Introduction
Regular exercise has a range of recognised benefits for physical health and mental well-being, both in terms of treating and preventing ill health. Government guidelines for adults recommend at least 150 min of moderate intensity activity each week (Department of Health, 2011), yet, according to the 2012 Health Survey for England report – the latest report with a specific chapter on physical activity – only 66% of men and 56% of women achieved these levels (Scholes and Mindell, Reference Scholes and Mindell2013). As a result, physical activity has continued to remain high on the government’s public health agenda. For example, tackling physical inactivity is a key strategy for delivering on many of the seven priorities identified by Public Health England to tackle the behaviours that increase the risk of poor mental and physical health (Varney et al., Reference Varney, Brannan and Aaltonen2014). A legacy commitment from the London 2012 Olympic and Paralympic Games is to increase the number of adults taking at least 150 min of physical activity a week and to reduce the number taking <30 min/week, year on year (Her Majesty’s Government, 2014).
Exercise referral schemes are one of the main routes through which exercise therapy is delivered in primary care in the United Kingdom [National Institute for Health and Clinical Excellence (NICE), 2006a]. There are different models of practice but they typically involve a primary care or allied health professional referring a patient to a dedicated exercise professional who designs a formal exercise programme tailored to the patient’s fitness level, motivation, and goals. The programme usually takes place within a leisure facility or gym over 10–12 weeks and is offered at a subsidised cost to encourage participation (Department of Health, 2001; BHF National Centre, 2009). Structured exercise programmes of this nature are appealing because of their capacity to offer safe and tailored physical activity in a supervised setting and because adherence can be more easily demonstrated than with lifestyle interventions (Richardson et al., Reference Richardson, Faulkner, McDevitt, Skrinar, Hutchinson and Piette2005).
Notwithstanding their popularity, adherence rates on the schemes are typically low and many participants fail to complete the scheduled sessions (Williams et al., Reference Williams, Hendry, France, Lewis and Wilkinson2007). This is particularly true of people referred with a mental health diagnosis, and research shows that while they may have similar initial rates of uptake as other participants, they are more likely to drop out (Crone et al., Reference Crone and Guy2008). Several studies have sought to investigate a range of issues in this group such as their initial uptake, subsequent participation and adherence, motivation to attend, perceptions about the schemes, and barriers to participation (Crone et al., Reference Crone, Smith and Gough2005; Crone and Guy, Reference Crone, Johnston, Gidlow, Henley and James2008; Myron et al., Reference Myron, Street, Robotham and James2009). While these have provided useful insights, the reasons for the high drop out rate still need to be better understood (Crone et al., Reference Crone and Guy2008).
A common feature in many exercise referrals schemes is that people with mental health problems often comprise a low proportion of those who participate. This can present a challenge for robust statistical investigation and may partly explain why not much is known about whether and how people referred for exercise on account of mental health problems differ from those referred for physical health problems. Of particular interest is whether any identified differences might advance understanding of the differing rates of adherence in the two groups; the main research question this study aims to address.
We report the results of a retrospective register-based analysis of Healthwise, an exercise referral scheme in the inner city London borough of Greenwich. While the scheme participants were mostly people with a range of physical health conditions, a relatively high proportion, 20%, were referred with a primary mental health diagnosis. Participation and adherence rates were high compared with similar schemes: 1089 participants were enrolled between January and December 2007, adherence was 58% at 13 weeks (the average duration of typical schemes), and 45% completed the full course duration of 20–26 weeks of regular exercise. This contrasts with a pooled adherence level of 49% reported from a systematic review of studies (Pavey et al., Reference Pavey, Taylor, Hillsdon, Fox, Campbell, Foster, Moxham, Mutrie, Searle and Taylor2012). Main results from the whole cohort have been reported elsewhere (Tobi et al., Reference Tobi, Estacio, Renton, Yu and Foster2012). This paper illuminates the distinctive socio-demographic features of mental health participants, comparing them with those referred for physical health conditions, and exploring associations with exercise adherence in both groups.
Method
Study setting
Healthwise was formed in 2005 as a partnership between the local council, local health authority, and a commercial provider of leisure services. It was aimed at adult residents with, and at risk of, physical and mental health illnesses for whom exercise therapy could be beneficial in terms of weight loss, improved fitness, and reduction in symptoms or risk. It also targeted people from a Black and Ethnic Minority (BME) background, who formed an estimated 29% of the borough’s population and, as a group, experienced worse health inequalities (Greenwich Teaching Primary Care Trust, 2008).
