There are many studies examining the outcomes of helpline use, for example telephone consultation for self-harm, Reference Evans, Morgan, Hayward and Gunnell1 calls to National Health Service Direct, Reference Gaffney, Crane, Johnson and Playforth2,Reference Cooper, Smith, O'Brien, Hollyoak and Baker3 anti-smoking Reference Owen4,Reference Platt, Tannahill, Watson and Fraser5 and rheumatology Reference McCabe, McDowell, Cushnaghan, Butts, Hewlett and Stafford6 helplines. However, relatively few have evaluated medication helpline services Reference Raynor, Sharp, Rattenbury and Towler7,Reference Joseph, Dean-Franklin and James8 and none has examined outcomes of information received from a psychiatric medication helpline.
The Maudsley Hospital operated a national helpline for information about psychotropic medication from 1997 to 2007 when funding ceased. The helpline provided information about medication used to treat mental illness and was staffed by experienced mental health pharmacists. It was a single telephone line, open from 11.00 to 17.00 on weekdays, and closed at the weekend and on public holidays. The helpline was available to anyone who wanted information about psychotropic medication. Questions commonly asked were about the adverse and discontinuation effects, choice, dose, efficacy and interactions of antidepressant and antipsychotic medication. Pharmacists took over 25 000 calls during the helpline's 10 years of operation.
Our study is the first to examine outcomes of using a psychiatric medication helpline and the impact of its use on other healthcare professionals.
Method
Callers to the helpline all had their enquiry details and information provided recorded. A standardised medication, medical and psychiatric history were recorded for each patient and information was provided on the basis of these data only. For patients on more complex regimens further probing of medication history of both tolerance and efficacy was made. Information supplied was individualised to each patient's history. Helpline pharmacists were not allowed to advise patients to change their medication; however, callers were always encouraged to discuss their enquiries and possible solutions with their doctor.
All those who called between January and May 2007 were asked to contribute to the study – helpline pharmacists asked for their permission to participate in a later telephone survey about the quality of the service provided by the helpline. Those who gave permission were asked for details of their daytime telephone number, the best time for them to be contacted and whether or not to leave a message on their answerphone. Helpline staff (O.O. and A.C.) contacted participants 1 month after their initial call to complete the previously piloted questionnaire. The staff member contacting the caller had not been involved in taking the original call.
The following information was collected from participants:
-
• age, gender and diagnosis
-
• reason for contacting the helpline
-
• frequency of self-referral to a healthcare professional
-
• action taken as a result of information received
-
• illness status
-
• alternative sources of information if the helpline was not available
-
• satisfaction with the service and quality of information received as rated on a scale of 1 (poor) to 5 (excellent).
Participants who could not be contacted at the first attempt were tried at least on one more occasion and a message was left on their answerphone where appropriate. Those who could not be contacted after two attempts were not contacted again.
Satisfaction scores were categorised into dichotomous variables with scores >3 grouped as ‘satisfied’ and scores ≤3 classified as ‘not satisfied’. The relationships between satisfaction and certain variables (gender, caller type (patient or relative/carer) and outcome) were evaluated using unadjusted odds ratios (OR) with 95% confidence intervals (CI).
Results
During the recruitment period, 777 calls were made to the helpline and 217 callers gave permission to be contacted again. In total, 123 individuals were later contacted and included in the study. Of these, only ten callers had contacted the helpline previously and none of the calls included in the analysis was a repeat contact. Caller characteristics can be found in Table 1 and enquiry types in Table 2.
