1. Introduction
The need for treatment to protect health and safety is the key provision justifying the use of outpatient civil commitment (OCC), also known as a community treatment order (CTO) under Australian law and in commonwealth countries. OCC-statutes, though varied by jurisdiction in interpretation and language, almost universally provide for protecting safety from actions associated with behavior considered an imminent danger or harm to self and others [1–4]. The U.K. Parliament's intention for the use of the CTO in the U.K. Mental Health Act of 2007 was to “…put [the assignment to a CTO] to the clinical decision about the risk in the community…. [5].” This study investigates the potential of CTO-assignment for people with severe mental illness (SMI) to fulfill two aspects of its legal mandate to provide needed treatment to “protect the safety of self and others”—i.e. protection of self from external-threats, victimization (exclusive of deliberate-self-harm), and protection of others from perpetrated-crimes.
A small proportion of individuals with SMI commit major crimes (i.e. homicides, rapes, assaults/abductions, and robberies). Yet, the risk of perpetrating such crimes in the SMI population, especially for those with untreated mental illness, has been found to be elevated by approximately three to 13 times when compared to general population-samples internationally in repeated studies [Reference Treatment Advocacy Center6]. Of equal concern for people with SMI is the population’s elevated-risk of victimization by crime. Adjudicated “helpless to avoid the hazards of freedom….mentally ill persons who meet this standard are clearly dangerous to themselves [Reference Dennis2].” Depending on the type of violent crime, victimization-prevalence-rates are reported to be 6–23 times greater among persons with SMI than among the general population [Reference Teplin, McClelland, Abram and Weiner7]. Teplin [Reference Teplin, McClelland, Abram and Weiner7], p.2] notes that: “symptoms associated with SMI, such as impaired reality testing, disorganized thought processes, impulsivity, and poor planning and problem solving, can compromise one’s ability to perceive risks and protect oneself [Reference Hiday, Swartz, Swanson, Borum and Wagner8–Reference Sells, Rowe, Fisk and Davidson13]. Moreover, factors correlated with victimization—substance abuse, conflicted social relationships, poverty, and homelessness [Reference Logan, Walker, Cole and Leukefeld14–Reference Cunradi, Caetano and Schafer17]—are common among persons with SMI [Reference Hiday, Swartz, Swanson, Borum and Wagner8, Reference Silver18, Reference RachBeisel, Scott and Dixon19].”
Previous individual-focused-research has reported associations of OCC with reduced safety-risks. These studies found OCC associated with reduced victimization (self-reports of crimes against persons and property) [Reference Hiday, Swartz, Swanson, Borum and Wagner20], arrests of all types [Reference Link, Epperson, Perron, Castille and Yang21], violent incidents, [Reference Phelan, Sinkewicz, Castille, Huz and Link22], and reduced mortality-risk [Reference Segal, Hayes and Rimes23–Reference Segal and Burgess25].
In Victoria, Australia, the CTO-statute is characteristic of most international jurisdictions (see, Appendix, Section I). The primary criteria for CTO-assignment involves an assessment indicating that the patient, due to mental illness, is in need of treatment to protect health and safety. The patient must be refusing such treatment and the treatment must be the least restrictive form of care. The patient can only be placed and/or retained on a CTO for the period her/his behavior continues to be a near-term threat to health and safety and during which treatment is available. The CTO-supervised-treatment functions as “a less restrictive alternative to psychiatric hospitalization” [26] by releasing inpatients whose behavior continues to pose health and safety risks earlier than would typically occur or by allowing continued community residence of patients posing health and safety risks without initial hospitalization. Both actions enable reduced inpatient time and potentially reduce community-risk [Reference Segal, Hayes and Rimes27].
