Complex post-traumatic stress disorder in ICD-11
The World Health Organization's ICD-11 has taken a new approach to diagnose disorders of traumatic stress.Reference Maercker, Brewin, Bryant, Cloitre, van Ommeren and Jones1 The ICD-11 includes two sibling disorders, post-traumatic stress disorder (PTSD) and complex post-traumatic stress disorder (CPTSD; see Brewin et al Reference Brewin, Cloitre, Hyland, Shevlin, Maercker and Bryant2 for a review). PTSD features symptoms reflecting three clusters: re-experiencing of the trauma in the present, avoidance of traumatic reminders and a persistent sense of threat. CPTSD includes the core PTSD symptoms plus additional symptoms that identify ‘disturbances in self-organisation’ (DSO), which may result from sustained, repeated and multiple forms of traumatic exposures. There are three DSO symptom categories: affective dysregulation, negative self-concept and disturbances in relationships. The recently promoted network approach to psychopathology defines mental disorders as sets of interacting symptoms.Reference Borsboom3 It assumes that symptoms can be associated with external factors, such as a traumatic event. Once triggered, a symptom may lead to other symptoms (e.g. flashbacks may lead to sense of threat, which may lead to anger problems) and maybe even activate symptom loops.Reference Cramer, van Borkulo, Giltay, van der Maas, Kendler and Scheffer4
CPTSD as symptom network
Network analysis allows for a visual representation of symptom interaction and can illustrate which symptoms are more central than others. These symptoms are arguably the most important elements in a disorder and clinicians could prioritise central over noncentral symptoms in their treatment approach to enable rapid response to therapy. The symptom ‘worthlessness’ was found to be the most central ICD-11 CPTSD symptom in one study.Reference Knefel, Tran and Lueger-Schuster5 Network analysis explores the interplay of symptoms and promotes a comprehensive understanding of CPTSD. However, it is not yet clear whether the network structure and centrality of symptoms is specific to certain groups or generalises across different populations with CPTSD. Although studies corroborate the stability of psychopathological networks, their replicability was recently debated.Reference von Stockert, Fried, Armour and Pietrzak6–Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk and Bockting8 In this study, we broaden the knowledge about CPTSD as a new diagnosis by analysing its network structure across different countries and providing researchers and clinicians the opportunity to better understand the symptom interactions underlying this condition.
This study aimed to investigate and compare, for the very first time, the network structure and symptom centrality of ICD-11 CPTSD in four nationally representative samples from Germany, Israel, the UK and the USA.
Method
Participants
Participants came from four nationally representative samples from Germany, Israel, the UK and the USA (total N = 6417). Reporting the experience of at least one potentially traumatic event (PTE) in a screening tool was an inclusion criterion for the UK and USA studies. This inclusion criterion was not required for the Israeli sample, as recent armed conflicts along with terror attacks put almost the entire Israeli population under direct or potential threat to life, corresponding with exposure to a traumatic event. Experience of a traumatic events was not an inclusion criterion in the German study; however, the trauma-specific symptom measures were only administered to those participants who reported such an experience. In this study, those participants who reported the experience of a PTE and showed functional impairment by symptoms of CPTSD were included. This inclusion criterion was administered to investigate the network structure of CPTSD only in participants who are actually impaired in their daily functioning by CPTSD symptoms and exclude those who experienced a PTE but are not impaired by any related symptom. Functional impairment was assessed with six queries in the International Trauma Questionnaire (ITQ), three assessing functional impairment as related to the PTSD symptoms and three as related to the DSO symptoms (German study: five items). All individuals who reported at least ‘moderate’ (a value of two or higher) functional impairment in one or more of the queries were included in the study. This resulted in a total sample size of N = 1591 (24.8%). The mean age for this sample was 43.55 years (s.d. 15.10, range 14–99) and the majority of the sample were women (67.6%). The higher rate of female participants represents the frequently reported gender differences in the prevalence of many anxiety and mood disorders.Reference Seedat, Scott, Angermeyer, Berglund, Bromet and Brugha9 The German sample was assessed with paper-and-pencil questionnaires, whereas all three other samples were assessed with online versions of the questionnaires. The estimates of a probable PTSD and CPTSD diagnosis in the included sample were 12.9% and 20.6%, respectively; these rates may vary from the original studies because of differences in applied diagnostic algorithms and subsamples selected for analyses (Table 1). The Institutional Review Board (IRB) of the respective institutions approved all studies (German study: IRB at Department of Medical Psychology, University of Leipzig; Israeli study: IRB at Ariel University; UK and USA studies: National College of Dublin Ethics Committee) and all participants gave written informed consent.
Table 1 Descriptive sample characteristics and symptoms profiles
Symptoms assessed with the International Trauma Questionnaire. CPTSD, complex post-traumatic stress disorder; PTSD, post-traumatic stress disorder.
a. Based on N = 274 for the German sample.
b. Estimates of probable PTSD and CPTSD may differ from the original studies based on differences in the used items, diagnostic algorithms and subsample selected for analyses.
c. t-tests comparing total means: Germany < Israel < USA < UK, all t-values > 2.78, all P-values < 0.006.
