Introduction
Coercion in psychiatry is a widely discussed and controversial issue. In fact, although coercive measures are justified by the need to preserve the patient’s health and safety and to protect others from their potentially harmful behaviors [Reference Szmukler and Appelbaum1], their use is in strong opposition to the principle of patient’s autonomy and self-determination also defended by the UN Convention on the Rights of Persons with Disabilities [2]. Furthermore, despite the increasing political and ethical attention to patients’ human rights and the scarce evidence of coercion’s benefits [Reference Luciano, Sampogna, Del Vecchio, Pingani, Palumbo and De Rosa3], its use is increasing almost everywhere [Reference de Stefano and Ducci4–Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster6] with great variations among countries [Reference Salize and Dressing7,Reference Riecher-Rossler and Rossler8]. A recent study compared the annual incidence of involuntary hospitalization for 22 countries across Europe, Australia, and New Zealand between 2008 and 2017 showing that time trends in annual rates raised in 11 out of 18 countries [Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster6]. Moreover, Rains et al. [6] found that incidences varied strikingly, ranging from 282 per 100,000 inhabitants in Austria to 14.5 per 100,000 inhabitants in Italy. Higher annual incidence rates were associated with lower absolute poverty, higher gross domestic product and per capita healthcare expenditure, larger proportion of foreign-born individuals and higher number of psychiatric beds [Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster6].
In previous studies, other area- and system-related characteristics have been associated with an increased risk of involuntary hospitalization. Rates of compulsory admission were higher in socioeconomically deprived and densely populated urban areas with higher proportions of young adults and ethnic minorities [Reference Weich, McBride, Twigg, Duncan, Keown and Crepaz-Keay9–Reference Bindman, Tighe, Thornicroft and Leese12]. In addition, several aspects of the referral process, such as being referred outside regular service hours [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Hoffmann, Haussleiter, Illes, Jendreyschak, Diehl and Emons14], by a general hospital [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Silva, Golay and Morandi15], a general practitioner [Reference Silva, Golay and Morandi15,Reference Eytan, Chatton, Safran and Khazaal16], or someone who does not know the patient [Reference Hustoft, Larsen, Auestad, Joa, Johannessen and Ruud17], and having a contact with the police at the time of admission [Reference Hustoft, Larsen, Auestad, Joa, Johannessen and Ruud17], were identified as predictors of involuntary hospitalization.
However, the most robust results point to the patient’s clinical profile as key determinant. People affected by schizophrenic, bipolar, or organic mental disorders, with poor insight, low treatment adherence, high level of psychotic symptoms and aggressiveness, and a history of previous involuntary treatment were more likely to be detained [Reference Luciano, Sampogna, Del Vecchio, Pingani, Palumbo and De Rosa3,Reference Donisi, Tedeschi, Salazzari and Amaddeo11,Reference Hoffmann, Haussleiter, Illes, Jendreyschak, Diehl and Emons14–Reference Kelly, Clarke, Browne, McTigue, Kamali and Gervin35]. On the contrary, affective disorders, anxiety disorders, and substance-related disorders were associated with a lower risk of coercion [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Silva, Golay and Morandi15,Reference Hotzy, Hengartner, Hoff, Jaeger and Theodoridou19,Reference Myklebust, Sorgaard, Rotvold and Wynn27,Reference Preti, Rucci, Santone, Picardi, Miglio and Bracco29,Reference Cougnard, Kalmi, Desage, Misdrahi, Abalan and Brun-Rousseau30,Reference Kalisova, Raboch, Nawka, Sampogna, Cihal and Kallert32]. Recently, a meta-analysis confirmed that previous involuntary hospitalization and diagnosis of psychotic disorders were associated with the greatest risk of involuntary psychiatric admission [Reference Walker, Mackay, Barnett, Sheridan Rains, Leverton and Dalton-Locke36].
