Introduction
It is estimated that one in seven general practitioner (GP) consultations is for a musculoskeletal problem, of which the most common is in the back (Jordan et al., Reference Jordan, Kadam, Hayward, Porcheret, Young and Croft2010). Once ‘red flag’ pathologies are ruled out, back and neck pain, particularly in the sub-acute and chronic phases, can be difficult to treat and costly in terms of GP visits and prescription drugs. Referral to secondary care and tracking patient progress leads to further costs and burden on general practice time. Although it is a minority of patients with musculoskeletal disorders who become severely disabled, the prevalence and incidence of back pain at the population level are such that effective management, particularly in the early stages, is of paramount importance not only to the individual, but to society at large.
A plethora of guidelines have been produced worldwide, in the main with consistent recommendations for the management of non-specific musculoskeletal conditions (Koes et al., Reference Koes, van Tulder, Lin, Macedo, McAuley and Maher2010). In the United Kingdom, the NICE guideline (2009) recommends that in cases of low back pain lasting more than six weeks, patients should be referred to either an exercise programme or a course of acupuncture or a course of manual therapy. Manual therapy is defined in the guideline as ‘spinal manipulation, spinal mobilisation and massage’. Mobilisation and massage are performed by a wide variety of practitioners. Manipulation can be performed by chiropractors and osteopaths, as well as by doctors and physiotherapists who have undergone specialist postgraduate training in manipulation.
In line with the Musculoskeletal Services Framework (2006), multi-professional clinical assessment and treatment (CAT) services have been set up for the management of musculoskeletal conditions in some areas of the United Kingdom. These services, which are at the primary–secondary care interface, have been shown to reduce inappropriate referrals to secondary care and waiting times for patients, increase orthopaedic conversion rates and be highly rated in satisfaction surveys of patients and GPs (Roddy et al., Reference Roddy, Zwierska, Dawes, Hider, Jordan, Packham, Stevenson and Hay2010; Sephton et al., Reference Sephton, Hough, Roberts and Oldham2010). Most recently, the Department of Health (2011) published guidance on patient choice of Any Qualified Provider, in which musculoskeletal services for back and neck pain were identified for implementation from April 2012. This is intended to empower patients, improve their outcomes and experience, enable service innovation and free up clinicians to drive change and improve practice.
In 2009, North East Essex Primary Care Trust (PCT) commissioned a manual therapy service comprising chiropractors, osteopaths and physiotherapists to manage patients referred by GPs with persistent back or neck pain. This service differed from the National Health Services (NHS) CAT model in that it was provided entirely by primary care independent healthcare professionals working in the community and focused on managing back and neck pain triaged by the GP in the first instance.
The primary goal of this service from the PCT perspective was to improve patient outcomes, provide more equitable access, choice and waiting times for patients, and to reduce demand on local NHS services, including referrals to physiotherapy outpatient clinics, imaging services, pain clinics and rheumatology and orthopaedic services. In view of the allocated resources and the shortage of evidence to support service development in this area, we evaluated the service during its one-year pilot phase in terms of: (1) the characteristics of patients with back or neck pain referred to the service; (2) the health outcomes in these patients at discharge; and (3) the experiences of these patients.
Method
Patients
Adult patients presenting to their GP with back or neck pain were assessed to rule out ‘red flag’ pathologies such as infection, cauda equina compression, malignancy and serious co-morbidity. These patients received ‘usual’ GP care including advice, reassurance and analgesia for a period of at least four weeks (most for between four and six weeks). Subsequently, patients were offered a course of manual therapy and, in consultation with their GP, a choice of provider (chiropractor, osteopath or physiotherapist). Patients were seen by their preferred provider within 14 days, when they were assessed and treated (up to six treatment sessions or additional treatments with the approval of the GP). At the end of treatment, patients were discharged and referred back to their GP with a report including any recommendations for further management. The service pathway is outlined in Figure 1.
