Borderline personality disorder is well known as a severe psychiatric condition. The prevalence of this disorder is estimated at 1–2.5% in the worldwide population, 1 and at 10–50% among psychiatric patients. Societal costs associated with borderline personality disorder are substantial. Reference Ten Have, Lorsheyd, Bijl and Osterthun2 Recently, the effectiveness of two out-patient psychotherapies – schema-focused therapy (SFT) and transference-focused psychotherapy (TFP) – was compared. Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3 Both treatments aim to achieve full recovery from the disorder, unlike other therapies. Reference Linehan, Armstrong, Suarez, Allmon and Heard4 In that comparison both forms of therapy succeeded in reducing disorder-specific and general psychopathologic dysfunction, and improving health-related quality of life, with SFT being more effective on all measures. However, the most effective treatment is not necessarily the most cost-effective treatment. In the context of healthcare budget constraints, an economic evaluation can inform decisions concerning which healthcare services to offer to patients. Therefore, a cost-effectiveness analysis was performed comparing these two forms of therapy.
Method
Patients and assessments
In a multicentre trial in The Netherlands, 86 patients from four study locations were randomly allocated to either SFT (n=44) or TFP (n=42). A pre-randomisation assessment was performed; subsequently, 3-monthly assessments were made for 3 years, with a final follow-up assessment 4 years after the baseline interviews. Both interventions were individual therapies consisting of 50 min sessions twice a week for 3 years. Central to SFT is the assumption of four schema modes specific to borderline personality disorder; recovery is achieved when dysfunctional schemas no longer control or rule the patient's life. Central to TFP is a negotiated treatment contract between patient and therapist, being the treatment frame; recovery is reached when good and bad representations of self (and others) are integrated and when fixed, primitive internalised object relations are resolved. Twelve participants in the SFT group and 22 in the TFP group left the study early. A further 6 (14%) participants in the SFT group and 2 (5%) in the TFP group successfully (according to therapist and patient) terminated treatment within 3 years. For details, see Giesen-Bloo et al. Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3
Resources used
At every assessment a structured cost interview was administered by an independent research assistant. Formal registries such as hospital information systems or insurer's databases are considered to be incomplete, since a considerable amount of resource use is situated outside (mental) healthcare institutions. Reference Van Asselt, Dirksen, Arntz and Severens5 Besides, individual patient data cannot be traced from registries. Therefore, patient-reported prospective cost diaries, Reference Goossens, Rutten-van Molken, Vlaeyen and van der Linden6 or retrospective cost interviews, Reference Van den Brink, van den Hout, Stiggelbout, Putter, van de Velde and Kievit7 are the preferred instruments covering all relevant events. We chose a 3-month recall interview, Reference Severens, Mulder, Laheij and Verbeek8 since a prospective cost diary was expected to lead to more missing items, given the patient characteristics. From a societal perspective, the cost interview covered work status and absence, sources of income, domestic activities, informal care, medication use, alcohol and drugs, out-of-pocket expenses, and consumption of healthcare and societal resources (including visits to general practitioners, hospitals, psychiatrists and psychologists, crisis centres, alternative healers, social work and drug rehabilitation centres). Informal care is an important item in mental healthcare, since people with mental illness can impose a heavy burden on their environment: those close to the patient (family, friends or neighbours) take care of the patient and take over domestic tasks. A key characteristic of informal care is that caregivers would not want to care for someone outside their social environment for a similar wage. Reference Van den Berg, Brouwer and Koopmanschap9 Out-of-pocket costs are actual expenses reported by the individual and are highly relevant in people with borderline personality disorder. These costs relate to (for instance) excessive smoking and shopping, binge eating and extremely high telephone bills. Reference Van Asselt, Dirksen, Arntz and Severens5
The cost interview (based on the cost diary described by Goossens et al) Reference Goossens, Rutten-van Molken, Vlaeyen and van der Linden6 was judged by various experts and pilot tested by research assistants in patients, after which both face validity and content validity of the interview were improved. The questions constituting the cost interview were read to the participants, who indicated whether or not they had been absent from work, used a particular healthcare facility, etc. Only costs related to the person's personality disorder were considered relevant, because unrelated costs were not expected to differ between the treatment groups. Patients were explicitly asked whether they thought resource use was linked to problems arising from their personality disorder. In the rare cases in which resource use was probably disorder-related but the patient indicated that it was not, patients' judgements were overruled. For instance, if patients had regular contact with social services because of problems with raising their children and they rated this as not disorder-related, the contacts were still included in the analysis. Since for alcohol and drugs it is difficult to decide which part of the cost is related to the personality disorder, all alcohol and drug expenses were considered to be disorder-related.
The number of therapy sessions was recorded by the therapist. The number, duration and time (inside or outside office hours) of telephone contacts with the therapist were extracted from the standardised session form therapists filled out after each session. Training and supervision costs were not taken into account, because they are training costs and as such not part of the therapy.
