The scope of imaging
Radiology is constantly evolving in its clinical application, playing a central role in numerous patient pathways in health care. Advances in sophisticated technologies have extended the scope of its application to every organ, offering not only essential services in diagnosis, monitoring treatment, and predicting outcomes but more recently therapy in the form of interventional radiology. The result of these developments is that the volume of activity is continuing to grow in all imaging techniques (often referred to as imaging modalities).
The term “imaging” encompasses a number of diagnostic tests, some of which may be performed outside a radiology department. There is great variation among countries and by specialty in how these processes are undertaken and where.
Imaging was originally founded on the plain X-ray. Despite the development of newer techniques towards the latter part of the 20th century, the plain X-ray still plays an important role in diagnosis (although its role is often to rule out pathology, rather than for primary diagnosis) and its uses continue to grow. However, the newer modalities of ultrasound, CT and MRI are increasing at a more rapid rate. Figure 9.1 shows the increased activity in England in the last 20 years. This demonstrates a 3.6% compound growth in the last five years.
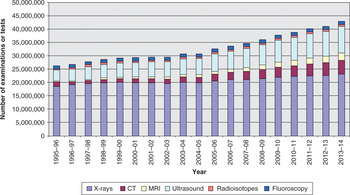
Figure 9.1 Total number of imaging and radiodiagnostic examinations or tests, by imaging modality, England, 1995–96 to 2013–14
Major growth can be observed in the more complex cross-sectional imaging techniques, with compound annual growth rates (CAGR) in the last 10 years of 10% for CT and 12.3% for MRI (see Table 9.1). There is slightly less growth recorded in ultrasound at 5.3%, but this may be an underestimate as a significant amount of ultrasound is now performed outside imaging departments and would therefore not be recorded in these figures.
Table 9.1 Compound annual growth rates (CAGR) for radiology modalities in England
| Modality | CAGR for past 5 years | CAGR for past 10 years |
|---|---|---|
| X-rays | 1.46% | 1.40% |
| CT | 9.13% | 10.05% |
| MRI | 9.70% | 12.32% |
| Ultrasound | 5.72% | 5.32% |
| Radio-isotopes | 0.25% | 0.70% |
| Fluoroscopy | 1.23% | 0.90% |
Although these figures are specific for England, a similar picture is seen throughout Europe and internationally. This growth is significantly in excess of that expected by demographic drivers and is predominantly due to the increased reliance on imaging particularly in areas such as cancer, vascular conditions (including stroke and cardiac disease), and trauma.
As well as the established diagnostic techniques, imaging continues to expand at pace particularly focusing on the concept of molecular imaging utilizing ultrastructural diagnostics, nanotechnology, and functional and quantitative diagnostics. The main example of this in current practice is the use of fusion imaging, which combines the structural information gained from CT (or MRI) with the functional information from positron-emitting radiopharmaceuticals in the form of positron emission tomography fused with computed tomography (better known as PET-CT). The result is the depiction of the spatial distribution of specific metabolic or biochemical activity with clear anatomical localization.
This improved image clarity and tissue differentiation in a number of situations has dramatically increased the range of diagnostic information, in many cases providing increased confidence in terms of underlying pathology. These fused images are vital tools in a number of clinical areas, notably cancer diagnosis and treatment, but they are also used in neuroimaging and cardiac imaging (Box 9.1).
Molecular imaging is rapidly gaining recognition as the future direction of imaging providing information of what is happening at the molecular/cellular level in terms of both structure and function. The main techniques currently in clinical practice utilize radiopharmaceuticals to provide functional information combined with traditional scanning techniques to provide structural information. However, there is active research into other techniques utilizing optical imaging for instance. The current research suggests that this form of imaging combined with genomics may be able to provide more personalized focused imaging in terms of earlier diagnosis, particularly in the field of cancer care, and allow more selective, effective treatment management.
