The atrial switch procedure was primarily invented for correction of parallel systemic and pulmonary circulation in patients with D-transposition of great arteries. This procedure, either by Senning or Mustard technique, corrects the circulation at the atrial level. Reference Talwar, Choudhary and Janardhan1 Following the advent of the arterial switch procedure and its widespread use in neonatal period, atrial switch operations are used only in limited number of D-transposition of great arteries patients presenting late with deconditioned left ventricle. Reference Rao2 Less commonly it is used in congenitally corrected transposition of great arteries as a part of a double switch procedure and in isolated ventricular inversion. Reference Talwar, Choudhary and Janardhan1,Reference Sebastian, Guleserian, Juraszek, Kane, Hamzeh and Forbess3 Very rarely, atrial switch operations are required in complex anatomical arrangements resulting in physiologically parallel circulation. Reference Das, Jayakumar, Young and Chan4 There are very few case reports on the atrial switch procedure in presence of anomalies of cardiac situs and systemic venous drainage. We present the case report of a two-year-old girl who was born with heart in the right chest with left atrial isomerism, common atrium, bilateral superior vena cavae, and interrupted inferior vena cava. There was supero-inferior arrangement of ventricles with concordant ventriculo-arterial connection. She was successfully operated with modified Senning procedure through left-sided atrium.
Case report
A baby girl was born at term following antenatal diagnosis of left atrial isomerism, criss-cross ventricular arrangement, and partial atrioventricular septal defect. Postnatal echocardiogram demonstrated left atrial isomerism, common atrium, interrupted inferior vena cava, and bilateral superior vena cava. Oxygen saturations were maintained at around 85% in air and she remained well and was discharged home. Detailed anatomical assessment by CT scan revealed a midline liver, left-sided splenunculi, dextrocardia, and left atrial isomerism with bilateral hyparterial (left) bronchial arrangement. Left superior vena cava (receiving the hemi-azygous vein as a continuation of interrupted inferior vena cava) was seen draining to left superior aspect of the atrial mass and right superior vena cava was opening inferiorly into middle of atrial mass separately from coronary sinus. Large hepatic veins drain to left side of the atrial mass. Unobstructed left and right pulmonary veins were joining the atrial mass posteriorly on either side. The ventricular arrangement was supero-inferior resembling criss-cross pattern of rotational abnormality. The right atrioventricular (tricuspid) valve was connected to superior morphological right ventricle. Ventricular-arterial concordance was demonstrated with the pulmonary artery crossing anteriorly from right to left. The left atrioventricular (mitral) valve was connected to inferior morphological left ventricle, giving origin to the aorta, which comes off posterior to the pulmonary artery and right ventricular complex with a left-sided arch (Fig 1, Fig. 2a, Fig. 3a).

Figure 1. Preoperative images- a. Chest X-ray showing dextrocardia and Midline Liver b. CT chest showing bilateral morphological left bronchial arrangement c & d. CT scan showing supero-inferior ventricular arrangement and ventriculo-arterial connection e & f. CT scan showing anomalous systemic venous drainage to common atrium. g & h. 3D reconstructed image anterior (G) and posterior (H) view showing dextrocardia with supero-inferior ventricular arrangement, systemic and pulmonary venous drainage. LV = left ventricle; RV = right ventricle; SVC = superior vena cava.

Figure 2. Intraoperative images- a. Intracardiac anatomy after left-sided atriotomy showing common atrium with left superior vena cava and hepatic veins draining into left-sided left atrium b. Creation of posterior wall of systemic venous baffle by unroofing right superior vena cava c. Formation of anterior wall of systemic venous baffle d. Completion of pulmonary venous baffle by suturing the left atrial free wall margin to pericardium. LSVC = left superior vena cava, PA = pulmonary artery, RV = right ventricle, LV = left ventricle.