Unit prices
Standardised Dutch unit prices were used. Reference Oostenbrink, Bouwmans, Koopmanschap and Rutten10 When a standardised unit price was not available, prices were based on tariffs. Medication costs were obtained from the Dutch Pharmacotherapeutic Compass. 11 Productivity costs, incurred when patients are unable to perform paid work, were calculated according to the human capital approach, Reference Rice and Cooper12 in which the number of hours of absence from work was multiplied by the actual gross wage per hour. For unpaid work and study, the number of hours absent was multiplied by a shadow price. The shadow price was also applied to the informal care. All unit prices were expressed in euros for the year 2000.
Outcome measures
Effectiveness was expressed as the proportion of recovered patients according to the Borderline Personality Disorder Severity Index (BPDSI) version IV, Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3,Reference Arntz, van den Hoorn, Cornelis, Verheul, van den Bosch and de Bie13 a 70-item index with nine dimensions, representing the DSM–IV borderline personality disorder criteria. Total scores range from 0 to 90. When the BPDSI score was below 15 at follow-up, patients were considered to have recovered. Additionally, effectiveness was expressed as quality-adjusted life-years (QALYs). A QALY is a measure of life expectancy, weighted by the health-related quality of life (HRQoL) represented by utility scores. Health-related quality of life was measured with the EQ–5D, which contains five dimensions: mobility, self-care, daily activities, pain/discomfort, and depression/anxiety. Reference Brooks14 Each dimension is rated at three levels: no problem, some problems and major problems. Based on preferences elicited from a general UK population, EQ–5D health states can be converted into utility scores. Reference Dolan15 The maximum possible number of QALYs within 4 years is 4 (4 years multiplied by 1, the optimal health state).
Cost-effectiveness
Two incremental cost-effectiveness ratios (ICERs) were determined. These ratios are calculated by dividing the difference in costs between the treatments by the difference in effectiveness between the treatments, and represents the extra amount of money that has to be invested or will be saved to gain or lose one extra unit of effect. The first ICER was the cost per recovered patient and the second ICER was the cost per QALY gained.
Data analysis
Costs and effects were discounted at 4%. Reference Oostenbrink, Bouwmans, Koopmanschap and Rutten10 Missing items in otherwise completed assessments were imputed with SPSS (version 12 for Windows) Missing Value Analysis, option regression. Completely missing assessments because of patients who left the study or completed the treatment before the 3-year limit were analysed by carrying the last observation forward, in accordance with Giesen-Bloo et al. Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3
For BPDSI recovery status results after 4 years, a logistic regression was performed with treatment group and baseline BPDSI score as covariates, again in accordance with Giesen-Bloo (further details available from the authors). Since cost data are generally highly skewed, and not distributed normally, bootstrap simulations with 1000 replications were performed to estimate uncertainty intervals around the mean costs. Reference Briggs, Wonderling and Mooney16,Reference Efron and Tibshirani17 For the same reasons, QALY scores and both ICERs were bootstrapped with 1000 replications. The uncertainty interval is represented by the 2.5th and 97.5th percentiles. Results of ICER bootstraps are presented in cost-effectiveness planes and cost-effectiveness acceptability curves (CEACs). Cost-effectiveness planes show differences in costs on the vertical axis and differences in effect on the horizontal axis. Bootstrapped cost-effectiveness pairs located in the northwest quadrant indicate SFT to be inferior to TFP (more costly and less effective than TFP). Cost-effectiveness pairs located in the south-east quadrant show SFT to be dominant over TFP (more effective and less costly than TFP). With respect to the other two quadrants (higher costs for better effectiveness and lower costs for lower effectiveness) the choice of an intervention depends on the threshold value, i.e. what society is prepared to pay for an effectiveness gain, or willing to accept as savings for effectiveness loss. The CEAC represents the probability that, given a certain threshold for the willingness to pay for a QALY or for recovering a patient, the intervention is cost-effective. Reference Van Hout, Al, Gordon and Rutten18
Secondary analyses
Secondary analyses were performed to assess robustness of the results, initially using the last observation carried forward method for patients who completed the therapy early with consent of the therapist but did not complete later assessments, and imputing baseline values for true ‘drop-outs’, i.e. patients who stopped therapy without consent of the therapist. We then conducted a ‘completers’ analysis, analysing data for only those patients who completed treatment. Patients who completed early with consent of their therapist were included in this analysis, those who dropped out were not.
As costs at baseline were not comparable between both groups, a correction was performed for the following measurements by means of a regression analysis as recommended by Manca et al. Reference Manca, Hawkins and Sculpher19 A correction was also performed for utility and BPDSI scores. An analysis per recovered patient with a healthcare perspective, meaning that only direct healthcare costs (including costs of therapy) were considered, was followed by an investigation of the impact of the unit price of a therapy session, the unit price of informal care and out-of-pocket costs on total costs. We separately doubled and halved the costs of these items. The results of the first four secondary analyses are again represented in a CEAC, combined with the CEAC of the main analysis.