The first sample comprised 280 participants from a representative sample of the German general population.Reference Maercker, Hecker, Augsburger and Kliem10 The sample was representative in terms of age, gender and residence in Germany. A trained study assistant visited each participant and supported their self-report if they had any difficulties understanding the questions. PTEs were assessed with a checklist including eight events (e.g. ‘threatened to be physically attacked’, ‘sexual abuse before the age of 14’), one question on ‘witnessing a traumatic event’ and an open question about ‘another terrible event or a catastrophe’. In the subsample, the most prevalent type of events were ‘witnessing a traumatic event’ (39.6%), ‘physical violence’ (27.5%), ‘severe accident’ (25.7%), ‘life-threatening illness’ (21.8%) and ‘rape’ (13.2%).
The second sample comprised 336 Israeli adults.Reference Ben-Ezra, Karatzias, Hyland, Brewin, Cloitre and Bisson11 The sample was recruited with stratified and random sampling methods from an internet panel that represented the general Israeli population. PTEs were assessed with the Life Events Checklist, revised version (LEC-RReference Gray, Litz, Hsu and Lombardo12). The LEC-R assesses exposure to 18 traumatic events, two of which specifically inquire about childhood trauma and the 19th item can be used to indicate exposure to a trauma that is not listed. The most prevalent PTEs in this sample were ‘physical assault as adult’ (43.8%), ‘transportation accident’ (42.0%), ‘combat or exposure to a war zone’ (36.6%) and ‘other unwanted or uncomfortable sexual experience’ (32.7%).
The third sample comprised 447 adults from the UK.Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker13 The sample was drawn through probability-based sampling from an online research panel that is representative of the entire UK adult population. PTEs were assessed with the Life Events Checklist for DSM-5 (LEC-5Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr14), assessing exposure to 16 traumatic events and one item can be used to indicate exposure to a trauma that is not listed. The LEC-5 was used twice, once referring to childhood and the second time referring to adulthood. The most prevalent PTEs during childhood in this sample were ‘physical assault’ (45.0%), ‘other unwanted or uncomfortable sexual experiences’ (34.2%), ‘sudden, unexpected death of a close person’ (32.0%) and ‘sexual assault during childhood’ (23.5%). In adulthood, the most prevalent events were ‘sudden, unexpected death of a close person’ (49.2%), ‘physical assault’ (40.0%), ‘other unwanted or uncomfortable sexual experiences’ (31.3%) and ‘transportation accident’ (30.2%). Additionally, ten adverse childhood experiences (ACEs) were assessed.Reference Felitti, Anda, Nordenberg, Williamson, Spitz and Edwards15 The most prevalent ACEs were ‘emotional neglect’ (55.0%), ‘verbal or physical threats’ (52.1%), ‘physical assault’ (48.3%) and ‘parental divorce/separation’ (43.4%).
The fourth sample comprised 528 adults from the USA.Reference Shevlin, Hyland, Roberts, Bisson, Brewin and Cloitre16 The participants for this study were a nationally representative household sample of adults currently residing in the USA. Data were collected using an existing online research panel that is representative of the entire USA population. Panel members were randomly recruited through probability-based sampling. PTEs were assessed with a 14-item version of the LEC-5.Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr14 The LEC-5 was used twice, for PTEs in childhood and in adulthood. In childhood, the most prevalent events were ‘sudden, unexpected death of a close person’ (42.6%), ‘natural disaster’ (41.1%), ‘transportation accident’ (38.4%) and ‘physical assault not by caregiver’ (30.9%). The most prevalent events in adulthood were ‘sudden, unexpected death of a close person’ (62.1%), ‘transportation accident’ (59.7%), ‘natural disaster’ (43.2%) and ‘physical assault’ (32.4%). Additionally, ten ACEs were assessed.Reference Felitti, Anda, Nordenberg, Williamson, Spitz and Edwards15 The most prevalent ACEs in this study were ‘parental divorce/separation’ (45.8%), ‘drug/alcohol problems in the home’ (41.9%), ‘emotional neglect’ (40.0%) and ‘verbal or physical threats’ (39.4%).
Measures
All four studies used the ITQReference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker13 to assess the symptoms of ICD-11 PTSD and CPTSD. The ITQ is a self-report measure of the ICD-11 symptoms of PTSD and CPTSD (see Karatzias et al Reference Karatzias, Cloitre, Maercker, Kazlauskas, Shevlin and Hyland17 for a recent review). The final version of the ITQ includes 12 items assessing symptoms and six items assessing functional impairment in the areas of relationships and social life, work and other important parts of life such as parenting or school.Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker13 Six of the symptom indicators measure three PTSD clusters (two items for each cluster): re-experiencing in the here and now, deliberate avoidance of traumatic reminders (internal or external) and a sense of current threat. A further six symptom indicators measure the three DSO clusters (two items for each cluster): affective dysregulation (hyperactivation and hypoactivation), negative self-concept and difficulties in relationships.