One of the most significant changes in radiology in the last 20 years has not come from developments in imaging techniques. Rather, the technological advances in information technology (IT) have had a major impact on the way that radiology is currently practised. The days of viewing X-rays on sheets of film are in the past. These days, when images are acquired, they can be post-processed, manipulated and also transmitted rapidly not just within a hospital but also anywhere in the world as soon as they have been acquired. This technology, referred to as picture archiving and communication systems (PACS), has challenged the traditional model of patient, scanner and radiologist all located in the same site (Box 9.2). Images can now be reviewed and reported from remote locations, opening up options for different delivery models.
Box 9.2 Picture archiving and communication systems
PACS (picture archiving and communication systems) is a health care technology for the short- and long-term storage, retrieval, management, distribution and presentation of medical images. PACS allows a health care organization (such as a hospital) to capture, store, view, and share all types of images internally and externally.
A PACS has four major components:
imaging systems, such as MRI, CT or X-ray equipment
a secure network for distribution and exchange of patient information
workstations or mobile devices for viewing, processing, and interpreting images
archives for storage and retrieval of images and related documentation and reports.
PACS has been a major driver for changing the way imaging services are delivered. The electronic storage and transfer of images facilitates quick and easy access to images and reports. In addition it has allowed the radiologist to review the images at a site remote from their acquisition, giving rise to teleradiology as a new concept.
So far in this chapter, the emphasis has been on the diagnostic role of imaging. However, imaging can also be used to guide therapy, a specialty referred to as interventional radiology (IR) (Box 9.3). This is now established as an alternative to conventional surgery in numerous conditions, offering less invasive alternatives with improved outcomes, safety, and cost-effectiveness, as well as more patient-focused care. As such, IR is a vital component of hospital medicine, providing life-saving care, both in and out of hours. IR services have replaced or enhanced many surgical procedures as well as allowing new treatments for patients which were not previously feasible. Interventional radiologists are part of the multiprofessional teams treating a wide range of pathologies and working closely with surgical colleagues.
Box 9.3 Interventional radiology
The impact of interventional radiology
Aortic aneurysm: Rupture of the abdominal and thoracic aorta can be prevented and treated by the insertion of covered stents, which have largely replaced conventional surgery for this condition. In some cases these procedures are now carried out under local anaesthesia.
Gastrointestinal haemorrhage: Embolization therapy is increasingly performed by interventional radiologists for the control of uncontrolled bleeding from the lower and upper gastrointestinal tract. This life-saving procedure carries a much lower risk to the patient and in many cases is the treatment of choice.
Postpartum haemorrhage: Bleeding after childbirth remains the most common cause of maternal death and the role of IR in managing this emergency is well established.
Cancer: By using minimally invasive techniques, early cancers can be destroyed using radiofrequency or cryotherapy. Patients avoid the need for major surgery and long-term outcomes are very favourable. Newer techniques allow selective radiotherapy or chemotherapy for the treatment of liver lesions. Embolization can be used to devascularize tumours prior to surgical resection with resulting improvements in safety.
Early management of stroke: In the early stages of stroke the infusion of thrombolytic agents dissolves the clot and mechanical removal of blood clots can be performed to minimize disability and reduce the risk of death. Patients who suffer stroke from subarachnoid haemorrhage (bleeding around the brain) are now most frequently treated by interventional radiologists using embolization techniques.
Renal obstruction: Obstruction of the outflow from the kidney is frequently complicated by infection, which leads to septicaemia (infection in the bloodstream) and risk of death. Interventional radiologists are able to bypass the obstruction, for example through percutaneous nephrostomies.
The interconnections of imaging in the hospital setting
Imaging plays a significant role in most hospital-based specialties. The exact workload of an imaging department depends, to a certain extent, on the clinical specialties available within the hospital (e.g. neurosurgery, oncology).
In UK hospitals, A&E and general practice (direct access) are the specialties with the highest radiology demand, followed by Trauma and Orthopaedics, and this makes up approximately 50% of the activity. There is further demand from other specialities such as general surgery, general medicine, obstetrics and gynaecology, rheumatology, geriatrics, gastroenterology, cardiology, thoracic medicine, vascular surgery, ophthalmology, ENT, neurosurgery, neurology, paediatrics, oncology, psychiatry and intensive care.
