Introduction
Cancer invokes the need for patients to receive not only curative services but also supportive care. The integration of appropriate anticancer therapies with psychosocial support improves the quality of treatment (Kang et al. Reference Kang, Go and Bruera2018). Therefore, healthcare professionals (HCPs) should care for the patient, by means of a holistic approach, based on compassion (Sinclair et al. Reference Sinclair, Norris and McConnell2016b).
Compassion literally means “suffering with” (Sinclair et al. Reference Sinclair, Beamer and Hack2017). It is a deep awareness of the suffering of another, associated with a wish to relieve it, through relational understanding, and actions (ibidem). It is linked with prosocial motivation and/or behavior (Sinclair et al. Reference Sinclair, McClement and Raffin-Bouchal2016a). Larkin considers compassion as “the essence of palliative and end-of-life care” (Larkin Reference Larkin2015). It implies a shift of gaze in the health workers from organic pathology to the patient’s well-being, considered in its entirety (Shih et al. Reference Shih, Hu and Lee2013). Compassion is based on understanding demeanor, the gentle touch of a shoulder, arm or hand, as well as verbal and nonverbal communication with terminally ill cancer patients [ibidem]. As expressed by Reference Brito-Pons and Librada-FloresBrito-Pons and Librada-Flores, compassion can bring health professionals closer to improving care for people at the end-of-life (Brito-Pons and Librada-Flores Reference Brito-Pons and Librada-Flores2018).
HCPs’ compassion can improve the quality of care of individuals facing the end-of-life and can contribute to maintaining and enhancing their sense of dignity.
There are 2 ways to understand dignity: the first is called basic dignity and is an intrinsic and inviolable feature of human life which does not depend on external conditions; the second is called dynamic dignity which is related to the patient’s perception of himself as well as external circumstances (Ashcroft Reference Ashcroft2005; Leung Reference Leung2007; Pullman Reference Pullman2004; Rodríguez-Prat et al. Reference Rodríguez-Prat, Monforte-Royo and Porta-Sales2016). Dignity conserving care has an important effect on end-of-life patients because it means preserving and respecting patient’s autonomy (Chochinov Reference Chochinov2007; Viftrup et al. Reference Viftrup, Hvidt and Prinds2021). Therefore, dignity conserving care should be integrated into the work of all HCPs working in palliative care, as a means of responding to unmet needs of patients and their families (ibidem). Delmar et al. emphasize a relational view of the human being: a patient’s dignity can be maintained through social support of healthcare providers (Delmar et al. Reference Delmar, Bøje and Dylmer2006). Thus, a compassion based relationship between health professional and patient could make the latter feel more accepted and supported and could help enhance the patients’ value and dignity.
To our knowledge, in the literature, studies focused on the practices to conserve dignity at the end-of-life (Brown et al. Reference Brown, Johnston and Östlund2011; Chochinov Reference Chochinov2002); however, there are no studies on the role of compassion regarding a patient’s dignity. Therefore, we hypothesized that the providers’ compassion could be associated with the sense of dignity perceived by patients in palliative care.
Thus, the present study aimed to investigate the association between end-of-life cancer patients’ sense of dignity, patients’ perceptions of HCPs’ compassion, and HCPs’ self-assessed compassion toward patients, investigating through specific attitudes and behaviors.
Moreover, end-of-life patients can be affected by dignity-related distress because of some problems related to inability to perform everyday life tasks (washing or dressing), psychological symptoms (anxiety, depression, fatigue), and physical symptoms (nausea, pain, breathing difficulties) (Johnston et al. Reference Johnston, Larkin and Connolly2015). On the basis of this, in this study, the relationship between compassion and patients’ physical and psychological symptoms, such as levels of anxiety and depression, was also investigated.
Methods
Study population
The sample consisted of 105 end-of-life cancer patients and 40 HCPs. For each patient, their referenced HCP, either physician or nurse, who volunteered to participate in the research, was tested. The reference HCP was tested as many times as the patients he/she was following. Participants were recruited from May 2019 to May 2020 in a hospital and in a hospice in Turin. Inclusion criteria for patients were the following: having a diagnosis of cancer; reporting a score on the Karnofsky Performance Status (KPS) ≤50 (Karnofsky Reference Karnofsky and MacLeod1949); being at least 18 years old; being able to give informed consent; meeting the criteria to access palliative care (Legge 15 Marzo 2010); the latter are the following: the presence of an advanced cancer for which there are no appropriate curative treatments, an estimated life expectancy of <4 months, and a KPS ≤50.
