Introduction
The type of chemotherapy used to relieve symptoms and/or control cancer without curing is known as palliative chemotherapy; however, palliative chemotherapy is often perceived by patients as a curative treatment (George et al. Reference George, Prigerson and Epstein2020b). When this misconception occurs, some studies suggest that patients may rely on their palliative chemotherapy treatment as a way to sustain more optimistic expectations regarding their disease and mortality (Buiting et al. Reference Buiting, Terpstra and Dalhuisen2013; Grunfeld et al. Reference Grunfeld, Maher and Browne2006). Few studies demonstrate anything more than modest, ephemeral enhancements in quality of life brought on by chemotherapy, which primarily reflect transient tumor shrinking (Wise Reference Wise2016).
The tendency of increasing the use of chemotherapy at the end of life has been described as an escalation of aggression in cancer treatment, which at the same time has indicated a worse quality of patient care (Buiting et al. Reference Buiting, Rurup and Wijsbek2011). Despite this, studies have been demonstrating that several patients fail to understand their prognosis, let alone the true benefits of available treatment options (Bernacki et al. Reference Bernacki and Block2014; George et al. Reference George, Matsoukas and McFarland2022; Lindhardt et al. Reference Lindhardt, Winther and Pfeiffer2021).
Several irregularities and conflicting interests – in the pharmaceutical industry, in government approval, and in the clinical use of cancer medication – ethically impact the care and costs of cancer patients (Wise Reference Wise2016). Nonrepresentative clinical trials with inaccurate outcomes and misinformed patients with unrealistic expectations can lead to interventions that are not in their best interest most of the time (Wise Reference Wise2016). Spending a 6-figure sum to extend life by a few weeks or months is already unaffordable and inadequate for many of the 20% of the (Western) population who will almost inevitably die from solid tumor metastasis (Wise Reference Wise2016).
By failing to understand how treatment may affect their lives, hoping for a cure or long survival, patients insist on treatments that, if at one time had some purpose, no longer do, and postpone conversations about the end of life while it is getting closer by the day (Bernacki et al. Reference Bernacki and Block2014). In a study that was conducted with the objective of understanding what Brazilian patients with advanced cancer know of their prognosis, the researchers concluded that the perceptions of patients and their oncologists regarding the goals of the treatment and their chances of cure were at odds (Paiva et al. Reference Paiva, Teixeira and Minto Lourenço2022). A clear and trustful discussion with patients and their families is important before making the decision to start palliative chemotherapy (Ekström et al. Reference Ekström, Brun and Eberhard2021). This is essential to avoid chemotherapy being provided near the end of life, distorting the focus of end-of-life (EoL) care (Ekström et al. Reference Ekström, Brun and Eberhard2021), since chemotherapy during the last 30 days of life is considered futile, with a risk of compromising quality of life near death (Näppä et al. Reference Näppä, Lindqvist and Rasmussen2011; Wright et al. Reference Wright, Zhang and Keating2014).
In a study that evaluated the quality of EoL care in 81 countries, in general, developed countries ranked first, as opposed to developing countries (Finkelstein et al. Reference Finkelstein, Bhadelia and Goh2022). According to this study, Germany ranked 15th, while Brazil ranked 79th. The absence of a national strategy for palliative care and limited or no integration of palliative care into the health-care system can be highlighted as some of the factors that contribute negatively to the quality of EoL care (Finkelstein et al. Reference Finkelstein, Bhadelia and Goh2022). In the Global Atlas of Palliative Care, developed by the World Health Organization in partnership with the Worldwide Hospice Palliative Care Alliance (World Health Organization (WHO), Worldwide Hospice Palliative Care Alliance (WHPCA) 2020), Germany is one of the countries with advanced health system integration – palliative care at an advanced stage of integration (Level 4b), the highest ranking referring to the quality of palliative care. Brazil was classified as a country with generalized provision of palliative care (Level 3b), that is, that still needs to make progress in various issues for the improvement of this care approach. Palliative care is still in its infancy in Brazil, but recent developments offer hope for its expansion (da Silva et al. Reference da Silva, Büscher and Moreira2017).
