Introduction
Sinus venosus defect is a rare cause of interatrial communication representing up to 11% of all cases. Peacock described this defect permitting the interatrial communications as distinct from the normal atrial septum; hence, it is not a true atrial septal defect. Reference Peacock1 It has been well-established that the morphological criterion for diagnosis is the integrity of the rims of the oval fossa. Reference Crystal, Al Najashi, Williams, Redington and Anderson2,Reference Ettedgui, Siewers, Anderson, Park, Pahl and Zuberbuhler3 Previous authors described “unroofing” of the right pulmonary veins as the explanation for such defects, on the basis that a “shared wall” normally separated these venous structures from the superior caval vein and the cavity of right atrium. Reference Van Praagh, Carrera, Sanders, Mayer and Van Praagh4 However, this concept has been refuted as this “shared wall” is in fact an interatrial groove arising from an infolding of the atrial walls between the atrial connections of the caval and pulmonary veins, rather than a true atrial septum. Reference Anderson, Webb and Brown5,Reference Butts, Crean and Hlavacek6 This aetiology was further validated by elegant episcopic microscopy studies. Reference Anderson, Brown and Moorman7,Reference Anderson, Mohun and Brown8 In a review by Crystal et al. describing patients with inferior sinus venosus defects, the authors described the defining diagnostic feature as the anomalous connection of one or more pulmonary veins to the inferior caval vein, with the anomalous pulmonary vein or veins retaining their connection with the left atrium. Reference Crystal, Al Najashi, Williams, Redington and Anderson2 Recent anatomical studies have provided further evidence to support these defects representing veno-venous bridges allowing the interatrial communication. Reference Anderson, Brown and Moorman7–Reference Tretter, Chikkabyrappa and Spicer10
The pre-operative diagnosis of sinus venosus defects can be challenging and may be missed by solely relying on conventional planes in transthoracic echocardiography. This is due to the defects’ close relationship with either the superior or inferior vena cava, outside the confines of the true interatrial septum. Reference Freed, Nadas, Norwood and Castaneda11–Reference Nasser, Tajik, Seward and Hagler13 Several studies have demonstrated echocardiographic subcostal sagittal-oblique bicaval view with use of colour flow mapping improves the detection rates of sinus venosus defects, notwithstanding the challenges in older obese patients due to poor echocardiographic windows. Reference Crystal, Al Najashi, Williams, Redington and Anderson2,Reference Ettedgui, Siewers, Anderson, Park, Pahl and Zuberbuhler3,Reference Mühler, Engelhardt and von Bernuth14–Reference Snarr, Liu and Zuckerberg18 Transoesophageal echocardiography is one of the imaging modalities of choice for this cardiac defect. Reference Oliver, Gallego, Gonzalez, Dominguez, Aroca and Mesa19–Reference Pascoe, Oh, Warnes, Danielson, Tajik and Seward21 Other advanced cardiac imaging modalities such as cardiac MRI, Reference Valente, Sena, Powell, Del Nido and Geva22 cardiac CT, Reference Abdel Razek, Al-Marsafawy, Elmansy, El-Latif and Sobh23,Reference Vyas, Greenberg and Krishnamurthy24 and rarely, cardiac catheterisation Reference Freed, Nadas, Norwood and Castaneda11 have been used to complement the diagnosis of sinus venosus defects and delineation of anomalous pulmonary venous drainage.
The standard treatment for this defect has, up until recently, been surgical repair, although transcatheter closure in a selected group of patients is now increasingly an option. Reference Velasco Forte, Byrne and Valverde25–Reference Butera, Sturla, Pluchinotta, Caimi and Carminati32 Surgery aims to baffle the anomalously venous connection via the interatrial communication into the left atrium with or without enlarging the interatrial communication. Various surgical techniques have been well described with good results, including a single-patch baffle, double patch baffle, or Warden repair. However, there are associated low risks of sinus node dysfunction, atrial arrhythmias, and pulmonary or systemic venous occlusion after surgery. Reference Stewart, Alexson and Manning33–Reference Binsalamah, Ibarra and Edmunds44
This study aimed to review the prevalence of complex sinus venosus defects defined as either the presence of multiple anomalous pulmonary venous sites or high insertion of the anomalous pulmonary vein into the superior caval vein, ascertain the imaging modalities employed in delineating the anatomical variants, and the surgical outcome in this cohort of patients.
Methods
All patients who had a diagnosis of sinus venosus defect with partial anomalous right pulmonary venous drainage who underwent surgical repair were identified retrospectively from a dedicated National Institute of Cardiology Outcomes Research database from 2008 to 2019. Each patient’s medical records, diagnostic imaging modalities, and follow-up details were documented. Ethical approval was obtained from the Hospital Research Ethics Board.
