In recent years, many disasters have occurred around the world. One of the events that affect human life is earthquakes. Compared with other disasters, earthquakes are uncontrollable, but its risk to affect human health is controllable by disaster risk reduction, such as building with appropriate building code, and anti-seismic structure. It affects more people by causing unwarranted damage more quickly. Reference Bavafa, Khazaie and Khaledi-Paveh1 Earthquakes are without a doubt one of the most life-threatening, catastrophic, and uncontrollable disasters. Every year, half a million earthquakes are estimated to occur around the world, but most of them go unnoticed because they strike remote areas or are too small. People suffer a variety of losses following an earthquake, depending on its size. Reference Farooqui, Quadri and Suriya2 Major disasters can have a significant impact on populations and health systems, particularly in low- and middle-income countries that are unprepared. Early intervention in major disasters, which is used for disasters that cause extensive destruction and damage, is important. Major disaster acute response activities often last only a few weeks. Disasters, on the other hand, have long-term consequences, and disaster management entails more than just quick fixes. Reference Goyet, Rayamajhi and Gyawali3 Disasters remain as events that society remembers when they happen and in the future. Even years later, people who were exposed to disasters still experience the effects of that day. The stress factor is also defended as a reaction mechanism of the person. It should not be overlooked that disasters such as earthquakes can cause acute distress but also lead to chronic stress through long-term deterioration in social and economic conditions. Reference Khatri, Tran and Baral4
The Izmir earthquake, which occurred on October 30, 2020, caused loss of life and property in Bornova Bayrakli districts. Reference Çalişkan and Kaya5 It was determined that the epicenter of the earthquake was Samos Island near Seferihisar, the earthquake magnitude was 6.9, and the earthquake lasted 15.68 s. The BayraklI district, which was heavily damaged in the earthquake, is approximately 70 kilometers away from the epicenter. As a result of this earthquake, 117 people died, 1034 people were injured, and 15,000 people were left homeless. Reference Karadaş and Öner6
Some survivors suffer from long-term distress and psychopathology, such as post-traumatic stress disorder (PTSD), depression, and other mental illnesses. The most prevalent of these negative psychological effects is PTSD. It has been shown that the consequences of being exposed to a disaster, such as the presence of physical injury, fear of death, loss of loved ones, and property damage, are stronger predictors of PTSD than the type of disaster. Reference Yang, Cui and Sim7 The factors that occur before, during, and after a disaster have an impact on psychological problems that arise because of the disaster. People are influenced by a variety of factors, including personal, social, and cultural factors. Reference Matsumoto, Sakuma and Ueda8
PTSD is a common psychiatric disorder caused by an event or series of events that are so painful or stressful that they pose a significant risk to a person’s life. Re-experiencing aspects of the traumatic event, feelings of helplessness, intense fear, frightening dreams, or avoiding the source of the trauma are all possible symptoms. PTSD may also experience physical symptoms, such as increased blood pressure and heart rate, fatigue, muscle tension, nausea, joint pain, headaches, back pain, or other types of pain. These symptoms have a significant impact on the affected people’s everyday life. Reference Marthoenis, Ilyas and Sofyan9 More severe exposure to a traumatic event is associated with more pronounced PTSD symptoms. Reference Matsumoto, Sakuma and Ueda8
Exposure to trauma in PTSD can result from first-hand experience, witnessing traumatic events, or learning of traumatic events that have occurred to close family members or peers. Anyone who feels fear, helplessness, or fear after a natural disaster such as an earthquake can be injured or even killed. Diagnosis of PTSD requires continuous recovery of the event, avoidance symptoms, adverse changes in general responsiveness, arousal, and increased responsiveness. Reference Farooqui, Quadri and Suriya2
Although many people have been exposed to traumatic events throughout their lives, some may meet the criteria for PTSD. But the majority develop sub-PTSD symptoms. Subthreshold symptoms are also considered clinically significant and may require treatment. Individuals with sub-PTSD exhibit higher rates of functional impairment of acute stress symptoms than healthy groups, although not as severely as those who meet the criteria for full PTSD. Insomnia, irritability, anxiety, startle reactions, and social withdrawal symptoms are common. Reference Mota, Tsai and Sareen10,Reference Highfill-McRoy, Levine and Larson11 It has been determined that sub-PTSD poses a risk for developing major depression, agoraphobia, substance use disorder and PTSD. It can be detected more frequently in military personnel, disaster relief workers, and health personnel. Therefore, considering the possibility of sub-syndromal PTSD in the days and weeks following trauma, clinicians may provide an opportunity for early treatment and a better prognosis. Reference McLaughlin, Koenen and Friedman12,Reference Wallace, Moss and Hodges13
In line with this information, it is essential to determine the coping levels of emergency service workers working in intense conditions due to exposure to possible trauma. Obtaining this information will play a critical role in preventing mental disorders that may occur due to the double position of emergency service personnel, both living the disaster and responding to the disaster. This study aimed to determine the psychological trauma and coping levels of the emergency service workers who were exposed to the 2020 İzmir earthquake and lived.