The CTO requires an individual to participate in community-based mental health treatment believed to reduce their risk of involvement in actions that are harmful. CTO-supervision also enables a timely return to an inpatient facility for treatment when new symptoms threaten to have dangerous or harmful consequences, when patients fail to comply with CTO-treatment-agreements, and when community care is either unavailable or ineffective (a situation where no less restrictive alternative exists). When the CTO is not complied with or is deemed ineffective--i.e. the patient is refusing required treatment, deemed “needed”, and their mental health is deteriorating--they can, in all Australian jurisdictions and most international ones, be directly returned to a psychiatric hospital [1, 4]. There it is determined if they continue to manifest the potentially harmful behavior that originally brought them into involuntary care and require readmission [1, 4]. Previous population-focused-research has reported an association between reduced homicide rates and the use of the “need for treatment” criterion in civil commitment, in both inpatient and outpatient settings [Reference Segal28]. Bringing people to hospital earlier in the course of their first psychotic episode for needed-treatment was found to be associated with reduced homicide rates [Reference Large and Nielssen29]. Using OCC to bring people in earlier to hospital in recurrent episodes of illness may have a similar outcome.
All Victoria’s psychiatric hospitals were closed in 2000 and the primary state-governmental-unit responsible for community-based-care was disbanded [Reference Gerrand30]. This unit had built a rather comprehensive community-care-system during the decade prior to this investigation, a system designed to ensure service for a deinstitutionalized population in community-based specialty-mental health services [Reference Gerrand30]. With the demise of this unit, and a shift to integrated-care focused around the general hospital, Victoria experienced a 25% reduction in community-based service, noted by comparing its offerings from 1990 to 2000 with those from 2000 to 2010 [Reference Segal, Hayes and Rimes27]. This reduction may have refocused the function of the CTO to crisis-management, given that 39% of CTOs ended in re-hospitalization [Reference Segal, Hayes and Rimes27]
This study focuses on questions of safety (exclusive of deliberate self-harm) in Victoria, Australia. It considers whether CTO-supervision is associated with reducing occurrence-risk of two major indicators of imminent danger or harm to self or others—i.e. perpetration and victimization of major crimes against persons. It also considers whether community-treatment-provision and the provision of needed treatment via timely return to an inpatient-facility while under CTO-supervision is associated with reduced-risks of dangerous or harmful behavior. Given the statutory mandates in the law with respect to the use of CTOs, it is therefore hypothesized that the experience of a CTO: 1) Will be associated with a reduced-risk of perpetrating and/or being a victim of “a major-crime-against-a-person”. 2) Will be associated with a reduced-risk of repeated major-crime-experience. And, 3) that providing community-based-treatment and/or employing CTO-supervision to return a person to the hospital will be associated with a reduced-risk of initial and repeat perpetrations and victimizations.
2. Method
Patient records from Victoria, Australia, were obtained from the Victorian Psychiatric Case Register/RAPID system for all 11,424 who experienced psychiatric hospitalization and/or their first CTO between 2000 and 2010, and 16,161 (matched and randomly selected patients) who had experienced psychiatric hospitalization without CTO-assignment (see Appendix, Section II A, for sampling details). Mental health records were linked via the Victoria Police Law Enforcement Assistance Program (LEAP) [31] to all police contacts in the State extending for an additional 2.4-year-period, yielding a 12.4-year study-period. Additionally, they were linked to records of: Corrections Victoria (documenting detention in police custody or prison), the Socio-Economic Indexes for Areas (SEIFA) (documenting neighborhood disadvantage [32]), and the Australian Mental Health Outcomes and Classification Network’s (AMHOCN) Health of the Nation Outcome Scale (HoNOS) assessments of symptom-severity-profiles (documenting potential need for treatment) [Reference Burgess, Coombs and Clarke33]).
2.1 Measurement
Mental health service/treatment contacts. A service contact in Victoria entails medication, supervision, therapeutic discussion, and support in daily activities. It “…is clinically significant in nature [and] includes activity which directly contributes towards…the therapeutic needs of a client's condition.” [Reference Victoria DHHS34] (See: Appendix, Section II.B.2).
Mental health episodes of care. All mental health treatment contacts (inpatient, voluntary outpatient community care, and CTO) were organized into episodes of care [Reference Tansella, Micciolo, Biggeri, Bisoffi and Balestrieri35]. Each psychiatric hospitalization (from day of admission to discharge) was considered a separate inpatient-episode. Each continuous period of outpatient-care without a break in service for 90 days or more defined a community-care episode [Reference Tansella, Micciolo, Biggeri, Bisoffi and Balestrieri35]. Service-breaks of 90 days or more followed by re-initiation of care defined the start of a new community-care episode. Each CTO-episode began when a patient was placed on orders and ended when the order was terminated. A community-treatment-day was any day during a community-care episode (voluntary or CTO) when the patient received at least one mental health system service contact.
