Case report
Pulmonary atresia intact ventricular septum comprises 1% of CHDs.Reference Daubeney, Delany and Anderson 1 It occurs as a spectrum, defined by complete obstruction of the pulmonary valve, with varying degree of tricuspid and right ventricular hypoplasia. Coronary abnormalities are frequently associated with this cardiac defect, including arterial stenosis or atresia in 4–25%. Reference Daubeney, Delany and Anderson1,Reference Hanley, Sade and Blackstone2 At the most severe end of the spectrum are those with severe right ventricle hypoplasia, right ventricle-dependent coronary circulation, and proximal coronary atresia. The outcome is excellent for patients amenable to biventricular repair. Patients undergoing single ventricle palliation also demonstrate good outcome, with reported 80% survival at discharge and post-Fontan survival up to 96%. Reference Hanley, Sade and Blackstone2,Reference Elias, Poh and du Plessis3 However, right ventricle-dependent coronary circulation is a risk factor for mortality, especially when associated with coronary ostial atresia. Reference Elias, Poh and du Plessis3–Reference Cheung, Richmond, Turner, Bacha and Torres5 Confounding the outcome of these infants is the presence of prematurity and low birthweight, both of which are associated with increased mortality and morbidity in infants undergoing cardiac surgery. Reference F.Daubeney, Wang and Delany6–Reference Costello, Pasquali and Jacobs8
Here we present a case with twin gestation, very preterm birth, very low birthweight, with pulmonary atresia intact ventricular septum, right ventricle-dependent coronary circulation, coronary atresia, and discontinuous pulmonary artery. The diagnosis was made at 16 weeks of gestation with suspicions for coronary fistulas. Due to premature rupture of membrane, the mother delivered at 28 weeks. Birthweight was 1.2 kg. Post-natal echocardiogram confirmed pulmonary atresia intact ventricular septum with severe tricuspid valve and right ventricle hypoplasia. Bilateral coronary ostia were atretic with right ventricular-coronary fistulas. The ductus was tortuous and there was right pulmonary artery stenosis at the ductal insertion site and suspected discontinuous pulmonary arteries.
The patient was intubated in the delivery room for respiratory distress. Given the patient’s multiple risk factors for poor outcome, the palliative care team was involved early. His parents were counselled of his poor prognosis, but they were committed to pursuing intervention for his heart disease. He was thus conservatively managed with mechanical ventilation, prostaglandin, diuresis, parenteral nutrition, and cautious enteral feeding. As expected due to prematurity and mal-distributed circulation, the patient was slow to wean from invasive ventilation. He had two brief bradycardic arrests associated with hypoxia secondary to airway dislodgement and mucous plugging. However, the underlying long-segment right pulmonary stenosis may have attenuated pulmonary over-circulation, allowing a period of stability when he was able to gain somatic growth. At 11 weeks, he decompensated with necrotising enterocolitis, which was treated with antibiotic and bowel rest.
He subsequently underwent cardiac catheterisation and cardiac CT that confirmed bilateral coronary ostia atresia, right ventricle-coronary fistulas (Fig 1), a large tortuous ductus arteriosus, and discontinuous right pulmonary artery (Fig 2). Qp:Qs was greater than 3:1 with cardiac index of 2.7–3 L/minute/m2. Mean right pulmonary artery pressure was 12 mmHg, and mean left pulmonary artery pressure was elevated at 25 mHg. Cardiac transplant team was consulted for potential transplant listing. However, given the urgency of his condition, we proceeded with surgical palliation with a shunt and correcting the discontinuous pulmonary arteries by end-to-end anastomosis and patching.
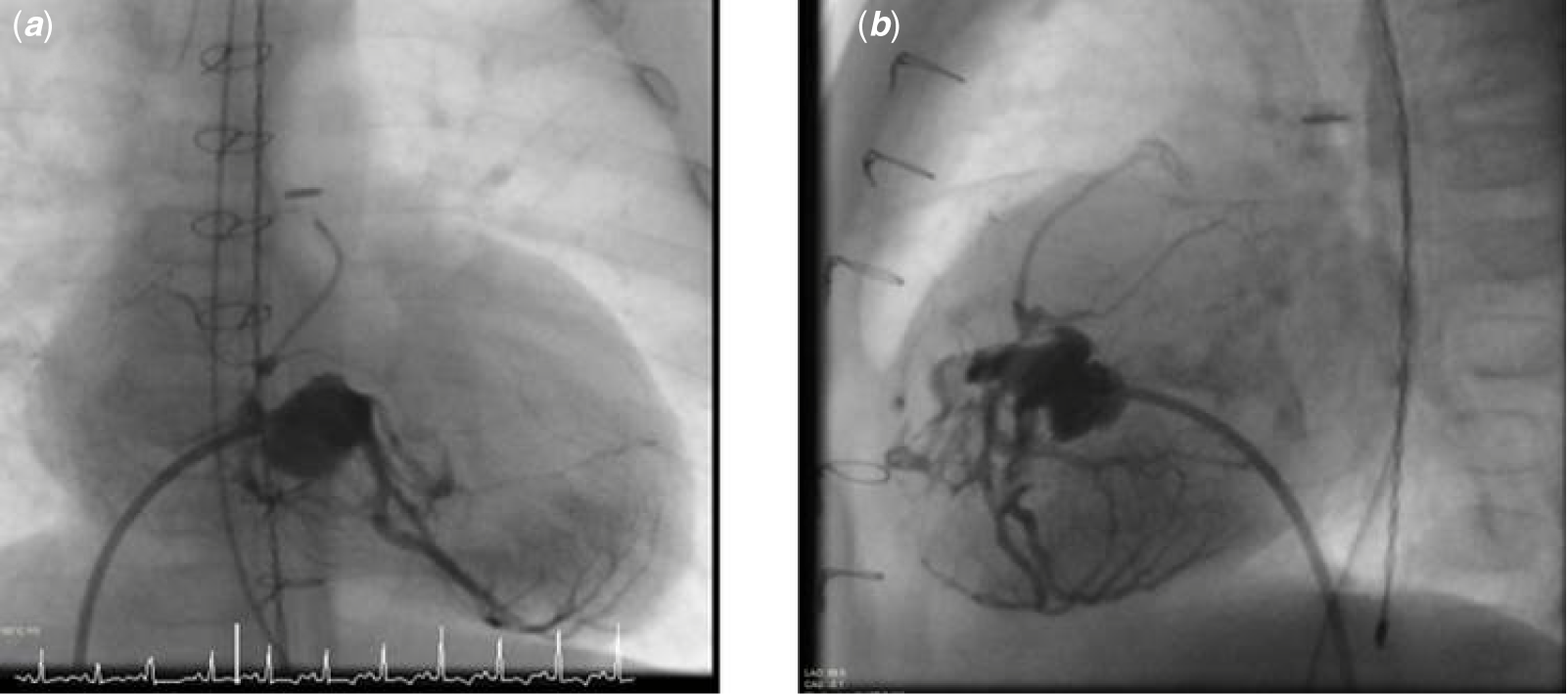
Figure 1. Cardiac catheterisation with right ventricle angiogram at 5 months. ( a ) Anterior-posterior and ( b ) the lateral projection. The right ventricle is unipartite and severely hypoplastic with multiple right ventricle-coronary fistulas.