Results
The demographic characteristics of the participants are shown in Table 1.
Table 1 Baseline characteristics of study participants (n=86)

| SFT group (n=44) | TFP group (n=42) | P a | |
|---|---|---|---|
| Age, years: means (s.d.) | 31.70 (8.9) | 29.45 (6.5) | 0.15 |
| Gender | |||
| Female, n (%) | 40 (90.9) | 40 (95.2) | 0.43 |
| Education, n (%) | |||
| Graduate/professional | 6 (13.6) | 4 (9.5) | 0.22 |
| College graduate | 3 (6.8) | 7 (16.7) | |
| Some college | 17 (38.6) | 14 (33.3) | |
| High-school graduate | 5 (11.4) | 10 (23.8) | |
| Grades 7–11 | 13 (29.6) | 7 (16.7) | |
| Employment status, n (%) | |||
| Homemaker | 8 (18.2) | 5 (119) | 0.89 |
| Student | 3 (6.8) | 6 (14.3) | |
| Employed | 9 (20.5) | 8 19.0) | |
| Disability | 17 (38.6) | 17 (40.5) | |
| Welfare | 7 (5.9) | 6 (14.3) |
SFT, schema-focused therapy; TFP, transference-focused psychotherapy
a. Based on the Pearson chi-squared test
Costs
Baseline assessment
At baseline, costs were not distributed normally (P=0.029, Kolmogorov–Smirnov test. The bootstrapped total costs at baseline were €4324 for TFP and €3331 for SFT, a difference of about €900. However, neither of the cost categories nor the total societal cost was significantly different between conditions.
After start of treatment
Bootstrapped societal costs over 4 years were €46 795 for TFP and €37 826 for SFT (non-significant difference; Table 2). The direct non-healthcare costs were significantly different between the two intervention therapies, mainly owing to informal care costs. With respect to direct healthcare costs, treatment costs (including costs of telephone contacts with the therapist for SFT) were about €2200 higher for SFT, whereas the costs of visits to mental healthcare centres and other healthcare facilities were about €3500 higher for TFP. Table 3 presents mean societal costs, EQ–5D utility scores, BPDSI scores and percentage recovered patients per measurement. Costs in both groups decreased with time. In addition, aside from the second assessment when costs were comparable between the two groups, the TFP costs were continuously higher.
Table 2 Total costs per cost item and bootstrapped costs for subtotals per patient for the schema-focused therapy group (n=44) and the transference-focused psychotherapy group (n=42)
| Cost category | TFP costs, € | SFT costs, € | Incremental costs, € | 2.5–97.5 percentile |
|---|---|---|---|---|
| Direct healthcare mean costs | ||||
| Psychotherapy | 10 876 | 12 946 | ||
| Contact with therapist by telephone | 2 | 132 | ||
| Other care at treatment centre | 875 | 565 | ||
| General practitioner | 191 | 112 | ||
| Healthcare, other a | 6883 | 3851 | ||
| Medication | 1494 | 1273 | ||
| Alternative healers | 190 | 91 | ||
| Subtotal | 20 512 | 18 969 | ||
| Bootstrapped subtotal, mean (s.d.) | 20 589 (2754) | 19 020 (2097) | –1269 | –8514 to 4973 |
| Direct non-healthcare mean costs | ||||
| Paid help | 255 | 170 | ||
| Societal services b | 353 | 238 | ||
| Informal care | 8223 | 3053 | ||
| Subtotal | 8831 | 3460 | ||
| Bootstrapped subtotal, mean (s.d.) | 8915 (2189) | 3482 (785) | –5433 | –10 385 to 1469 |
| Lost production mean costs | ||||
| Paid work | 890 | 2016 | ||
| Unpaid work | 3612 | 536 | ||
| Domestic tasks | 7107 | 8255 | ||
| Subtotal | 11 609 | 10 807 | ||
| Bootstrapped subtotal, mean (s.d.) | 11 495 (2886) | 10 704 (2394) | –791 | –8204 to 6443 |
| Out-of-pocket mean costs | ||||
| Reported by patient c | 2821 | 1953 | ||
| Alcohol and drugs | 3238 | 2804 | ||
| Subtotal | 6059 | 4757 | ||
| Bootstrapped subtotal, mean (s.d.) | 6073 (897) | 4752 (734) | –1321 | –3578 to 991 |
| Total societal mean costs | 47 010 | 37 994 | ||
| Bootstrapped total costs, mean (s.d.) | 46 795 (5630) | 37 826 (3411) | –8969 | –21 775 to 3546 |
SFT, schema-focused therapy; TFP, transference-focused psychotherapy