Demographic and clinical details
Demographic details including patient age, gender, and weight at the time of the diagnosis and surgical repair were recorded. We documented the clinical symptoms at the initial presentation and the imaging modality used to reach the diagnosis. The primary outcome was procedural success (defined as successful completion of intended surgical procedure without revision). In addition, we noted any significant procedure-related complications.
Results
Patient demographic details are shown in Table 1. From 2008 to 2019, 37 children (20 male and 17 female) underwent surgical repair for sinus venosus defect with partial anomalous pulmonary venous drainage. Thirty-six of the patients have a diagnosis of superior sinus venosus defect and one patient was diagnosed with an inferior sinus venosus defect.
Table 1. Patient demographic details, patterns of anatomical variation, and surgical outcomes

Abbreviations: →=to; 2°ASD=secundum atrial septal defect; BPA=branch pulmonary arteries; CHD=congenital heart disease; CMR=cardiac magnetic resonance imaging; CoA=coarctation; CTA=computer tomographic angiogram; CXR=chest X-ray; DCSA VSD=doubly committed subarterial ventricular septal defect; Diagnostic Cath=diagnostic cardiac catheterisation; DS=down syndrome; FHx=family history; FTT=failure to thrive; ICV=inferior caval vein; LA=left atrium; LRTI=lower respiratory tract infection; PDA=patent ductus arteriosus; PH=pulmonary hypertension; PS=pulmonary stenosis; R SCV=right superior caval vein; RA=right atrium; RLPV=right lower pulmonary vein; RM/RLPV=right middle and right lower pulmonary veins; RMPV=right middle pulmonary vein; Rt PAPVD=right partial anomalous pulmonary venous drainage; Rt PVs=right pulmonary veins; RU/RMPV=right upper and right middle pulmonary veins; RUPV=right upper pulmonary vein; RVVO=right ventricular volume overload; SCV/RA=right superior caval vein and right atrial junction; SCVs=superior caval veins; SVD=sinus venosus defect; SVT=supraventricular tachycardia; TOE=transoesophageal echocardiogram; TTE=transthoracic echocardiogram.
The median age at diagnosis was 4.2 years (range 0.5−15.5 years of age). In 32 of 37 (86%) patients, sinus venosus defect was diagnosed and partial anomalous pulmonary venous drainage were suspected or diagnosed by two-dimensional transthoracic echocardiogram including a subcostal sagittal-oblique bicaval view scanning from the sinus venosus defect to the anomalous pulmonary venous connection (Fig 1). In 5 of the 37 patients, the sinus venosus defect could not be visualised on transthoracic echocardiogram alone. In three of these five patients, who presented with unexplained right ventricular volume overload, the final diagnosis was achieved by transoesophageal echocardiogram (Fig 2); one of these three patients underwent further diagnostic cardiac catheterisation and cardiac CT. In two of these five patients, the diagnosis of sinus venosus defect and partial anomalous pulmonary venous drainage was reached intra-operatively. One of these two patients has an additional diagnosis of complex ventricular septal defect and the other was diagnosed with an inferior sinus venosus defect.

Figure 1. (movie clip): Transthoracic echocardiogram subcostal sagittal-oblique bicaval view scanning from the sinus venosus defect to the anomalous pulmonary venous connection.