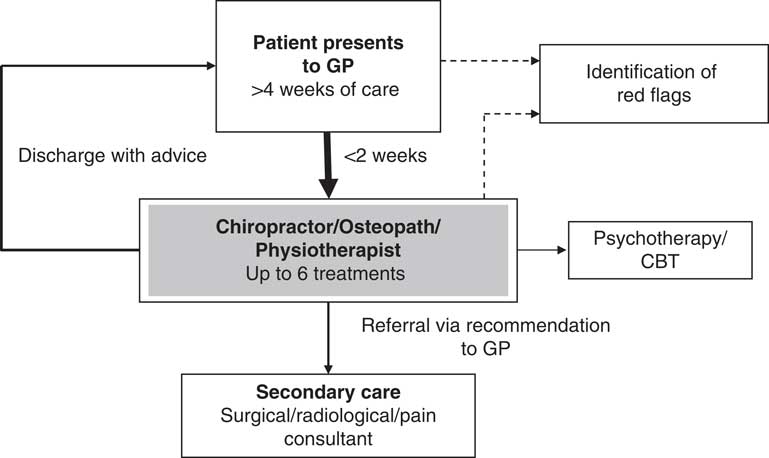
Figure 1 Multidisciplinary primary care service for general practitioner (GP) referred back and neck pain
Service design
The service was developed by a team of clinicians, commissioners and patient representatives over a period of two years culminating in an agreed service plan. Eligible patients were those seen by the GP for persistent back or neck pain, and suitable for manual therapy according to the guideline. The service was pragmatic, and each patient was assessed and treated by their preferred provider as would occur in usual practice. No restrictions were placed on treatment protocols, only on the number of treatments (up to six), which were free at the point of delivery.
In June 2008, all independent providers of chiropractic, osteopathy and physiotherapy in North East Essex were invited to bid for provision of services under the Any Willing Provider contract. The service was initially run as a one-year pilot from April 2009 to March 2010 and continually monitored throughout.
Data collection
Part way through the pilot phase (August 2009), the PCT decided to evaluate the service using patient-reported outcome measures. On entry to the service (baseline), patients were asked to complete a comprehensive questionnaire including sociodemographics and clinical characteristics of their complaint. Outcome measures included the Bournemouth Questionnaire (BQ), a validated outcome measure for back (Bolton and Breen, Reference Bolton and Breen1999) and neck (Bolton and Humphreys, Reference Bolton and Humphreys2002) pain, and designed for use in the routine practice setting, and the Bothersomeness questionnaire (Dunn and Croft, Reference Dunn and Croft2005). Patients completed a second questionnaire at discharge from the service which, in addition to the BQ and Bothersomeness questionnaires, included a global improvement scale (7-point scale: very much improved, much improved, slightly improved, no change, slightly worse, much worse and very much worse), a patient satisfaction with treatment scale (5-point scale: very satisfied, satisfied, unsure, dissatisfied and very dissatisfied) and details of medication usage, other healthcare utilisation and work status.
Data analysis
Descriptive statistics were used to summarise the sociodemographics and clinical characteristics of the patients referred to the service. Confidence intervals were not included as this was a specific service evaluation and the findings are not necessarily generalisable.
Percent changes in BQ scores were calculated as the change in score from baseline to discharge compared with baseline score (([baseline score-discharge score]/baseline score) × 100). Percent change scores less than or equal to 0 were arbitrarily categorised as ‘deterioration’, from 1 to 10 as ‘small improvement’, from 11 to 30 as ‘moderate improvement’ and >30 as ‘significant improvement’. In support of this categorisation, a >30% score change is often reported as the minimal clinically important difference for outcome measures used in non-specific musculoskeletal disorders (Ostelo et al., Reference Ostelo, Deyo, Stratford, Waddell, Croft, Von Korff, Bouter and de Vet2008). For raw change scores on the Bothersomeness scale, a change score between baseline and discharge <0 was categorised as ‘deterioration’, 0 as ‘no change’ and >0 as ‘improvement’.
Data analysis was carried out using SPSS, v17.0.
Approval
This study was considered a service evaluation and as such did not require ethics approval (National Research Ethics Service, 2010). All patients were informed in writing that the information given in the questionnaires would be used anonymously in the evaluation of their care.