Table 3 Costs, EQ–5D utility scores, disorder severity scores and patient recovery over the course of the study

| TFP group (n=42) | SFT group (n=44) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Assessment | Cost, € Mean (s.d.) | Utility score Mean (s.d.) | BPDSI score Mean (s.d.) | Patients recovered % | Cost, € Mean (s.d.) | Utility score a Mean (s.d.) | BPDSI score Mean (s.d.) | Patients recovered % | ||||||
| 1 | 4238 (3319) | 0.49 (0.26) | 34.84 (8.76) | 0 | 3339 (3222) | 0.46 (0.31) | 33.14 (7.13) | 0 | ||||||
| 2 | 3712 (2702) | 049 (0.32) | 29.28 (7.91) | 2 | 3785 (2461) | 0.49 (0.30) | 27.43 (9.53) | 14 | ||||||
| 3 | 4049 (4027) | 0.66 (0.26) | 28.06 (8.86) | 5 | 3549 (2057) | 0.50 (0.31) | 24.34 (11.33) | 18 | ||||||
| 4 | 3711 (2905) | 0.60 (0.31) | 27.16 (8.53) | 7 | 3113 (1806) | 0.46 (0.35) | 25.31 (9.58) | 11 | ||||||
| 5 | 3413 (2502) | 0.63 (0.26) | 24.33 (10.56) | 19 | 2804 (1621) | 0.54 (0.32) | 22.41 (10.40) | 25 | ||||||
| 6 | 3160 (2589) | 0.60 (0.28) | 25.53 (9.66) | 14 | 2536 (1479) | 0.50 (0.35) | 21.28 (11.14) | 34 | ||||||
| 7 | 2878 (2273) | 0.63 (0.29) | 24.96 (10.81) | 17 | 2370 (1511) | 0.55 (0.32) | 21.90 (11.02) | 27 | ||||||
| 8 | 2798 (2325) | 0.62 (0.30) | 24.01 (11.03) | 19 | 2500 (1807) | 0.59 (0.32) | 19.57 (11.99) | 36 | ||||||
| 9 | 2788 (2325) | 0.61 (0.30) | 22.91 (11.40) | 31 | 2348 (1653) | 0.63 (0.31) | 19.04 (10.64) | 36 | ||||||
| 10 | 2552 (2273) | 0.60 (0.32) | 23.47 (10.42) | 24 | 1961 (1402) | 0.60 (0.34) | 19.90 (11.03) | 36 | ||||||
| 11 | 2554 (2304) | 0.60 (0.31) | 23.01 (11.79) | 29 | 1947 (1348) | 0.61 (0.32) | 18.01 (11.52) | 48 | ||||||
| 12 | 2546 (2343) | 0.58 (0.33) | 24.04 (11.80) | 26 | 1963 (1392) | 0.59 (0.32) | 18.52 (11.64) | 48 | ||||||
| 13 | 2652 (2599) | 0.60 (0.32) | 22.71 (10.61) | 24 | 1946 (1617) | 0.67 (0.29) | 17.76 (11.32) | 45 | ||||||
| 14 b | 10 198 (10 878) | 0.61 (0.32) | 21.98 (11.00) | 29 | 7172 (9912) | 0.63 (0.34) | 16.94 (11.34) | 52 | ||||||
BPDSI, Borderline Personality Disorder Severity Index; SFT, schema-focused therapy; TFP, transference-focused psychotherapy
a. For utility scores in SFT, data for 1 patient were missing for all measurements, therefore n=43 here
b. Assessment 14 covers a whole year, therefore costs are about four times as high
a. Crisis help, first aid, psychotherapy other than the intervention under study, community healthcare, psychiatric hospital, general hospital, physiotherapy
b. Social work, addiction clinic and counselling, sex counselling, abortion clinic
c. Mostly costs of binge eating, excessive smoking, excessive use of mobile telephone, impulsive shopping
Effectiveness
BPDSI score
The proportion of patients who had recovered after 4 years was 52% for the SFT group and 29% for the TFP group (Table 3). Logistic regression analysis with treatment group and BPDSI baseline score as covariates showed a significant effect in favour of SFT (Wald test 4.45, P=0.035; OR=2.64, 95% CI 1.07–6.49). Without the baseline BPDSI the group effect was similar. (For details of the BPDSI results, see Giesen-Bloo et al; Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3 further details are available from the authors.)
Quality-adjusted life-years
For one participant no EQ–5D score was available, therefore QALY results and ICERs for cost per QALY are based on 85 patients. Table 3 shows that baseline utility scores were not distributed normally (P=0.037, Kolmogorov–Smirnov test). Baseline utility scores were 0.49 for the TFP group and 0.46 for the SFT group (P=0.734, Mann–Whitney test). In TFP, utility scores increased early in treatment and more or less remained stable, whereas in SFT utility scores continued to increase. As a result, total QALYs over the 4-year period were 2.15 for SFT and 2.27 for TFP. The bootstrapped difference in QALYs between SFT and TFP of −0.12 (95% UI −0.51 to 0.28) was not statistically significant.