Respondents are instructed to respond in relation to how much they have been bothered by each PTSD symptom in the past month and are instructed to answer the DSO items in relation to how they typically feel, think about themselves and relate to others. All items are answered on a five-point scale anchored by ‘not at all’ (0) and ‘extremely’ (4). Criteria for a probable PTSD diagnosis require a score of ≥2 (‘moderately’) for at least one of the two symptom indicators from each of the three PTSD clusters, plus endorsement of functional impairment associated with these symptoms (a score of ≥2 ‘moderately’). A probable CPTSD diagnosis requires that the PTSD criteria are met in addition to a score of ≥2 (‘moderately’) for at least one of two symptom indicators from each of the three DSO clusters plus endorsement of functional impairment associated with these symptoms. The ICD-11's taxonomic structure means that an individual can only be diagnosed with PTSD or CPTSD, not both. The studies in English-speaking countries used the English version of the ITQ,Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker13 the German study used the German versionReference Knefel, Lueger-Schuster and Maercker18 and the Israeli study used the Israeli version.Reference Ben-Ezra, Karatzias, Hyland, Brewin, Cloitre and Bisson11 All versions have proven good psychometric properties (English version;Reference Karatzias, Shevlin, Fyvie, Hyland, Efthymiadou and Wilson19 German version;Reference Knefel, Tran and Lueger-Schuster5 Israeli versionReference Gilbar, Hyland, Cloitre and Dekel20). Cronbach's alpha of the total scale was good in all samples, ranging from α = 0.87 to α = 0.90, and α = 0.89 in the total sample.
Data analysis
We conducted four steps of analysis, following the statistical procedure described by Fried et al:Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk and Bockting8 network estimation, network inference, network stability and network comparison. We used the R statistical environment21 for all analyses and the package qgraphReference Epskamp, Cramer, Waldorp, Schmittmann and Borsboom22 to visualise the networks. The statistical procedure is described in more detail in the supplementary material available at https://doi.org/10.1192/bjp.2018.286.
Missing values
We excluded participants who had 20% or more missing values in the 12 ITQ items. In the German sample, two people were excluded, resulting in the final number of 280 participants, and ten people from the USA sample were excluded, resulting in the final number of 528 participants. No person from the Israeli or the UK sample was excluded. In the final four data-sets, there were only a few missing values (0.52% of all data points were missing). We used pairwise complete observations to estimate the correlations among the symptoms in these four data-sets. To rule out a possible bias introduced by excluding 12 individuals and using pairwise complete observations for the analysis, we additionally used a multiple imputation technique to estimate missing values. There were no relevant differences between the correlation matrices based on the imputed and the non-imputed data (see supplementary material, Data Analysis: Missing values for more details).
Network estimation
Symptom networks consist of nodes, representing symptoms, and edges, reflecting the pairwise relations between two nodes. We used the fused graphical lasso to jointly estimate the network structures of the four samples. Because CPTSD symptoms can be considered ordered-categorical, the estimation of the 12-item networks are based on the polychoric correlations among symptoms (see supplementary material, Data Analysis: Network estimation for more details).
Network inference
We used three parameters to describe the connectedness of each node in the four jointly estimated networks: the centrality index node strength, the predictability of each node, and the bridge strength of each node. Strength refers to the sum of all edges connected to a specific node.Reference Opsahl, Agneessens and Skvoretz23 Predictability refers to the estimated shared variance of each node with all of its neighbours.Reference Haslbeck and Fried24 Bridge strength is defined as the sum of all edges that exist between each PTSD node and all six DSO nodes, and vice versa. (see supplementary material, Data analysis: Network inference for more details).
Network stability
We examined the stability of the individually estimated networks,Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk and Bockting8 including estimating 95% confidence intervals around the edge weights and estimating a correlation-stability coefficient for strength centrality (see supplementary material, Data analysis: Network stability for more details).
Network comparison
We compared the networks across the four samples in several ways: We correlated the edge weights across the four networks and then used an overall test to investigate whether all edges in all pairs of networks were identical. With post hoc comparisons, we identified the number of edges that significantly differed between each pair of networks. We tested the extent to which the similarity of the global strength (sum of all edge weights within each network) differed across the networks. Finally, we estimated a network across all four samples with the data from only those participants who fulfilled the criteria for PTSD or CPTSD as per ITQ algorithm (n = 512), and compared the results to a network of those with significant functional impairment but without a diagnosis (n = 1079) to investigate possible differences between these groups (see supplementary material, Data analysis: Network comparison for more details).
Results
Descriptive statistics
Participants from the four samples reported different profiles of symptom distress (Table 1). The similarity of the symptom profiles varied, ranging from rather similar to unrelated to quite dissimilar: The Spearman rank correlation between the mean values of the 12 items ranged from ρ = 0.71 (German and Israeli sample) to ρ = 0.06 (Israeli and UK sample) to ρ = −0.34 (German and UK sample). The mean symptom profile correlation was ρ = 0.31.