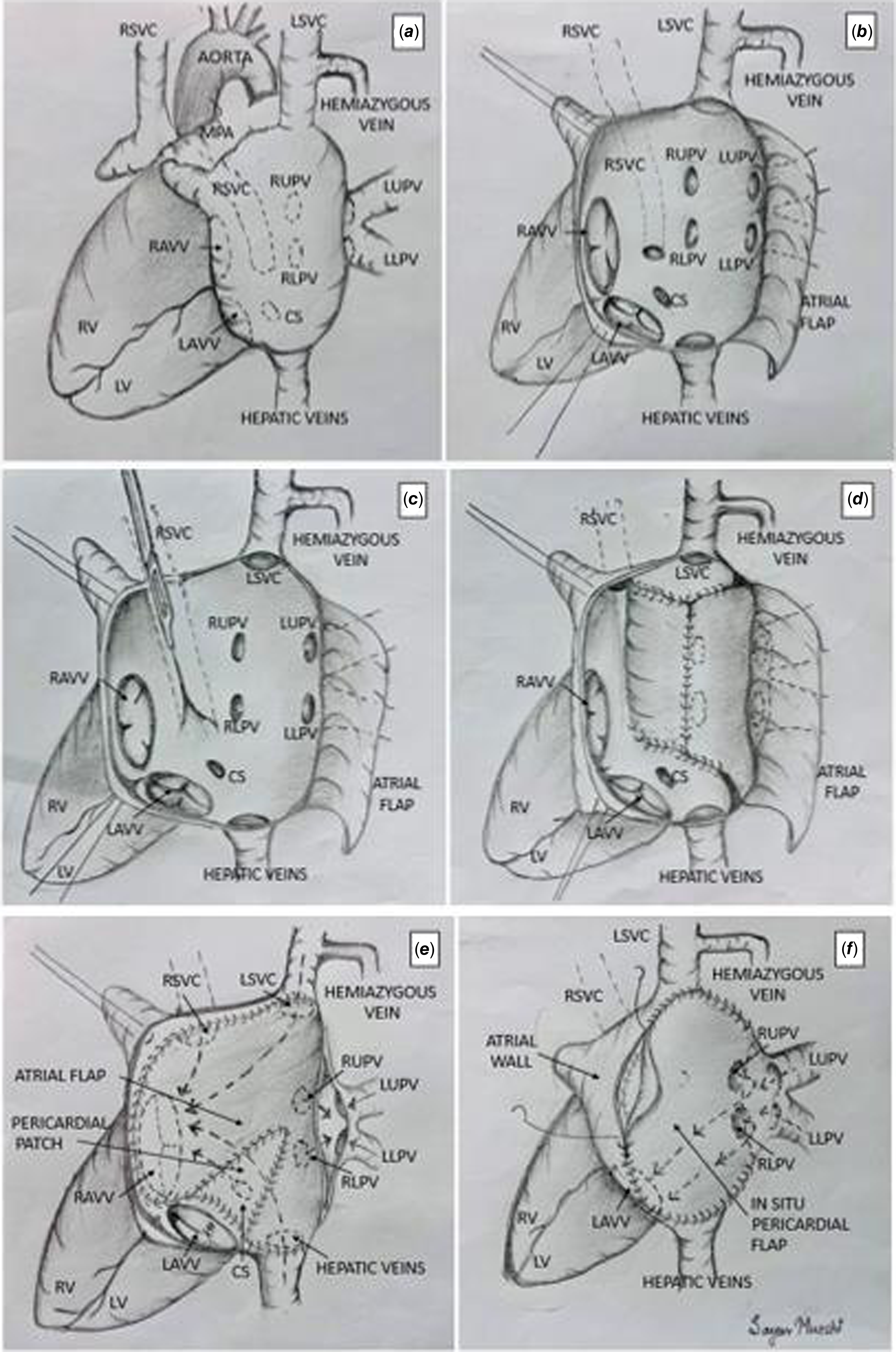
Figure 3. Schematic diagram for modified Senning procedure in dextrocardia with left atrial isomerism, and anomalous systemic venous drainage. RSVC = right superior vena cava; LSVC = left superior vena cava; MPA = main pulmonary artery; RUPV = right upper pulmonary vein; RLPV = right lower pulmonary vein; LUPV = left upper pulmonary vein; LLPV = left lower pulmonary vein; CS = coronary sinus; RAVV = right atrio ventricular valve; LAVV = left atrio ventricular valve; RV = right ventricle; LV = left ventricle.
