septal defect and mild conduit stenosis with an unobstructed aortic arch and normal biventricular function.
Discussion
Aortic valve atresia and interrupted aortic arch are rare combination with unique considerations regarding cerebral and myocardial perfusion. This anatomy with a type C interruption has only been described three other times in the literature, Reference Decaluwe, Delhaas and Gewillig1–Reference Norwood and Stellin4 with only one case involving circle of Willis dependent circulation. Reference Malankar, Glatz, Weinberg and Gaynor3 The other two cases involved the presence of bilateral ductus. Reference Decaluwe, Delhaas and Gewillig1,Reference Norwood and Stellin4 There have been a greater number of reported cases of aortic atresia with type B interruption with wider variety in cerebral and myocardial perfusion, including aberrant right subclavian artery and circle of Willis dependent circulation; bilateral ducti; aortopulmonary window; double aortic arch; fistulous connection from the pulmonary artery to the left coronary artery. Reference Lacour-Gayet, Kandachar, Al-Bulushi and Maddali2
The aforementioned case reports are increasingly describing complete neonatal repair, including the case of the type C interruption presented by Malankar et al. Reference Malankar, Glatz, Weinberg and Gaynor3 While similar in our approach with a Yasui and interrupted arch repair, I would like to highlight our unique arterial cannulation approach which avoided circulatory arrest by having two arterial cannulae which allowed for preserved cerebral perfusion via the right subclavian arterial cannula. In all, this was an interesting case of rare anatomy with successful complete biventricular repair with Yasui and type C interrupted aortic arch repair via median sternotomy.
Acknowledgements
Thank you to Dr Cristina Fuss, OHSU Department of Radiology, for her assistance with selecting and labelling the above figure. Thank you to Dr Lars Grosse-Wortmann, OHSU Department of Pediatric Cardiology, for his guidance on this case report.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the Helsinki Declaration of 1975, as revised in 2008.