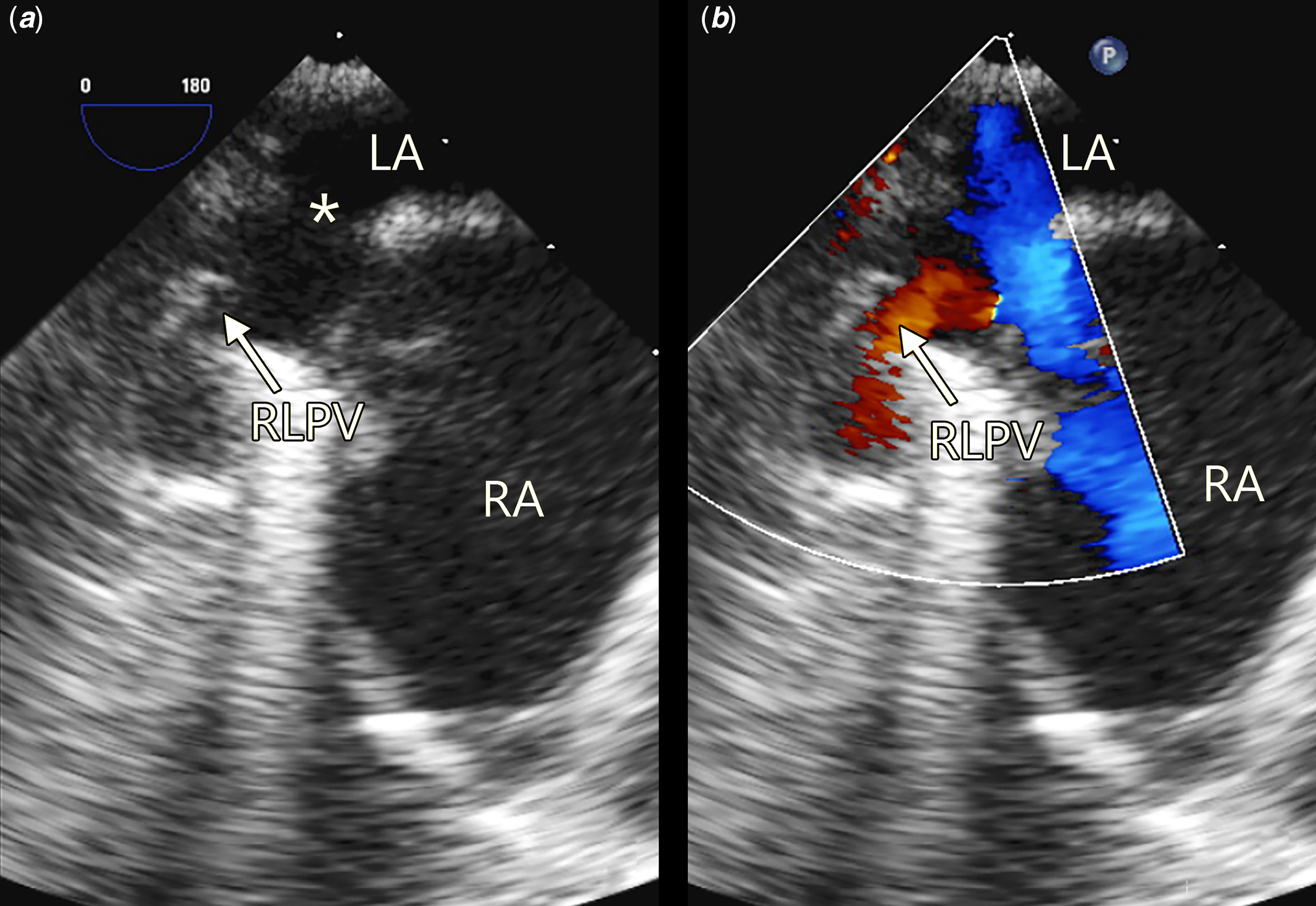
Figure 2. ( a and b ) Transoesophageal echocardiogram demonstrating the sinus venosus defect (*) and the anomalous right lower pulmonary vein (RLPV) draining directly into the right atrium (RA). LA=left atrium.
Variations of pulmonary venous drainage
The most common type of partial anomalous pulmonary venous drainage noted in this cohort was right upper and/or right middle pulmonary veins draining into the right superior caval vein. The patterns of insertion of the pulmonary veins are variable with low right superior caval vein being the commonest insertion point (19 of 37 patients). In ten cases, the anomalous pulmonary veins inserted into the right superior caval vein and right atrial junction (Fig 3). In three cases, the anomalous pulmonary veins drain directly into right atrium.