Surgery was undertaken at 2 years of age through median sternotomy with both superior vena cava and hepatic vein cannulated for venous drainage. After aortic cross-clamping and cardioplegic arrest, an incision was made in the left-sided atrial wall, a few millimetres below the atrioventricular groove, and this was extended superiorly up to left-sided superior vena cava and inferiorly up to hepatic venous confluence. This was used as the anterior flap of the systemic venous baffle. Another incision was made anterior to the left-sided pulmonary veins and extended superiorly and inferiorly to harvest posterior wall of the systemic venous baffle, which was deficient as there was no inter-atrial septum. (Fig 3b). Right-sided superior vena cava was opening towards the left side of the common atrium with a thin wall separating it from posterior right atrial wall for a good distance. The wall was incised, rotated as the posterior flap, and anastomosed to the posterior margin of lateral atrial wall thereby completing the posterior wall of systemic venous baffle (Fig. 2b,c, Fig. 3c,d). The cleft in the left atrioventricular valve was repaired to achieve a competent valve. The anterior wall of systemic baffle was created by anastomosing the anterior free edge of the lateral atrial wall to the hepatic venous confluence and ran posterior to the left atrioventricular valve and anterior to the right atrioventricular valve to reach the left-sided superior vena cava. A piece of autologous pericardial patch was used to cover a deficiency in this layer (Fig 2c, Fig 3e). The incised wall of the left pulmonary veins was sutured to the adjacent pericardium, making the veins open into pericardial cavity. The pulmonary venous baffle was then completed by anastomosing the free wall of the left-sided atrium to the pericardium over left-sided superior vena cava as a Shumacker modification (Fig 2d, Fig 3f). The aortic cross-clamp was removed after thorough de-airing and heart regained in sinus rhythm. The cardiopulmonary bypass was weaned off uneventfully. Tans-oesophageal echocardiography showed unobstructed systemic and pulmonary venous baffles with good biventricular function and competent atrioventricular valves (Fig 4). The post-operative recovery was smooth and uneventful, and the child was discharged home.

Figure 4. Postoperative images- (a) & (b) post-operative echocardiography showing unobstructed systemic and pulmonary venous baffle with laminar flow.
Discussion
Heterotaxy syndrome is characterised by abnormal arrangement of the thoracoabdominal organs across the left-right axis of the body. It is an abnormality of the laterality where the sidedness is primarily determined by the morphology of the atrial appendage on each side. Reference Das, Jayakumar, Young and Chan4,Reference Jacobs, Anderson and Weinberg5 In left atrial isomerism or bilateral left-sidedness, there is duplication of left atrial appendage on either side. This condition is often associated with other cardiac anomalies like persistent left superior vena cava, pulmonary veins connecting bilaterally to the atria, interrupted inferior vena cava, and other intracardiac defects. Reference Uemura, Ho, Devine, Kilpatrick and Anderson6 In such conditions, detailed description of segmental anatomy in terms of veno-atrial, atrioventricular, and ventriculo-arterial connection is of utmost importance to understand the physiology of circulation and to determine the anatomical repair. In our patient, the three systemic venous channels were primarily draining into the left-sided left atrium, which was connected to the inferior morphological left ventricle through the left atrioventricular valve. The right-sided left atrium was connected to the superior morphological right ventricle through the right atrioventricular valve. In the setting of common atrium or deficient interatrial septum, there was adequate mixing of pulmonary and systemic venous drainage as the pulmonary veins were opening on either side of the common atrium. In the truest sense of the segmental anatomy, this condition is different from isolated atrial or ventricular inversion. Reference Sebastian, Guleserian, Juraszek, Kane, Hamzeh and Forbess3,Reference McElhinney, Reddy, Silverman and Hanley7 However, atrial switch procedure can be applied in such condition to achieve physiological correction of circulation.
In this patient, the surgical management was complex and technically difficult due to multiple factors. Firstly, the Senning procedure was undertaken through the left-sided morphological left atrium due to dextrocardia with small right-sided atrium. In presence of adequate right-sided atrium, Senning procedure can be undertaken in dextrocardia through the right atrium by displacement of heart into the widely opened left pleural space. But this approach is again technically difficult due to limited access to the atrium and inadequate exposure. Reference Talwar, Choudhary and Janardhan1 Secondly, three systemic veins were draining abnormally into the left side of the common atrium, which made the creation of systemic venous baffle challenging. Thirdly, there was lack of autologous tissue to reconstruct the systemic venous baffle due to absent interatrial septum. However, we preferred the Senning procedure due to potential for growth of the autologous tissue with less chance of long-term baffle obstruction. Reference Hörer, Herrmann and Schreiber8 This was achieved by using the intervening membrane between right-sided superior vena cava and common atrium to reconstruct the posterior wall of systemic venous baffle. Lastly, the supero-inferior arrangement of ventricular arrangement with abnormal position of the left and right atrioventricular valve further made the determination of suture line for anterior layer of systemic venous baffle difficult. Overall, the detailed understanding of the segmental anatomy is very important for reconstruction of unobstructed systemic and pulmonary venous baffles.
To conclude, atrial switch is technically difficult and challenging in congenital cardiac defects with abnormal situs and anomalous systemic venous drainage. We demonstrate successful modified Senning repair in a patient with dextrocardia, left atrial isomerism, common atrium, anomalous systemic venous drainage, and abnormal ventricular arrangement.
Acknowledgements
We are thankful to our colleagues from department of cardiac imaging for their support.
Financial support
None.
Competing interests
None.