A study conducted in 7 European countries – including Germany – with the objective of providing a structured overview of legislation, existing regulations, and the different health-care policies regarding palliative care, indicated that all of these countries have national laws, statutes, or policies regarding palliative care, representing an important step toward improving this area of care (Van Beek et al. Reference Van Beek, Woitha and Ahmed2013). Germany was the first of the countries evaluated to have a specific palliative care law, combining prerequisites such as professional qualification, multidisciplinary teams, and organization and participation of volunteers to encourage home care (Van Beek et al. Reference Van Beek, Woitha and Ahmed2013). In the case of Brazil, only recently, in the year 2018, national guidelines were published for the organization of palliative care within the Unified Health System (Sistema Único de Sáude – SUS) (Brasil. Ministério da Saúde 2018).
Considering that, among patients with advanced life-limiting diseases, an inaccurate understanding of prognosis is common and is associated with negative outcomes (e.g., increased choice of disproportionate and minimally beneficial treatments in the last week of life) (George et al. Reference George, Matsoukas and McFarland2022) and the socioeconomic, cultural, and health system differences in Brazil and Germany, this study aimed to explore the expectations of Brazilian and German patients regarding metastatic cancer and palliative chemotherapy. This objective was guided by the following question: What are the expectations of metastatic cancer patients regarding palliative chemotherapy?
Methods
Design
This multicenter study was developed using the qualitative phenomenological method, with semi-structured, in-depth interviews, with open-ended questions. This study was reported according to the Consolidated Criteria for Reporting Qualitative Studies, when applicable (Tong et al. Reference Tong, Sainsbury and Craig2007).
Setting
This study was conducted in Brazil and Germany (where the first author of this study completed her interchange Ph.D. course). In Brazil, data were collected from cancer patients hospitalized and/or undergoing outpatient treatment at the Hospital das Clínicas of the Federal University of Minas Gerais and at the Felício Rocho Hospital, both large general hospitals, providing care to the population mostly through the Brazilian Unified Health System (SUS), located in the city of Belo Horizonte – MG. In Germany, data were collected at the Albertinen-Krankenhaus Hospital, a large hospital located in the city of Hamburg. In addition, some patients who were under palliative care at home were visited by the researcher in their homes, under the supervision of a palliative care physician from the Albertinen-Krankenhaus Hospital.
All Brazilian participants received care from the public health system. The German participants had private health insurance.
Participants
Sampling and approach method
The selection of the study sample was based on convenience (Moser and Korstjens Reference Moser and Korstjens2018), considering patients who agreed to participate in the study during the time allotted in the research project schedule for data collection in both countries (the researcher’s intention was to interview as many patients as possible during the time allocated for data collection). Regarding the sample size, a minimum of 10 interviews was chosen, based on the literature for the interpretive phenomenological study (Moser and Korstjens Reference Moser and Korstjens2018).
Patients were approached according to the specificities of each place where data were collected, mostly before or after medical appointments or chemotherapy. It is worth noting that none of the patients approached, either in Brazil or in Germany, refused to participate in the study.
Eligibility criteria
Adults with metastatic cancer on palliative chemotherapy, with a clinical condition that would allow the interviews to be conducted – performance status less than or equal to 3 according to the ECOG Performance Status Scale (Oken et al. Reference Oken, Creech and Tormey1982), regardless of sex and level of education, were eligible. This information regarding the patients’ clinical conditions was obtained from the physicians and nurses responsible for patient care.
Data collection
Data collection was performed by one of the researchers (C.P.A.). A procedural test was performed initially, with data collection from one patient, both in Brazil and Germany. In Germany, the researcher conducted the interviews in German (each patient was asked if the researcher’s communication was well understood, with affirmative responses in all cases). The researcher had been living in Germany for a year prior to the research, which allowed her to complement her German language studies as a second language. In addition, the preparation for the interviews was carried out with the assistance of a native German-speaking teacher in order to further improve her language skills. In Brazil, the researcher conducted the interviews in Brazilian Portuguese.
After providing written consent, the interview was conducted at a place of the patient’s preference, usually at the hospital where they were being treated. In some cases, patients preferred to be accompanied by a family member and/or a professional carer during the interview.