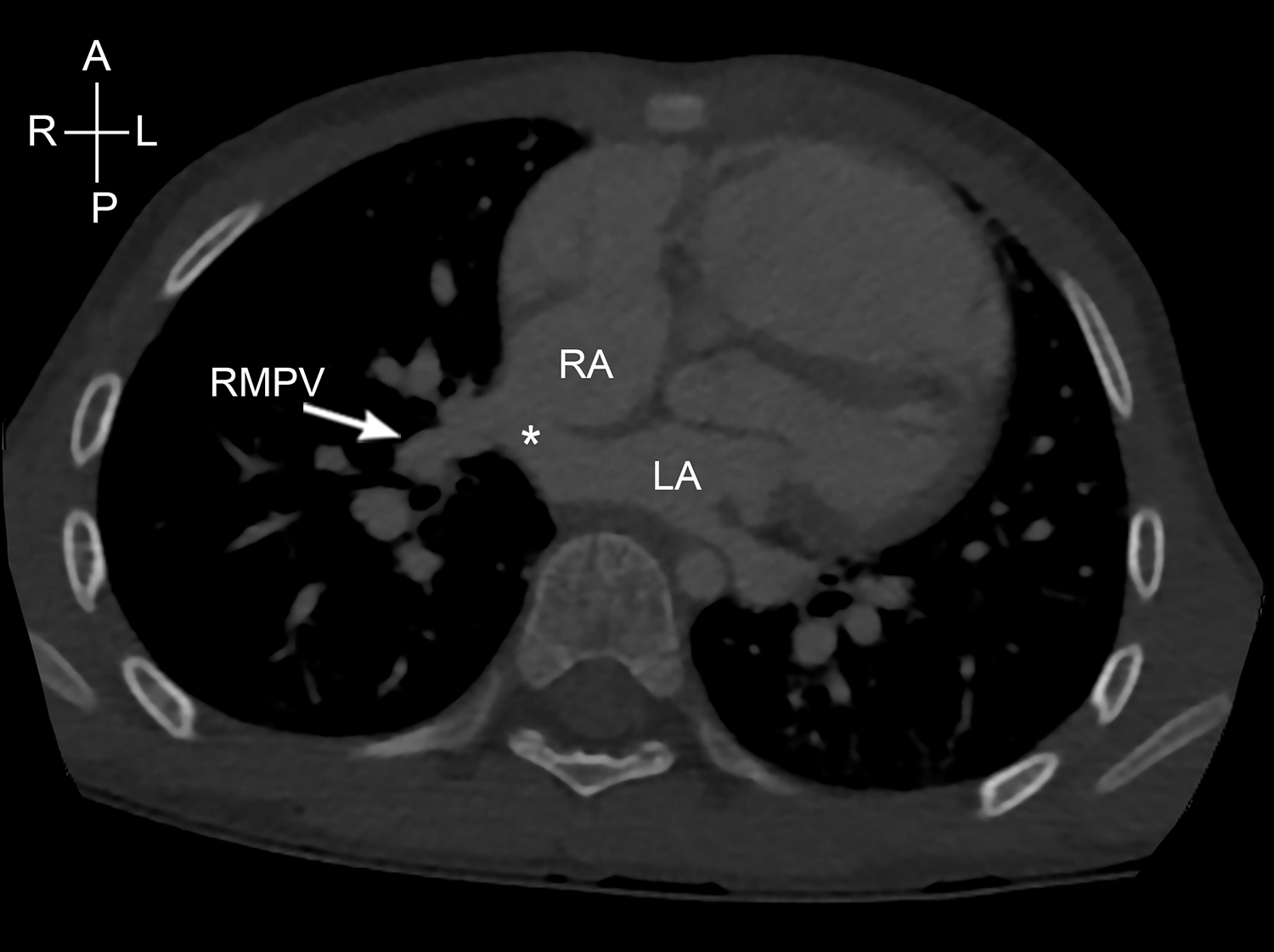
Figure 3. Computed tomography demonstrating right middle pulmonary vein (RMPV) draining to the right superior caval vein/right atrium junction. LA=left atrium; RA=right atrium.
Five patients had complex pulmonary venous variants. Four patients had high insertion of anomalous vein into the superior caval vein (Fig 4) and three patients had multiple anomalous veins draining to different sites, two of whom had high drainage of one vein to the superior caval vein (Fig 5). Six of the 37 patients have bilateral superior caval veins.