Network estimation
Figure 1 depicts the results of the four jointly estimated networks. In the German, Israeli, UK and USA sample, 43, 46, 45 and 48 of all possible 66 edges were estimated to be above zero (65.2%, 69.7%, 68.2%, and 72.7%, respectively), indicating that the symptoms had substantial connections with each other. The visual inspection of the four networks shows many consistent edges, such as strong connections between dream-flshb, hyper-strtl, avdin-avdex, fail-worth and dist-close (see Table 1 for full symptom names).
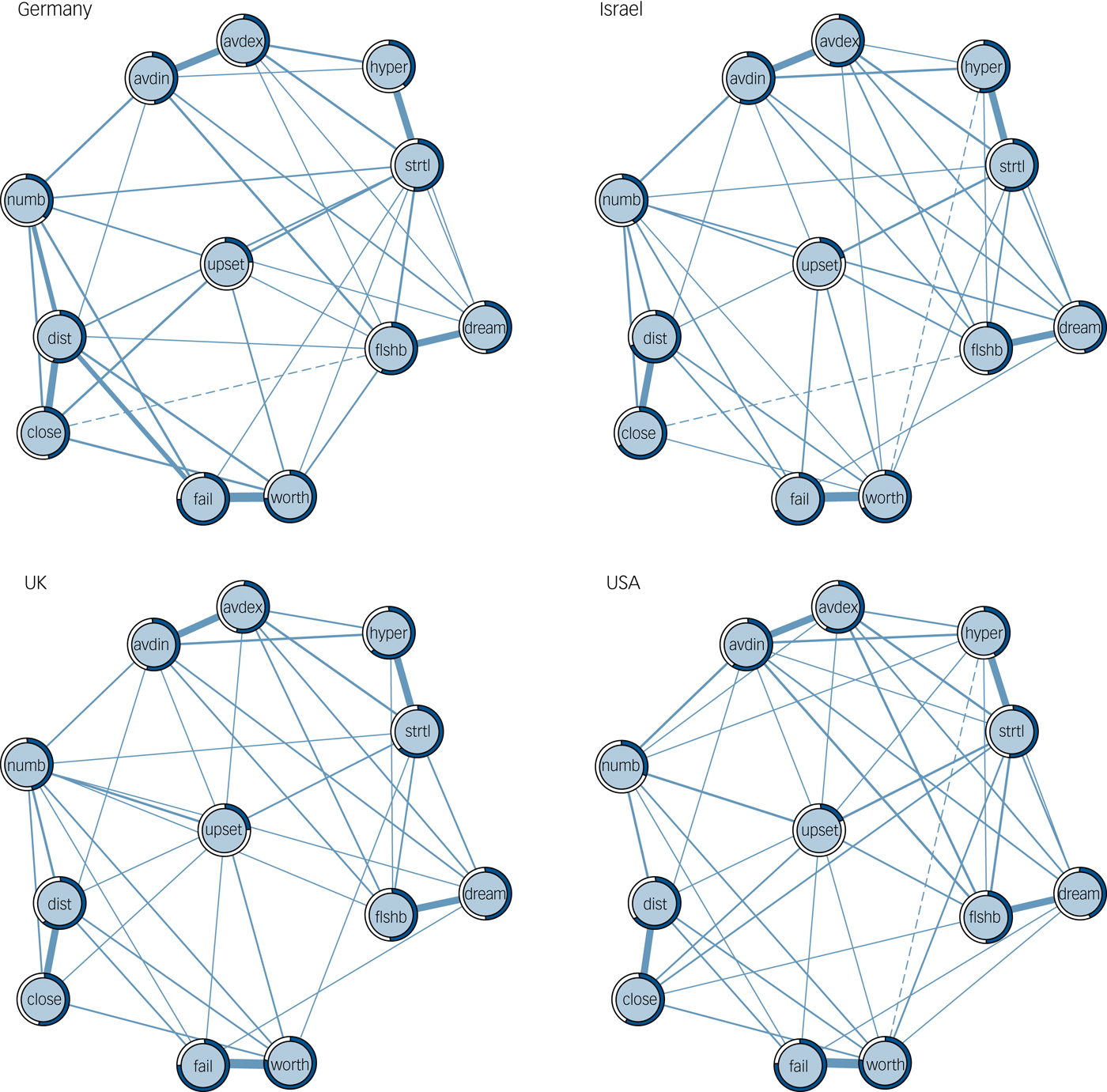
Fig. 1 Regularized partial correlation networks across the four samples. Edge thickness represents the degree of association, solid edges indicate positive relations and dashed edges indicate negative relationships. The grey area in the rings around the nodes depicts predictability (the variance of a given node explained by all its neighbours).
avdex, external avoidance; avdin, internal avoidance; close, difficulties feeling close to others; dist, feeling distant or cut off from others; dream, distressing dreams; fail, feelings of failure; flshb, intrusive recollections/flashbacks; hyper, hypervigilance; numb, emotional numbing; strtl, exaggerated startle response; upset, long-time upset; worth, feelings of worthlessness.