The model of imaging provision varies throughout Europe. In many countries the hospital-based imaging department remains the main provider of imaging for emergency and urgent care, as well as planned care and community services. As discussed in the next section, in some countries the demand from primary care and from office-based practice is met by imaging services based off-site from acute hospitals.
In looking at new models of delivery, it may be more useful to consider where imaging plays a role in patient pathways and at what stage in this pathway imaging is best accessed. Table 9.2 is not exhaustive but lists the more common pathways and presentations relying on imaging.
Table 9.2 Common pathways and presentations relying on imaging
| Suspected or diagnosed cancer | Breast, brain and neuro-axis, head and neck, lung, oesophagus and stomach, colon and rectum, liver, pancreas, kidney and ureter, bladder, prostate, testes, ovary, uterus and cervix, lymphoma, musculoskeletal, melanoma |
| Cardiovascular disease | Chest pain, heart failure, pulmonary embolism, venous thromboembolism, aortic aneurysm, peripheral vascular disease |
| Respiratory disease | Chest infection/pneumonia, chronic obstructive pulmonary disease, restrictive lung disease |
| Head and neck | Deafness, balance disorders, tinnitus, sinus disease, thyroid disease, visual disturbances incl. field defects |
| Neurological conditions | Acute stroke, transient ischaemic attack, headache, epilepsy, multiple sclerosis, dementia, Parkinson’s disease and other movement disorders |
| Trauma | Head injury, fractures, chest and abdominal injury |
| Musculoskeletal | Back pain, myelopathy and radiculopathy, joint pain, osteoarthritis, rheumatoid arthritis |
| Pregnancy | |
| Genito-urinary | Renal failure, renal stone disease, renal tract obstruction, pelvic mass, pelvic pain, haematuria |
| Endocrinology | Hypertension, Cushing’s disease, adrenal disease |
| Surgical | Acute “surgical” abdomen, paediatric surgical conditions |
Diagnostic radiology does not just offer an image acquisition and reporting service. Radiologists work closely with their clinical colleagues to ensure that patients get the most appropriate investigation and that the interpretation of the report is understood in relation to the clinical context. In this role, the radiologist plays an important part in the MDT approach to patient care, which has been acknowledged as a significant factor in improving outcomes, particularly in cancer care (Reference MorrisMorris et al., 2006; Reference StephensStephens et al., 2006; Reference CooryCoory et al., 2008). This has led to the development of MDT meetings where clinical radiologists (who usually lead the meetings) with their diagnostic pathologist colleagues work alongside their clinical colleagues to decide the correct clinical plan for each patient. These diagnostic specialists aid surgeons and oncologists in developing appropriate care plans based on the staging of the cancer. In this function it is now common for the biopsy of the primary tumour to have been performed by a radiologist under imaging guidance aided by the pathologist’s interpretation. Figure 9.2 illustrates the extent of these MDT meetings in a typical large hospital.

Figure 9.2 Multidisciplinary team meeting (MDTM) participants
IR also interacts with a large range of clinical services, as illustrated in Figure 9.3. The patients treated by interventional radiologists may be inpatients on wards in the hospital, but more frequently are treated as day cases. Larger imaging departments may have their own day-case facilities, but if not, the IR service needs access to such a resource.
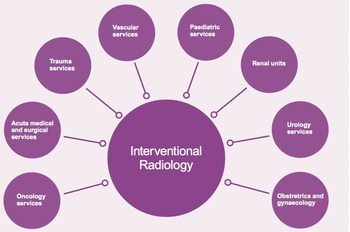
Figure 9.3 Interventional radiology interactions with hospital departments
Links with services outside hospitals
Patients access imaging services from a number of different situations, including:
hospital inpatients
outpatient services based in hospitals
consulting rooms outside hospitals
primary care doctors/health care professionals
self-referral.
Imaging activity referrals from outside the hospital setting are increasing significantly. This is influenced by a number of factors including a drive to earlier diagnosis of conditions such as cancer and heart disease (Independent Cancer Task Force, 2015), as well as the increasing capability to support patients to manage their health care outside the hospital. In areas such as plain X-ray and ultrasound the workload from primary care can often amount to over 50% of the imaging activity.