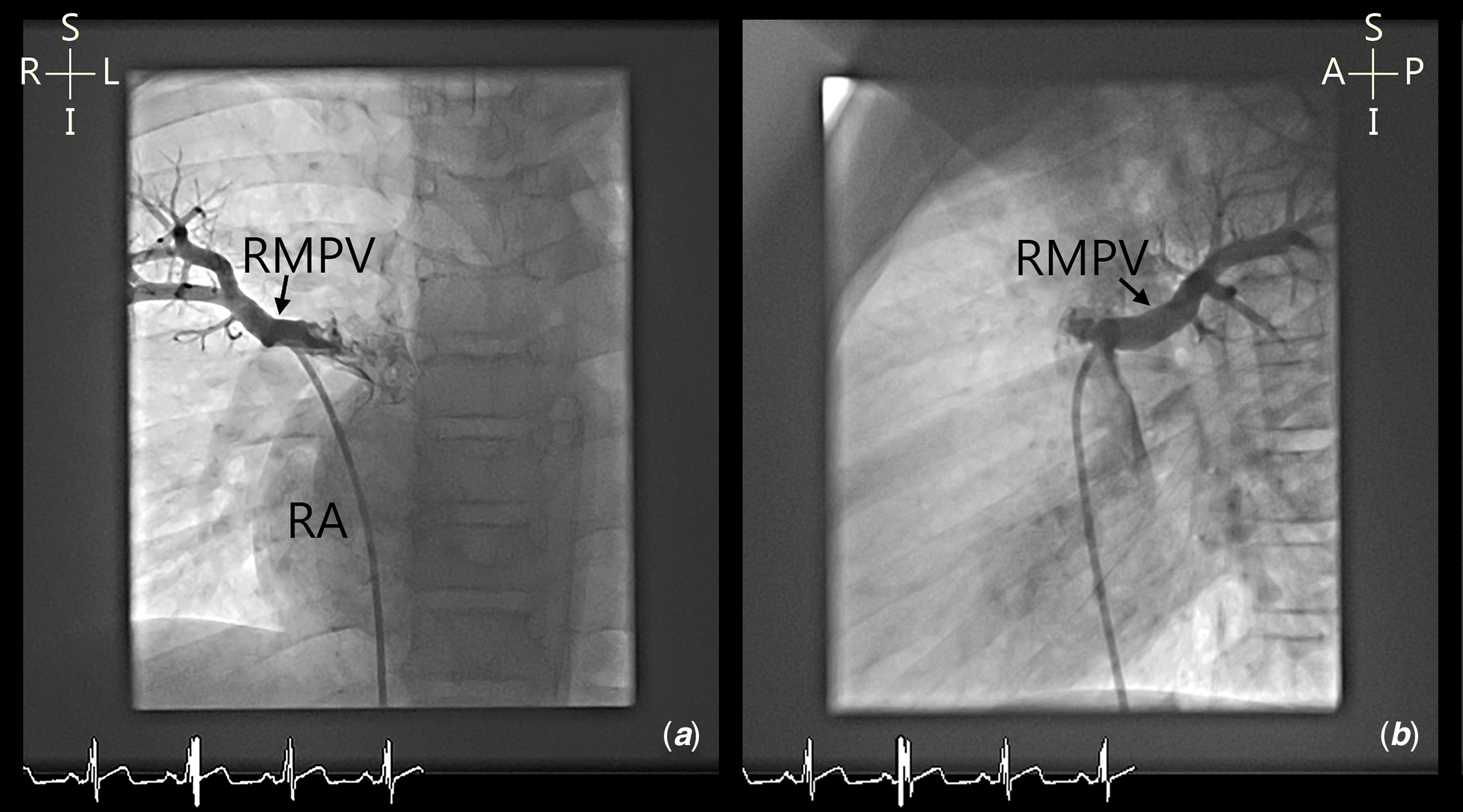
Figure 4. ( a and b ) Cardiac angiography demonstrating anomalous right middle pulmonary vein (RMPV) into right superior caval vein/right atrium junction. RA=right atrium.
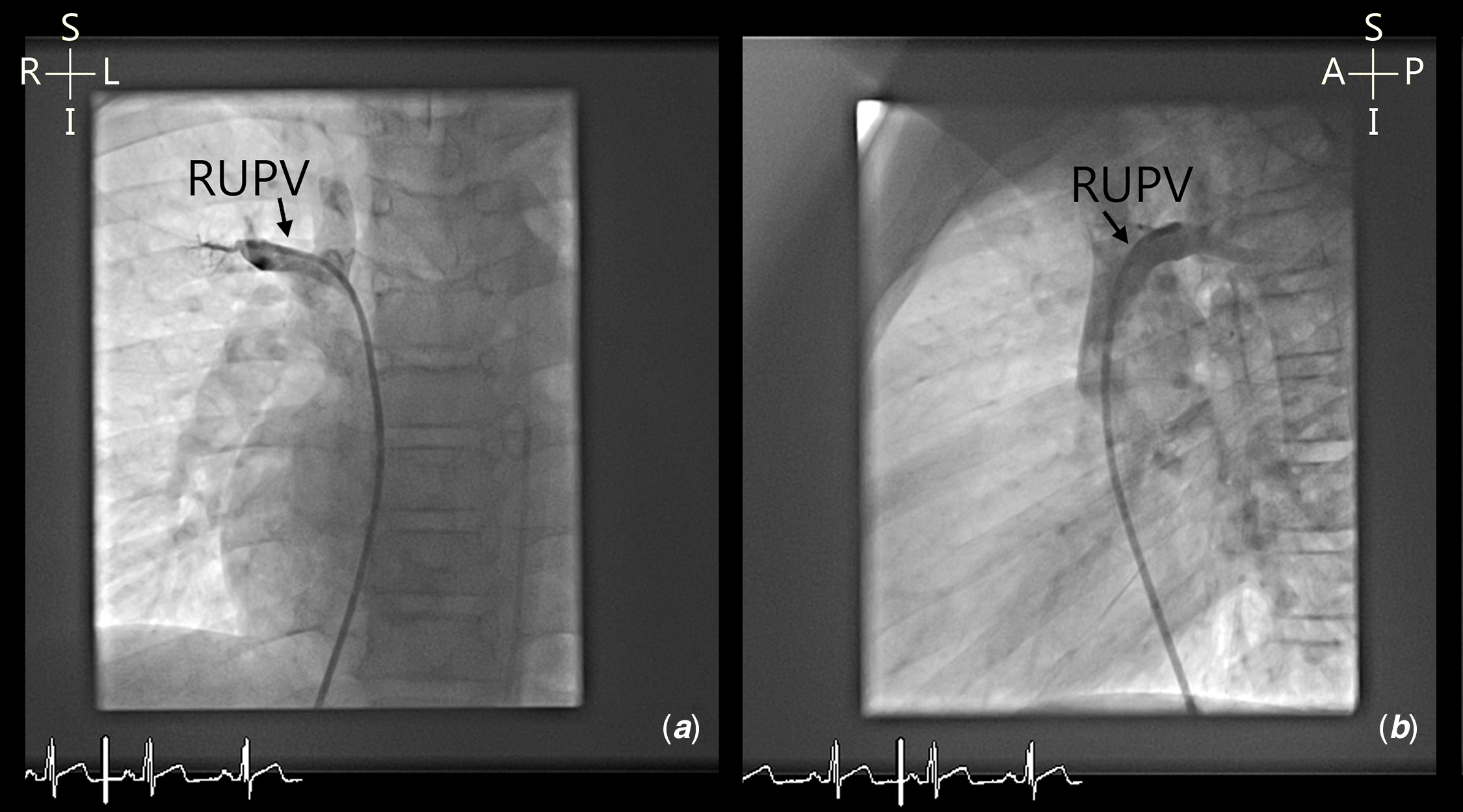
Figure 5. ( a and b ) Cardiac angiography demonstrating high insertion of right upper pulmonary vein (RUPV) into right superior caval vein.
Surgical management
The median age at the time of surgery was 5.2 years (range 1.6−15.8 years) and median weight was 21.7 kg (range 10.7−88 kg). Thirty-one patients underwent a double patch repair, four patients underwent a Warden repair, and two patients underwent a single-patch repair. Of the four patients who underwent a Warden repair, two of these four patients had a high insertion of right-sided anomalous pulmonary vein into the superior caval vein, one of these four patients had bilateral superior caval veins with relative hypoplastic right superior caval vein, and one patient had drainage of the right lower pulmonary vein to the right atrial and superior caval vein junction.
Follow-up
The median range of follow-up was 3.2 years (6 days–11.4 years). There was no mortality, reoperation, residual shunt, or pulmonary venous obstruction reported. One patient developed moderate degree of obstruction at the superior caval vein and right atrial junction at 8 months post-operatively; he subsequently underwent successful balloon dilatation to relieve the obstruction. One patient developed atrial flutter 2 months post-operatively and required cardioversion with restoration of sinus rhythm. No patient developed sinus node dysfunction.
Discussion