Measures of imminent threats to safety were limited to LEAP-reports of perpetrations of and victimizations by major crimes against persons, i.e. homicides, rapes, assaults/abductions, and robberies [Reference Police36]. Victoria’s crime incident rates were computed using LEAP data from 2000 to 2012 [31], the 12.4-year study period, and Victoria’s Australian Bureau of Statistics population data [37]. Incident rates were computed for each year and the mean of the rates over the 12.4-year period was reported herein.
Measuring Neighborhood Disadvantage. All the postal-codes in Victoria are SEIFA-ranked for socio-economic disadvantage, ranging from one (most disadvantaged) to 644 [32]. The lowest ranked postal-code where the individual lived during the study was used as the indicator of their neighborhood socio-economic disadvantage [Reference Sampson, Raudenbush and Earls38].
Validating and accounting for a need for treatment. Clinician determinations of a need for treatment at inpatient admission and discharge (when CTO-placement typically occurred) were validated with independent Health of the Nations Scale (HoNOS) severity-score profile assessments conducted in parallel to the CTO-evaluations [Reference Segal, Hayes and Rimes27]. The Health of the Nation Outcome Scale (HoNOS) is a 12-dimension-profile with established reliability and validity [Reference Burgess, Coombs and Clarke33]. Individual HoNOS dimensions are rated from zero, no problem, to four, an extremely problematic situation [Reference Eagar, Buckingham and Coombs39]. A serious problem with any HoNOS-dimension would contribute to a decision of eligibility for CTO-placement validating a need for treatment determination [Reference Phelan, Slade, Thornicroft, Dunn, Holloway and Wykes40–Reference Burgess, Trauer and Coombs44].
2.2 Analyses
Study analyses used SPSS 24.0 [Reference IBM Corp45]. Logistic regression models with propensity-score adjustment included the following variables to address study hypotheses.
Outcome variables: “having committed at least one perpetration”, “being a victim of at least one victimization”, and engaging in a “repeat perpetration” or a “repeat victimization” (CTO’s potential associations with recidivism) were each coded 1=presence, 0=absence.
Intervention-effect-measures as independent variables. All models were run twice, once with “CTO-cohort membership” (1 = CTO vs 0=non-CTO) as the intervention-effect independent variable and once with “CTO-initiated re-hospitalization” as the intervention-effect independent variable. All models initially included a measure of community-treatment-days, and subsequently the number of units of “ten community-treatment-days” the patient experienced in a community-care episode and an evaluation of observed significant interaction effects between “ten community-treatment-days” and CTO-assignment. Ten-community-treatment-days per episode was chosen because it was the average difference between the numbers of community-treatment-days provided to the two cohorts. The “number of community-treatment-days per month” and the “number of community-treatment-hours per treatment day” were considered measures of treatment intensity and were evaluated in the models.
Confounding influences as independent variables: In addition to the intervention measures, a propensity-score adjusting for selection into the CTO-cohort, and involvement in crime/victimization prior to the study, the following potential confounding influences were entered into the models stepwise in three blocks:
Block 1: SEIFA ranking [32], potential bias-indicators (Non-English Speaker, Aboriginal and/or Torres Strait Islander status), and imprisonment or held in custody during the study period.
Block 2: Demographic, diagnostic, risk-period, and service use indicators including: gender, age, unemployment status, age at entry to the mental health system, time in the study, diagnosis (schizophrenia, affective disorder, dementia, paranoia), duration of inpatient care, episode start year, and < 11th grade education,
Block 3: Need for treatment validity controls: Twenty-four HoNOS-items assessing the severity of symptom profiles, 12 measured at inpatient admission, and 12 at hospital-release [Reference Eagar, Buckingham and Coombs39].
Additional detailing of the model theory and the basis of variable selection is available online (see: Appendix, Section-II-B, C & D).
Challenges to generalizability. OCC/CTO statutes--in the U.S., U.K., Australia, Norway, as well as other jurisdictions address risks attributable to “mental illness” without diagnostic restrictions [1, 4]. Yet for purposes of comparison with other studies, final models were re-run excluding patients with dementia and other nervous system disorders.