Although imaging is usually thought of as a tool to confirm a diagnosis, it is important to emphasize the role of the negative test in excluding significant disease. In many pathways early access to imaging can avoid unnecessary hospital outpatient appointments and, more importantly, unnecessary hospital admissions.
In many European countries there is direct access to imaging from primary care for all main modalities (i.e. CT, MRI, ultrasound and plain X-ray). This applies particularly to the field of musculoskeletal problems where there is high demand for MRI in the management of back pain and joint pain.
There are varying delivery models across Europe to meet these demands. In some countries the hospital imaging service also provides imaging services for referrals from outside the hospital, while in other countries much of this activity is provided in centres located outside hospitals either linked to or independent of the hospital departments. These centres may also provide services for “outpatient” imaging from specialists who work in office practice, notably in insurance- or private-based health care systems.
Workforce
There are two main clinical professions that deliver imaging in Europe: radiologists and radiographers.
A radiologist is a doctor who is also an imaging expert with specialized training in obtaining and interpreting medical images. As mentioned already, radiologists can also treat diseases by minimally invasive, image-guided surgery (interventional radiology). Like other doctors, a radiologist must first qualify as a doctor from an accredited medical school and spend a variable period in clinical practice. Following this, they will undertake further postgraduate training before qualifying as a radiologist (usually for a further five years in most European countries).
A radiographer (or medical imaging technologist) is a trained health professional whose primary role is to produce medical images that assist radiologists and other doctors to diagnose or monitor a patient’s injury or illness. In most European countries they have undergone training at degree level or equivalent followed by in-post further subspecialization. Some radiographers extend their role beyond that of image acquisition. This practice is more common in the United Kingdom than in most other European countries. Such activities include interpretation of ultrasound tests, mammography screening, and trauma plain film reporting.
The United Kingdom is probably the most advanced European country in developing a career progression in its radiology workforce through the development of four tiers of radiographer training and professional development. These include:
Assistant practitioner (not a trained radiographer): an assistant practitioner performs protocol-limited clinical tasks under the direction and supervision of a registered practitioner (radiographer).
Practitioner (state registered, degree educated): a practitioner autonomously performs a wide-ranging and complex clinical role, and is accountable for his or her own actions and for the actions of those they direct.
Advanced practitioner (state registered): an advanced practitioner, autonomous in clinical practice, defines the scope of practice of others and continuously develops clinical practice within a defined field.
Consultant practitioner (state registered): a consultant practitioner provides clinical leadership within a specialism, bringing strategic direction.
A smaller workforce of nurses, health care assistants, and physicists as well as administrative and clerical roles supports these two professional groups. The development of PACS is creating a key role for IT support.
The legislative and regulatory framework varies, particularly with ultrasound. For example, in many countries (including the United Kingdom), radiologists have little involvement in performing and interpreting obstetric ultrasound. The obstetric ultrasonographers may be radiographers who have trained specifically in this practice, but may also be obstetricians and midwives.
A similar picture can be seen, to varying degrees, in other specialties where clinicians have acquired their own ultrasound equipment and provide a focused ultrasound service to support their specialty interest, e.g. urology, orthopaedics, or vascular surgery. This practice is most advanced in cardiology, where the cardiologists have developed their own expertise to acquire and interpret images as well as carry out interventional procedures under radiological guidance. In the United Kingdom, for instance, the term echocardiography refers to ultrasound of the heart and is usually performed within the cardiology department by separately trained technicians under the supervision of cardiologists, while cardiologists, rather than radiologists, often report CT and MRI of the heart and great vessels. This may be carried out on separate dedicated scanners in large centres, but more commonly the radiographers in the main imaging department acquire the images.
Existing barriers to delivering optimal imaging services
As the role of imaging has gained greater importance in health care, there is a real challenge to respond to the increased demand due to a number of factors, which has led to significant variation in the use of radiology in Member States across Europe. Figure 9.4 illustrates the variation in CT and MRI activity across Europe.