Network inference
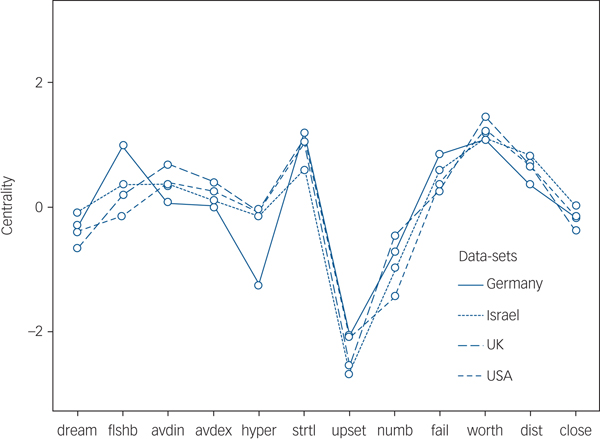
The standardised strength centrality estimates are presented in Fig. 2. These estimates were very similar across the four networks with Spearman correlations ranging from ρ = 0.80 (German and UK sample) to ρ = 0.99 (UK and USA sample). Worth and avdex were among the nodes with the highest strength metric in all samples and upset was the node with the smallest centrality value in all networks. The average predictability of the nodes is graphically presented in Fig. 1 and ranged from 0.51 (German sample) to 0.56 (UK sample), with a total mean of 0.53. This indicates that, on average, 51–56% of the variation of each symptom could be explained by its neighbouring symptoms. Strength and predictability were closely related (correlations from ρ = 0.78 to ρ = 0.86), reflecting their conceptual similarity. The two nodes with the highest bridge strength were strtl and upset, which means that strtl was the PTSD symptom with the strongest average connection to DSO symptoms and upset was the DSO symptom with the strongest average connection to PTSD symptoms.
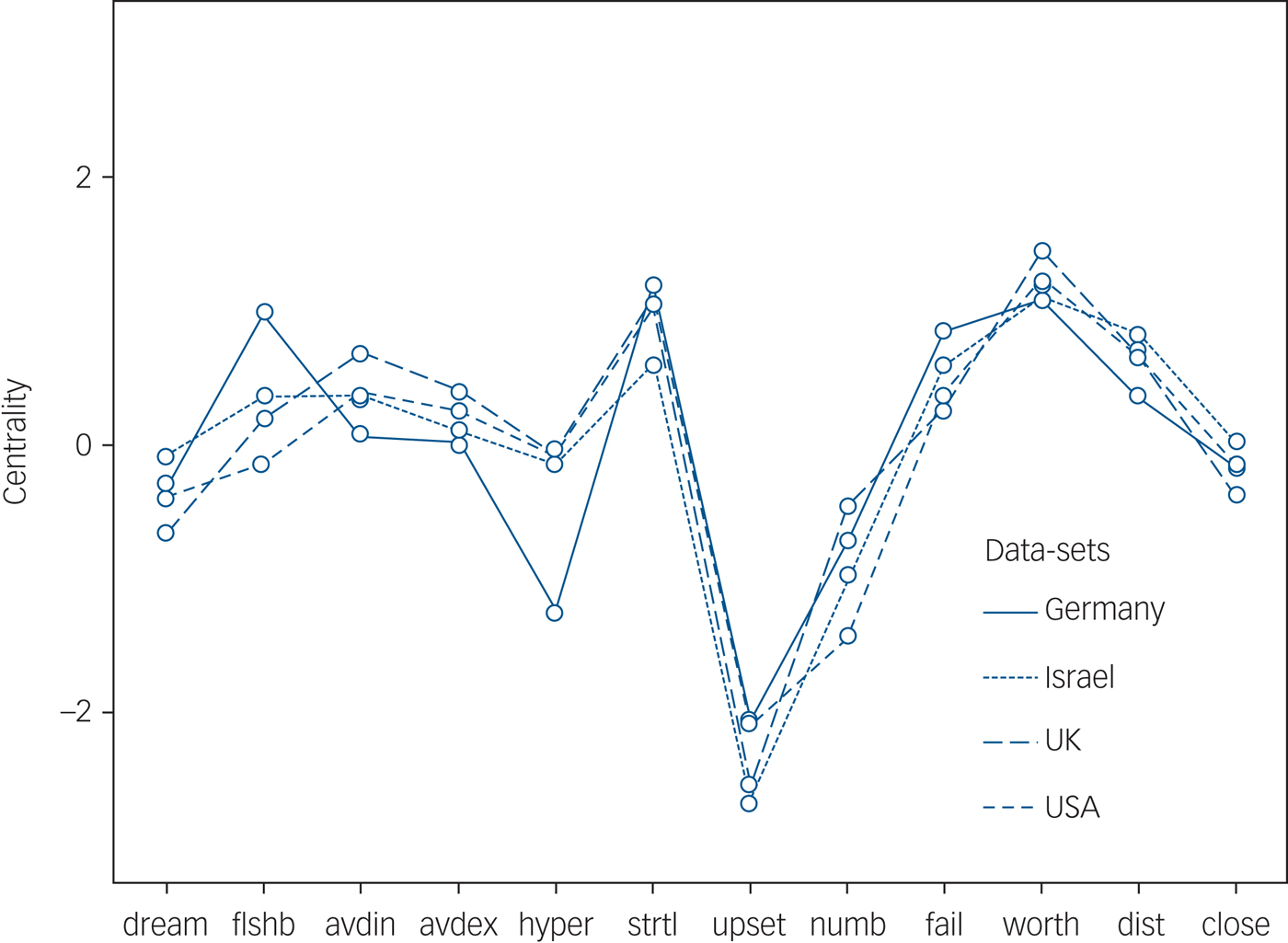
Fig. 2 Standardised node strength centrality of the 12 CPTSD symptoms across the four samples. See Table 1 for full symptom names.