Methods
Study Design and Sample
This descriptive study was conducted on the nurses and physicians working in the emergency service who provided medical intervention to earthquake affected people in the 2020 Izmir earthquake (EQ-2020-000215-TUR).
The research population consisted of 55 men and 70 women between the ages of 18 and 65, consisting of physicians and nurses working in the emergency department of Ege University Faculty of Medicine. In a previous similar study, the sample size was calculated with the G*Power 3 program, taking into account the mean and standard deviation values of trauma variables in health-care workers. Reference Demirtürk Selçuk and Demirağ14 The number of individuals to be sampled was 125, with a 95% confidence interval and a 5% margin of error. Initially, 128 people were included in the study and were interviewed. Then, 15 doctors and nurses were excluded from the study because they filled in the scales incompletely. The study was completed with a total of 113 doctors and nurses. After the purpose of the research was explained to the participants, they were informed that participation in the study was completely voluntary and that they could withdraw from participating if desired. It was reported that the data of those who withdraw from the study would not be used in the research.
Inclusion criteria for the study were volunteering to participate in the research and working as a physician or nurse in the emergency department, and being on duty at the hospital during the Izmir earthquake. Exclusion criteria from the study included working outside the emergency department, being on leave on the day of the earthquake, and having a chronic mental illness (serious mental disorder, eg, schizophrenia, bipolar affective disorder).
Data Collection
A Google form was used to create the study questions. Participants were notified of the event through WhatsApp. The data were taken between September 15 and October 15, 2021. The survey is set up so that each participant can only fill out 1 form with their Google account. Participants who agreed to participate in the study were able to continue by clicking the “I agree to participate in the study” button before filling out the questionnaires. Consent was sought in this manner in the digital world. Participants who agreed to participate in the survey completed the data collecting tools online. The questionnaire was completed while taking the necessary precautions to ensure that no more than 1 response was allowed.
Data Collection Tools
Survey data is an online survey using the Sociodemographic data form, Strategies for Coping with Earthquake Stress Scale (SCESS), Post-earthquake Trauma Level Determination Scale (PETLDS), State-Trait Anxiety Inventory (STAI), and Post-Traumatic Cognition Inventory (PTCI).
Socio-Demographic Information Form: The form developed by the researchers included diagnostic questions such as age, gender, marital status, educational status, occupation, history of psychiatric illness, history of mental illness in the family, and years of professional experience. Reference Yiğitoğlu, Keskin and Köktaş15
Strategies for Coping with Earthquake Stress Scale (SCESS): The scale measures people’s coping strategies with earthquake stress. The scale was developed by Yöndem and Altay. Reference Yöndem and Eren16 There are 16 questions in the content of the scale. The scale consists of 3 sub-dimensions: Religious Coping (RC) (items 1, 2, 3, 4, and 5), Positive Reappraisal (PR) (items 6, 7, 8, 9, 10, and 11), and Seeking Social Support (SSS) (12, 13, 14, 15, and 16) items). It is a 4-point Likert-type scale. (1 = Never; 4 = Always). There is no total score. The score range for the religious coping subscale is 5-20 points, 6-20 points from the positive reappraisal subscale, and 5-20 points from the social support seeking subscale. A high score indicates that the individual uses that coping strategy more, while a low score indicates that the individual uses it less. For the reliability study of the scale, the Cronbach alpha internal consistency reliability coefficient was calculated as 0.85.
Post-Earthquake Trauma Level Determination Scale (PETLDS): PETLDS is a tool developed by Tanhan and Kayri to measure the stress levels experienced by individuals after an earthquake. Reference Tanhan and Kayri17 It consists of 20 questions in total. sub-PTSD symptoms were scaled with a 5-point Likert scale. Expressions in the Likert style are in the form of; “strongly disagree,” “little agree,” “moderately agree,” “strongly agree,” and “completely agree.” The lowest score that can be obtained from the scale is 20, and the highest score is 100. In this context, low, medium, and high levels of posttraumatic stress were examined with posttraumatic CHAID analysis. CHAID analysis builds a predictive model, or tree, to help determine how variables best merge to explain the outcome in the given dependent variable. A score of 45 and below indicates no stress, 46-62 indicates intermediate stress, and a score of 63 and above indicates high stress. The increase in the scores obtained from the scale shows that the individuals’ level of being affected by the earthquake also increases. The internal consistency coefficient (Cronbach’s alpha) of the PETLDS was found to be .87.