Inclusion criterion for healthcare providers was working in palliative care.
Exclusion criteria for patients were the following: having a diagnosis of a severe psychiatric disorder and having a cognitive impairment that would not allow the patient to provide his informed consent or complete the protocol.
Patients received psychological support, namely all admitted patients receive a psychologist consult as a part of their routine care. During the first consultation, the psychologist explained the research. Accordingly, 20 patients refused to participate in the study because they were not interested, 10 were excluded because of cognitive impairment, and 105 participated in the study. Participating patients were administered the various scales by the psychologist, with HCPs scales being completed thereafter. The Edmonton Symptom Assessment System (ESAS), the Patient Health Questionnaire-9 (PHQ-9), the Generalized Anxiety Disorder Assessment (GAD-7), and the Patient Dignity Inventory (PDI) were administered to patients (see “Measures” section).
To assess patients’ perception of compassion, the Compassion Patient Survey (COMP_PT) (see “Measures” section) was created ad hoc for the study.
HCPs fulfilled the Compassion Healthcare Provider Survey (COMP_HCP) (see “Measures” section) that was created ad hoc for the study. These 2 surveys were created based on Sinclair’s definition of compassion (Sinclair et al. Reference Sinclair, Beamer and Hack2017).
The study was approved by the “Comitato Etico Interaziendale A.O.U Città della Salute e della Scienza di Torino – A.O. Ordine Mauriziano – A.S.L. Città di Torino”: protocol number 0034403, procedure number CS2/1178, date of approval: 29/03/2019. The authors state that the research was conducted in accordance with the latest version of the principles of the Declaration of Helsinki.
Measures
Data were collected through the following instruments:
The PDI (Bovero et al. Reference Bovero, Sedghi and Botto2018; Chochinov et al. Reference Chochinov, Hassard and McClement2008) is a 25-item scale which measures various sources of distress related to patients’ dignity. It is divided into 5 subscales: Psychological Distress, Social Support, Physical Symptoms and Dependency, Existential Distress, andLloss of Purpose and Meaning. The items are on a 5-point Likert scale ranging from 1 (not a problem) to 5 (an overwhelming problem).
The COMP_PT is a 10-item scale, which is a measure of the level of HCPs’ compassion perceived by the patient in the past 2 weeks. It is composed by the following items: (1) I felt the healthcare provider was particularly receptive to my needs; (2) I felt listened to with sincere attention by the healthcare provider; (3) The attitude of the healthcare provider allowed me to stay positive; (4) the healthcare provider smiled when he/she entered my room; (5) The healthcare provider was emotionally troubled by the manifestations of my stress; (6) my stress was tolerated without judgment; (7) I felt encouraged and supported by the healthcare provider; (8) the healthcare provider conveyed a gentle touch with me; (9) the healthcare provider kept eye contact when he/she talked with me; and (10) the healthcare provider was able to put himself/herself in my shoes. The items are on a 5-point Likert scale ranging from 0 (never) to 4 (always). A higher score corresponds to a greater level of compassion of the HCP perceived by the patient.
The COMP_HCP is a 10-item scale, which is a measure of HCPs self-reported level of compassion manifested toward patients in the past 2 weeks. The items are the same as the COMP_PT but referred to the HCPs self-perceived compassion toward their patients. The items are on a 5-point Likert scale ranging from 0 (never) to 4 (always). A higher score corresponds to a greater level of compassion of the HCP.
The ESAS (Bruera et al. Reference Bruera, Kuehn and Miller1991; Moro et al. Reference Moro, Brunelli and Miccinesi2006) measures the severity of 9 symptoms experienced by cancer patients: pain, fatigue, nausea, depression, anxiety, drowsiness, appetite, malaise, and shortness of breath. In the last item named “other”, patients can report other symptoms such as itching, hiccups, etc. The symptoms intensity is rated on an 11-point Likert scale, ranging from 0 (no symptom) to 10 (worst possible symptom).