Results
The service was provided by three chiropractic, three osteopathic and 10 physiotherapist clinics in the independent sector. The number of practitioners in each clinic ranged from 1 to 9. Providers worked to agreed referral and clinical protocols, and price, and although there was competition there was also co-operation between individual providers to ensure service integration for the benefit of patients. In total, 2810 patients were referred into the service during the pilot phase. Of these, 23% (n = 646) were seen by chiropractors, 32% (900) by osteopaths and 45% (1264) by physiotherapists. Almost all (97%) patients were seen within two weeks of GP referral. Of these patients, questionnaire data were available from 696 patients accessing the service between August 2009 and March 2010.
Sample characteristics at baseline
The demographic and clinical characteristics of the study sample are shown in Table 1. The mean age of the sample was 52 years, approximately two-thirds was female and just over half was in paid employment. Of these, approximately a third had taken some time off work for their complaint, and a third reported having taken time off work in the past for a similar complaint. Approximately two-thirds of the sample considered their overall levels of physical activity to be either more or about the same compared with people of a similar age, and apart from their musculoskeletal complaint the majority of patients considered themselves to be in excellent to good general health.
Table 1 Baseline characteristics of patients referred to the service (n = 696)
For categorical variables, values are numbers (%).
*For continuous variables, values are means (±SD).
All patients had either back and/or neck pain and in some cases additional pain in the leg, shoulder/arm, and headache. Although the complaint in most patients could be categorised as non-specific pain, patients were included with clear signs of radiculopathy. Approximately two-thirds of patients had had a similar complaint(s) in the past, and most patients presented with either sub-acute (less than three months; 51%) or chronic (less than three months; 49%) pain. Of the patients with chronic pain, about half (49%) had had their pain for over 12 months. Using the definition of a whole month pain-free in the previous six months to categorise episodic pain, most patients were defined as non-episodic, with 61.2% describing their pain as ‘constant’ and 77% describing it as being severe enough to limit or change their day-to-day activities for more than one day in the previous month. Over half of patients were taking either prescribed or over the counter medication for their pain and, apart from their GP and service provider, most were not seeking care from another practitioner. When asked about their expectations of the treatment they were about to receive, the overwhelming majority expected to either recover or improve.
Health outcomes and patient satisfaction
Patients on average received six treatments over a period of just under eight weeks. Figure 2 shows the percent change in total BQ scores from baseline to discharge. Approximately two-thirds (64.6%) of patients were categorised as being significantly improved. Using change scores on the Bothersomeness scale (Figure 3), again approximately two-thirds (69.9%) of patients were categorised as improved. Using the global improvement scale, a similar proportion (67.8%) to that using the BQ and Bothersomeness scales reported that they were either very much or much improved. Approximately 7% reported that there was no change, and 1.7% that their condition had worsened. Almost all patients (99.5%) reported that they were either very satisfied or satisfied with the treatment they received. There were no treatment-reported incidents.
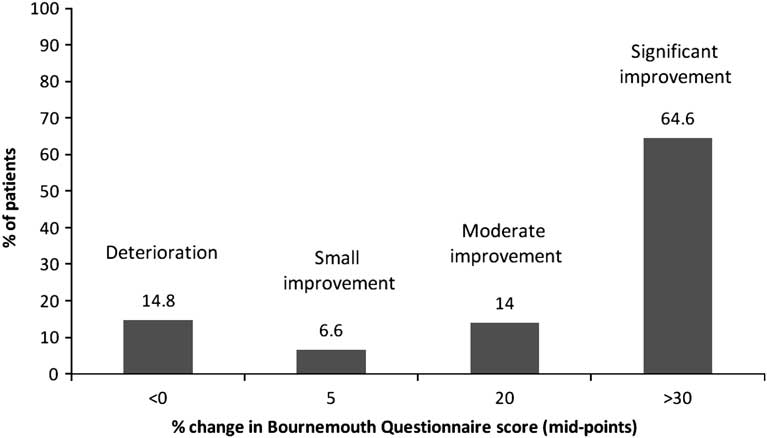
Figure 2 Percentage change in Bournemouth Questionnaire scores from baseline to discharge
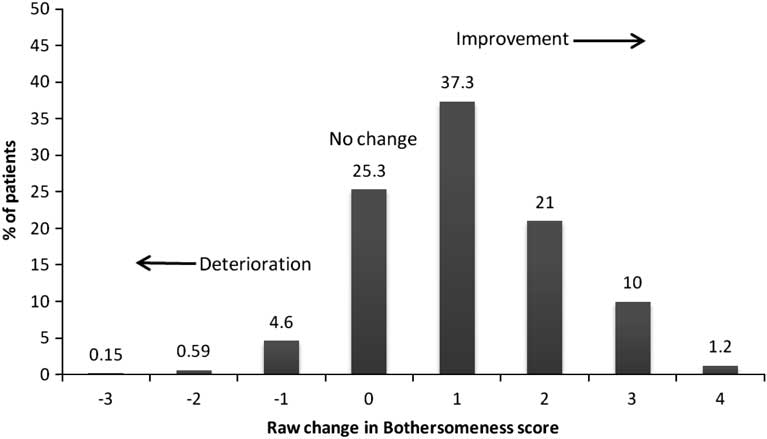
Figure 3 Raw change in Bothersomeness score from baseline to discharge
A small proportion (3%) of patients was referred back to their GP with the recommendation for referral to secondary care services. The remaining patients (97%) were given self-management advice and recommended for discharge. In terms of medication usage, approximately 65% of patients taking medication at the outset reported a significant reduction. A small minority of patients (7%) had utilised other healthcare, including their GP, while being treated by their service provider.