Referrals were made from general practice (GP) surgeries in the borough to a leisure facility where participants were enrolled on a supervised, tailored exercise programme over a period of 20–26 weeks. This duration was double the length of most other schemes which generally last about 10–12 weeks (BHF National Centre, 2009). The referrals represented a wide range of clinical conditions distributed across six broad categories (Table 1). Participants attended motivational and educational classes and had access to a range of courses including group exercise, healthy walks, gym-based sessions, water workouts, and swimming. Physical and physiological assessments were performed at enrolment and at seven, 13 and 20–26 weeks.
Table 1 Clinical referral categories of participants

Programme data
All records entered in the scheme register between 1 January and 31 December 2007 (n=1089) were extracted. Using a 12-month time frame cancelled out the effect of seasonal variations in exercise levels (Ma et al., Reference Ma, Olendzki, Li, Hafner, Chiriboga, Hebert, Campbell, Sarnie and Ockene2006; Tucker and Gilliland, Reference Tucker and Gilliland2007). We excluded 322 cases that were still in progress at the time and another 66 cases that were ineligible for other reasons (did not qualify, did not start, missing data on key variables). The final cohort (n=701) was separated into mental health (n=141) and physical health (n=560) groups. The latter was composed of all the non-mental health categories described in Table 1.
Primary outcome
Adherence was the main outcome measure for this study and determined by both the frequency and duration of attendance. The justification for this definition is detailed in Tobi et al. (Reference Tobi, Estacio, Renton, Yu and Foster2012). We defined adherers as participants who attended at least 80% of their scheduled sessions and had records of two progress assessments at the midpoint (13th week) and end (20–26th week) of the programme. Non-adherers were those who attended <80% of sessions and/or failed to undergo any of the two assessments. The 80% cut-off point was based on participant data analysed in an earlier study (Gidlow et al., Reference Gidlow, Johnston, Crone, Morris, Smith, Foster and James2007).
Process measures
Explanatory variables were selected from the participant register and included age, gender, ethnicity, occupational group, medical reason for referral, blood pressure (BP), height, and weight. Body mass index (BMI) at enrolment was computed from height and weight measurements. Although BP and BMI were measured as continuous data, we also categorised them to reflect recognised clinical cut-off points. Accordingly, BP at enrolment was classified as normal if the systolic (SBP) and diastolic (DBP) readings were <140 and <90 mmHg, respectively, or high if either the SBP was ⩾140 or DBP ⩾90 mmHg (NICE, 2006b). BMI was categorised as healthy (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (⩾30 kg/m2) in line with national guidance (NICE, 2005). Each participant was assigned an Index of Multiple Deprivation (IMD) score based on their postcode address. The IMD is a composite measure of relative deprivation in small areas of England called Lower Super Output Areas and uses the scores for the areas to rank them from 1 (most deprived) to 32 482 (least deprived) (Office of the Deputy Prime Minister, 2004).
Data analysis
After exploratory analysis to ascertain completeness of the data and normality of the distribution, analysis was done in three steps. Bivariable analysis was carried out to first explore differences between the mental health and physical health sub-cohorts (step 1) and then between adherers and non-adherers within each group (step 2). We used the χ 2 test to compare categorical variables and the t test for continuous variables. In the final step, binomial logistic regression was used to estimate the effect of factors associated with exercise adherence at group level. Significant multicollinearity and interactions were excluded before fitting all covariates that demonstrated association with adherence at the 20% level into regression models. The Hosmer–Lemeshow test was used to check overall model fit. Principal analyses were presented with three key statistical items – point estimate, confidence interval, and P-value – in line with reporting guidelines (Peacock and Kerry, Reference Peacock and Kerry2006; Vandenbroucke et al., Reference Vandenbroucke, von Elm, Altman, Gøtzsche, Mulrow, Pocock, Poole, Schlesselman and Egger2007). All analysis was done with PASW Statistics 18.
Results
Characteristics of participants
Table 2 presents the socio-demographic characteristics of participants with physical and mental health conditions. Compared to those with physical health conditions, mental health referrals were more likely to be younger (41.3 versus 47.4 years, P<0.001) and white (71 versus 61%, P=0.03). The profile of occupational categories in the groups also differed significantly (P<0.001). Proportionally twice as many mental health than physical health participants were unemployed (61 versus 33%) while the ratio was reversed among those who were retired (9 versus 20%). Only in managerial/professional roles was there some parity (10 versus 12%).
Table 2 Comparative profile of participants
IMD=Index of Multiple Deprivation; BMI=body mass index; BP=blood pressure.
a t Test.
b χ 2 Test.