State-Trait Anxiety Inventory (STAI): STAI: Spielberger et al. (1970) developed this inventory, which consists of 2 subscales, a trait and a state, each with 20 questions. Reference Spielberger, Gorsuch and Lushene18 It is appropriate for those over the age of 14. The State Anxiety Scale (SAS) determines how a person feels at a given time and under specific circumstances. The Trait Anxiety Scale (TAS) assesses how a person feels regardless of the scenario or circumstances. Öner and Le Compte conducted a study on the STAI Turkish adaptation, validity, and reliability. Reference Öner and Le Compte19 The highest score of 3 is given when the presence of these feelings is reported as many, and the lowest score of 1 is given if it is reported that they are absent. A score of 36 or below for the STAI subscales indicates no anxiety, 37-42 indicates mild anxiety, and a score of 43 and above indicates high anxiety. The overall score is used in the inventory evaluation. A higher score suggests that the person more anxious.
Post-traumatic Cognition Inventory (PTCI): This is a Likert self-assessment scale consisting of 36 items from 1 to 7. Scores from the scale range from 36 to 252. Foa et al. administered the scale to a sample including clinically diagnosed PTSD patients. The total score of the scale is 133 as the cut-off point for PTSD. Reference Foa, Ehlers and Clark20 A high-scale total score indicates the density of false cognition associated with the traumatic experience. Reference Foa, Ehlers and Clark20 Translated into Turkish by Güleç et al., validity and reliability studies were carried out. Reference Güleç, Kalafat and Boysan21 The scale has 3 subscales: Negative Perception of Oneself (NPO), Negative Perception of the World (NPW), and Self-Blame Subscale (SB). The internal consistency coefficient of the scale is 0.95.
Data Analysis
For statistical analysis, SPSS (IBM SPSS Statistics version 22.0; SPSS Inc., Chicago, IL) was used. The continuous variables were given an arithmetic mean and standard deviation, while the categorical variables were given numbers and percentages. The normal distribution of data was determined using the Kolmogorov-Smirnov test. The link between the independent and dependent variables was determined using T- and F-tests. Reliability analysis was used to establish the scales’ reliability coefficients (Cronbach’s alpha). A 95 percent confidence interval was used to assess the results. For all analyses, statistical significance was considered as a P-value of 0.05.
Ethical Considerations
All procedures performed in studies involving human participants followed the ethical standards of institutions and/or national research committees and the 1964 Declaration of Helsinki and subsequent amendments or equivalent ethical standards. Before starting the study, it was approved by the Health Science University and the Institutional Review Board for Non-Intervention Clinical Studies of the Ministry of Health of Turkey (Number 21-7.1T/22.). The people involved in the study were informed of the purpose, methodology, expected benefits, and predictable risks of the study and obtained written consent. Informed consent was obtained from all individual participants in the study.
Results
Socio-demographic Findings
In the research, 113 people were reached and data collection was made. Of the people whose data were collected in the study, 66 (58.4%) were female and 47 (41.6%) were male. The age range of most of the participants is in the 26-30 age group. Additionally, 75 nurses (66.4%) and 38 physicians (33.6%) working in the emergency department participated in the study, and 78 (69%) of the participants have been working for less than 5 y. The rate of participants having a history of mental illness is between 3.5% and 4 people. There were 8 people (7.1%) with a family history of psychiatric illness. In the study, when the mental health status of the participants before the earthquake was evaluated, it was determined that 4 people were treated for psychiatric illness (serious mental disorder-schizophrenia, bipolar affective disorder were excluded) before the earthquake. It was determined that 2 of them were treated for somatic symptom disorder and the others for bulimia nervosa, insomnia disorder (Table 1).
Table 1. Socio-demographical characteristics of participants (N: 113)

Evaluation of the MEAN SCORE of the Scales
PETLDS mean scores show that the participants have intermediate stress. Participants scored the highest number of points in PR from the subscales of the SCESS and used PR coping the most; they used SSS and RC coping strategies less frequently, respectively. The average scores of the participants on STAI’s TAS and SAS scales were high. Participants scored above the cutoff score on the PTCI. This showed that post-traumatic negative cognitions were high (Table 2).