The interviews were conducted using a semi-structured questionnaire that addressed the following open questions: “What is the disease prognosis provided by your doctor?” “Were the diagnosis and treatment explained to you in detail by your doctors?” “What are your expectations regarding disease progression and the treatments/care provided?” “Do you spend most of your time at home or in the hospital?” “Would you be willing to try experimental treatments with no guarantee of success and that could worsen your situation?” and “What do you consider more important? Living potentially longer on chemotherapy, or living in care focused on ending pain and having a better quality of life, regardless of time?” The sociodemographic data were collected using an instrument developed by the authors.
The interviews lasted for approximately 40 minutes (some lasted up to 2 hours). There was no need for more than one meeting with each patient for data collection. A variety of data collection techniques were used, considering that using more than one method can improve data integrity, improving the results (Casey and Murphy Reference Casey and Murphy2009). The data collection techniques adopted were face-to-face in-depth interviews (aiming to explore participants’ experiences, perceptions, thoughts, and feelings), as well as participant observation and field diary notes (Moser and Korstjens Reference Moser and Korstjens2018). During the interviews, the researcher took notes of the central points mentioned by the participants (those related to the study’s objective). Immediately after the end of the interview, the researcher recorded an audio log on a smartphone reproducing the main parts of the interview (to prevent important data from being lost). These recordings were made based on what had been noted in the field diary, and during the recordings, the researcher aimed to synthesize the content of these notes with the greatest level of detail possible, including the reproduction of patients’ lines during the interview. It is worth noting that the researcher made it clear in her recordings what was a reproduction of the participants’ speech and what was an impression of hers. Later these audio logs were transcribed and analyzed, along with the field diary notes (Moser and Korstjens Reference Moser and Korstjens2018).
Data analysis
In phenomenology, the analysis aims to describe and interpret the meaning of an experience, often identifying essential main and subordinate themes, so that the result of a phenomenological study is a detailed description of themes that capture the essential meaning of a lived experience (Moser and Korstjens Reference Moser and Korstjens2018). Thus, for the data analysis, the 6 stages of thematic analysis proposed by Braun and Clarke were fulfilled (Braun and Clarke Reference Braun and Clarke2019). Data analysis and collection occurred simultaneously, so that each interview was analyzed according to inductive thematic analysis based on the manual transcription and data familiarization (Braun and Clarke Reference Braun and Clarke2019). Subsequently, their coding and recoding were carried out, in addition to the elaboration of representative themes for the participants’ universe (Clarke et al. Reference Clarke, Braun, Hayfield and Smith2015). Thus, for the data analysis, the 6 stages of the thematic analysis were fulfilled, namely: (1) data familiarization: transcription of the interviews, reading, and rereading of the data were carried out. The researchers also made notes of ideas regarding what the data had suggested; (2) generation of initial codes: the search for words and phrases related to the research questions was carried out, identifying the codes – at this stage, comparisons were made to identify themes that recurred throughout the interviews; (3) elaboration of themes: the codes were organized according to their similarity; (4) review of themes: rereading the themes and the data collected to analyze the internal homogeneity of the theme and heterogeneity between the themes; (5) defining and naming the themes: assigning a title to express the content of the interpretation; (6) producing the report: writing the article and articulating speeches that represented the themes.
Results
Participant characterization
A total of 48 patients participated in the study, of which 28 (58%) were Brazilian and 20 (42%) were German. Of the total number of participants, 17 (35%) were men and 31 (65%) were women. The participants’ mean age was 41 (minimum age = 22 and maximum age = 86). Regarding the level of education, all German participants had higher education, while among Brazilians, the prevalent level of education was complete primary/middle school. All participants had metastatic cancer. The types of cancer were breast, prostate, bowel, pancreas, and bladder cancer. At the time of data collection, the only treatment the study patients were receiving was palliative chemotherapy. In Brazil, all patients were receiving treatment through the SUS. In Germany, all patients had health insurance. In Germany, the patients were middle/upper class; in Brazil, middle/lower class.