The two clinical measures of health state captured in the data set were BMI and BP. Although mean BMI was significantly lower in mental health referrals (30.8 versus 32.5 kg/m2, P=0.01), the average value in both groups fell within the range of obesity. Mental health participants had a lower proportion of people with high BP (33 versus 45%, P=0.01), but were also less likely to maintain attendance over the duration of the scheme (38 versus 47%, P=0.04).
Factors associated with exercise adherence
The same variables in Table 2 were further used to explore adherence-related factors within each group (Table 3). Among mental health referrals, exercise adherence was more likely in participants with an elevated baseline BP (43 versus 26%, P=0.03). With physical health participants, those more likely to adhere were older (49 versus 46 years, P=0.002), unemployed (27 versus 39%), or retired (26 versus 15%, P=0.01).
Table 3 Group-level factors associated with exercise adherence
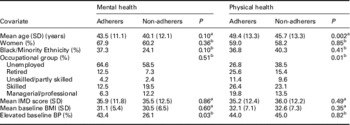
IMD=Index of Multiple Deprivation; BMI=body mass index; BP=blood pressure.
a t Test.
b χ 2 Test.
Table 4 shows the result of regression models for the two groups. We used associations with adherence at P<0.20 significance level to select covariates to build the models. Accordingly, age, ethnicity, and BP were fitted to the mental health model, and age and occupation to the physical health model. While no covariates were found to be independently predictive in the mental health group, occupation was associated with adherence in the physical health group where the odds of retired participants adhering were almost twice those of unemployed participants after adjusting for age (OR=1.85; CI=1.00–3.43; P=0.05).
Table 4 Adjusted odds ratios (OR) for exercise adherence

CI=confidence interval; Ref.=reference category.
Discussion
Although there has been a sustained growth in the number of exercise referral schemes in the United Kingdom since 1990s, inadequate monitoring and participating profiling has limited efforts to better understand who these schemes are accessible to and suitable for. Consequently, the importance of more appropriate targeting at the point of referral as a means of improving participation rates has been highlighted (Department of Health, 2001; James et al., Reference James, Johnston, Crone, Sidford, Gidlow, Morris and Foster2008; BHF National Centre, 2009). The need to understand these factors is especially important among groups with lower participation rates for whom the schemes may be ill designed or even inappropriate. In the case of mental health participants, the growing use of exercise therapy in the mental health service, including in people with serious mental illness (Ellis et al., Reference Ellis, Crone, Davey and Grogan2007), has given added impetus to efforts to develop more evidence-based practice.
Several factors may explain the comparatively lower numbers of mental health referrals. One reason may be that the schemes have traditionally been designed to deal with physical health conditions (Directorate of Health Promotion, 2003) and so naturally tend to recruit participants with these problems. Questions have also been raised about whether health professionals refer inappropriately. Health professionals are known to make subjective judgements about which patients might be most motivated to adhere (Din et al., Reference Din, Moore, Murphy, Wilkinson and Williams2015). Furthermore, their referral behaviour may be influenced by perceptions about the strength of the evidence, notwithstanding that associations between exercise and mental well-being have been repeatedly recognised for many years (Stathopoulou et al., Reference Stathopoulou, Powers, Berry, Smits and Otto2006). Whatever the reason, low numbers of mental health participants has meant that few studies have been able to undertake any robust analysis of this group from a quantitative perspective. Our participant cohort was different in this respect, having a relatively high proportion (20%) of mental health referrals.
Our analysis found that participants referred with a primary mental health condition were more likely to drop out of the ERS, consistent with findings elsewhere (Dugdill et al., Reference Dugdill, Graham and McNair2005; Crone et al., Reference Crone and Guy2008). Older age and poorer physical health are factors typically associated with lower levels of physical activity in the general population (Craig et al., 2009) and, presumably, adherence. But the mental health cohort were comparatively younger and, given their lower mean BMI and lower proportion of people with elevated BP, arguably in better health than the physical health group. So, even though it might reasonably be inferred that they would be more likely to maintain attendance, that was not the case. The sole factor that was significantly associated with adherence among the mental health group was an elevated BP at the time of enrolment, which may possibly have acted as a motivation to adhere to the exercise regime. However, when age and ethnicity were taken into account, the association was no longer apparent. BMI, the other clinical measure of health state, did not show any relationship.