The PHQ-9 (Kroenke et al. Reference Kroenke, Spitzer and Williams2001; Mazzotti et al. Reference Mazzotti, Fassone and Picardi2003) is a 9-item self-report scale, which measures the frequency of depressive symptoms in the past 2 weeks. The items are on a 4-point Likert scale (from 0 [never] to 3 [nearly every day]). Moreover, the instrument contains a questionnaire that investigates how much the presence of one of the depression symptoms described above interfered with work, with taking care of things and with being together with others, on a 4-point Likert scale (from no difficulty to extreme difficulty).
The GAD-7 (Spitzer et al. Reference Spitzer, Kroenke and Williams2006), Italian version, is a 7-item self-report scale, which measures the frequency of anxiety symptoms in the past 2 weeks. The items are on a 4-point Likert scale (from 0 [never] to 3 [nearly every day]). Moreover, the instrument contains a questionnaire that investigates how much the presence of one of the anxiety symptoms described above interferes with work, with taking care of things and with being together with others, on a 4-point Likert scale (from no difficulty to extreme difficulty).
Statistical analysis
Data administration and statistical analysis were performed using the Statistical Package for Social Sciences software 25.0 for Windows®.
Descriptive statistics, such as frequencies, means, and standard deviations, were used to describe the sample. Through the Shapiro–Wilk test, it was observed that the variables do not follow a normal distribution, thus the associations between the variables were explored with the nonparametric Kendall’s test. p values ≤.05 and .01 were considered statistically significant.
Results
Sociodemographic data of the sample
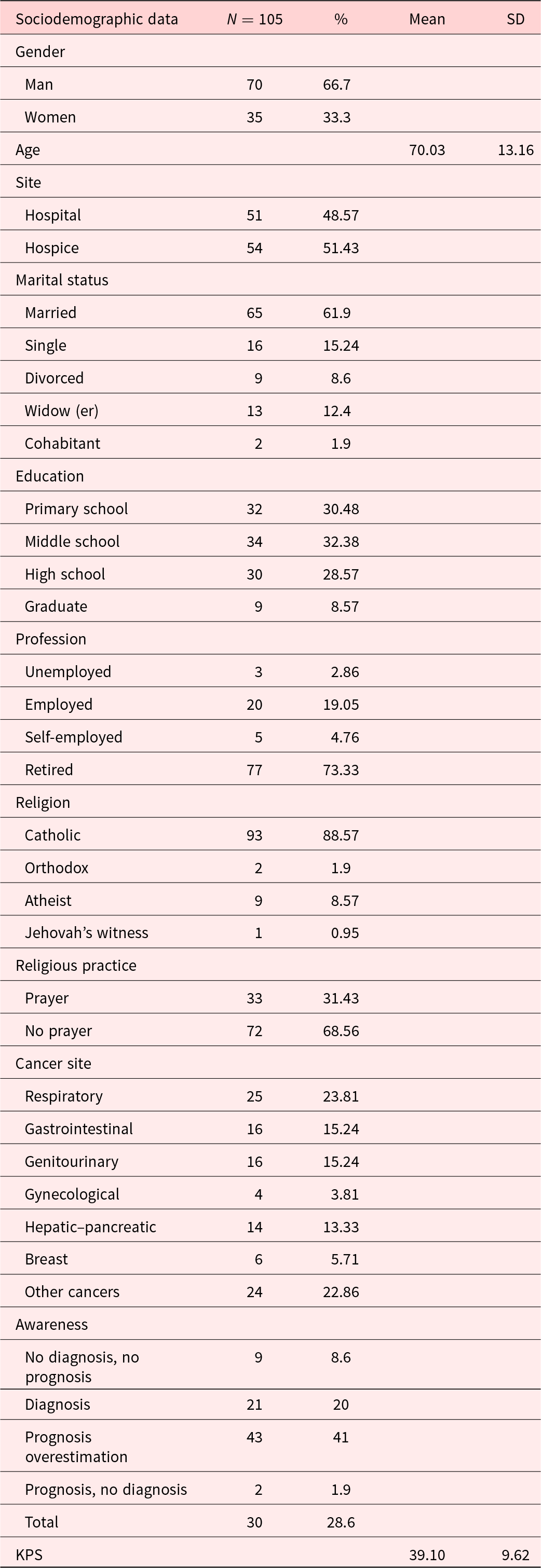
Sociodemographic data of healthcare providers are shown in Table 1. Sociodemographic data of patients are shown in Table 2.