The expectations of metastatic cancer patients regarding palliative chemotherapy
The general idea captured from the interviewees’ speech was that their diseases were curable or “while there is chemotherapy, there is life”; thus, the data analysis enabled the elaboration of the central theme, entitled “Mistaken expectations of metastatic cancer patients regarding palliative chemotherapy: While there is chemotherapy, there is life,” with 5 subthemes, namely: (1) communication and expectations; (2) normal life; (3) the person behind the disease; (4) religiosity and spirituality; and (5) the fortitude to choose between continuing or discontinuing treatment. The following 5 themes were semantic themes that were isolated from the data’s apparent meaning and did not go beyond what participants directly indicated (Table 1).
Table 1. Theme and subthemes
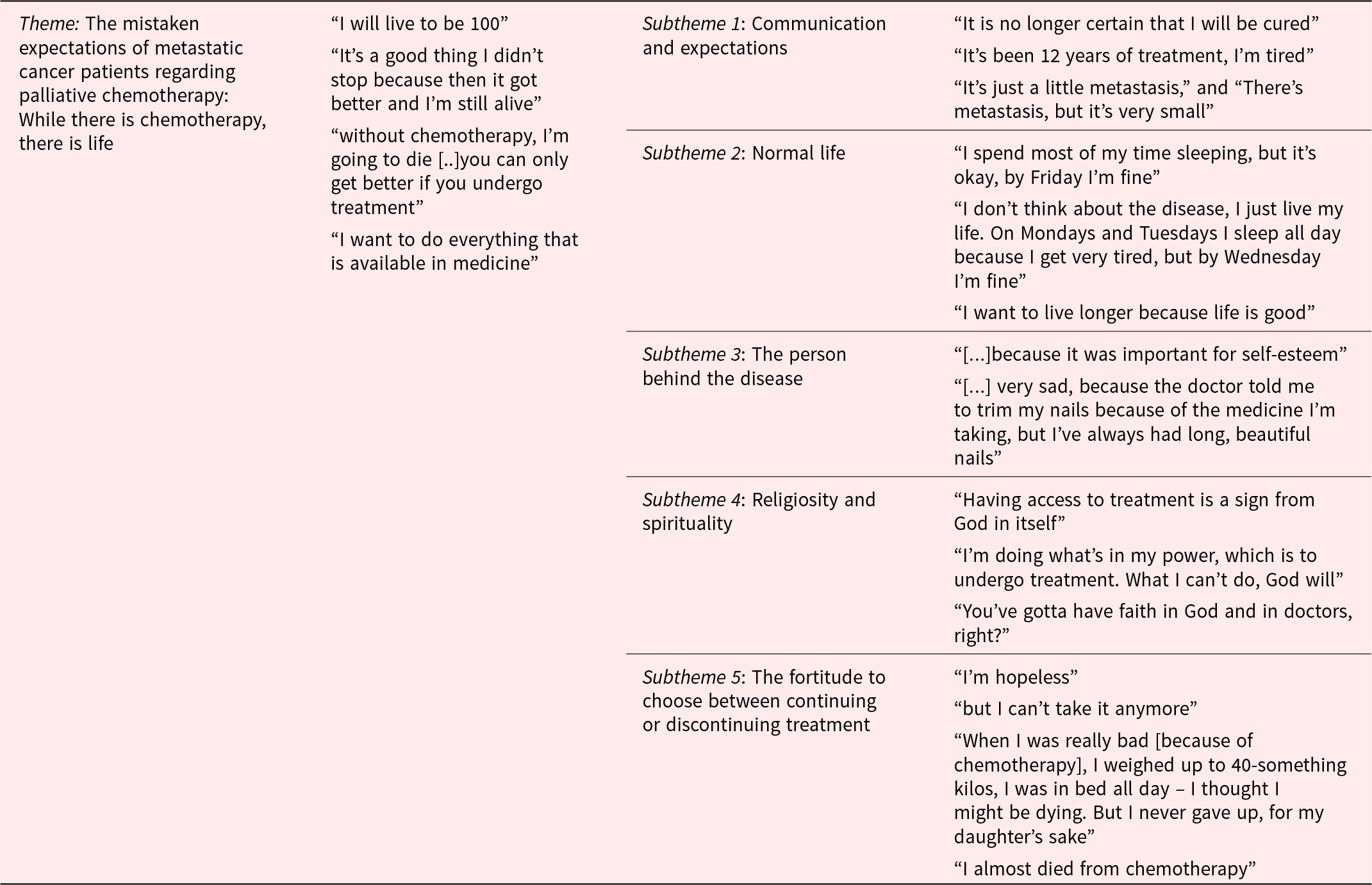
Theme: Mistaken expectations of metastatic cancer patients regarding palliative chemotherapy: While there is chemotherapy, there is life
The report of a 58-year-old Brazilian patient illustrated well the study’s central theme. She said that she had been undergoing treatment for 12 years and that as long as she stayed on chemotherapy, she would live as long as she had to as if she was free of the disease: “I will live to be 100.” Another patient, in her 30s, said that she became seriously ill because of chemotherapy and that she only did not give up because of her daughter, but that “It’s a good thing I didn’t stop because then it got better and I’m still alive.” This idea was recurrent in several interviews.