The following challenges and barriers are thought to be the major influences on the current usage and effectiveness of imaging in Europe.
Evidence-based access to imaging
It is difficult to draw conclusions from a comparison of imaging activity between different countries, as there is a lack of evidence to indicate what the appropriate level should be and this will anyway vary with patterns of disease. In France and the United Kingdom, for example, national societies have developed evidence-based guidelines to encourage referring doctors to use imaging appropriately. These guidelines have been adopted by a number of other European countries with varying effectiveness (Reference RemediosRemedios et al., 2014; Royal College of Radiologists, 2016). The use of imaging tests involving radiation (CT, plain X-ray and nuclear medicine) is governed by European legislation in the form of the newly updated European Directive 2013/59/Euratom. This states, among other things, that all requests for such tests are “justified” by a responsible trained health care professional. The goal is to protect patients from unnecessary exposure to radiation. Despite this, there is evidence of an inappropriate over-usage of radiology in certain clinical situations. There is also likely to be overuse of MRI and ultrasound, although as these do not involve exposure to ionizing radiation, they are not governed by this regulation.
However, the concern does not just relate to possible over-usage of imaging. There is evidence suggesting the variation in cancer outcomes in Europe is partly due to variation in early access to imaging for diagnosis in suspected cancer.
Workforce issues
The marked growth in imaging activity in the last 10 years has been met with differing degrees of workforce expansion across Europe, but in most countries the increase in radiologists and to a lesser extent radiographers has lagged behind the growth in activity. The situation is most acute in those countries that started from a low base of radiologist per head of population. Figure 9.5 illustrates the variation in a number of European countries.
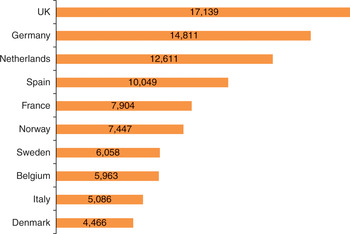
Figure 9.5 Number of inhabitants per radiologist, 2011 (including residents in training)
The situation with radiographers is not as acute, although in the United Kingdom, for instance, radiographers and ultrasonographers are included with radiologists on the government shortage occupational list for immigration purposes. This situation is mitigated somewhat by the United Kingdom approach to skill-mix, described earlier.
This shortage of radiologists is further compounded by the fact that they have developed additional roles, for instance in interventional radiology, the performance of biopsy techniques, and in their role in the MDT mentioned earlier. A recent survey from the European Society of Radiology found that 58% (out of 31 respondents) reported having too few radiologists for their current needs and 55% (out of 30 respondents) replied that they would not have enough radiologists in training to serve their respective nations.
In addition, there has been a drive to subspecialization with the increasing complexity of imaging techniques. This is creating a real challenge, particularly in smaller hospitals/services where it is proving increasingly difficult to provide an expert specialized opinion over seven days a week, throughout the year. Networking between hospitals is seen as a partial solution to this.
Equipment
There is also considerable variation in the equipment base across Europe. This is illustrated in Figure 9.6, which compares the provision of CT and MRI scanners in a number of European countries and international comparators.

Figure 9.6 Scanner equipment per million people in selected OECD countries, 2015 (or nearest year)
The international economic crisis has coincided with the recent rapid increase of imaging activity described earlier. This has significantly constrained the previous regular turnover of imaging equipment, resulting in a higher than usual amount of aged equipment, at a time when technological developments continue. This is leading to increasing levels of obsolescence.
This slow-down in equipment replacement is not only the direct result of shrinking budgets, but also the consequence of adaptive strategies leading to better use of resources. Radiology, based on highly technical hardware and diagnostic pathways, offers a fertile ground for workflow standardization resulting in productivity gains. Efficiency plans focus on a variety of measures including: merging of departments/hospitals, sharing of equipment, closing down excess capacity, policies for equipment upgrade, patient throughput optimization, and extension of opening hours. New equipment often offers improved imaging quality and reduced radiation exposure, due to the improvement of X-ray technology or to the substitution of non-ionizing technologies (e.g. MRI).