This study describes a heterogeneous group of children with sinus venosus defects, the majority of them were asymptomatic at presentation. The diagnostic sensitivity for sinus venosus defects was 86% (32 of 37) using transthoracic echocardiographic imaging including modified subcostal bicaval views. Transoesophageal echocardiography imaging was helpful in establishing the presence of sinus venosus defect in an additional three patients, increasing the total diagnostic yield of the echocardiographic examination from 86 to 94.5%. Transoesophageal echocardiographic imaging is proven to be a reliable supplementary diagnostic modality particularly in the subgroup of patients who are obese or in the older patients, in whom a subcostal approach frequently provides images of a poor quality. Reference Oliver, Gallego, Gonzalez, Dominguez, Aroca and Mesa19,Reference Gnanapragasam, Houston, Northridge, Jamieson and Pollock20
This study highlighted a variation in preference for modality of the complementary imaging to aid confirmation of the diagnosis of sinus node defects, which is at the discretion of the attending paediatric cardiologist. With evolution in advanced cardiac imaging modalities, cardiac MRI and cardiac computer tomographic angiogram are increasingly used to aid diagnosis. Diagnostic cardiac catheterisation is rarely used nowadays to avoid radiation exposure. Reference Freed, Nadas, Norwood and Castaneda11,Reference Valente, Sena, Powell, Del Nido and Geva22–Reference Vyas, Greenberg and Krishnamurthy24
This study shows that the variation of the anomalous right pulmonary venous connections remains a diagnostic challenge. From this retrospective study and in the previous studies, Reference Valente, Sena, Powell, Del Nido and Geva22–Reference Vyas, Greenberg and Krishnamurthy24 MRI (Fig 6) and CT imaging appear to be superior amongst imaging modalities in accurately delineating the anomalous pulmonary venous drainage, although the individual cardiologist’s preference may vary between these modalities.