A German patient, at the very start of the conversation, reported being upset that he was “on the third line of treatment, which is the last one.” When asked whether the line was the last because of treatment limitations per se or because his plan did not cover others, he became thoughtful and asked for the question to be directed to the doctor because he “for sure wants to do the next one if there is one” (later the doctor confirmed that this was a treatment limitation). An 87-year-old German patient came crying into the room where the interview was going to be carried out and said that her wound prevented her from undergoing further chemotherapy cycles and that “without chemotherapy, I’m going to die.” She stated that every person has hope, but that “there is only a chance to get better if you do the treatment.” When her doctor knocked on the door, she asked him to confirm that “everything that is possible is being done” because she “wants to do everything that is available in medicine.”
Subtheme 1: Communication and expectations
This subtheme portrays how communication is essential to patients’ understanding (correct or mistaken) of the treatment’s objective. Most patients interviewed expressed clearly mistaken expectations regarding the potential of palliative chemotherapy on the disease. Despite this, almost all patients responded that they had been informed in detail about the disease and the treatment. One patient, who was in his early twenties, a university student, and well aware of his illness, defined palliative treatment as follows: “It is no longer certain that I will be cured,” a conclusion the patient came to because of a statement by his doctor that studies showed a “19% chance of response.” In other words, this patient understood that he had a 19% chance of being cured. Misconceptions about percentages, the meaning of “response” to treatment, remission, and test results were frequent. A young patient, who seemed extremely optimistic, said: “The results are surprising the doctors.” The same patient said: “The doctors explained everything clearly, and yes, I’m quite curious.” A German patient said he was very happy, “because the first drug reduced the tumor” (this patient was on the third line of antineoplastic chemotherapy). When asked if the tumor reduction made a difference in his health status, he became thoughtful and said “no.” Another patient with metastatic breast cancer said, “It’s been 12 years of treatment, I’m tired,” with a clear expectation that at some point the treatment would be stopped and she would continue living without the disease. Other patients, especially women with breast cancer, made it clear that, although they recognized incurability, they believed they could live with longevity, regardless of the disease, as long as they stayed in treatment.
Apparently, the patients failed to understand the natural evolution of the disease, which led them to believe in a situation entirely manageable with chemotherapy. One of the patients stated: “It’s been 13 years like this, I’ve gotten used to it.” An important source of misunderstanding seemed to concern the patients’ understanding of what metastatic cancer really represents. Patients tended to focus on the size of the tumors as if this was more relevant than the existence of metastases. Some patients stated phrases such as: “It’s just a little metastasis,” and “There’s metastasis, but it’s very small.”
This is one way to determine how mistaken the patients’ understanding of their prognosis was from their future plans. A German patient with pancreatic cancer demonstrated a clear understanding of how serious his situation was, especially given the type of tumor. He said in April that he hoped “to make it to Christmas.” Then, he said: “Christmas is far away, I want to see my next granddaughter being born” (which would happen in about a month). Another patient, a Brazilian, stated: “I will be 80 years old next year… If I’m alive,” and cried. A college student patient, with a grim prognosis and on an experimental chemotherapy drug explained what he intended to do after he graduated.