Discussion
It is apparent that there is a need for provision of services to deal with patients with non-specific musculoskeletal complaints, particularly back pain, to reduce the burden on general practice management and enhance the efficiency of the use of secondary care services both in terms of reduction in inappropriate referrals and increased conversion rates to surgery (Roddy et al., Reference Roddy, Zwierska, Dawes, Hider, Jordan, Packham, Stevenson and Hay2010; Sephton et al., Reference Sephton, Hough, Roberts and Oldham2010). Although it is now established in secondary care that CAT centres are well placed to carry out triage and place the patient in the most appropriate pathway, we describe here a primary care service working in partnership with GPs in the delivery of faster, local and evidence-based care for patients. Given the new Any Qualified Provider initiative (Department of Health, 2011), the evaluation of this service is particularly timely.
The patients in this study represent a young middle-aged group, just over half of whom were in paid employment and who, apart from their musculoskeletal condition, considered themselves to be generally active and otherwise in good health. Their musculoskeletal pain was sub-acute or chronic in nature, typically recurrent, and severe and prolonged enough to spur them to seek help from their GP. Unlike patients with an acute episode that almost always resolves within days to a few weeks, this subgroup of patients is not only costly in terms of GP and other healthcare resources, but is at risk of severe disability and prolonged incapacity.
This service was capable of handling almost 3000 patients in one year, all of whom were seen within two weeks. In evaluating the service, two-thirds of patients reported improvement after six treatments and were recommended for discharge with advice on self-management. Although a significant minority did not report improvement, less than 3% were recommended for subsequent referral to secondary care. Thus, we describe a service that appears to offer effective management in the community, associated with shorter waiting times and a high level of patient satisfaction. Evaluation by the PCT demonstrated that the service reduced primary care consultations, imaging and inappropriate referrals to secondary care. Referrals to spinal surgeons reduced by more than 25%. As a result of the pilot, the service was extended to March 2012.
A strength of this study was that this was a real-time evaluation of a new service, in which we observed a large sample assumed to be typical of patients with non-specific musculoskeletal pain being treated by GPs. We were unable to do a precise calculation on the saving of costs to the NHS, particularly as we did not know how many of these patients would have been referred to secondary care if the new service had not been in place. Moreover, as an uncontrolled study we are unable to interpret any of the outcomes as being directly attributable to the treatment. However, all patients had pain for more than four weeks and many for considerably longer. It is unlikely therefore that natural history accounted in any significant manner for the observed outcomes in these patients. In terms of outcomes, patients completed questionnaires in the presence of their treating clinician, which may have led to reporting bias on their part.
This study describes a musculoskeletal service provided by chiropractors, osteopaths and physiotherapists in the community capable of providing high-quality evidence-based care. The service enabled patients to be seen quickly and to exercise choice on their preferred provider in consultation with their GP. We are currently collecting similar data in the main phase of this service provision with the aim to further evaluate the service.
Acknowledgements
We are grateful to all the providers in the service and to NHS North East Essex, in particular Ms Sarah Esson, for help and support in providing the data for this article.