Table 1 Diagnostic, service, and cultural background characteristics of psychiatric patients with a history of hospitalization who have or have not been placed on community treatment orders.

2.3 Ethics
Study procedures were approved by ethics committees of the Victorian Department of Health and Human Services, the University of California, Berkeley, and the Victoria Police. Authors have no conflicts of interest to report.
3. Results
The average age of the sample (N = 27,585) was 39 ± 17.3, 56% were males, 31.9% had <12th grade education, 60% were unemployed, and 49% had never been married. Their diagnoses were schizophrenia (66%), major affective disorder (10%), paranoid or psychotic disorder (8%), dementia and other nervous system disorders (11%), and other disorders (3%) (Table 1).
During the study period, the sample logged 14,774 perpetrations, including 140 homicides, 886 rapes, 12,235 assaults and abductions, and 1513 robberies. They suffered an aggregate of 6991 victimizations, including 23 homicides, 1073 rapes, 5293 assaults or abductions and 602 robberies (Table 2).
The CTO-cohort had almost twice the number of community-treatment episodes (6.0 ± 4.4 vs. 3.3 ± 2.9) than the non-CTO-group, with almost 40% more treatment-days per episode (26.6 ± 30.1 vs. 16.1 ± 26.7). Of their community-treatment-episodes, 2.3 ± 2.4 involved a CTO (46% had 2 CTO-episodes). Overall, the CTO-cohort experienced 25,696 CTO-episodes whose duration was M = 220.7 ± 256.5 days (Median = 158.1; Interquartile range 269 days). Of these, 5.9% were initiated from the community, and 39.2% ended in re-hospitalization (see Table 1).
Based upon group characteristics (Table 2), crude perpetration rates per 100,000 during the study were respectively for the CTO and Non-CTO cohorts, 7.5 and 5.6-times higher than for Victoria’s citizens. Crude victimization rates were respectively 3.7 and 3-times higher. During the study period, the CTO-cohort members logged 7182 perpetrations and 3251 victimizations compared to 7592 perpetrations and 3740 victimizations for the Non-CTO-cohort. The CTO- cohort had a significantly higher number of perpetrations and victimizations per person than the Non-CTO-cohort: respectively, 0.63 ± 2.2 versus.47 ± 2.0 perpetrations per person (F = 38.08, df 1, 27,584, p <.001) and.29 ±.8 versus.23 ±.82 victimizations per person (F = 27.39, df 1, 27,584, p <.001).
Focusing on individual involvement in at least one perpetration and/or victimization (Table 3), a greater proportion of the CTO than the non-CTO-cohort had committed at least one perpetration (17% vs 13%) and had been the victim of at least one victimization (16% vs 13%). These perpetration and victimization figures however do not take into account the between-group differences that affect risk differentially in the two cohorts.
Most notably the Non-CTO-cohort lived in better neighborhoods (SEIFA Ranking, 250 vs 219, F = 216.61, df = 1, 27,175, p <.001) and experienced less unemployment (54% vs 69%, ChiSq = 628.56, df = 1, p <.001) both factors associated with less crime-risk. Additionally, regardless of cohort, perpetrators and victims lived in more disadvantaged neighborhoods. Their neighborhoods differed from those without recorded incidents by ten SEIFA-percentile-ranks (28th vs. 38th percentile for the CTO-cohort and 33rd vs. 43rd percentile for the non-CTO-cohort; see Table 3).
Table 2 Exposure to CTOs, crime and victimization incidents over 12.4 years among psychiatric patients with a history of hospitalizationa.