When expectations regarding the treatment were unclear, they were asked what the doctor had said about the duration or quantity of chemotherapy. Some patients answered that they did not know. Others said, “These things are better left unknown, I prefer not to know” or “I don’t ask many questions either.” A patient with intestinal cancer emphasized that “it was supposed to be over, but he had to be hospitalized and delayed the last one.” The events that prevented the continuity of chemotherapy, even when they resulted in long hospital stays, great pain, and weakness, were generally seen as complications that were part of a curative treatment and not as the natural course of an incurable disease. Some patients claimed that they had “finished the treatment” and were “just undergoing management.” One of them even stated: “I am even cured already.” The patients’ misunderstanding of the real expectations was such that at least 2 German patients reported that there were people with incurable diseases in Germany, but that if they went to the United States for treatment, they could be cured.
Subtheme 2: Normal life
This subtheme indicates that despite living with a serious and advanced disease, patients seek ways to lead a “normal life” as far as possible. Although many patients claimed to lead a normal life, at the same time, they reported spending most of their time sleeping. Although they said that they did not live for chemotherapy, their description of their activities demonstrated the opposite: “I spend most of my time sleeping, but it’s okay, by Friday I’m fine” (account of a patient who underwent chemotherapy 2 Mondays out of every 3). “I don’t think about the disease, I just live my life. On Mondays and Tuesdays I sleep all day because I get very tired, but by Wednesday I’m fine” (on Friday this patient spent the whole day in the hospital undergoing chemotherapy).
Of all the patients, only 2 women said they were still working – one had just learned of her diagnosis and the other said she had reduced the pace of her work as a hairdresser in her own place. A German patient said, “I want to live longer because life is good.” She said a few times, crying, that her cancer “is incurable, unfortunately.” She said that her expectation about the treatment was one of hope (she looked at the researcher and said: “hope, right?”). She also said that she had hard feelings toward the first doctor who diagnosed her and told her she was going to die.
Subtheme 3: The person behind the disease
In this subtheme, it was found several times that the disease occupies a prominent place in the life of patients and their families; however, the person beyond the disease is still there, with their preferences and desires. In several conversations, patients reported greater discomfort over issues that were not related to the disease or treatment. At least 3 patients with breast cancer highlighted the discomfort due to the prosthesis placement more than the disease. They reported having been pressured to undergo the procedure “because it was important for self-esteem,” but said they had never had the desire to undergo reconstruction surgery. These patients externalized significant psychological suffering from the surgery, as well as pain and postoperative complications. One of the patients said that after 5 years of reconstructive surgery: “I don’t like having something inside me that is not mine.” A German patient said that no one had asked her whether she wanted to undergo a mastectomy, and she is unsure whether she would have agreed if she had been asked. This same patient said that the mastectomy was quite traumatic, especially due to her husband’s difficult reaction.
The main complaint of a 79-year-old patient was that she was “very sad, because the doctor told me to trim my nails because of the medicine I’m taking, but I’ve always had long, beautiful nails.” Another patient said that she had been using a medication before “that wasn’t working at all.” Asked if the new one was any better, she replied “it’s all rubbish.” Much of the conversation with this patient focused on her discomfort at having been hospitalized for more than 20 days, being forced to eat meals with food she could not stand (other patients made the same complaint). The patient claimed that she had even stopped eating – she would only eat when a friend brought her something. In the end, she said that the doctor discharged her because “she needed to eat.” A severely debilitated patient, who was receiving chemotherapy in bed, reported that she had to undergo an exam in October and that this was making her very anxious: “I think about it all the time, I cry, I get even aggressive. […] I’m from the countryside, you know… but I wanted to help my doctor.” A German patient complained that her daughter tried to get her driver’s license and said that she was a good driver. She said that she suffered a lot because of the lack of reconciliation with her daughters and that she thought daily “about what have I done wrong?.”
A patient, in particular, said that the system itself focuses more on the disease than on the person. His main concerns were about his mortgage and paying his bills, as he could no longer work. This same patient even mentioned that it might be more important for him to have the electricity bill waived, for instance, than having access to a high-cost medication.