avdex, external avoidance; avdin, internal avoidance; close, difficulties feeling close to others; dist, feeling distant or cut off from others; dream, distressing dreams; fail, feelings of failure; flshb, intrusive recollections/flashbacks; hyper, hypervigilance; numb, emotional numbing; strtl, exaggerated startle response; upset, long-time upset; worth, feelings of worthlessness.
Network stability
Overall, the stability analyses provided support for the robustness and moderate accuracy of our results based on the correlation-stability coefficient and the bootstrapped confidence intervals around the estimated edges. The confidence intervals around the edge weights were moderately large, indicating a moderate accuracy of the network estimation. Small edges should be interpreted cautiously (see supplementary material, Results: Network stability and Fig. 1 for more details).
Network comparison
Spearman correlations of the edge weights between the samples ranged from 0.78 (German and USA sample) to 0.86 (Israeli and UK sample), indicating strong similarities. The network comparison test is an overall test of network similarity. We compared all six pairs of networks and found that three of these comparisons showed significant differences: between the German and Israeli (P = 0.028), the German and the USA (P = 0.007) and the UK and the USA (P = 0.001) networks. The three other comparisons did not detect any difference between the edge weights across the networks (i.e. the German and UK, Israeli and UK, and Israeli and USA networks). We then used a post hoc test comparing all edges between the networks and found only one significantly differing edge in the comparison of the German and USA networks (the edge connecting upset-numb), between the Israeli and USA networks (fail-dist) and between the UK and USA networks (hyper-strtl). The global strength of the networks, which is a measure of the overall connectivity within a network, was 5.18 for the German, 5.32 for the Israeli, 5.31 for the UK and 5.18 for the USA network. The network comparison test showed no significant difference for the comparison of the overall connectivity between any two networks. Collectively, these results suggest a strong similarity between the networks.
Next, we estimated a network for the total sample of 1591 persons (Fig. 3a), which was similar to the structures of the four jointly estimated networks. Worth had the highest strength, followed by strtl, and dist. The least central symptom in this network was upset (Fig. 3c). Finally, we compared the network of those individuals who fulfilled the criteria for PTSD or CPTSD to the network of those who did not. The overall network comparison test revealed a significant result. Post hoc analysis showed significant differences in three edges: dream-flshb, avdin-avdex and hyper-strtl, with larger edges in the group without diagnosis (Fig. 3b). The Spearman correlation of the edge weights between the two groups was 0.62. The global strength of the networks was not significantly different (4.97 for the group with a diagnosis and 5.14 for the group without a diagnosis). The centrality estimates were similar between the groups (Fig. 3c).