Table 1. Caller characteristics
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 29 (23.6) |
| Female | 94 (76.4) |
| Call from | |
| Self | 87 (70.7) |
| Relative | 36 (29.3) |
| Age, years | |
| ≤29 | 5 (4.1) |
| 30-39 | 26 (21.1) |
| 40-49 | 36 (29.3) |
| 50-59 | 23 (18.7) |
| 60-69 | 25 (20.3) |
| ≥70 | 7 (5.7) |
| Caller did not want to disclose | 1 (0.8) |
| Diagnosis (callers may have more than one) | |
| Depression | 41 (24.8) |
| Schizophrenia | 39 (23.6) |
| Anxiety | 38 (23) |
| Bipolar disorder | 30 (18.2) |
| Autistic spectrum disorders | 6 (3.6) |
| Attention deficit hyperactivity disorder | 2 (1.2) |
| Myalgic encephalomyelitis | 2 (1.2) |
| Personality disorders | 2 (1.2) |
| Anorexia | 1 (0.6) |
| Tourette's syndrome | 1 (0.6) |
| Dementia | 1 (0.6) |
| Intellectual disability | 1 (0.6) |
| Do not know | 1 (0.6) |
Table 2. Enquiry types
| Type of enquiry (may be more than one enquiry per caller) | Number of calls |
|---|---|
| Adverse drug reactions | 51 |
| Choice of treatment | 33 |
| Drug interactions | 17 |
| Antidepressant discontinuation | 15 |
| Dose of medicines | 12 |
| Effectiveness of treatment | 10 |
| Indication | 6 |
| Withdrawal of medicines | 6 |
| Pregnancy/lactation | 4 |
Self-referral to a healthcare professional
Seventy-three callers (59.3%) contacted a healthcare professional after receiving information from helpline staff. The healthcare professionals most likely to be contacted were a psychiatrist (33.3%), a general practitioner (GP) (17.9%) and a community psychiatric nurse (7.3%).
Changes in treatment
After contacting the helpline, most callers (n = 65; 52.8%) continued with their current treatment without any change. Of these, several commented that even though they had no treatment modifications, there was some form of change in their situation. The responses included feeling reassured (n = 7); awaiting a psychiatric appointment (n = 4); treatment monitored more carefully (n = 2); medication review planned (n = 1); considering clozapine (n = 1); caller's psychiatrist called the helpline for further information (n = 1); 49 callers made no further comments.
Overall, 22 callers (17.9%) discontinued treatment and 26 (21.1%) commenced or switched treatments. Reasons for discontinuing treatment included: stopping fluoxetine because of concurrent mania (n = 1), stopping lamotrigine because of a rash (n = 1) and stopping potentially teratogenic medicines (n = 1); 19 callers discontinued treatment for reasons unrelated to the call. Reasons for commencing or switching treatment included changing an antihypertensive drug to one less likely to interact with lithium (n = 1) and commencing a depot antipsychotic (n = 1). The remaining 24 callers had switched or commenced treatments for reasons unrelated to the call.
Ten (8.1%) callers had some form of dose adjustment made to their treatment: dose increase (n = 4), dose decrease (n = 5) and dose regimen change (n = 1).
Condition change
When asked whether the information provided had helped alter their condition, 52.8% callers felt their condition was not affected, 42.3% felt it was made better and 4.9% thought it was made worse.
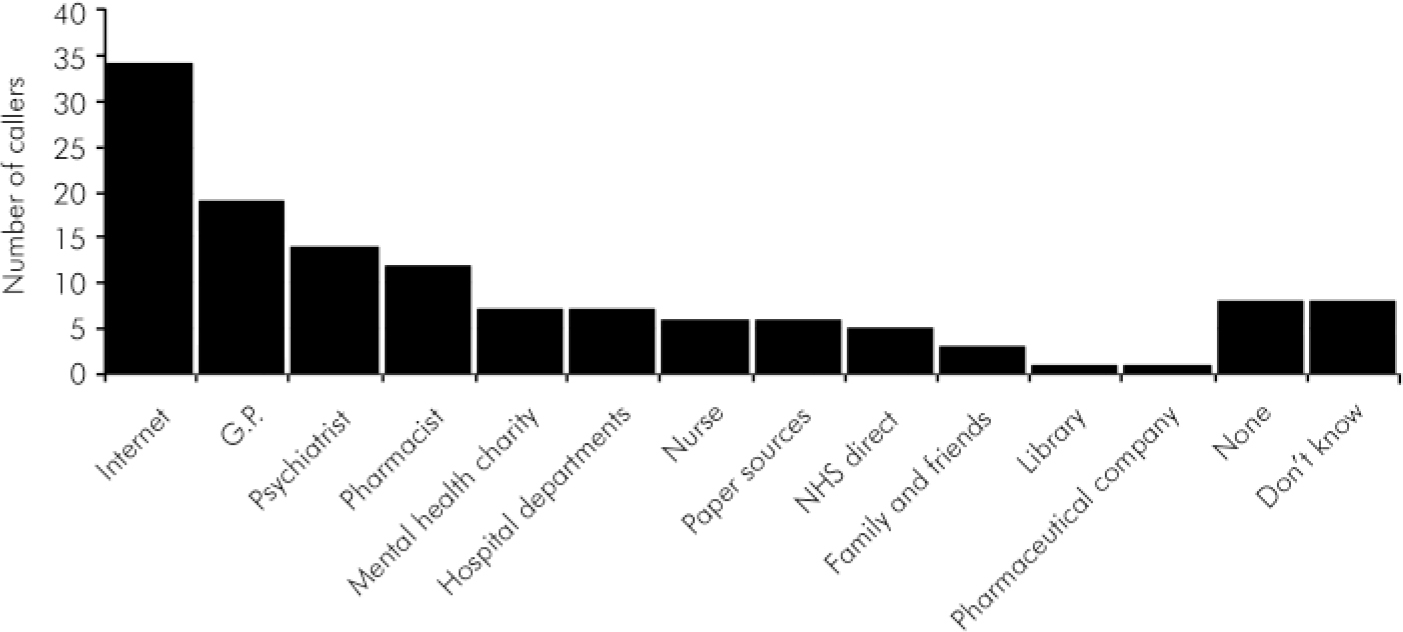
Fig. 1. Alternative sources of information for helpline callers.