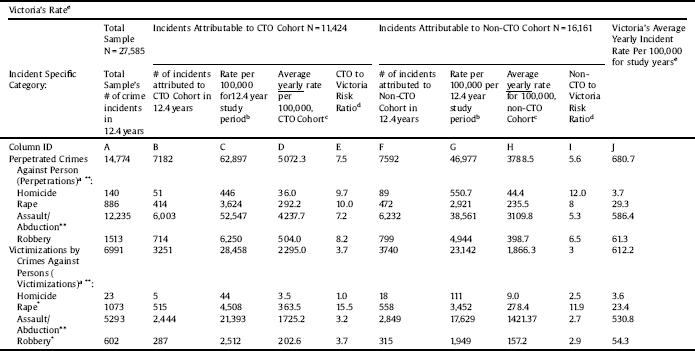
aCrimes and victimizations against persons (CAPs & VAPs) include all homicides, rapes, assaults/abductions, and robberies.
bThe rate per 100,000 = [(B/NCTO)(100,000)] or [(F/NnonCTO)(100,000)].
c verage Yearly Incident Rate Per 100,000 for the study years= C/12.4 for CTO cohort; G/12.4 for non-CTO cohort.
dRatio of CTO patients’ yearly rate per 100,000 to Victoria’s yearly rate per 100,000 = D/J; Ratio of non-CTO yearly rate per 100,000 to Victoria yearly rate per 100,000= H/J.
eVictoria’s Average Yearly Incident Rate Per 100,000 for the study years. Victoria’s crime incident rates are computed using LEAP reports from 2000 to 2012 and Victoria population data. The crime incident rate was computed for each year. The mean of the rates taken over the 12.4-year period is reported herein.
*CTO and non-CTO samples differed significantly at between p =.001 and p =.005.
** CTO and non-CTO samples differed significantly at p <.001.
Table 3 Characteristics of CTO and Non-CTO- psychiatric patients having at least a single contact with police associated with an incident of perpetrating a crime against a person (Perpetration) or being a victim of a crime against person (Victimization).

*Lowest SEIFA score for the areas in which the cohort members were in residence.
Table 4 reports the results of Logistic regression models that adjust for these differences in considering whether the CTO-experience was associated with initial perpetration and/or victimization risk after giving explanatory priority to potential confounding-risk-factors. The first set of models in Table 4, Model 1, were statistically significant (when “initial-perpetration” was the dependent variable and all control variables were included: N = 26,015, χ2 = 4737.18, df = 46, 25,969, p <.001; similarly, when “initial-victimization” was the dependent variable: N = 26,015, χ2 = 3162.98, df = 46, 25,969, p <.001); and, CTO-placement was associated with reduced initial-perpetration and victimization risks. As the additional confounding-risk-factors were taken into account in stepwise fashion in Model 1, the association of reduced initial-perpetration-risk with CTO-assignment increased from 13% (Exp(B) =.87, CI 95% =.80–.95, p =.002), to 17% (Exp(B) =.83, CI 95% =.76–.91, p <.001). For initial-victimization-risk, from 9% (Exp(B) =.91, CI 95% =.84–.99, p =.040), to 11% (Exp(B) =.89, CI 95% =.81–.97, p =.011) (See Table 4). When the final fully controlled models were rerun without patients diagnosed with “dementia and other nervous system disorders”, associations changed little: reduced initial-perpetration-risk was 15% (Exp(B) =.85, CI 95% =.77–.94, p =.002), initial-victimization-risk was 10% (Exp(B) =.90, CI 95% =.82–.99, p =.028).
A small but significant association attributable to each community-treatment-day was found for initial-perpetration-risk (Exp(B) = 0.993, CI 95% =.990–.995, p <.001), and initial-victimization-risk (Exp(B) = 0.998, CI 95% =.996–.999, p <.040) (see Table 4, Model 1, models inclusive of all control variables). Given the small association effect for each community-treatment-day, the models were re-estimated evaluating the effect of “ten-community-treatment-days”. During each community-care-episode, the significant interaction between ten-community-treatment-days and CTO-placement was associated with a 3.4% reduced-initial-perpetration-risk for each additional ten-community-treatment-days (Exp(B) =.966, CI 95% =.943–.988; p =.003), but not significantly related initial-victimization-risk.
In addition, when the two potential measures of intensity of community service were inserted into Model 1 (containing all control variables) for both initial perpetrations and victimizations, the “number of community-treatment-days per thirty-days” of a community-care-episode was associated with an increase in initial-perpetration risk (Exp(B) = 1.010, CI 95% = 1.006–1.015, p <.001) and not significantly associated with initial-victimization risk. The “number of contact hours per community-treatment-day” was not significantly associated with initial-perpetration-risk but was associated with a slight increase in initial-victimization-risk (Exp(B) = 1.004, CI 95% = 1.000–1.008, p =.042).