Table 2. Average scores from the scales and their evaluation by gender
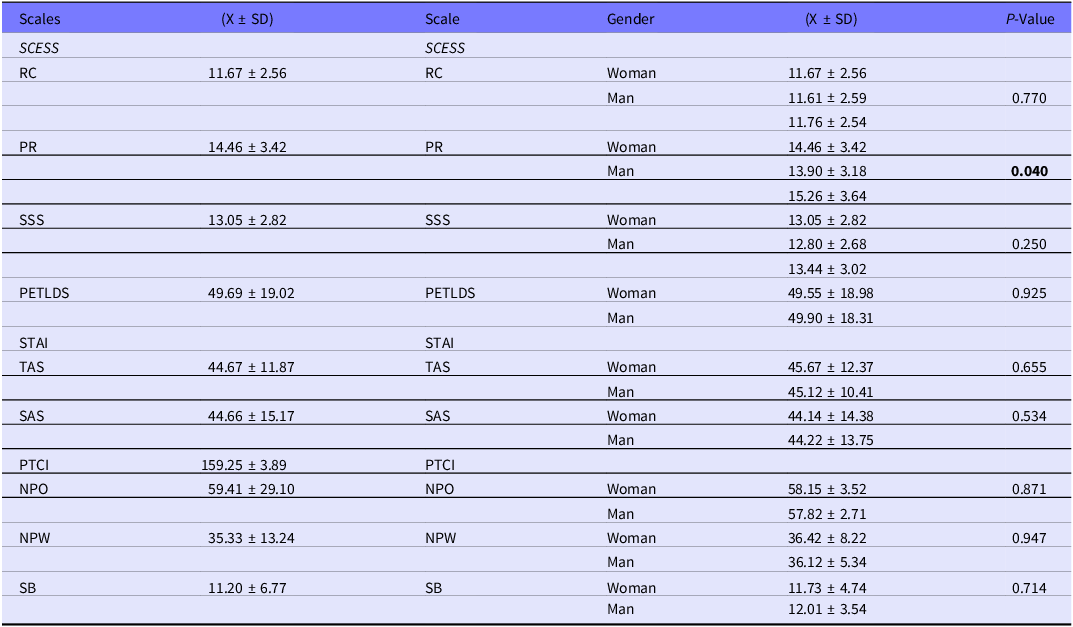
Abbreviations: Mean (X), standard deviation (SD), religious coping (RC), positive reappraisal (PR), seeking social support (SSS), Trait Anxiety(TAS), State Anxiety (SAS), negative perception about oneself (NPO), negative perception about the world (NPW), self-blame (SB), analysis of the Post-Traumatic Cognitions Inventory (PTCI), Post-Earthquake Trauma Level Determination Scale (PETLDS).
The Cronbach alpha value for SCESS, PETLDS, STAI, PTCI scales were found to be 0.80, 0.95, 0.53, 0.96, respectively.
Evaluation of PETLDS, SCESS, STAI, PTCI Scales and Sub-scales Scores According to Sociodemographic Characteristics
A significant difference was found between the groups in the positive reappraisal subscale of the SCESS according to the gender of the participants (P < 0.05). It was determined that men got higher scores on the scale. There is no significant difference between the RC and SSS subscales of SCESS, PETLDS, STAI and subscale, PTCI and subscale scores according to the gender of the participants (P > 0.05) (Table 2).
When the scores obtained from the scales according to age were evaluated, a significant difference was found between the groups in the SCESS positive reappraisal subscale. It was determined that this difference was due to the 26-30 age group getting the highest score with the Bonferroni further analysis (P < 0.05) There is no significant difference between the RC and SSS subscales of SCESS, PETLDS, STAI and subscale, PTCI and subscale scores according to the age group of the participants (P > 0.05) (Table 3).
Table 3. Evaluation of SCESS, PETLDS, STAI, and PTCI according to age

Abbreviations: Mean (X), standard deviation (SD), religious coping (RC), positive reappraisal (PR), seeking social support (SSS), Trait Anxiety(TAS), State Anxiety (SAS), negative perception about oneself (NPO), negative perception about the world (NPW), self-blame (SB), analysis of the Post-Traumatic Cognitions Inventory (PTCI), Post-Earthquake Trauma Level Determination Scale (PETLDS).
When the scale analysis was examined according to educational status, a statistically significant difference was found in the undergraduate and graduate groups between academic level and the positive reappraisal sub-dimension of the SCESS (P = 0.042; P < 0.05). With the Bonferroni advanced analysis performed to determine which group caused the difference, it was determined that the difference was because the university group scores were higher than those of the graduate group (P = 0.042; P < 0.05). There is no significant difference between the RC and SSS subscales of SCESS, PETLDS, STAI and subscale, PTCI and subscale scores according to the educational status of the participants (P > 0.05) (Table 4).