Sources of information
If the helpline was not available, the sources of information most likely to have been used were the internet (n = 34), GP (n = 19), psychiatrist (n = 14) and a pharmacist (n = 12) (Fig. 1).
Caller satisfaction
The majority of callers were satisfied with the information they have received from the helpline (score 5, n = 70) (Fig. 2) as well as service provided (score 5, n = 80) (Fig. 3).
Relationship between variables and satisfaction with service
Thirty-five callers (85.4%) who had a diagnosis of depression were satisfied with the service, as well as the majority of those with a diagnosis of schizophrenia (89.7%) or anxiety (86.8%). All callers with a diagnosis of bipolar affective disorder were satisfied with the service.
There was no relationship between gender (female v. male) and caller satisfaction level (OR = 2.59, 95% CI 0.75–8.85). Likewise, type of caller (patient v. carer) and outcome (change in medication v. no change in medication) had no significant impact on degree of satisfaction (OR = 1.84, 95% CI 0.54–6.25 and OR = 0.61, 95% CI 0.18–2.03 respectively).
Discussion
Main findings
Almost half of callers in this study (47%) reported changes to their medication (stopping, starting, switching or dose adjustment) after consulting the Maudsley psychiatric medication helpline. A majority of callers (53%) reported no quantifiable changes in their medication but may have benefited from reassurance, referral, review and monitoring. Over half of callers (59%) contacted a healthcare professional, most commonly a doctor, after contacting the helpline. Almost all patients felt that, in relation to the information they had received from the helpline, their condition was the same or better. As expected, callers would mainly use the internet or contact a medical professional for advice about psychiatric medication if the helpline had been unavailable. However, more than one in ten callers was not aware of alternative sources of information.
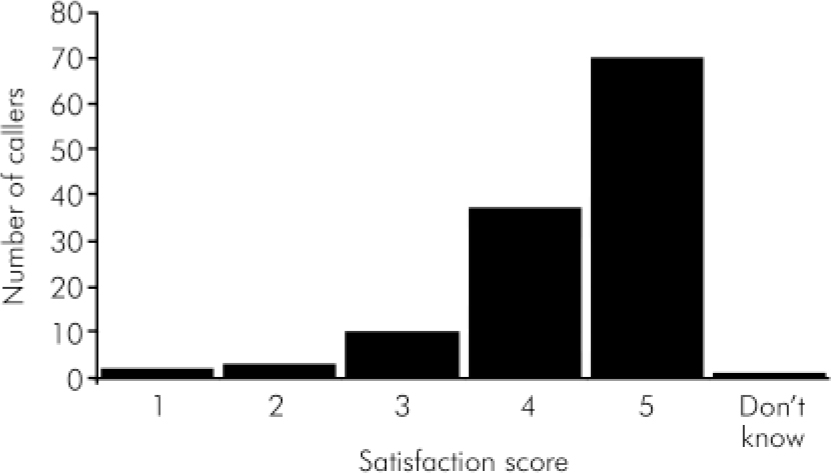
Fig. 2. Caller satisfaction with information received.