The second set of Logistic regression models, Model 2, in Table 4 show the results of regressing exposure to at least one “CTO-initiated re-hospitalization” on initial-perpetration and initial-victimization. All the models were statistically significant. In the fully controlled models, when initial-perpetration was the dependent variable: N = 26,015, χ2 = 4728.59, df = 46, 25,969, p <.001; when initial-victimization was the dependent variable: N = 26,015, χ2 = 3166.44, df = 46, 25,969, p <.001. In these models, exposure to at least one “CTO-initiated re-hospitalization” was associated with a 13% reduced-risk in initial-perpetration (Exp(b) =.87, CI 95% =.77–.97, p =.016) and a 17% reduced-risk in initial-victimization (Exp(b) =.83, CI 95% =.74–.93, p =.002) after taking into account all controls. When these models are re-run without patients with “dementia and other nervous system disorders”, the associations with reduced-risk-estimates changed little. For exposure to at least one “CTO-initiated re-hospitalization” the association with reduced-risk in initial-perpetration remained 13% (Exp(b) =.87, CI 95% =.77–.98, p =.023), and was 15% for initial-victimization-risk (Exp(b) =.85, CI 95% =.75–.95, p =.006) after taking into account all controls.
Table 4 Logistic regression models showing predictors of having perpetrated or being a victim of a major crime against a person over 12·4 years among 27,585 patients with a history of psychiatric hospitalizationc.
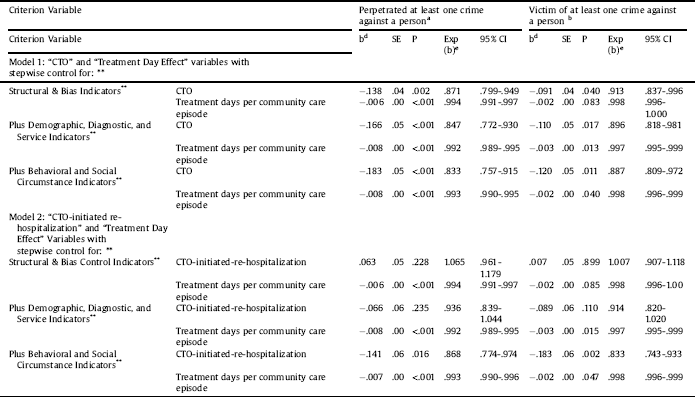
a Model 1: When crime against a person is the dependent variable and the “CTO effect” is the primary independent variable and all three groups of control variables are included in the model, χ2 = 4737.18, df = 46,25,969, p <.001; N for regression = 26,015. Model 2: When crime against a person is the dependent variable and “CTO terminated with hospitalization” is the primary independent variable and all three groups of control variables are included in the model, χ2 = 4728.59, df = 46, 25,969, p <.001; N for regression = 26,015.
b Model 1: When victimization by a crime against a person is the dependent variable and the “CTO effect” is the primary independent variable and all three groups of control variables are included in the model, χ2 = 3162.98, df = 46, 25,969, p <.001; N for regression = 26,015.
Model 2: When victimization by a crime against a person is the dependent variable and “CTO terminated with hospitalization” is the primary independent variable and all three groups of control variables are included in the model, χ2 = 3166.44, df = 46, 25,969, p <.001; N for regression = 26,015.
c Many “b”, and “SE” coefficients appear as 0.00 or 0.99 as they have not been extended to more than two decimal places in order to allow all of the data reporting in a single table. The zeros 0.00 or 0.99 refer to small and sometimes significant effects of the adjustment variables.
d “b” is a multiple-partial slope indicating how much change can be expected for a unit change in a predictor variable associated with a unit change in the criterion variable, i.e. after all other predictors have been given causal priority in explaining the change.
e Exp(b) is an odds ratio providing an indication of relative risk. When below one it indicates a reduced risk of one minus the odds ratio, when above one it is an indicator of the percent of increased risk.