Cost-effectiveness
Societal costs per recovered patient
As the societal costs in the SFT group were lower and recovery rate was higher compared with the TFP group, SFT was dominant over TFP (Table 4). The bootstrapped results (Fig. 1) show that 91% of the cost-effectiveness pairs are in the south-east quadrant, where SFT is dominant. Another 8% lie in the north-east (i.e. more costly, more effective) quadrant, and 1% is located in both west quadrants, where SFT is less effective than TFP. The CEAC (Fig. 2, main analysis) indicates that, regardless of the threshold value, the chance that SFT is cost-effective is over 90%.

Fig. 1 Bootstrapped costs and effects for cost per recovered patient, showing 1000 bootstrap replications for incremental cost-effectiveness of schema-focused therapy compared with transference-focused psychotherapy. Costs are plotted on the y axis and effects on the x axis, so a bootstrap replication in the south-east quadrant means that schema-focused therapy is less costly and more effective than transference-focused psychotherapy for that replication.
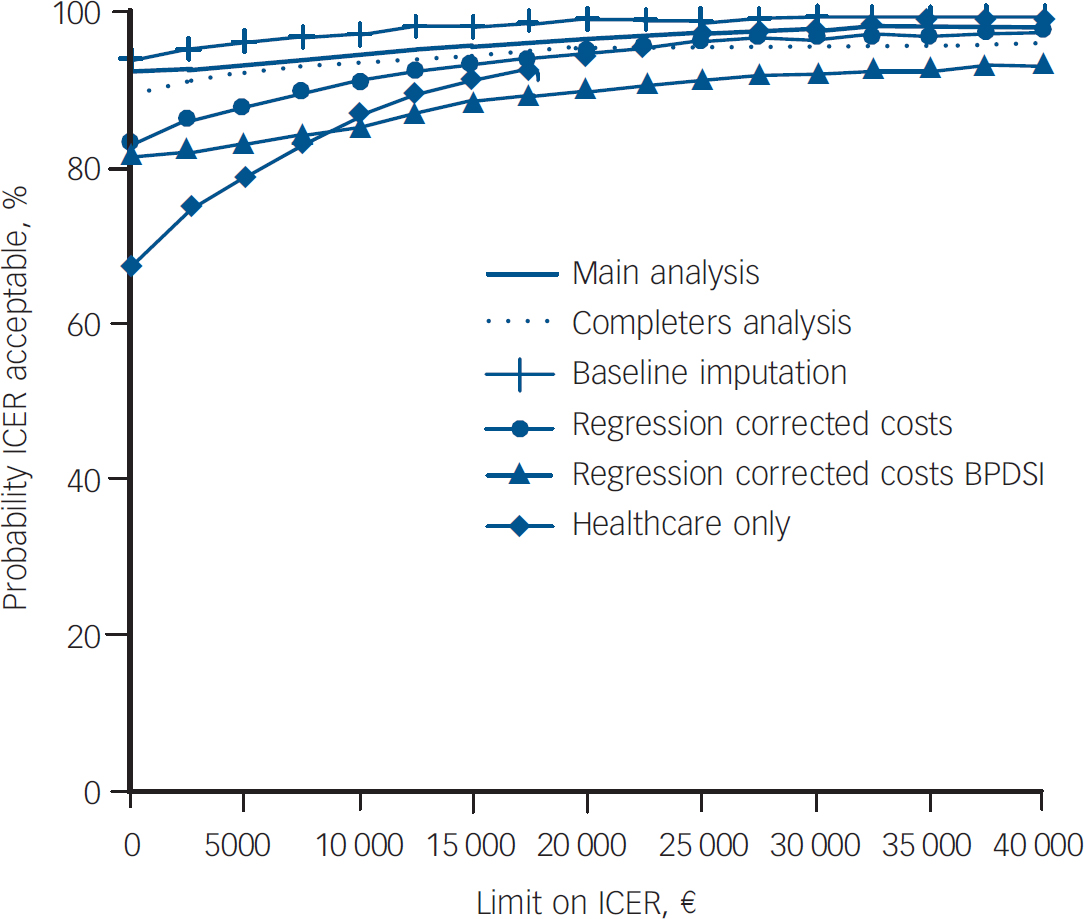
Fig. 2 Cost-effectiveness acceptability curves for secondary analyses of cost per recovered patient. BPDSI, Borderline Personality Disorder Severity Index; ICER, incremental cost-effectiveness ratio. The curves indicate the probability (y axis) of schema-focused therapy being cost-effective compared with transference-focused psychotherapy, given the threshold value (x axis) for recovering a patient.