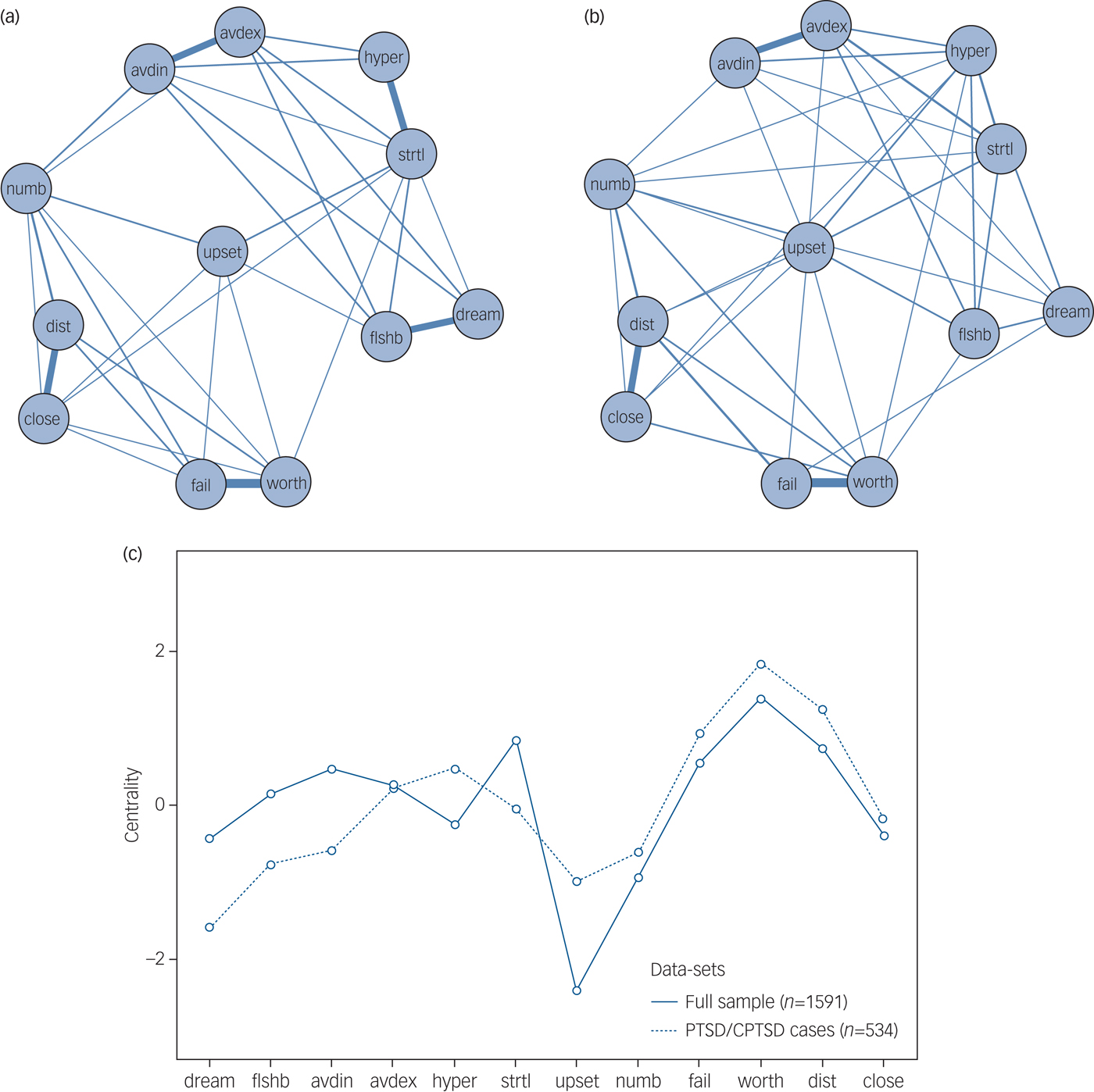
Fig. 3 Network analysis in the combined data-set. (a) Cross-sample network (n = 1591) depicts the average of the four individual networks. (b) Cross-sample network of the subgroup who meet diagnostic criteria for PTSD or CPTSD (n = 512). (c) Standardised node strength centrality for the cross-sample networks. See Table 1 for full symptom names.
avdex, external avoidance; avdin, internal avoidance; close, difficulties feeling close to others; dist, feeling distant or cut off from others; dream, distressing dreams; fail, feelings of failure; flshb, intrusive recollections/flashbacks; hyper, hypervigilance; numb, emotional numbing; strtl, exaggerated startle response; upset, long-time upset; worth, feelings of worthlessness.
Discussion
In this study, we investigated the network structure of ICD-11 CPTSD with the newly developed ITQ in four national representative samples from Germany, Israel, the UK and the USA. The samples varied in their cultural background, demographic characteristics, trauma experiences and symptom severity. Overall, we found that the symptoms comprising a cluster according to the ICD-11 classification were strongly associated with each other in all networks, except for the two symptoms assessing affective dysregulation. The estimated networks were sufficiently stable and ‘feelings of worthlessness’ and ‘exaggerated startle response’ were consistently among the most central symptoms. The latter also showed the strongest connections among the PTSD symptoms with DSO and ‘long-time upset’ showed the strongest connections among the DSO symptoms with PTSD. The networks showed strong similarity across the four samples and across the subsamples with and without a probable PTSD/CPTSD diagnosis.