**In addition to the two factors noted in the table, a propensity score for selection into the CTO cohort and involvement in crime/victimization prior to the study, the models adjust for three groups of control variables by adding the additional controls to the models in steps:
1. Structural and potential bias indicators: The lowest (most disadvantaged) SEIFA rank of a neighborhood in which the person resided during the study period, Aboriginal or Torres Strait Island heritage, required an interpreter in tribunal hearings, not born in Australia or New Zealand, whether their preferred language was not English, and the days spent in prison during the study period.
2. Demographic, Diagnostic, and Service Indicators: gender, age, unemployment status, age at entry to the mental health system, time in the study, diagnosis (schizophrenia, affective disorder, dementia, paranoia), duration of inpatient care, episode start year, < 11th grade education.
3. Indicators of behavior and circumstance: 24 HoNOS psychosocial assessments of the patient’s life situation, 12 completed at admission and 12 at discharge from inpatient care over the study period.
There were 4129 individuals with one or more perpetrations (M = 3.6 ± 4.3, Median = 2.0, Range 58), and 3995 with one or more victimizations (M = 1.75 ± 1.47, Median 1.0, Range = 18). Proportionally the groups did not differ significantly on either criterion. In fully controlled models, when repeat-perpetration is the dependent variable and CTO-supervision is the primary independent variable, model statistics are: N = 3,973, χ2 = 743.62, df = 46, 3927, p <.001 and CTO-use was associated with a 22% reduced-risk in repeat-perpetrations (Exp(B) =.78, CI 95% =.66–.93, p =.006). CTO-initiated re-hospitalization was only marginally significant in association with repeat-perpetrations (Exp(B) =.82, CI 95% =.66–1.00, p =.054). When repeat-victimization is the dependent variable, only CTO-initiated re-hospitalization was significant as a primary independent variable. Model statistics are: N = 3859, χ2 = 249.73, df = 46, 3813, p <.001. CTO-initiated return to hospital was associated with a 22% reduced-risk in repeat-victimization (Exp(B) =.78, CI 95% =.66–.95, p =.017).
4. Discussion
During the 12.4-year study-period the crude-perpetration-rates per 100,000, respectively for the CTO and Non-CTO cohorts, were 7.5 and 5.6-times higher than for Victoria’s citizens. Crude-victimization-rates were respectively 3.7 and 3-times higher (Table 2). The higher rates seem to confirm that hospitalized-psychiatric-patients posed a greater safety-threat to others and to themselves, exclusive of self-harm, than do members of the general-public.
The numbers of hospitalized patients that engaged in at least one perpetration or experienced a victimization was proportionally greater in the CTO vs the Non-CTO-cohort (Table 3). From these statistics, it would appear that CTOs are not likely to address the frequency of crime even within the hospitalized population. These statistics are, however, crude figures that do not take into account the fact that the CTO-cohort was characterized by more risk-factors associated with violent crime and victimization than the non-CTO-cohort. The CTO-cohort included younger unemployed males living in more socially disadvantaged neighborhoods. Its HoNOS severity-profiles appeared to validate a need for treatment exceeding that of the non-CTO-cohort, particularly in areas of potentially dangerous behavior [Reference Segal, Hayes and Rimes27]. The Logistic models enabled adjustment for between group differences (Table 4). They controlled for prior crimes and gave explanatory priority to alternative-risk-factors over the CTO in assessing perpetration and victimization risk. After these potentially confounding factors were taken into account, the CTO was associated with a 17% reduced-risk in initial-perpetration and an 11% reduced-risk in initial-victimization. CTO-supervision was also associated with a reduced-risk of 22% in repeat-perpetration. These results echo findings of dramatic decreases in police contacts and violent behavior associated with OCC-implementation in New York [Reference Link, Epperson, Perron, Castille and Yang21, Reference Phelan, Sinkewicz, Castille, Huz and Link22].