Figure 6. ( a and b ) Magnetic resonance angiography highlighting drainage of the right upper (RUPV) and right middle (RMPV) pulmonary veins draining into the right superior caval vein. RA=right atrium; LA=left atrium.
The surgical techniques used in our cohort of patients included a single-patch repair, double repair, and the Warden repair. The double patch repair was the dominant procedure performed. This is dependent on the complexity of the anatomy, anomalous pulmonary venous connections, and the surgeon’s preference. A meta-analysis published by Okonta and Tamatey Reference Okonta and Tamatey45 looking at ten previous publications comparing the outcome of double- or single-patch repair reported that the adoption of double patch repair or the use of transcaval repair technique in single-patch repair was associated with a lower risk of venous obstruction. One patient (1/31 or 3%) from the double patch repair cohort from our study developed an obstruction at the superior caval vein and right atrial junction at 8 months post-operatively. He underwent successful balloon dilatation to relieve the obstruction subsequently. The incidence of superior caval vein obstruction in this study is comparable Reference Said, Burkhart and Schaff46 or lower when compared to previous studies. Reference Stewart, Bailliard, Kelle, Backer, Young and Mavroudis34,Reference Iyer, Somanrema, Pathak, Manjunath, Pradhan and Krishnan47 Post-operative sinus node dysfunction is more common in patients with single-patch or two-patch repair. Reference Stewart, Bailliard, Kelle, Backer, Young and Mavroudis34,Reference Warden, Gustafson, Tarnay and Neal36,Reference Hofmann, Dave, Schmiady and Hübler41,Reference Iyer, Somanrema, Pathak, Manjunath, Pradhan and Krishnan47,Reference Attenhofer Jost, Connolly and Danielson48 In this study, no patient developed sinus node dysfunction. Potential mechanisms causing sinus node dysfunction may include an anatomic anomaly of the sinus node and surgical trauma to the sinus node or to its blood supply. Reference Attenhofer Jost, Connolly and Danielson48,Reference Arensman, Boineau, Balfour, Flannery and Moore49 Atrial arrhythmia is commonly reported both early and late after closure of these interatrial communications. Reference Stewart, Bailliard, Kelle, Backer, Young and Mavroudis34,Reference Iyer, Somanrema, Pathak, Manjunath, Pradhan and Krishnan47,Reference Attenhofer Jost, Connolly and Danielson48,Reference Murphy, Gersh and McGoon50,Reference Meijboom, Hess and Szatmari51 One patient in this cohort developed late onset atrial flutter that responded to cardioversion. Potential mechanisms for atrial arrhythmia in these patients may include sinus node dysfunction with bradycardia-dependent atrial arrhythmias, scar-dependent multiple re-entries, and increased atrial size.