Funding issues
Within Europe, there are many different types of funding models for health care, mostly based on revenues from taxation or social insurance. There is also great diversity in how imaging is reimbursed. However, in the current economic climate, many facilities have faced substantial budgetary pressures, forcing reorganization of facilities, staffing arrangements, and equipment.
The reduction in budgets for radiology departments can give rise to a biphasic effect on volumes within a fee-for-service model. There can be an initial tendency to increase the volumes to compensate for the reduction in revenues resulting from the reduced procedural reimbursements, followed by a trend to reduce the volume of procedures requested, due to the attention paid to appropriateness.
In systems where there are global budgets, there is a tendency to increased utilization of low-cost techniques, such as ultrasound and plain radiography, to attempt to substitute for the higher costs of higher tech procedures, such as MRI and CT. This is one of the explanations for the disproportionate place of ultrasound and radiography in some countries, in comparison with more sophisticated imaging techniques.
Organizational constraints
As mentioned previously, there are varying models of imaging provision, which are influenced by a number of national and local drivers. The traditional model is that of imaging departments as part of an acute hospital and from this central base services are provided to the hospital and local community in terms of access to primary care requests. This has the advantage of centralization of high-cost equipment and skilled staff. However, the disadvantages include poor access for non-hospital patients and dealing with the competing agendas of acute/emergency care and planned/community care through one department. In many countries alternatives to this model have developed, ranging from provision of ultrasound services in primary care facilities, through mobile ultrasound, X-ray, CT and MRI services, to fully comprehensive planned care diagnostic centres (non-emergency) offering a full range of imaging services often alongside other health care activities (e.g. laboratory testing, consultation rooms, day-case procedures).
Hospital design and imaging service location
A key constraint to providing appropriate, responsive imaging services within a hospital is the location and design of the imaging department. Historically, the imaging department has usually been in one location with the possible exception of A&E, where there was provision for plain X-ray examinations.
As the role of imaging has developed as an integral part of the examination of the patient, the need to co-locate imaging equipment with certain clinical services has become essential. This can be solved relatively easily in the case of ultrasound but, in the absence of a new building, the relocation of MRI and CT scanners provides a considerable challenge. This is not just due to the problem of finding an appropriate space but is compounded by the specific radiation protection considerations for CT and equivalent safety considerations for MRI with its high magnetic field.
CT scanning should now be an integral service within an emergency department to deal with conditions such as acute trauma and stroke. In addition, as most inpatient scanning occurs within the first few hours of admission, it makes sense from both a patient-centred and efficiency approach to locate ultrasound, CT and MRI close to the admissions unit.
The problem is that many hospitals do not have a centralized admissions function and therefore the challenge of delivering this approach is often too great. This results in considerable movement of patients around the hospital, which at best results in a poor experience for the patients and at worst can delay management and in some situations raise safety issues.
There are similar drivers of patient-centredness and efficiency within the outpatient setting with an impetus to offer one-stop clinics, which include consultation, investigations, and sometimes treatment in one visit. Thus in certain specialties that are high users of diagnostics (e.g. orthopaedics, gastroenterology, gynaecology), it makes sense to ensure that imaging facilities are either in the clinic area or adjacent to it.
This need for co-location creates the challenge of ensuring an appropriate level of staffing for such equipment. To a certain extent the development of PACS has solved this problem for radiologist support, but there can still be considerable challenges for radiographer and technologist staffing with potential for redundancy of scanning time.
The future of imaging services
There is no evidence that the current increase in demand for imaging services is likely to reduce in the next five years. Recent work commissioned by Cancer Research UK suggests that the current increase in demand for CT, MRI and ultrasound will continue at the current rates (Reference Cancer ResearchCancer Research UK, 2015). Although there is less reliance on plain X-rays in certain areas of medicine, trauma and orthopaedics will continue to rely on skeletal plain films while the chest X-ray is unlikely to reduce in usage.