Among socio-demographic characteristics, being a young man, homeless, unemployed, with a migration background, and a low educational level were identified as being associated with involuntary admission [Reference Luciano, Sampogna, Del Vecchio, Pingani, Palumbo and De Rosa3,Reference Weich, McBride, Twigg, Duncan, Keown and Crepaz-Keay9,Reference Donisi, Tedeschi, Salazzari and Amaddeo11,Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Hoffmann, Haussleiter, Illes, Jendreyschak, Diehl and Emons14,Reference Luo, Chen, Zhong, Guo, Li and Cai18,Reference Hotzy, Hengartner, Hoff, Jaeger and Theodoridou19,Reference Feeney, Umama-Agada, Gilhooley, Asghar and Kelly22,Reference Myklebust, Sorgaard and Wynn26,Reference Lay, Nordt and Rossler28,Reference Cougnard, Kalmi, Desage, Misdrahi, Abalan and Brun-Rousseau30,Reference Crisanti and Love31,Reference Thomsen, Starkopf, Hastrup, Andersen, Nordentoft and Benros33]. However, these findings are less consistent, with several studies showing the opposite [Reference Eytan, Chatton, Safran and Khazaal16,Reference Singh, Burns, Tyrer, Islam, Parsons and Crawford25,Reference Juckel and Haussleiter37] or finding no association [Reference Silva, Golay and Morandi15,Reference Canova Mosele, Chervenski Figueira, Antonio Bertuol Filho, Ferreira de Lima and Calegaro20,Reference Myklebust, Sorgaard, Rotvold and Wynn27,Reference Kalisova, Raboch, Nawka, Sampogna, Cihal and Kallert32,Reference Ng and Kelly38].
Most of the above mentioned studies aimed at identifying predictors of involuntary hospitalization using traditional statistical methods, mainly regression models [Reference Donisi, Tedeschi, Salazzari and Amaddeo11,Reference Silva, Golay and Morandi15–Reference Luo, Chen, Zhong, Guo, Li and Cai18,Reference Canova Mosele, Chervenski Figueira, Antonio Bertuol Filho, Ferreira de Lima and Calegaro20,Reference Di Lorenzo, Vecchi, Artoni, Mongelli and Ferri21,Reference van der Post, Peen and Dekker24–Reference Myklebust, Sorgaard, Rotvold and Wynn27,Reference Preti, Rucci, Santone, Picardi, Miglio and Bracco29–Reference Crisanti and Love31,Reference Ng and Kelly38], which made the statistical interaction between risk factors difficult to model and interpret [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Lemon, Roy, Clark, Friedmann and Rakowski39,Reference Lewis40]. Machine learning (ML) may overcome this limitation. ML algorithms are “trained” to find patterns in large amounts of data in order to make predictions based on new data and reveal previously “unseen” nonlinear interactions between variables [Reference Günther, Kirchebner and Lau41,Reference Chekroud, Bondar, Delgadillo, Doherty, Wasil and Fokkema42]. A recent German study used a decision-tree-generating algorithm (CHAID Chi-Square Automatic Interaction Detector), to detect risk factors for involuntary admission on a weighted sample of 10,171 inpatients [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13]. Beside main diagnosis, this study identified several modifiable predictors of involuntary hospitalization, such as the absence of outpatient treatment prior to admission or admission outside of regular service hours. Consequently, several preventive measures were suggested to address these factors and reduce the rate of involuntary inpatient treatment [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13]. In 2020, Karash et al. [Reference Karasch, Schmitz-Buhl, Mennicken, Zielasek and Gouzoulis-Mayfrank43] improved this first predictive decision tree model by optimizing ML techniques and broadening the dataset to include environmental socioeconomic data. Three main subgroups of patients were identified as at highest risk of involuntary admission: (a) patients with an organic mental disorder, retired, admitted outside of regular service hours, and living in assisted housing; (b) patients with suicidal tendencies but no affective disorder, with unclear previous suicide attempts, or living in areas with high unemployment rates; and (c) psychotic patients, living in densely built areas with a large proportion of small or one-person households [Reference Karasch, Schmitz-Buhl, Mennicken, Zielasek and Gouzoulis-Mayfrank43]. ML algorithms were also employed by Günther et al. [Reference Günther, Kirchebner and Lau41] to predict the use of coercive measures (seclusion, restraint, and involuntary medication) in a sample of 370 forensic offender patients with schizophrenia. Overall, 10 factors out of a set of 569 potential variables were identified as best predictors of coercion with a balanced accuracy of 73.3%. Previously, another Swiss study on 393 hospitalized patients had also shown that ML was useful in predicting coercion, reaching results comparable to binary logistic regression but with better generalizability [Reference Hotzy, Theodoridou, Hoff, Schneeberger, Seifritz and Olbrich44]. Further studies were recommended by the authors to evaluate the potential of these methods on larger samples.