Figure 2. Cardiac CT in the axial plane demonstrating discontinuous pulmonary arteries with the main ductus arteriosus feeding the left pulmonary artery and a small segment of the ductus arteriosus going to the right pulmonary artery. The right pulmonary artery is severely stenotic with long-segment narrowing.
At 12 weeks and 3.12 kg, the patient underwent surgical palliation with a 3.0 modified Blalock–Taussig shunt, ductus ligation, pulmonary coarctectomy, and right pulmonary arterioplasty. Post-operative echocardiogram demonstrated stable ventricular function with no evidence of ischaemia. He was supported with low dose vasoactive post-operatively. On post-operative day #2, he underwent sternal closure. He was extubated on post-operative day #4 and transferred out to the floor on post-operative day #12, where he remained during the interstage period. Follow-up cardiac catheterisation during the interstage period showed confluent pulmonary arteries, although the right pulmonary artery was diffusely hypoplastic (Supplementary File, Fig 1). Subsequently, he underwent a bidirectional Glenn and right pulmonary arterioplasty at 26 weeks and 4.4 kg. His post-operative course was unremarkable. He was transferred out of the ICU on post-operative day #4. Two weeks after surgery, he was discharged home. Presently, at 4 months after discharge, he is doing well at home on room air with no cardiac symptoms, eating all by mouth, and gaining weight. Follow-up echocardiograms have consistently demonstrated stable function without significant valvular regurgitation, unrestrictive atrial septum, and patent Glenn anastomosis.
Discussion
Pulmonary atresia intact ventricular septum with right ventricle-dependent coronary circulation is a challenging disease with guarded outcome due to elevated risk of myocardial ischaemia. Patients with bilateral coronary ostia atresia are the highest risk group, with two separate case series reporting 100% mortality in their cohorts with right ventricle-dependent coronary circulation and bilateral coronary ostial atresia. Reference Guleserian, Armsby, Thiagarajan, del Nido and Mayer4,Reference Cheung, Richmond, Turner, Bacha and Torres5 Here we report a remarkable course of a very preterm patient with an unusual diagnosis of pulmonary atresia intact ventricular septum with right ventricle-dependent coronary circulation, bilateral coronary atresia, and discontinuous pulmonary artery. This is the first report case of rare occurrence of pulmonary atresia intact ventricular septum with discontinuous pulmonary arteries. The largest population-based morphology study of 183 pulmonary atresia intact ventricular septum patients in Europe showed that 8% of patients had hypoplastic pulmonary arteries, but all pulmonary arteries were confluent. Reference Daubeney, Delany and Anderson1
Prematurity and low birthweight were additional complicating factors predicting occurrence of serious adverse events. There is a gap in data for the outcome of very premature infants with very low birthweight with single ventricle heart disease and extremely limited in pulmonary atresia intact ventricular septum. The lack of data likely reflects poor outcome or reluctance to pursue surgical interventions because of anticipated poor outcome. Despite being very preterm with very low birthweight with complex unpalliated single ventricle heart disease, this patient was successfully managed with conservative medical therapy to ultimately undergo delayed surgical palliation with a shunt as well as pulmonary arterioplasty and subsequently cavopulmonary anastomosis. He is doing well but requires close monitoring of his cardiac function as well as neurodevelopmental and respiratory status due to his prematurity and long hospitalisation. The strategy of conservative medical therapy, careful operative planning, and delayed surgical palliation was successful to get this patient home safely despite multiple negative risk factors predicting poor outcome. Outcome data for very preterm infants with single ventricle as well as pulmonary atresia intact ventricular septum are needed to improve decision-making in these challenging patients.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951122000038
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
Not applicable.