Table 4. Evaluation of SCESS, PETLDS, STAI, and PTCI according to educational status

Abbreviations: Mean (X), standard deviation (SD), religious coping (RC), positive reappraisal (PR), seeking social support (SSS), Trait Anxiety(TAS), State Anxiety (SAS), negative perception about oneself (NPO), negative perception about the world (NPW), self-blame (SB), analysis of the Post-Traumatic Cognitions Inventory (PTCI), Post-Earthquake Trauma Level Determination Scale (PETLDS).
SCESS, PETLDS, STAI, PTCI scores did not differ according to marital status, profession, years of professional experience, diagnosed psychiatric illness family history of mental illness of the participants (P > 0.05).
Evaluation of the Correlation Among the PETLDS and SCESS, PTCI, STAI Scales
There is a positive and high degree of correlation between the religious coping sub-dimension of the SCESS and the PETLDS (P < 0.001). As the level of impact from the earthquake increased, the use of religious coping increased. There was a moderate positive correlation between the religious coping sub-dimension of the SCESS and the state anxiety (P < 0.001) and trait anxiety (P < 0.001) subscales of the STAI. As the level of impact from the earthquake increased, the level of anxiety also increased. In other words, those most affected by the earthquake have higher anxiety and use more religious coping mechanism.
A moderate correlation was found between the religious coping sub-dimension of SCESS and the negative perception about oneself sub-scale of PTCI (P < 0.001). There is a high degree of positive correlation found between the social support-seeking sub-dimension of SCESS and the negative perception about oneself subscale (P < 0.001), negative perception about the world subscale (P < 0.001), and self-blame (P < 0.001) subscale of PTCI (P < 0.001).
A high degree of positive correlation was also found between the social support seeking subscale of SCESS and the state anxiety (P < 0.001) and trait anxiety (P < 0.001) subscales of STAI.
There is a positive corelation between PETLDS and the negative perception about oneself subscale (P < 0.001), negative perception about the world subscale (P < 0.001), and self-blame of the PTCI. There is a significant positive correlation between the PETLDS and trait anxiety (P < 0.001) sub-scales of the STAI. The state anxiety (P < 0.001) and trait anxiety (P < 0.001) sub-scales of the STAI and negative perception about oneself, negative perception about the world, self-blame subscales of PTCI, and also showed a high degree of positive correlation.
Effect of Variables on PETLDS and SCESS Scores
To determine the variables that predict the coping strategies of the participants in our study, variables such as STAI, PETLDS PTCI, age group, education, and gender were analyzed. PTCI, gender, and education significantly predict SCESS, together explaining 48% of the total variance (R = .68; R2 = .48; F = 52.15; P < 0.05). According to the standardized regression coefficient (ß), PTCI (ß = .60) took precedence over gender (ß = .23) and education (ß = .17) in the relative importance of the predictor variables on SCESS. Looking at the significance tests of the regression coefficient, it is seen that the predictive variables PTCI (P < 0.05), gender (P < 0.05), and education (P < 0.05) are significant predictors on SCEES. Additionally, Cohen’s f2 value was calculated to determine the effect size and f2 = .83 for the anxiety variable. In terms of Cohen (1988) criteria, it can be said that the effect size in the current study is high.
When evaluating the variables that predict the status of being affected by the earthquake; PTCI, STAI, religious coping sub-dimension of the SCESS significantly predict PETLDS, together explaining 52% of the total variance (R = .57; R2 = .52; F = 34.18; P < 0.05).