Subtheme 4: Religiosity and spirituality
In this subtheme, it was identified how religiosity and spirituality are some of the coping strategies used by patients to deal with the disease. Most patients mentioned the importance of spirituality and/or religiosity in coping with the disease. It was noted, however, that faith was often understood as providing access to treatment or to doctors who could invariably cure the disease. The following phrases were frequent: “Having access to treatment is a sign from God in itself,” “I am quite fortunate to be able to undergo the treatment,” “I’m doing what’s in my power, which is to undergo treatment. What I can’t do, God will,” “You’ve gotta have faith in God and in doctors, right?” and “First it’s God, and then it’s the doctors who have to believe.” Regarding the search for meaning and sense in the experience of the disease, a patient said that everyone affected with this disease asks themselves “why me?.” It is worth noting that in Brazil, talking about God was frequent among the interviewees, unlike the German patients, who did not refer at any time to any superior being.
Subtheme 5: The fortitude to choose between continuing or discontinuing treatment
Finally, this subtheme portrays the dilemma many patients experience regarding the continuation or discontinuation of their and dealing with the consequences of their choices. A severely debilitated patient, after more than 2 lines of court-ordered treatment, claimed to be very sad and cried profusely during the interview. Sometimes it seemed that he was sad because he understood the end of life (“I’m hopeless”), and other times because he acknowledged: “but I can’t take it anymore” as if living or dying was an option depending on how much more he could endure, the level of fortitude he still had to undergo treatment.
“Cancer will not defeat me” (Krebs schaffen mich nicht) and “I will die of something else” were recurring phrases. A patient reported that “When I was really bad [because of chemotherapy], I weighed up to 40-something kilos, I was in bed all day – I thought I might be dying. But I never gave up, for my daughter’s sake,” “I almost died from the chemotherapy” and “chemotherapy almost killed me, but I won” were phrases said by other patients. A German patient stated that he could not stop the treatment for his 15-year-old daughter and for his wife, “who is afraid that she cannot handle all the responsibilities by herself.” Despite this, he said he was sad, “because he thinks positively, but his wife doesn’t.”
Discussion
This study aimed to explore the expectations of Brazilian and German patients regarding metastatic cancer and palliative chemotherapy. It was expected that differences between the statements of German and Brazilian patients would be found, considering the cultural, historical, and socioeconomic differences between both countries, in addition to the availability of palliative and EoL care in both countries. However, what had the greatest impact was the similarity of the patients’ statements, regardless of their nationality. People with metastatic cancer in Brazil and Germany, inserted in different care cultures and from different social backgrounds, tend to believe in the curative potential of treatments. As pointed out in the results and in line with the existing literature, several patients mistakenly perceive their palliative treatments as curative, fail to consider themselves as having a terminal stage disease, overestimate their life expectancy (Chen et al. Reference Chen, Cronin and Weeks2013; Epstein et al. Reference Epstein, Prigerson and O’Reilly2016; Weeks et al. Reference Weeks, Catalano and Cronin2012), and remain hopeful of being cured and hear but fail to understand the prognosis (Lindhardt et al. Reference Lindhardt, Winther and Pfeiffer2021).
The conversations about care objectives are often conducted by physicians who are unfamiliar with the patient, do not routinely address patients’ nonmedical objectives, and often do not provide patients with sufficient information about prognosis to allow for appropriate decisions; moreover, they tend to conduct communication about such issues at a belated time (Bernacki et al. Reference Bernacki and Block2014). Also, according to a systematic review on interventions to improve prognostic understanding in advanced stages of life-limiting illnesses, even after carrying out interventions to improve communication, inaccurate understanding of prognosis was common among 31–95% of patients (George et al. Reference George, Matsoukas and McFarland2022). These data lead to thoughts on another important aspect that needs to be discussed: How many patients may be unable to understand complex issues. The need for informed consent for procedures and treatments such as chemotherapy generally disregards people who are fully able to perform daily activities but are often functionally illiterate (individuals who, although they can recognize letters and numbers, are unable to interpret and understand simple texts). Clarifying the prognosis of a serious illness and expecting the patient to make a truly informed decision can be fiction in several cases. But even if this communication issue is overcome, it is important to discuss to what extent the patient’s will – if and when truly informed – can impose conduct on health systems, as, for example, in cases of lawsuits for chemotherapy medication for the treatment of terminally ill patients. Even among people who have already surpassed the general indexes of life expectancy, there is hardly a natural acceptance to live only that far (Araújo Reference Araújo2020).