Table 4 Results of main and secondary analyses
| TFP group (n=42) | SFT group (n=44) | ICER | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Costs, € | Proportion of patients recovered | QALYs | Costs, € | Proportion of patients recovered | QALYs (n=43) | Costs per recovered patient (n=86) | Costs per QALY, € (n=85) | ||||||
| Main analysis | 47 010 | 0.29 | 2.27 | 37 994 a | 0.52 | 2.15 | Dominance | 90 457 saving/QALY lost | |||||
| Completers analysis (n=53) | 42 267 | 0.38 | 2.47 | 35 567 | 0.59 | 2.34 | Dominance | 51 541 saving/QALY lost | |||||
| (n=21) | (n=21) | (n=21) | (n=32) | (n=32) | (n=32) | ||||||||
| Baseline values for drop-outs | 49 733 | 0.19 | 2.05 | 39 821 b | 0.43 | 2.17 | Dominance | Dominance | |||||
| Regression corrected costs only | 28 227 | 0.29 | 2.27 | 23 195 | 0.52 | 2.15 | Dominance | 41 933 saving/QALY lost | |||||
| Regression corrected costs and QALYs | 28 227 | NA | 1.97 | 22 115 | NA | 1.87 | NA | 64 008 saving/QALY lost | |||||
| (n=43) | |||||||||||||
| Regression corrected costs and BPDSI score | 28 227 | 0.67 | NA | 23 195 | 0.82 | NA | Dominance | NA | |||||
| Healthcare perspective | 20 512 | 0.29 | NA | 18 969 | 0.52 | NA | Dominance | NA | |||||
| Half unit-price session | 41 572 | 31 521 | |||||||||||
| Double unit-price session | 57 886 | 50 939 | |||||||||||
| Halt unit-price informal care | 42 899 | 36 467 | |||||||||||
| Double unit-price informal care | 55 232 | 41 047 | |||||||||||
| Half out-of-pocket costs | 45 599 | 37 017 | |||||||||||
| Double out-of-pocket costs | 49 831 | 39 947 | |||||||||||
BPDSI, Borderline Personality Disorder Severity Index; ICER, incremental cost-effectiveness ratio; NA, not applicable; QALY, quality-adjusted life-year; SFT, schema-focused therapy; TFP, transference-focused psychotherapy
a. Costs for n=43 are €36 630 (used for calculation costs/QALY)
b. Costs for n=43 are €39 538 (used for calculation costs/QALY)
Societal cost per QALY
The incremental cost-effectiveness ratio based on the QALY shows that €90 457 is saved when one QALY is sacrificed, as SFT was less costly and less effective than TFP (Table 4). The bootstrapped results (Fig. 3) show that 68% of the cost-effectiveness pairs are in the south-west quadrant, where SFT is less costly and less effective. The south-east quadrant (i.e. the dominance quadrant) contains 28% of the replications, and the final 4% are located in the inferiority quadrant. The cost-effectiveness acceptability curve (Fig. 4, main analysis) indicates that the probability of SFT being cost-effective decreases with an increasing threshold value. Assuming that society's maximum willingness to pay is €20 000 for a QALY gain (or accepts a minimum compensation of €20 000 for a QALY loss), the probability that SFT is cost-effective is 84%.
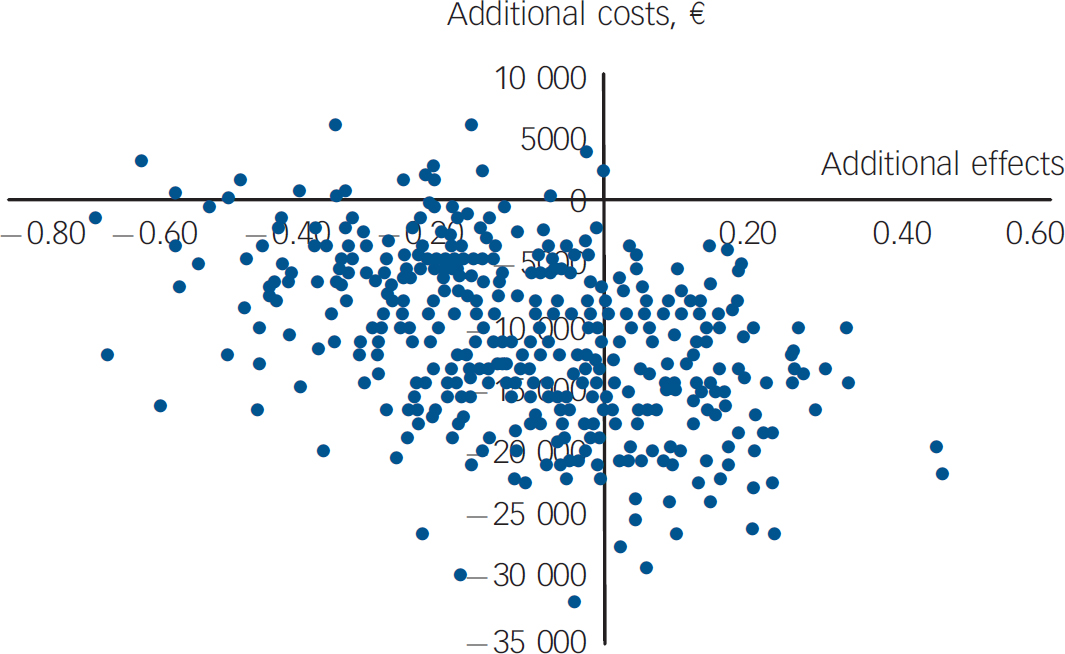
Fig. 3 Bootstrapped costs and effects for cost per quality-adjusted life-year, showing 1000 bootstrap replications for incremental cost-effectiveness of schema-focused therapy compared with transference-focused therapy. Costs are plotted on the y axis and effects on the x axis, so a replication in the south-west quadrant means that schema-focused therapy is less costly but also less effective than transference-focused psychotherapy for that replication.