Discussion
In this study, mental trauma and coping with trauma situations in emergency service workers, who gave medical intervention to earthquake victims in the 2020 İzmir earthquake, were evaluated. In the study, the participant was determined to be intermediate traumatic and anxiety levels of the participants were above the average. Reference Tanhan and Kayri17,Reference Öner and Le Compte19 Studies have shown that emergency room personnel are at high risk for mental health problems, including anxiety, depression, and psychological distress. Reference Taylor, Cocks and Ashe22,Reference Lu, Mueser and Yanos23 In particular, it has been determined that post-traumatic stress disorder is approximately 2 to 3 times more common among various groups of emergency service personnel (eg, ambulance specialists, rescue workers) than in the general population. Reference Taylor, Cocks and Ashe22 We defined as traumatic according to the results of the scale, as a clinical this may not be sufficient to meet the symptoms of PTSD, more often it may be considered sub-PTSD. This study has implications for the nosology and symptoms of PTSD. We believe that the part of health-care workers in our study can be evaluated as subsyndromal PTSD. Reference Lu, Mueser and Yanos23 Identification of subsyndromal PTSD provides the opportunity for early treatment and better prognosis. As McFarlane and colleagues argue, subsyndromal PTSD should not be viewed merely as a normal response to an abnormal event. Reference McFarlane, Lawrence-Wood and Van Hooff24 Post-traumatic stress symptoms, even at the subsyndromal level, have been found to be associated with increased anxiety symptoms with significant social and occupational impairment, as is full PTSD. Administrative steps may be necessary to ensure that health-care personnel identified as having subsyndromal PTSD receive trauma-focused treatment and long-term follow-up. Reference Lawrence-Wood, Baur and Lawrence25,Reference McLaughlin, Demyttenaere, Koenen, Bromet, Karam and Koenen26
When exposed to more stress, they should be considered as “symptoms that are a harbinger of later mental disorders.” We found that the younger participants and those with the highest education level (doctoral) were more affected by the earthquake, which may make them more at risk in terms of trauma. We found that men, the youngest group (20-25 y old), those with a master’s degree, use “positive reappraisal” as a coping mechanism. The subsyndromal group is not defined as completely non-pathological, because clinically significant impairments are significant. According to Mylle and Maes (2004), taxonomy is important because the diagnosis also defines the medico-legal positions of the subjects and the position of individuals with subthreshold PTSD is uncertain. Reference Mylle and Maes27 However, in the literature, PTSD symptoms are higher in the subsyndromal group compared with the healthy ones. Although not a clear diagnostic category, subthreshold PTSD may not be part of a normative response to trauma but should be considered because it can cause significant impairment and be chronic. It was researched to determine the stress level left on the health workers who experienced and responded to the 30 October Izmir earthquake. Because Turkey is in an earthquake zone, it faces damages resulting from disasters. It is necessary to take preventive measures to minimize the losses and damages that may occur after the earthquake and to prevent mental health problems that may arise after the quake. Reference Akalın, Şakiroğlu and Eren28
A relationship was found between postearthquake trauma and negative perceptions of the individual and the world, self-blame. According to the theoretical premise of cognitive models of psychopathology, dysfunctional cognitive processing in the form of distorted evaluations is very important in the emergence of psychological disorders. Negative post-traumatic cognitions are important in the development, persistence, and treatment of PTSD. It has been determined that these cognitions contribute to the individual’s sense of “present threat,” thereby increasing vulnerability to develop PTSD. Reference Hyland, Murphy and Shevlin29–Reference van Heemstra, Scholte and Ehring31 Levels of postearthquake trauma were found to be linked to state and trait anxiety, as well as religious coping. Religious coping was found to be more prevalent, especially when the individual’s negative self-perceptions increased. When people are confronted with trauma, crisis, or stressful events, they often use a variety of coping strategies. Coping can be defined as the thoughts and behaviors that individuals use to manage the internal and external demands of situations that are considered stressful. Spirituality may be quite beneficial in the aftermath of a terrible event. When faced with distress or trauma, most people turn to religion or spirituality as a coping mechanism, and they often find it to be effective. Reference Mesidor and Sly32,Reference Park, Sacco and Mills33 It appears to be the primary mechanism through which spirituality and religion influence psychological outcomes. Reference Mesidor and Sly32 When it comes to dealing with stress and major life events, religion’s ability to provide meaning in life is especially apparent. Religious coping can be defined as “the degree to which religion is a part of the process of understanding and coping with critical life events”. Reference Pargament, Ano, Wachholtz, Paloutzian and Park34
Social assistance has been shown in studies to help people recover after a disaster. One of the most commonly reported coping mechanisms among survivors is seeking help. Individuals’ perceptions about their family, friends, and society are referred to as perceived social. Understanding and satisfying the needs of disaster-affected people requires a familial context. Social support is a resource that changes the negative perception of self and affects psychological and physical well-being, psychosocial adaptation, and personal gains. Reference Mesidor and Sly32,Reference Samuel and Burger35 It has been observed that increased social support improves mental well-being, particularly in cases of increased anxiety. It was observed that there was an increase in state and trait anxiety levels, negative cognitions about oneself, negative cognitions about the world, and self-blame increased the behavior of seeking social support after the earthquake in the study participants.