Through the reports, it was also possible to identify patients’ need to be seen beyond their disease. Being recognized as a person until the end of their lives and knowing the truth about their illness are relevant needs of cancer patients in palliative care (Vilalta et al. Reference Vilalta, Valls and Porta2014). Some patients do not desire excessive attention and kindness; they just expect their close ones to behave normally (Taleghani et al. Reference Taleghani, Yekta and Nasrabadi2006). According to a review study that aimed to identify preferences for palliative care among patients in the palliative phase of their illness, patients would like a form of palliative care that allows them to “live a meaningful life” (Sandsdalen et al. Reference Sandsdalen, Hov and Høye2015).
According to the results, in addition to spirituality/religiosity being identified as an important coping strategy by patients, faith was often perceived as enabling access to treatments that could cure the disease. It is worth noting that this was part of the Brazilian patients’ profile. In Brazil, it was very common for people to talk about God (not necessarily in a religious manner); however, in Germany, none of the patients talked about faith, religion, or spirituality. A study conducted in the US examined whether religious belief in miracles modifies how patients receive news about cancer progression and understand prognosis (George et al. Reference George, Balboni and Maciejewski2020a). Among most patients with moderate to strong religious belief in miracles, news of cancer progression was associated with no change in their understanding of the prognosis (George et al. Reference George, Balboni and Maciejewski2020a). In other words, there is evidence that religious belief in miracles can limit the impact of prognostic information, even when that information involves concrete medical data from test results (George et al. Reference George, Balboni and Maciejewski2020a).
One of the subthemes identified points to the conflict that patients face in choosing whether to continue or even discontinue treatment. Many patients feel guilty for an eventual lack of optimism – which is often absolutely accurate. Buiting et al. (Reference Buiting, Rurup and Wijsbek2011) demonstrate that the use of chemotherapy even in the final stages of the disease can be justified by the way doctors and patients interact, with stances from both toward “not giving up”.
The use of acknowledged methodological references that guided the definition of data collection and analysis techniques grants greater reliability to this study’s results. The fact that the interviews were not recorded may be considered a study limitation; however, the decision to not record them was made as it was understood that this could intimidate the interviewees, when the intention was, on the contrary, to provide them with the greatest possible freedom to speak about anything that seemed relevant. Despite the cultural differences and specificities of the health systems of each country (e.g., in Brazil, participants received care from the public health system, and German participants had private health insurance), the reports of all participants were similar considering the themes presented in this study’s results.
Implications for clinical practice
In this sense, the findings of this study may contribute to the clinical practice of both oncologists and palliative care teams, especially regarding communication of prognosis and treatment goals. The understanding, by the patient, that his or her disease is curable or incurable seems to be insufficient to properly address the issue of wrong expectations of advanced cancer patients. They may often misunderstand the goals of palliative chemotherapy, believing that it will keep them alive for a long time, as long as they tolerate it – as hemodialysis for renal failure, for example. Thus, we are convinced that our study can help direct the development of guides/checklists aimed at facilitating the communication process in clinical practice between health-care professionals and people with advanced cancer. We also hope that clinicians will use the data from this manuscript and apply them in their routine.
Furthermore, the findings of this study point out the importance of developing communication skills in all health-care professionals who somehow deal with terminally ill patients. In addition, it helps to corroborate the importance of early involvement of palliative care professionals in cases of life-threatening illness, considering their proper training in communication skills especially for seriously ill patients.
Conclusion
Regardless of cultural aspects, metastatic cancer patients on palliative chemotherapy tend to believe in the curative potential of treatments. Dividing expectations only into curable or incurable, as seen in previous studies, is insufficient, as even patients who have acknowledged the incurability of their disease expect to live, as long as they remain under treatment as if the disease did not exist: “While there is chemotherapy, there is life.”
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Ethical approval
This study was approved by the Ethics Committees of the Pontifícia Universidade Católica de Minas Gerais (CAAE registration no. 76655317.0.0000.5137, opinion no. 2.560.620). After being informed of the study’s goals, the interviews’ confidentiality and protection of anonymity, as well as the fact that participation in the study was entirely voluntary and they might discontinue at any moment, participants submitted written informed consent.