Fig. 4 Cost-effectiveness acceptability curves for secondary analyses of cost per quality-adjusted life-year. ICER, Incremental cost-effectiveness ratio. The curves indicate the probability (y axis) of schema-focused therapy being cost-effective compared with transference-focused psychotherapy, given the threshold value (x axis) for a quality-adjusted life-year.
Secondary analyses
Costs per recovered patient
Table 4 also shows the secondary analyses. For costs per recovered patient, results were robust, meaning that SFT dominates TFP. The cost-effectiveness acceptability curves demonstrate that, regardless of the threshold value, the probability that SFT is cost-effective is consistently over 90% (Fig. 2). From a healthcare perspective, the CEAC is less favourable for SFT. With respect to varying the unit prices and the out-of-pocket costs, total costs of SFT stayed below costs of TFP in all cases.
Costs per QALY
With respect to costs per QALY (Table 4), results were robust when using the completers analysis and the regression corrected analyses. However, using the baseline values for imputation of missing values, SFT became dominant. The cost-effectiveness acceptability curves (Fig. 4) show that baseline value imputation leads to more favourable results for SFT compared with the main analysis. However, regression correction and a completers analysis both lead to less favourable results for SFT. The descending CEACs mean that the probability of SFT being cost-effective decreases if the value society attaches to a QALY increases, dropping from 96% (best case) to 53% (worst case).
Discussion
Schema-focused therapy, compared with TFP, was cost-effective when clinical outcome was considered. However, results in terms of QALYs were uncertain. Total societal costs were not statistically significantly different between treatments, although costs for TFP were almost e9000 higher than for SFT; only the costs of informal care were significantly higher for the former therapy. This might be a consequence of the fact that in SFT professional support is a central part of therapy, offering patients the possibility of telephone contacts and extra sessions with their therapist, whereas TFP may be more reliant on informal care. The fact that the larger part of the total costs in both therapies was outside the healthcare sector demonstrates the importance of using a societal viewpoint in economic evaluations of interventions for borderline personality disorder. Although direct healthcare costs were not statistically significantly different, there were notable differences between both groups. For the SFT group costs of psychotherapy and telephone contacts were higher, whereas for the TFP group the costs of general practitioner care, mental healthcare and other healthcare facilities were higher. Again, it can be speculated that these differences might be explained by the fact that patients found more comfort and support in SFT, whereas in TFP this was additionally sought in other healthcare facilities.
QALYs
Utility scores increased from 0.49 to 0.61 in the TFP group and from 0.46 to 0.63 in the SFT group, improvements of 0.12 and 0.17 respectively. The minimally important difference for EQ–5D utility scores is considered to be 0.03 points; Reference Marra, Woolcott, Kopec, Shojania, Offer, Brazier, Esdaile and Anis20 both therapies thus had a clinically relevant effect on quality of life. Therefore, in this sample, the EQ–5D can be considered sensitive to change. However, the resulting QALY was unable to discriminate significantly between the two intervention therapies, although the proportion of recovered patients was higher in the SFT group. Quality-adjusted life-years based on the 4-year period were slightly lower for the SFT group, resulting in an ICER indicating a saving of over €90 000 for a QALY loss.
To date there is no consensus about a reasonable threshold value for cost-effectiveness. Most studies with the explicit goal of determining a threshold found values ranging from €10 000 to €27 000. Reference Gyrd-Hansen21–Reference Laupacis, Feeny, Detsky and Tugwell23 However, in practice, thresholds used for appraisal of new interventions may be higher, around €40 000 for the UK and €80 000 for The Netherlands. Reference Devlin and Parkin24,25 The CEACs show a range of thresholds, varying from €0 to €40 000. In this study, when applying a €20 000 per QALY threshold, SFT in the main analysis would have an 84% probability of being cost-effective. In the secondary analyses, the worst-case scenario had a probability of 68% and the best-case scenario had a probability of 94%. Given this range, the probability that SFT is more cost-effective than TFP in terms of QALYs can be considered moderate to high, in addition to the fact that this probability was already high for the analysis per recovered patient.
