Duration of untreated psychosis (DUP) broadly refers to the time elapsing between onset of psychosis and treatment initiation. Its relationship with outcome has been intensely studied in the framework of the development of early intervention strategies for psychosis. Results of such research are however still a matter of controversy, some studies showing a negative impact of long DUP on outcome (Reference Clarke, Whitty and Browne1–Reference Schimmelmann, Huber, Lambert, Cotton, McGorry and Conus4) while others do not (Reference Craig, Bromet, Fennig, Tanenberg-Karant, Lavelle and Galambos5–Reference Malla, Schimtz and Norman8). In a systematic literature review, Marshall Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace(9) nevertheless concluded that there is a significant, albeit small to moderate, negative association between DUP and outcome, and most early intervention programmes rank reduction of DUP as a primary priority.
From a clinical point of view, reduction of DUP emerges as a logical target when witnessing the collateral damage suffered by patients who experience long delays prior to onset of care Reference McGorry(10). Additionally, recent imaging data have shown that the prodrome and the early phase of psychotic disorders are periods of active and progressive structural changes in key brain areas such as the hippocampus Reference Pantelis, Velakoulis and McGorry(11). If one assumes that there is an active process of neuroprogression underlying these changes, then the longer the DUP, the greater the time available for this potentially neurotoxic process to unfold Reference Berk(12). The nature of the pathogenic process remains to be fully elucidated; however, it probably includes reduction in neurotrophins, oxidative stress and inflammatory cytokines. Given the evidence that appropriate treatment is potentially neuroprotective Reference Lieberman, Tollefson and Charles(13), reduction in DUP could therefore be associated with reduction in potentially cumulative brain insult, and hence improvement in symptomatic and functional outcomes.
In the last few years, assessment of psychosis onset has been the object of a considerable attention, and this interest has led to both a degree of consensus about its definition and the development of scales specifically designed to determine the date of its initial occurrence Reference Singh, Cooper and Fischer(14,Reference Yung, Yuen and McGorry15). A closer look at this literature reveals on the other hand that criteria applied to define the endpoint of DUP, in other words the time of treatment initiation, is much less consistent and vary greatly between studies.
According to international guidelines, an adequate treatment of first episode psychosis should combine adapted medication (generally utilising low-dose strategy) and psychosocial intervention delivered in the context of easily accessible and specialised treatment teams (16–18). However, despite the availability of such guidelines, the concept of ‘treatment initiation’ usually refers to the commencement of very incomplete and often ill-defined interventions (Table 1). These include ‘initiation of medication’, ‘commencement of any form of treatment', ‘initiation of adequate treatment', ‘time of first effective treatment', as well as ‘hospitalisation’ or ‘entry to a specialised programme’. In addition, adherence to treatment is in the vast majority of cases not assessed when in fact clinical experience reveals that enrollment in a specialised service or prescription of medication does not necessarily equate with the person being fully engaged with the service, receiving sufficient psychosocial support, or taking medication as prescribed.
Table 1 Definitions of treatment initiation in the literature
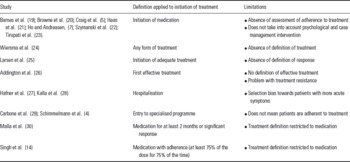
In the studies mentioned above, it is therefore highly likely that many patients for whom DUP was defined as having concluded actually remained untreated or partially treated. Only two studies defined treatment initiation on the basis of adherence to or observed response to medication treatment Reference Singh, Cooper and Fischer(14,Reference Malla, Norman and Manchanda30). However, by focusing on this aspect of treatment, they neglect the importance of psychosocial intervention in the recovery process Reference Malla and Norman(31), while recent randomised controlled trials have now clearly proven that integrated early intervention programmes that include specialised psychosocial treatment lead first episode psychosis patients to a better outcome than generic mental health programmes Reference Garety, Craig and Dunn(32,Reference Petersen, Jeppesen and Thoru33).
This lack of consistency in definition is concerning, considering that an absence of consensus on what ‘treatment initiation’ actually comprises could very well be one of the critical factors that so far limited the conclusiveness of studies exploring potential consequences of DUP. While research exploring DUP impact on outcome should not interfere with common sense arguments justifying the necessity of mental health services reforms aimed at facilitating treatment access for patients with psychosis Reference McGorry(10), conclusive research on DUP, based on valid data, would only provide more momentum to such a reform process.
It seems therefore timely to establish a clearer definition of what should be considered as the end of the DUP period. First, given that medication is a key element in treatment of the vast majority of first episode psychosis patients, antipsychotic treatment initiation should belong to the definition. However, adherence to treatment ought to be assessed as well and the medication criterion considered fulfilled only if patients have taken their treatment for at least 75% of the time during at least 4 weeks. Second, based on the above data supporting the efficacy of specialised treatment, end of DUP should be considered only when patients are well engaged in an early intervention programme. It is clear that psychosocial treatments remain inconsistently available, and subject to the vagaries of service, economic, training and resource variables, but this is precisely what research on the impact of DUP is all about: to show that adequate treatment provided early has a positive impact on outcome of psychosis. Once this point established, the argument to justify the need for a reform of mental health programmes and for an earlier access to adequate psychosocial and medication treatment in early psychosis would only be stronger. However, in order to supply evidence-based arguments to this debate, the definition of DUP needs to be applied with more precision.
Acknowledgements
Financial and material support: Dr Philippe Conus is supported by the Leenaards Foundation, Switzerland, and by a Visiting Scholar Award from Melbourne University, Australia.