Research into the effectiveness of screening in ovarian and lung cancer will shortly be published. It is likely that this will suggest the introduction of screening programmes for at-risk patients. In lung cancer this would result in a further marked increase in CT of the chest.
One of the limiting factors to the expansion of the use of CT has been the risk of repeated radiation exposure, but the new generation of scanners has markedly reduced radiation levels. This is one of the drivers behind calls to evaluate lung cancer screening programmes and is likely to increase the use of CT in other presentations.
The usage of PET-CT will further increase in the next five years, predominantly in the area of cancer management, but the role of fusion imaging is likely to expand beyond cancer. One such area of expansion appears to be in neurological conditions, particularly dementia. Other forms of molecular imaging are most likely to remain as research tools in the next five years with no immediate plans for widespread use in clinical practice.
The scope of interventional radiology continues to expand. A proportion of IR has focused in the area of vascular disease. This will continue to expand with further applications in areas such as thrombectomy in the treatment of acute stroke. There is also likely to be a further major expansion in the use of interventional image-guided therapy in cancer care. This will extend beyond its established use in symptomatic relief and palliation. There are already a number of indications for its primary use in treatment (e.g. neo-adjuvant embolization, image-guided ablation and brachytherapy, trans-arterial chemo-embolization (TACE), selective internal radiation therapy (SIRT), and isolated perfusion chemotherapy).
The implication of current and future developments in imaging for the organization, management and design of the hospital in the mid-21st century
Although some of the functions of hospitals may change in the future, the management of emergency and urgent care will remain their primary focus. Imaging will continue to play a vital role in supporting this activity, with an increasing reliance on CT particularly for trauma and the acutely ill patient.
It is therefore important that the planning of imaging facilities is part of any planning of new emergency and admission departments in order to deliver timely, safe and efficient services. Imaging will also be required in high dependency areas such as intensive therapy units, high dependency units and certain wards. Thus, great thought needs to be put into hospital design to avoid inappropriate siting or unnecessary duplication of imaging facilities with resultant unnecessary redundancies.
It is likely, therefore, that imaging will no longer be housed in one department and consideration will need to be made in terms of staffing, particularly in facilities that need to be accessible 24/7. With the challenges of workforce supply, described earlier, it is essential that the efficient flow of patients through imaging is a key consideration in hospital design.
The challenge that imaging departments face in balancing the demands of emergency and urgent care with planned care could be addressed, but this is dependent on two main factors. The first of these relates to the future role of the acute hospital in dealing with planned care, particularly in the form of outpatient facilities. If these remain on the main hospital site, then there will need to be imaging provision alongside them, particularly where the concept of the one-stop visit is to be achieved.
The second factor is the demand for access to imaging from primary care. In this situation there is no need for the patient to attend the hospital and in fact there are definite advantages both to the patient and to the hospital if such visits can be avoided. This could be achieved by further development of imaging services outside hospitals. To make these cost-effective, they may need to be centralized in diagnostic centres for modalities such as CT and MRI, while ultrasound could potentially be delivered in GP surgeries if there is appropriate demand.
If such diagnostic centres were to be developed, they would also have the potential to provide an alternative facility for hospital outpatients, particularly if the diagnostic centres had facilities for consultations and minor procedures.
All hospitals that deal with emergency and acutely ill patients need access to interventional radiology. As with radiology, this must be available 24/7. Although the emergency work will require inpatient beds with full clinical support, there will also be a demand for planned procedures which can be performed on a day-case basis. Consequently, a facility that can deliver this should be located adjacent to the interventional suite. Although all hospital emergency Should this be ‘hospital emergency departments’ or ‘hospital emergency patients’? and inpatients will need access to interventional radiology services, it is unlikely that all acute hospitals of the future will have enough demand for such work to justify their own comprehensive funded service. The solution to this will be the development of various forms of network where either the patient is transferred to the experts (or possibly the experts travel between hospitals).
For radiology to continue to play a key role in health care it must be able to respond to the workforce needs and therefore adequate provision must be made for education and training.