Table 1. Sociodemographic data of HCPs

a Professionals working in health and social care.
Table 2. Sociodemographic data of the patients
Associations between patients’ perception of compassion and sense of dignity
COMP_PT negatively correlated with “Psychological Distress” PDI subscale (τ = −.171, p ≤ .05), “Social Support” PDI subscale (τ = −.208, p ≤ .01), and PDI total score (τ = −.167, p ≤ .05). See Table 3. No significant associations were found between COMP_HCP and PDI.
Table 3. Correlations between compassion and PDI subscales

COMP_PT: The Compassion Patient Survey, COMP_HCP: The Compassion Healthcare Provider Survey, PDI: Patient Dignity Inventory.
* p ≤ .05; **p ≤ .01.
Significant correlations are highlighted in bold.
Associations between patients’ perception of compassion and patients’ symptoms
COMP_PT negatively correlated with the following ESAS subscales: “Fatigue” (τ = −.152, p ≤ .05) and “Depression” (τ = −.171, p ≤ .05). See Table 4.
Table 4. Correlations between compassion and ESAS subscales

COMP_PT: The Compassion Patient Survey, COMP_HCP: The Compassion Healthcare Provider Survey.
* p ≤ .05.
Significant correlations are highlighted in bold.
No significant associations were found with GAD and PHQ-9 scores.
COMP_HCP significantly correlated with PHQ-9 (τ = .154, p ≤ .05), but it did not significantly correlate with ESAS, GAD.
Discussion
The present study aimed to investigate the association among the sense of dignity perceived by the patient, the level of compassion of the HCPs noticed and perceived by the patients and levels of compassion that HCPs felt to have toward patients, investigated through specific attitudes and behaviors.
Patients who perceived their HCPs to be more compassionate, had less dignity-related distress.
Similarly, when patients considered their clinician to be more compassionate, they had fewer symptoms of fatigue and depression. This data may suggest that HCPs’ compassionate care could alleviate patients’ physical and psychological symptoms. In fact, as suggested by the literature, compassion has the potential to enhance palliative care outcomes, improving patients’ quality of life and their satisfaction (Rodríguez-Prat et al. Reference Rodríguez-Prat, Monforte-Royo and Porta-Sales2016). Thus, it could play a significant role also with respect to further alleviating symptom distress.
Moreover, the results showed the positive association between compassion that HCPs felt they had toward their patients and patients’ symptoms related to depression. It could be that patients with depression may require additional support and encouragement to communicate their needs and concerns. HCPs may prioritize building trust and relationship with these patients to facilitate open communication and ensure that their needs are addressed effectively. Also, HCPs may understand that depression in oncology patients can exacerbate their suffering and decrease their quality of life. This understanding prompts them to approach these patients with compassion.
However, the results of the present research highlighted how the association between compassion that HCPs felt they had toward their patients and patients’ dignity-related distress was not significant. Probably, the reduction of patients’ dignity-related distress is associated with the perceived compassion. In line with this result, Lown et al. (Reference Lown, Muncer and Chadwick2015), showed that patients’ perception of HCPs’ compassion correlated with increased immune responsiveness, reduced hospitalizations, decreased intensive care utilization at the end-of-life, and better psychological adjustment for cancer diagnosis.
Alternatively, these findings could suggest that patients with higher symptom distress could be less able to perceive compassion from their healthcare providers. This has important clinical ramifications as it suggests that while patients with high symptom distress may seem less receptive to HCPs’ compassion, they may be in fact be those who need it the most.