Evaluating the scores obtained from the age scale showed that there was a significant difference between the groups in the positive reassessment subscales of SCESS, with the 26- to 30-y-old group receiving the highest score. According to Ericsson’s Psychosocial Theory, people of different ages encounter different life events, go through a series of life stages of psychosocial development, and the major social emotions at each life stage. It solves the conflict well. Reference Erikson36 Folkman and Lazarus (1980) have a contextual theory of aging. Reference Folkman and Lazarus37 They argue that different types of stressors appear with age, and that these differences in stressors affect coping strategies and health outcomes. Adults’ stress exposure differs depending on their life context, according to the contextual theory of Folkman and Lazarus (1980). Reference Folkman and Lazarus37 As a result, it exhibits a variety of stress levels. According to 1 study, as people get older, they are less affected by stress and anger. Reference Stone, Schwartz and Broderick38 According to Socioemotional Selectivity Theory, which explains the change in emotional functioning with advancing age, it has been found that, as perceptions of time alive decrease (a natural consequence of aging), people prioritize achieving emotion-focused goals over knowledge-based goals. Reference Sliwinski, Freed and Scott39 In another study investigating the level of stress during the COVID-19 (coronavirus disease 2019) period, it is found that the stress level decreases with increasing age; the adolescent population perceives the highest amount of stress, while middle-aged adults perceive the least amount of stress. Reference Singh, Mani Pandey and Datta40 According to another study, post-traumatic growth and post-traumatic stress have a low-level significant positive relationship. This demonstrates that those who have growth because of a traumatic event also have stress symptoms. Reference Kardaş and Tanhan41
According to the gender of the participants, it was determined that men got higher scores in the positive PR subscale of SCESS. In addition to the effects of the COVID-19 pandemic on physical health, it can also have several adverse effects on people’s mental health. However, these adverse effects may differ according to gender. In a previous study, coping with negative situations in life was evaluated in young adults, and it was found that young male adults exhibit faster-coping strategies. Reference Salas-Rodríguez, Gómez-Jacinto and Hombrados-Mendieta42 It has been determined that men can make decisions faster than women and have more tendency to take risks. It has been determined that women have difficulty coping with negative situations, experience more anxiety, and show depressive symptoms. Reference Yang, Luo and Zhou43 At the same time, studies in the literature have found a significant relationship between young age and the female gender with the probability of developing these problems. Reference Serrano-Ripoll, Meneses-Echavez and Ricci-Cabello44 The sample formed with the majority of the middle age group may have affected the result. Again, in this context, the fact that the male group was significant even though the female group in the sample group was high revealed results incompatible with the literature.
It was determined that postgraduate graduates received high scores in the positive re-evaluation sub-dimension of the SCESS according to their education level. In the literature, Baysak et al. (2019) also found that positive re-evaluation increased as the level of education increased; In this context, the result supports the literature. Reference Baysak, Eroğlu and Utku45 After disasters with devastating effects such as earthquakes, people’s trauma response levels and coping levels may differ. Reference Erdener46 According to Erdener (2019), it was concluded that those who graduated from university and graduate school experienced more secondary trauma. Reference Erdener46
At the end of the study, there was no significant difference between the occupational groups of physicians and nurses in terms of coping with stress. Many factors cause occupational stress. Occupational stress has become a growing problem in health-care workers in recent years. Reference Trifunovic, Jatic and Kulenovic47 The reason why there was no difference between occupational groups in the study may be because the sample mainly consisted of nurses and that both occupational groups had the same intense working conditions. In addition, both occupational groups act with high professional responsibility when intervening with the patient. There may be similar increases in work intensities, especially during disasters, which may give similar reactions to being affected by the disaster. Different results were also found in the studies. According to a study on mental health, nurses with occupational group-specific differences were found to have the highest mental health disorders and burnout. Reference Diekmann, Böckelmann and Karlsen48 According to another study, it was found that, while the state anxiety scores of doctors and nurses are very close to each other, the trait anxiety scores of nurses are higher than doctors. Still, this difference was not statistically significant. Reference Sakaoğlu, Orbatu and Emiroglu49 A disaster is a natural event that has irreversible consequences. The psychological dimension of health workers affected by all the damage and who are involved in the response is among the issues that need to be addressed in detail. Implementation of recovery programs for health workers after disasters have been seen among the methods that can be effective. According to a published study, it was emphasized that health systems should support the health and well-being of doctors and nurses with evidence-based interventions to improve community health and increase the quality and safety of care must be provided. Reference Melnyk, Kelly and Stephens50
In the study, no significant difference was found in the SCESS in terms of past mental health problems and having a family member with a psychiatric illness. In fact, those with a history of mental illness are often expected to have high postdisaster stress levels. Understanding the traumatic response within a psychopathological framework is vital. It is rarely possible for PTSD to occur in isolation following a traumatic event. The perception of isolation or lack of social connection with others is associated with loneliness. May evoke psychological responses that often occur in situations such as depression, anxiety, or substance use. Reference Hyland, Murphy and Shevlin29 In the literature, it was determined that people with a previous history of mental illness showed depressive symptoms after the earthquake. It is seen that those who have a history of mental illness in the past have high levels of help expectations and postearthquake stress. Reference Kılıç51,Reference Uğur, Kartal and Mete52 In another study, it was reported that there might be differences in the level of the psychological impact of individuals in coping with trauma after an earthquake. It has been determined that, after disasters such as earthquakes that occur suddenly and whose consequences are unpredictable, there may be psychological problems that improve in a few weeks. Reference Kılıç51 According to Baysak et al. (2019), it was seen that mental health problems experienced in the past were effective in coping with postearthquake stress. Reference Baysak, Eroğlu and Utku45 The low rate of participants with a history of mental illness and a family history of mental illness in the study may have affected the result.