Likewise for imaging to continue to develop and support health care in the future, adequate provision and funding of research involving imaging is essential and this is likely to be concentrated in larger hospitals. The provision of imaging is essential to much of medical research, particularly in the monitoring of new therapies. However, there is a need to carry out primary imaging research if the true potential of new technologies is to be achieved.
At present the radiology department remains predominantly the domain of the radiologist, but this is changing and there is no specific reason why other clinical specialists trained in imaging should not use imaging facilities (if possessing appropriate skills). If the case for this is established, then a coordinated imaging resource is far preferable to the growth of isolated services often with unused capacity and challenges of equality of access.
The opportunities and barriers to making this vision of the future a reality
As imaging continues to develop, it will remain heavily dependent on appropriate levels of workforce and equipment, but IT solutions have the potential to improve the efficiency of services. There are already electronic requesting systems in existence that are linked to evidence-based resources to aid the clinician in requesting the most appropriate test first time and avoiding unnecessary investigations and delays.
There is considerable interest and research into the use of artificial intelligence (AI) in the interpretation of imaging investigations. Although this is not yet at the stage of routine practice, it is likely that this will prove significant and may eventually substitute for radiologists in certain investigations.
As radiology increases in its complexity, it will be even more challenging for every hospital imaging department to employ enough radiologists to provide a comprehensive service throughout the week. One partial solution to this is the provision of efficient comprehensive PACS systems. This opens up options for transferring images in real time to radiologists outside the acquiring hospital. If used appropriately, this can facilitate the development of networks of expertise, which will support smaller hospitals and enable them to provide appropriate comprehensive services in a timely fashion. This can be particularly effective in the emergency situation, avoiding onerous rotas for small numbers of radiologists. An example where PACS can be used to provide support to such hospitals is that commonly seen in neuroradiology where a hub and spoke model often exists, with neuroradiologists supporting local radiologists with second opinions. There are also examples of network solutions where a group of subspecialized radiologists provide a service across a number of hospitals. In the emergency situation services now exist that offer radiologist reporting “out of hours”, removing the need for onerous on-call rotas for the local radiologists.
These solutions will not overcome the need for a significant increase in the radiologist workforce, but will help to ensure the effective use of radiologists.
There is an obvious need for this subspecialization radiological expertise within the hospital setting to provide expertise to the various clinical specialties that imaging supports. However, a great deal of radiology provision to primary care is of a relatively general nature and it will be important that adequate expertise remains to deal with this relatively large workload in a timely manner. Thus it will be important that radiology departments ensure that the development of subspecialization does not leave this important element of their work under-provided for. This is an area where the extended role of the radiographer may be a solution in some areas, particularly in the interpretation of the plain X-ray and in the performing and reporting of general ultrasound by sonographers. Some of their current work may be replaced by non-radiographer technologists working under their supervision.
Another challenge already mentioned is appropriate levels of imaging equipment. As there will be an increase in competition for space in existing hospitals, PACS also offers the solution to consider locating imaging equipment off the main site. This equipment, if sited effectively, could give better access to patients who do not require hospital facilities (e.g. outpatients and primary care patients). By decanting this work off the main site, it could have the added benefit of improving efficiencies in delivering inpatient imaging support.
Another issue to be considered, particularly in cross-sectional imaging (CT and MRI), is the increase in obesity in the European population. This has added another challenge to manufacturers who now have to consider increasing both the size of the machines and their weight limitations to accommodate the increasing number of patients who would not physically fit in the traditional scanners.
Finally, whatever innovative solutions are explored, these will not be effective unless an appropriate funding system is in place. This is obviously challenging in the current economic climate; however, there is no doubt that inadequate or inappropriate funding mechanisms have the potential to significantly hold back the effective use of imaging in the hospital of the future. It has to be realized that in many circumstances effective imaging services will deliver higher quality health care with efficiency savings elsewhere in the system, for example in reduced length of stay, avoidance of hospital admission, and reduction of unnecessary outpatient appointments.
Thus, it is essential that imaging services are an integral part of the planning of the hospital of the future to ensure that resources are used effectively and the potential improvements in both quality and efficiency of patient care are realized.