Previous research also found that negative trauma-related cognitions such as ‘worthlessness’ play a central role in the network structure of ICD-11 CPTSDReference Knefel, Tran and Lueger-Schuster5 and DSM-5 PTSD,Reference von Stockert, Fried, Armour and Pietrzak6 and are predictive of non-remittance.Reference Galatzer-Levy, Karstoft, Statnikov and Shalev25 Negative self-appraisals can be considered as vulnerability to develop PTSD after traumatic experiencesReference Bryant and Guthrie26 and as a maintaining cognitive factor.Reference Dunmore, Clark and Ehlers27 Our results confirm the central role of a negative self-concept in the symptom network of CPTSD. Another core feature of PTSD is ongoing sense of threat,Reference Maercker, Brewin, Bryant, Cloitre, van Ommeren and Jones1 which is reflected by the central role of ‘exaggerated startle response’ in the symptom networks. PTSD has fear or horror at its heart, based on the patient's challenges to separate the ‘here and now’ from the ‘there and then’.Reference Brewin28 Finally, challenges to calm down after being upset showed the strongest connection from DSO to PTSD, supporting the potential value of incorporating adaptive emotion regulation strategies into treatment.Reference Cloitre, Koenen, Cohen and Han29 A number of interventions have been found effective in addressing similar symptoms.Reference Foa30, Reference Ehlers, Clark, Hackmann, McManus and Fennell31 Taken together, our results suggest the potential value of cognitive, exposure-based and emotion regulation interventions in the treatment of CPTSD.Reference Schnyder, Ehlers, Elbert, Foa, Gersons and Resick32
Our results provide evidence of the robustness of CPTSD. The network of those individuals who had a probable PTSD/CPTSD diagnosis was very similar to the network of those who showed functional impairment by PTSD/CPTSD symptoms, but did not fulfil all criteria. Only three edges differed between these groups, with stronger connections in the group without probable diagnosis. The symptoms seem to be weaker connected in those with a diagnosis, suggesting that PTSD and CPTSD represent more stable conditions with fewer plasticity compared with subthreshold conditions. However, these findings require further replication. Furthermore, each symptom was closely associated with the other symptom of their respective symptom cluster. This is similar to factor-analytical studies, where symptoms within a factor are strongly related to each other.Reference Hyland, Shevlin, Brewin, Cloitre, Downes and Jumbe33 Network models and factor models are mathematically similar.Reference Kruis and Maris34 However, although factor models assume the presence of underlying latent factors, the network model emphasises the mutual interaction between symptoms. Only the affective dysregulation symptoms did not show a strong association with each other in any of the networks. This is understood as consistent with the goals of the measure's development: these symptoms cover two types of problems in the regulation of affects, hyperactivation and hypoactivation, reflecting both under- and over-regulation of affect. It is likely that a specific person does present with either one feature or the other, not both, which can explain the small correlation between these symptoms. The closer association of the symptoms reflecting the other clusters can be explained by the conceptual similarity of the symptoms or by a direct causal interaction of these symptoms. For example, the two symptoms of re-experiencing might covary strongly because both reflect the involvement of an involuntary perceptual memory system that is distinct from ordinary episodic memory on a psychological levelReference Brewin28 or reflect specific alterations in the neural basis related to memory on a neurological level.Reference Whalley, Kroes, Huntley, Rugg, Davis and Brewin35 It is also possible that the experience of repeated flashbacks during the day directly influences the experience of nightmares during the night, and vice versa, on symptom level. The most central symptoms provide a good starting point for symptom-specific interventions.Reference McNally, Robinaugh, Wu, Wang, Deserno and Borsboom36 The networks in this study are cross-sectional and it is thus also possible that central symptoms are a consequence rather than the cause of other symptoms in the network.Reference Bos, Snippe, de Vos, Hartmann, Simons and van der Krieke37 Future research should investigate the association of cross-sectional (between-person) networks with longitudinal (within-person) networks. Treatment studies should explore the treatment response rapidity by addressing central nodes with specific interventions.
Our findings add support to the questioned replicability of network analytical studies. Although the samples showed differences in symptom profiles and participant characteristics that might reflect cultural differences, we found very similar networks across the samples.Reference von Stockert, Fried, Armour and Pietrzak6–Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk and Bockting8 Nevertheless, this work is limited in a number of ways. First, the ITQ is a self-report measure. Second, the samples differed in some respects: the assessment procedure was not the same in all studies (online versus paper-pencil) and the response rates differed between the four original studies (Germany: 52% of all valid addresses who were contacted; Israel: 31% of those who were sent an email invitation; UK: 39.6% of the participants who were screened for inclusion; USA: 46.3% of the participants who were screened for inclusion), possibly biasing between-group comparisons. Third, the study findings in community samples may not generalise to treatment-seeking clinical samples. Although some of the participants in this study may be accessing treatment, from our data it was not possible to differentiate their symptom networks from those who do not access treatment. Fourth, the accuracy of the individual networks was limited based on the smaller sample sizes. Fifth, the cross-sectional nature of the samples does not allow for any causal inference. Finally, although samples came from three different continents, all represent high-income countries. It is not clear whether our results would generalise to samples from low- and middle-income countries.
In conclusion, this study supports the generalisability and construct validity of ICD-11 CPTSD. Future research should investigate the network structure of CPTSD in diverse populations who are also culturally and socioeconomically diverse.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2018.286.
Funding
An internal research grant was awarded to M.B.-E. from Ariel University (grant no. RA1700000037). The sponsor had no involvement in study design, data collection, analysis, interpretation of the results, writing of the report or the decision to submit the article for publication.






eLetters
No eLetters have been published for this article.