Although the surgical repair of this defect remains the gold standard, in recent years transcatheter closure has become an option in a select group of patients. In 2014, Garg et al. Reference Garg, Tyagi and Radha26 reported a transcatheter closure of sinus venosus defect in a patient with bilateral superior caval veins, using a covered stent in the superior caval vein to close the defect and redirect the right upper pulmonary vein flow around the stent into the left atrium. With meticulous pre-procedural planning using balloon interrogation, Reference Garg, Tyagi and Radha26–Reference Abdullah, Alsalkhi and Khalid28 three-dimensional printed models, Reference Velasco Forte, Byrne and Valverde25,Reference Riahi, Velasco Forte and Byrne29,Reference Hansen, Duong and Jivanji30 image fusion guidance Reference Thakkar, Chinnadurai, Breinholt and Lin31 or even holographic augmented reality, Reference Butera, Sturla, Pluchinotta, Caimi and Carminati32 these initial reports have demonstrated the feasibility and safety of transcatheter closure of sinus venosus defect in these patients in short to medium term (Fig 7). The transcatheter approach however may not be suitable in patients with right upper pulmonary vein that connects to high right superior caval vein or a relatively hypoplastic right superior caval vein especially in the presence of bilateral superior caval veins due to the risk of pulmonary venous obstruction by the covered stent. Reference Riahi, Velasco Forte and Byrne29
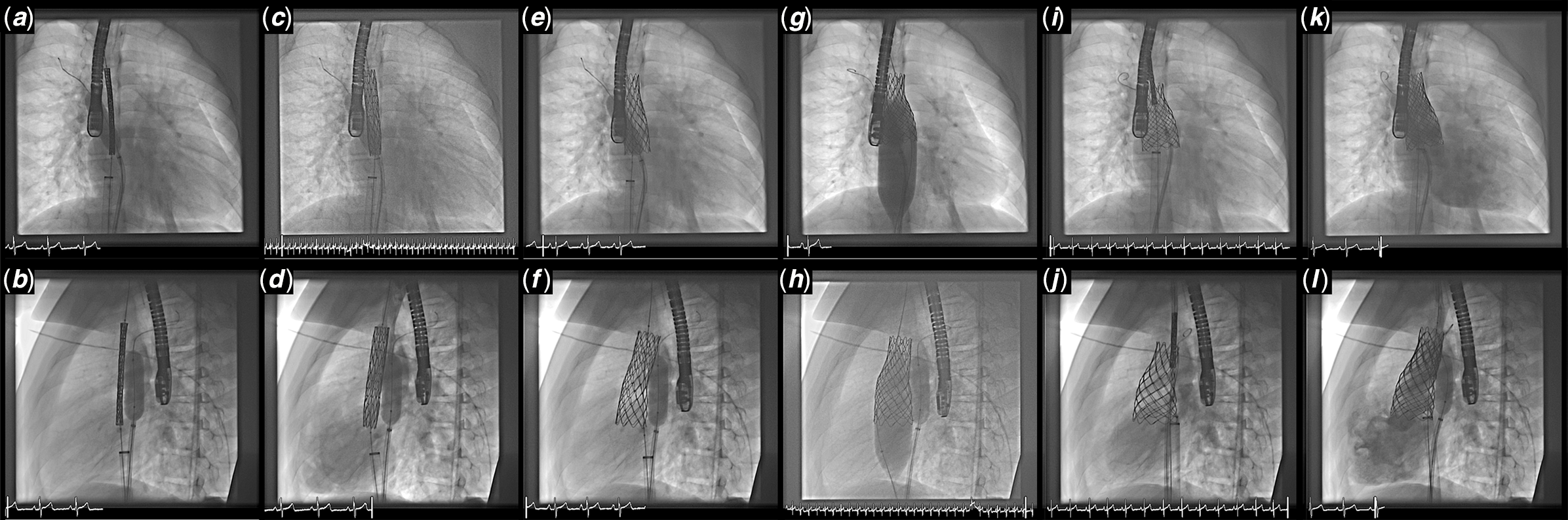
Figure 7. This series of angiography images show the steps in using a covered stent to repair a sinus venosus defect. ( a and b ) Anteroposterior (AP) and lateral views of a un-expanded 7 cm long 10-Zig covered CP stent mounted on a 28 mm BIB and introduced on a veno-venous guide wire rail and a separate pulmonary vein protection balloon (14 mm Atlas Gold balloon); ( c and d ) The inner balloon of a 28 mm 8 cm long BIB is expanded and the position adjusted on TOE imaging to overlap the crest of atrial septum; ( e and f ) The stent is further expanded by inflating the outer balloon; ( g and h ) Further flaring of the lower half of the stent is performed until the stent abuts the septum and there is no or minimal residual shunt on TOE. (h and i) An un-expanded bare-metal anchor stent and (k and l) post-expanded bare-metal anchor stent is the place to secure the flared conical Covered CP stent. The pulmonary vein is protected throughout by keeping the high pressure balloon inflated inside the pulmonary vein whenever the covered stent is dilated.
Conclusion
Complementary imaging modalities to transthoracic echocardiography are often required to delineate the exact pulmonary venous patterns in patients with sinus venosus defect. The pattern of anomalous pulmonary venous connection may be highly variable and complex in up to 14% of patients, including high insertion points and multiple drainage sites. Despite this, surgical treatment is associated with an excellent outcome and minimal complications. With progressive evolution in congenital cardiac catheterisation, a move to transcatheter closure has been shown to be suitable in select cases.
Acknowledgements
We are grateful to Ms. Ruth Brennan for assistance in formatting the manuscript and Mr. Andrew Pendred for assistance in providing the images.
Financial support
None.
Conflict of interest
None.
Ethical approval
This work complies with the ethical standards of the relevant national guidelines and with the Helsinki Declaration of 1975, as revised in 2008 and was approved by the Ethics committee at CHI Crumlin, Dublin, Ireland.











