INTRODUCTION
In 2013 the Canadian Association of Emergency Physicians (CAEP) conducted an inaugural academic symposium to develop a list of recommendations to promote educational scholarship among emergency physicians in Canada.Reference Bandiera, LeBlanc and Regehr 1 - Reference Bhanji, Cheng and Frank 3 The resulting manuscripts emphasized the importance of educational scholarship among emergency physicians in Canada and outlined the systemic and institutional supports necessary to develop clinician educators. Subsequently, this was identified as an area of leadership for emergency physicians.Reference Gordon 4 , Reference Sinclair, Worthington and Joubert 5 Despite this success, it is challenging to begin conducting research in medical education.
Most residents and physicians in emergency medicine have familiarity with the critical appraisal of quantitative diagnostic and therapeutic trials. However, translating this familiarity into research success remains challenging.Reference Perry, Snider and Artz 6 This is especially true in medical education, where biomedical methodologies are often proposed to study questions that are more appropriately investigated using techniques developed in the social sciences.Reference Schuwirth and van der Vleuten 7 The perception that medical education research is “easy” relative to clinical research also persists,Reference Schuwirth and van der Vleuten 7 despite the availability of numerous masters and PhD level programs focused on preparing trainees to conduct rigorous medical education research.
Herein, as part of a series of writer’s guides aimed at residents and junior scholars, we describe a scoping reviewReference Arksey and O’Malley 8 of the literature that outlines a list of recommendations for conducting and publishing quantitative educational research. In addition, we present a list of guidelines that establish the reporting and writing standards relevant to this field. We hope that this writer’s guide will aid junior investigators as they conduct quantitative research in medical education.
METHODS
Search methodology
The authors conducted a focused literature review of three databases. An initial search using the MEDLINE database was restricted to English-language articles published from 2006 through January 2016 using “and/or” combinations of the following search terms: “research design,” “quantitative,” “quantitative methods,” and “medical education.” A second search using ERIC database was performed of English language articles published from 2006 through January 2016 using “and/or” combinations of the following search terms: “research design,” “quantitative,” “quantitative methods,” and “medical education.” A final search was conducted using Google Scholar, which was limited to English-language papers from 2006-2016 using the keywords “medical education” and “quantitative research.” These articles were amalgamated in Mendeley, and duplicates were removed.
Inclusion criteria
Articles focused on quantitative research in medical education that outlined reporting guidelines, discussed the evaluation of quality in quantitative research, or provided advice on conducting quantitative research. Articles that focused on other forms of education scholarship, mixed methodologies, or did not address any of the study questions were excluded.
Article review
The results of the literature search were uploaded into Mendeley for analysis. Two authors (BT, PC) developed and performed the literature search and conducted the title and abstract review. The first 30 articles were reviewed in parallel to calibrate the reviewers. The subsequent 70 articles were reviewed separately, but in parallel. A kappa value was calculated to quantify inter-rater reliability. The remaining articles were then divided between the two authors (BT, PC) and reviewed by a single reviewer. A hand search of the reference lists of the included articles was conducted to identify those that were not found in the literature search.
A full text review of the included articles was conducted by two authors (BT, PC) with disagreements resolved through a discussion resulting in consensus. During the full text review, any quality evaluation criteria or reporting guidelines mentioned in the papers were abstracted along with recommendations for the conduct of quantitative medical education research.
Analysis
During the full text review, a list of quality markers was developed by two reviewers (BT, PC) by extracting recommendations mentioned in text, figures, charts, diagrams, pictures, or tables. These recommendations were annotated and organized by article from which they were extracted. Two authors (BT, PC) performed a simple thematic analysis refining and aggregating the recommendations into a final common list. Items deemed alike were amalgamated into a single descriptive statement (Table 1). Simultaneously, during the full text review, reporting guidelines and quality assessment tools that were relevant to quantitative research and were mentioned in the text, figures, charts, diagrams, pictures, or tables were extracted and compiled.
Table 1 Results of the qualitative analysis of literature-based recommendations for the performance of quantitative medical education research
RESULTS
Scoping review
The results of the literature review are outlined in Figure 1. The database search identified 356 articles (270 from Medline and 88 from ERIC with 2 duplicates), of which 46 were included on title/abstract review. The Google Scholar search conducted on January 18, 2016 returned 895,000 results. Of the 250 which were reviewed, 7 were included on title/abstract review. An additional 8 articles were included from a review of the references of the included studies.