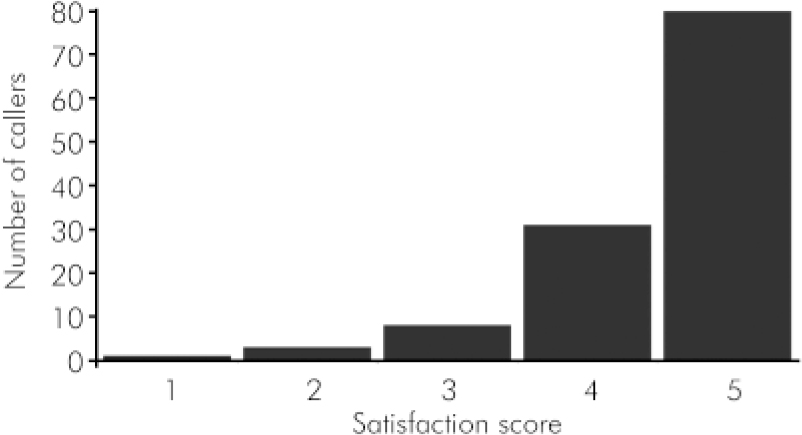
Fig. 3. Caller satisfaction with service provided.
Overall satisfaction with the quality of information and service provided by the helpline was very high. Gender, type of caller and medication change did not appear to influence satisfaction with service.
Previous studies
Our study results are similar to the few previous studies that have evaluated patient medication helplines, albeit with some differences. The only other study examining service use outcome used different assessment methods, for example ten action statements that a caller could choose from. Reference Joseph, Dean-Franklin and James8 The authors found first that callers stated that a problem with their medicines had been avoided as a result of using their helpline, and second, they reported changes (both worsening and improvement) in caller anxiety. Most other studies of medication helpline use analysed service availability and call frequency. Reference Raynor, Sharp, Rattenbury and Towler7,Reference Graeme9 Compared with other similar studies, caller satisfaction in our study was high. Reference Joseph, Dean-Franklin and James8,Reference Graeme9
Increasingly, telephone medication information services are being used with specific aims rather than more general information provision, for example to improve polypharmacy and newly prescribed medication adherence. Reference Wu, Leung, Chang, Lee, Zee and Tong10,Reference Elliott, Barber, Clifford, Hoenr and Hartley11
Limitations
A 1-month interval was chosen because this timeframe gave callers the opportunity for follow-up by a healthcare professional while being short enough for callers not to forget important details of the original call. Unfortunately, over two-thirds of callers did not give initial permission to be contacted to complete a questionnaire. Reasons for this include a desire for anonymity of some callers, number of repeat callers and reluctance of some callers to allow follow-up of our service. Of those that did give permission, a minority were lost to follow-up (largely because of an inability to be contacted). These factors considerably affected the sample size and perhaps also generalisability of the study.
There was a predominance of calls from females and patients, rather than relatives/carers, but these factors do not appear to have had a major impact on caller satisfaction. Previous studies have found that women were more likely than men to search for information on the internet and exhibit help-seeking behaviour. Reference Powell and Clarke12,Reference Oliver, Pearson, Coe and Gunnell13 Our study reflects similar trends regarding caller behaviour as related to gender.
Call outcome classified as ‘no change’ in medication could mask changes such as referral to a psychiatrist, greater monitoring of medication, medication review and the unquantifiable effect of the caller feeling reassured.
Callers frequently contacted a healthcare professional after calling the helpline. The questionnaire did not address whether this contact was already planned at the time of the call, therefore it follows that healthcare professional contact after calling the helpline may not have been related to helpline contact. Some callers reported asking for advice so that they could discuss knowledgeably their treatment with the prescriber at their next appointment. It is also probable that contacting the helpline could increase rather than reduce caller contact with other healthcare professionals.
It is entirely possible that callers may have misunderstood the question ‘In relation to the information you received from the helpline on your condition, is your condition better, worse or unchanged?’ and merely described their current condition rather than the effect of helpline information on their condition.
The study used a semi-structured questionnaire to assess outcomes of helpline use. However, open questions would have allowed helpline staff to further explore with callers the outcomes of helpline use. This could have provided a more thorough analysis of outcome given the narrative nature of each caller's history.
Implications
Uses of information provided by the helpline are numerous and often go beyond a need for mere factual information. Development of helplines with more specific aims and more measurable outcomes could be the future for these services.
Declaration of interest
None.
Acknowledgements
The study was funded by a research grant awarded by the trustees of the South London and Maudsley NHS Foundation Trust.








eLetters
No eLetters have been published for this article.