Studies using re-hospitalization as their primary outcome measures, including the three randomized OCC-studies [Reference Steadman, Gounis, Dennis, Hopper, Roche and Swartz46–Reference Burns, Rugkåsa, Molodynski, Dawson, Yeeles and Vazquez-Montes48], unfortunately, conflate their outcome-measure with their intervention-measure—i.e., providing supervision enabling timely-return to hospital when new symptoms threaten to have dangerous consequences. This conflated dependent variable makes it difficult to determine whether the results of these trials are positive or negative [Reference Segal49]. The findings herein support CTOs’ protective role of providing needed community-based treatment and providing needed-treatment via re-hospitalization. Community-treatment-days, in the context of Victoria’s reduced community-service-commitments [Reference Segal, Hayes and Rimes27], when compared to re-hospitalization, appeared to play a relatively smaller part in association with reduced perpetration and victimization-risk. CTO-initiated re-hospitalization was associated with a 13% reduced-risk in initial-perpetration, a 17% reduced-risk in initial-victimization, and a 22% reduced-risk in repeat-victimization. There was no significant relationship between initial-victimization-risk for every “ten-community-treatment-days” associated with CTO-placement, though there was an associated 3.4% reduced-risk in initial perpetration, amounting to a 9.0% reduced-risk in initial-perpetration for the average CTO-patient who received 26.6 community-treatment-days per community-care-episode vs. the 16.6 days in the non-CTO-group.
Victoria’s experience seems to follow an international deinstitutionalization-dynamic where mental health systems are reorganized around general-hospital-integrated-care [Reference Segal, Jacobs and Deinstitutionalization50]. The mandated objectives of OCC, protecting safety of self and others from the behavioral consequences of severe mental illness, are displaced by the goal of “prevention of hospitalization”, stigmatizing hospital-use. This empowers factions opposing hospitalization based on human rights concerns and those groups committed to cost-savings in mental health services to cut beds [Reference Slade and Goldman51]. Reduced availability of general-hospital-beds creates pressure for earlier discharge to accommodate new acute patients [Reference Torrey, Fuller, Geller and Jacobs52]. In the absence of strong Assertive Community Treatment or equivalent-case-management, hastened discharge leads to a high probability of readmission for symptoms associated with the original hospital-stay [Reference Segal, Watson and Akutsu53]. The “revolving-door” effect is exacerbated in managed-care-systems where hospitals are paid a fixed fee per admission--profiting when admissions are short and re-hospitalization is billable as a new encounter. CTOs, in the absence of adequate community-care, carry out their mandate to enable the provision of needed-treatment: crisis-returns to hospital, the default requirement in the absence of adequate-community-treatment [Reference Segal49]. Critics, conflating outcome and treatment intervention, misrepresent this intervention as CTO’s failure to “prevent hospitalization”, making no mention of inadequate community-based treatment, cutbacks in such service associated with concentrating care in the general hospital complex, the financing incentives for readmissions [Reference Patel54], and the dire behavioral risks to long-term recovery potentially avoided with CTO-supervision. It is time to add greater legitimacy to both the need for expanded community and hospital-based resources for needed-treatment as well as less restrictive alternatives to the criminal justice system, which is the next stop for many denied access to inpatient care when they need it [Reference Talbot55].
Herein we have addressed only two of the many ways OCC may contribute to providing needed treatment to protect health and safety. There are many threats to health and safety where the evaluation of the role of OCC requires different outcome measures. In order to improve and better understand OCC we need future research efforts focused on other statutorily justified objectives that are evaluated with behavioral outcomes that would indicate a success or failure of OCC in meeting these objectives.
The study’s limitations are inherent in issues that impede direct generalization of crime data to other nations [Reference Farrington, Langa and Tonry56], its use of administrative and criminal justice data, and its correlational case-control methods. Though it may be possible that a return to hospital ending a CTO-episode was independently initiated, this was unlikely without the influence of the mental health team. While the correlational methods do not confirm causation these methods remain among the best available. In this area, a substantively valid clinical trial does not appear to be possible for ethical and legal reasons [Reference O’Reilly and Vingilis57–Reference Mustafa59]. The adjustments or controls for confounding influences in the statistical models herein give all forty-six control factors explanatory priority over the explanation that the CTO is accounting for the study results. The models therefore provide a conservative estimate of the CTO association. Finally, the study results were robust in the face of a challenge to their diagnostic generalizability.
Author contributions
All authors have contributed to the conception and design, or analysis and interpretation of data, the drafting and revisions of the article, and its critically important and intellectual content. All have given approval of the manuscript submission.
Conflicts of interest
Authors Have No Conflicts Of Interest Associated With This Study.
Appendix A Supplementary data
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.eurpsy.2018.12.001.







Comments
No Comments have been published for this article.