Thus, there could be conditions that predispose patients’ ability to perceive compassion that extends beyond HCPs’ efforts and expressions of compassion. External conditions might include the patients’ personality, their disposition to psychosocial support, the clinical environment, and their sense of connection with others. As palliative care clinicians can attest, patients with acute suffering, especially those who are perceived as demanding, often require considerable compassion from HCPs. Based on the results of this study, this may be due in part to patients inability to perceive HCPs’ compassion due to symptom-related distress. This evidence may suggest that patients’ perceptions of compassion are dependent on having their psychosocial and physical needs met. Thus, a psychological intervention addressing psychosocial factors (personality traits, psychosocial support, sense of connection with others, etc.) could improve their reception of compassion, although further research is needed to investigate this hypothesis.
At the same time, HCPs could have varying levels of compassion for different reasons due to the ability to tolerate the suffering of a patient in pain, the burden and the lack of time and training. One of these reasons could be the “cost of caring” of clinicians frequently exposed to death and dying that could generate emotional exhaustion; the latter refers to the feeling of exhaustion due to the physical and psychological distress that mainly could occur in professionals who work for the public, such as HCPs (Gómez-Urquiza et al. Reference Gómez-Urquiza, Albendín-García and Velando-Soriano2020).
Relative to treatment, assuming the relevant role of compassion in healthcare, it is important to increase the attention to compassionate approaches. While the importance of compassion in healthcare is clear, currently, in Italy, the cultivation of compassion remains a largely personal endeavor with only 30% of palliative care professionals indicating they received formal training on the topic (Bovero et al. Reference Bovero, Adriano and Di Girolamo2023). Sinclair et al.’s (Reference Sinclair, Torres and Raffin-Bouchal2016c) grounded theory model, the Healthcare Compassion Model, could be an adequate starting point to implement specific teaching and training programs for palliative care professionals. Furthermore, since patients’ symptoms might play a role in compassionate care, there is a need to pay more attention to patient care to reduce his distress, for example through specific interventions such as dignity therapy, and individual meaning-centered psychotherapy (Breitbart et al. Reference Breitbart, Pessin and Rosenfeld2018; Chochinov et al. Reference Chochinov, Kristjanson and Breitbart2011).
This research has some notable limitations. The distribution among groups did not allow for the assessment of differences in the levels of compassion between the various health professions (nurses, oncologists, medical internists, hematologists, and social healthcare providers).
Moreover, not all of the patients’ healthcare providers were recruited, only those HCPs who agreed to participate which was quite low. This may have resulted in data bias and the recruitment of HCPs who were interested and skilled in compassion. Likewise, not all patients who received psychological support were recruited, only those who consented to participate.
Furthermore, as this was a cross-sectional study, this prevented the evaluation of the length of the clinician–patient relationship and prevented the assessment of how the duration of the relationship might impact compassion.
In addition, no validated instruments measuring compassion were used in the study. Thus, further research is required to develop validated instruments to assess compassion.
Finally, there is a need to conduct more studies to investigate the predisposition of compassion to patients and HCPs and to understand whether patients’ symptoms or whether specific HCP’s conditions influence compassion.
Promoting interventions on patients’ symptoms and implementing specific training on HCPs may improve compassionate care.
Conclusion
This study identified that compassion is a significant factor in patients’ perceptions of dignity and alleviating psychosocial distress. The reason for this could be due to patients’ predisposition to receive compassion and/or the failure of clinicians to provide adequate compassion to those who suffer. Regarding this latter point, progress in improving compassion in healthcare is impeded by the lack of formal training and valid and reliable measures. These findings might indicate the importance of continuing to investigate the correlation between these constructs. Exploring compassion at the end-of-life could encourage dignity-conserving care.
Acknowledgments
The authors thank all the healthcare providers and patients for participating in the study.
Author contributions
Andrea Bovero conceived the presented idea.
Irene Di Girolamo recruited data with supervision from Andrea Bovero, Rossana Botto, and Giuliano Carlo Geminiani.
Rossana Botto analyzed and interpreted data.
Irene Di Girolamo drafted the work and wrote the manuscript.
Andrea Bovero, Rossana Botto, helped Irene Di Girolamo to revise the work.
Andrea Bovero, Irene Di Girolamo, Rossana Botto, and Giuliano Carlo Geminiani did their final approval of the version published and are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. There is no one else who fulfills the criteria that have been excluded as an author.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sector.
Competing interests
The authors have no conflict of interest to declare.