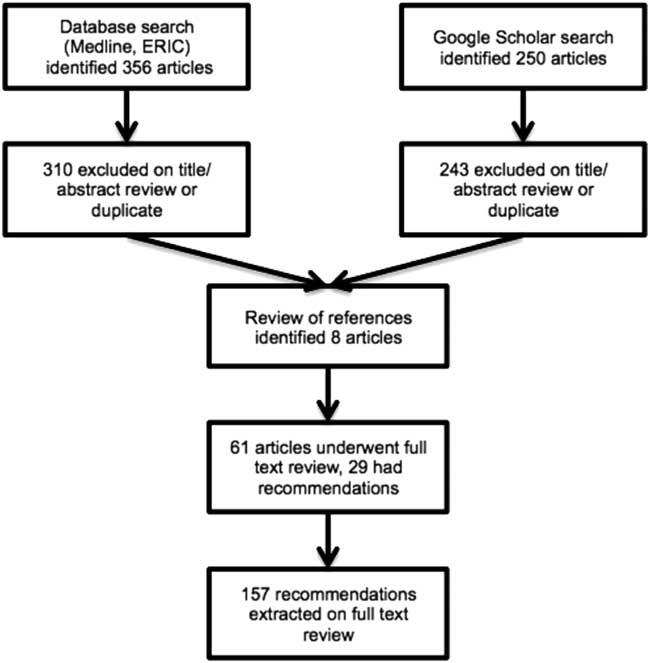
Figure 1 Flow diagram for systematic review.
The title/abstract review of articles 31 to 100 resulted in concordance on 97.1% (68/70) of the items with a kappa of 0.935 (95% CI=0.847-1.0). The full text review excluded an additional 32 articles; 157 recommendations were extracted from the remaining 29 articles.
Thematic analysis
The simple thematic analysis of the recommendations for quantitative medical education research resulted in 3 themes (study design, writing, and submission), 14 categories, and 86 items (see Table 1).
Quality evaluation tools and reporting guidelines
Table 2 outlines the fourteen quality evaluation tools and reporting guidelines that were found during the full text review, which were applicable to quantitative medical education research.
Table 2 Summary of reporting guidelines and quality assessment tools relevant to quantitative medical education research
*AEM Score = Academic Emergency Medicine Score, MERSQI = Medical Education Research Study Quality Index.
DISCUSSION
Our scoping reviewReference Arksey and O’Malley 8 identified 86 recommendations for conducting and 14 tools/guidelines for reporting high-quality medical education research using quantitative methods. The recommendations found in the literature were congruent; however, their usefulness will be limited by the high number of items that were found. Although the qualitative analysis decreased the gross number of recommendations substantively, 86 may still be too many to consider. Regardless, we believe that reporting the complete list will be helpful to both inform future research and allow junior researchers to identify those items most pertinent to them. Moving forward, we will aim to triage the recommendations to determine which are the most important so that those can be focused on. Multiple methods of achieving consensus among diverse populations have been proposed and could be applied to identify the most important recommendations.Reference Hsu and Sandford 23
A significant number of quality evaluation criteria and reporting guidelines were found that were applicable to quantitative medical education research. Whereas some of these tools are quite broad,Reference Lo, Mertz and Loeb 13 covering quantitative research in general, others are extremely specific, outlining specifically how to report quantitative medical education research using a specific methodology.Reference Cohen, Mcgaghie and Wayne 16 Because these guidelines outline the criteria for identifying and producing high-quality research, they should serve as a starting point for junior medical education scholars who are designing quantitative studies. We anticipate that these scholars will know what type of quantitative research that they are conducting and quickly identify the most relevant tools for their work using Table 2.
Although this work is likely to provide a helpful starting point for junior researchers, the complexity of medical education research is such that no advice or sets of guidelines can replace formal training in research methodologies nor advice from experts in the field.Reference Perry, Snider and Artz 6 , Reference Sherbino 24 Indeed, as the depth and scope of quantitative research in medical education continue to grow, increasing amounts of expertise and/or collaboration with skilled partners will be needed to produce high-quality, publication-worthy scholarship.Reference Sherbino 24
LIMITATIONS
Although our literature review returned a reasonable number of articles for review, the restrictiveness of the search could be criticized. We believe that the databases and search terms that were selected were appropriate for the topic of interest and, given that medical education research has advanced substantially in the past decade, restricting the review to articles published within the last 10 years allowed more modern and applicable lists of recommendations and reporting guidelines to be identified. However, in limiting the search to the English language, we likely missed literature that could have added to our findings.
CONCLUSION
In this paper, we attempted to provide guidance for junior researchers and authors in the form of key recommendations and reporting guidelines. We achieved this through a scoping review of the literature and thematic analysis, with a focus on quantitative educational research and scholarship. We believe that these results will assist junior researchers who heed the recommendations and guide them to key tools for their type of research.
Competing interests: None declared.