BPDSI v. EQ–5D
It is difficult to explain what the reason for the divergence between BPDSI and QALY results might be. When a patient recovers from borderline personality disorder, one would expect the HRQoL to improve correspondingly to at least some extent. In the long run, this was indeed the case: the slopes in increase of HRQoL were significantly steeper in the SFT group than in the TFP group. Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3 However, during the first half-year of treatment, QALY and BPDSI scores diverged markedly, and as a consequence, during the first 2 years of treatment, the HRQoL in the SFT patients was lower than that in TFP patients. This difference is difficult to understand as it was not paralleled in any of the clinical outcome measures. At follow-up at 4 years, the HRQoL in the SFT group was slightly higher than the HRQoL in the TFP group, but not enough to offset the total QALY difference. Maybe SFT is initially experienced as more burdensome by patients, and it may take time for clinical improvement to be translated into an increase in HRQoL. Another reason for the discrepancy might be a difference in responsiveness between the EQ–5D, which has 5 items each with three-point scale responses, and the BPDSI, which has 70 items with mostly ten-point scale responses. There is little published information concerning the use of the EQ–5D in a population with borderline personality disorder. For depression, the EQ–5D seems useful and sensitive to change; Reference Hayhurst, Palmer, Abbott, Johnson and Scott26,Reference Sapin, Fantino, Nowicki and Kind27 in schizophrenia, results are contradictory. Reference Van de Willige, Wiersma, Nienhuis and Jenner28,Reference Prieto, Sacristan, Hormaechea, Casado, Badia and Gomez29
Limitations
A number of limitations should be addressed. First, we used the last observation carried forward method to impute missing assessments. Although this is in accordance with the clinical study, this method is regarded as naïve. Reference Oostenbrink and Al30 We therefore also performed a multiple imputation. Reference Rubin and Schenker31 However, probably because of the high cumulative drop-out at the last three measurements, point estimates resulting from the multiple imputation tended heavily towards extreme (and even impossible) values. Because this tendency could not be justified from the trends in the observed data, we have not included the multiple imputation results in this paper. Second, the fact that we only included disorder-related costs might have led to bias in the estimate of the total costs, since patient judgement of what is and what is not disorder-related may be flawed. However, as we do not expect patients' judgements in the SFT group to differ systematically from those in the TFP group, this presumably did not affect the incremental costs. Third, the time horizon of the analysis was 4 years; more long-term information should be collected to confirm the results now presented. Fourth, the economic evaluation was limited to the comparison of only two possible treatments. Other alternatives, such as natural course and care as usual, have not been considered. The use of a single randomised controlled trial as a vehicle for economic evaluation is often an insufficient basis for decision-making, because decision-makers need to be informed about costs and effects for the full range of alternative interventions. Reference Sculpher, Claxton, Drummond and McCabe32 In that respect, our study has contributed evidence to the broader case of cost-effectiveness of treatment for borderline personality disorder.
Implications of the study
As this is the first cost-effectiveness analysis of psychotherapy in the field of borderline personality disorder from a comprehensive societal perspective, it is difficult to place the results in a broader perspective. Even for the much better-documented case of treatment for depression, comparisons between studies are complicated because of vastly different interventions, outcome measures and cost perspectives. Reference Barrett, Byford and Knapp33 The same applies to personality disorders in general and borderline personality disorder in particular. However, our study shows that long-term psychotherapy for borderline personality disorder improves HRQoL and decreases societal costs. In terms of recovered patients, there is a high probability that SFT is more cost-effective than TFP. In terms of QALYs, the probability that SFT is cost-effective is moderate to high.
Future research should further investigate the reason for the discrepancy between the BPDSI and QALY scores, and the relation between the EQ–5D and other measures of quality of life among people with borderline personality disorder. Furthermore, we agree with Giesen-Bloo et al that different comparators such as care as usual and natural course should be studied, Reference Giesen-Bloo, van Dyck, Spinhoven, van Tilburg, Dirksen, van Asselt, Kremers, Nadort and Arntz3 including economic evaluations with a longer period of follow-up.
Acknowledgements
We are grateful to all patients, research assistants and therapists who took part in this trial. We thank Fons Kessels for his support in performing the statistical analyses. The clinical trial and the economic evaluation were financially supported by the Dutch Healthcare Insurance Board (CVZ grant OG 97-002).











eLetters
No eLetters have been published for this article.