The proportion of BME participants in the mental health group was significantly lower than in the physical health group (although similar to that of the general population in the borough). However, without information about rates of mental ill health among different ethnic groups in the primary care patient pool from which participants were referred to the ERS, it is difficult to infer any significance to this. But studies of mental health services for BME people highlight variations in the referral practices of GPs and their perceptions about who might benefit from the scheme. This can manifest in different ways such as the tendency for services to medicate BME patients in preference to other forms of therapy or a lack of cultural competence making misdiagnosis and inappropriate treatment more likely (Bhui et al., Reference Bhui, Warfa, Edonya, McKenzie and Bhugra2007; Fountain and Hicks, Reference Fountain and Hicks2010). Ethnic disparities in health care access, both in mental health and other service areas, continue to remain a significant scientific and policy challenge and focus of health services research.
Although information about levels of motivation at enrolment was not available to us, lower levels of adherence among individuals with mental health problems may relate to the nature of many mental health problems themselves being associated with poor motivation. People with depression will experience lack of energy and no longer experience the enjoyment they once did while exercising or undertaking a range of daily activities (Seime and Vickers, Reference Seime and Vickers2006). This is particularly the case for those with long-term conditions. They often need a more supportive or even assertive approach to adhere to social interventions aimed at improving their quality of life. However, people with anxiety-related disorders may seek to avoid social situations, such as the group-based activities within the programme, which might exacerbate their anxiety. Ironically, these group activities are supposed to serve as a means of providing the added social support these participants are known to require.
Attention needs to be drawn to the policy context in which the programme was implemented and its potential influence on outcomes. Few ERS studies address the influence of the wider context of service delivery to explain adherence outcomes, but this can be important. Healthwise was developed as part of a broader strategic agenda to tackle local health inequalities and the referral policy prioritised BME participants who for the most part suffered worse health outcomes. If any targeted support was given to them in the programme, then it could contribute to the higher adherence rates seen in the physical health group where there was a comparatively higher proportion of BME participants.
Finally, our analysis relied exclusively on the routinely collected demographic and physiological data, but it is difficult to reach any firm conclusions about the absence of variation in attendance in the mental health referral group, solely on this basis. Participation in activities is a complex behaviour that, useful as it is, quantitative data can only present a partial picture of. Evidence from qualitative research plays a vital role in describing the processes that influence people’s physical activity behaviour (Mckenna and Mutrie, Reference McKenna and Mutrie2003). Qualitative research is particularly useful in understanding the experiences, psychological and social influences, and contexts that enable, support, and sustain physical behaviour, or otherwise constrain it. Qualitative ERS studies have been conducted, including research in relation to mental health participants, but the still limited understanding suggests a place for mixed method studies that combine both quantitative and qualitative perspectives. Physical activity research papers based on mixed methods are increasingly appearing in the literature as researchers recognise the added value they can bring (Thomas et al., Reference Thomas, Silverman and Nelson2015).
The study had several limitations. Although we used a 12-month time frame in an attempt to adjust for seasonality effect, this may not have been sufficient. It is possible, for instance, that people with mental health conditions are more commonly referred during the winter months when these conditions are often exacerbated. Reliable data on the time of referral to the ERS were not available. The physical health of individuals with mental health illness is often poor, with many being overweight or obese, having hypertension, diabetes, or dyslipidaemia, and at significant risk of developing cardiovascular disease or other comorbidities. Similarly, people with physical health conditions may also experience depression, stress, and other common mental disorders. By disaggregating the groups only on the basis of their primary medical diagnosis without considering comorbidities, this confounder was not accounted for. We were also not able to verify the accuracy of the referral diagnosis. Another problem was the limited participant information available. Factors such as levels of physical activity and motivation at the start of the programme are known to influence adherence to exercise, and several studies (Bock et al., Reference Bock, Albrecht, Traficante, Clark, Pinto, Tilkemeier and Marcus1997; Marshall and Biddle, Reference Marshall and Biddle2001) have applied models of motivational readiness for behavioural change to explain the process of exercise adoption and maintenance. Finally, given that Healthwise operated in a primary care setting, all the mental health participants were diagnosed with common mental disorders (anxiety, depression, stress). The results will not necessarily be the same for people with serious mental illness.
Conclusion
This retrospective study of an exercise referral scheme highlights the differences between participants with a primary mental health diagnosis and those with physical health ones. It provides useful insights, previously unavailable, into the differing rates of adherence in the groups. The information can guide service commissioners and providers in developing strategies to maintain exercise tailored to the unique characteristics of the different participant groups.
Acknowledgements
The data analysed in this study were taken from an evaluation of Healthwise funded by Greenwich Leisure Limited (GLL) and NHS Greenwich.