Limitations
This study has several limitations. When analyzing the study’s findings, it is important to keep in mind the study’s limitations. The most significant limitation is that data were collected by means of self-report questionnaires with rating scales. This methodology is based on the participants’ personal statements, and it is possible that their responses are not always accurate or precise. Second, because the data were gathered through online surveys, not all workers could be reached. Participants who had no prior experience with the Internet and were unable to access the survey may have responded less or not at all. Another limitation is related to the sample size of the study. Data were collected from health-care personnel working in the emergency department of a hospital. Future studies may be considered to be repeated in more hospitals, with different clinical staff and with a larger sample size. The final limitation is that the study design was cross-sectional, outcomes and predictors include the time and participants when the study data were collected.
Conclusions
In our study, psychological trauma and posttraumatic coping levels of health-care workers exposed to earthquakes differed according to age, gender, and educational status. Our study Participants scored above the cutoff score on the PTCI. This result suggests that the participants may have sub-syndromal PTSD. Sub-syndromal PTSD occurs when persons experience many of the symptoms of PTSD, with some impairment, but do not meet full diagnostic criteria. Reference Wallace, Moss and Hodges13,Reference Foa, Ehlers and Clark20 It is important to conduct a 1-to-1 psychological evaluation for a definitive clinical diagnosis. Anxiety levels have been found to be high. Postearthquake trauma levels were found to be directly related to state and trait anxiety levels and religious coping levels. Again, a relationship was found between religious coping and the individual’s negative cognitions. In our study, we found that the participants showed moderate levels of stress symptoms in terms of being affected by the earthquake, and high levels of negative postearthquake cognitions and anxiety. Participants’ negative posttraumatic cognitions, gender, and education levels were found to be predictive variables on coping strategies; religious coping strategies, posttraumatic cognitions, anxiety levels were found to be predictive variables on being affected by the earthquake. Considering the increasing frequency of natural disasters around the world, it is important to evaluate the psychological impact of disasters on emergency medical personnel working at the forefront of disasters. Future research should focus on interventions to improve emergency health-care workers’ knowledge and competencies in dealing with disaster exposure and disaster situations.
Implications for Health-care Workers’ Practice
It emphasizes how much the psychological problems that may arise after a natural disaster affect the health-care workers who work in intense and critical conditions. Undoubtedly, both are responding and experiencing the event after a natural disaster that occurs unexpectedly can cause severe psychological destruction for people. Health-care workers are also among the groups that are most affected by this situation psychologically. It is inevitable for health-care workers to receive both environmental and professional support after this severe trauma. Participating in the in-house training, playing an active role in the practices, and being informed about what can be done due to the event, will play a role in alleviating this situation. It is important to know what to do after the trauma, prepare psychologically for the conditions and conditions of the case, and manage the course of the process well. Our results show that years of experience effectively cope with posttraumatic stress. Accordingly, more training may be required in orientation training groups.
Studies show that health-care workers’ anxiety levels are high due to intense working conditions. The addition of psychological stress that may occur after trauma to health-care workers who are already working under extreme conditions can cause severe losses in their lives and is an issue that needs to be rehabilitated.
Policies and plans need to be made to manage the mental problems of health-care personnel after a disaster. It is important that government officials organize systematic, coordinated disaster mental health support services within the scope of postdisaster rehabilitation services to improve the resilience skills of health response workers. Coordination and comprehensive programs to address post-trauma are key to the success of an effective and sustainable mental health program after disaster.
Competing interests
We have no conflict of interest to declare.