The purpose of this study was to use ML models to identify which characteristics predicted the use of compulsory admission on a large sample of psychiatric patients (N = 25,584).
Methods
Study setting
This study was set in the canton of Vaud (794,384 inhabitants in 2017), a mixed urban–rural region of Western Switzerland. The canton is divided into four psychiatric districts, each one served by a psychiatric hospital. In 2015, the four psychiatric hospitals provided a total of 0.6 psychiatric beds per 1,000 inhabitants [Reference Silva, Golay and Morandi15], below the total number for Switzerland (0.9/1,000 inhabitants) and for Europe (0.7/1,000 inhabitants) [45,46]. On the contrary, according to data from the Swiss Health Observatory, in 2016 the canton of Vaud registered the highest rate of involuntary admissions in Switzerland (2.3 per 1,000 inhabitants), well above the national average (1.6 per 1,000 inhabitants) [47,Reference Schuler, Tuch and Peter48] and among the highest in Europe [Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster6].
Involuntary admissions in Switzerland are regulated at federal level by the Article 426 of the Swiss Civil Code (CC) which states that “a person suffering from a mental disorder or mental disability or serious neglect (the patient) may be committed to an appropriate institution if the required treatment or care cannot be provided otherwise.”
Therefore, need for treatment is the legal requirement for involuntary admission. Lack of capacity to consent to treatment or the fact of posing an imminent danger to oneself or others are not required to decide on an involuntary hospitalization. However, danger to oneself or others is the prerequisite to detain a person suffering from a mental disorder who has voluntarily entered an institution and wishes to leave (Art. 427 CC). In this particular case, detention may last a maximum of 3 days, at the end of which the patient may leave the institution, unless a compulsory admission is ordered.
The federal law is then executed at cantonal level, with important regional differences. In the canton of Vaud, only the Adult Protection Authority (APA) and medical doctors designated by the Department of Health and Social Action, namely general practitioners, psychiatrists, pediatricians, and on-call doctors, are allowed to order an involuntary admission [49]. APA orders have no time limit, but a mandatory revaluation after 6 months, 12 months, and then every year. Instead, involuntary admissions ordered by medical doctors cannot exceed 6 weeks, unless the APA issues an extension order.
Study design
This study retrospectively analyzed the routinely collected data of all psychiatric admissions that occurred between January 1, 2013 and December 31, 2017 in the four psychiatric hospitals of the canton of Vaud, Switzerland. Available data included socio-demographic characteristics, like gender, age, marital status, and nationality. Several clinical characteristics were also available, as primary diagnosis, aggregated into 10 main categories based on the ICD-10 system, a secondary diagnosis of addiction and/or personality disorders, and the 12 item-level scores of the Health of the Nations Outcome Scale (HoNOS) [Reference Lauzon, Corbière, Bonin, Bonsack, Lesage and Ricard50,Reference Golay, Basterrechea, Conus and Bonsack51], which measure the patients’ mental and social functioning. Within the four hospitals, an additional observer-rated item on psychotropic medication compliance is also routinely assessed. This was also included in the analyses. Finally, we took into account the available information on the referral process, such as who referred the patient, to which hospital, the legal status of the hospitalization (voluntary or involuntary) and whether they were admitted during regular service hours (Monday/Friday from 8:00 a.m. to 18:00 p.m.) or outside regular service hours (Monday/Friday from 18:00 p.m. to 8:00 a.m., weekends and public holidays).
All data were anonymized and the Human Research Ethics Committee of the Canton Vaud (protocol #2016–00768) granted approval for this study.
Statistical analysis
The included sample (N = 25,584) was split into two subgroups based on legal status of the hospitalization (voluntary hospitalization [VH; n = 15,797] vs. involuntary hospitalization [IH; n = 9,787]) and compared on all the available characteristics. Categorical variables were tested using Pearson’s Chi-square tests. Ordinal and continuous variables were analyzed through nonparametric Mann–Whitney U tests. All statistical tests were two-tailed. Because of the large sample size, significance level was set at p < .01 and effect sizes according to Cohen [Reference Cohen52] were calculated.
In order to identify the main predictors of involuntary hospitalization, we used two ML algorithms, Classification and Regression Tree (CART) [Reference Breiman, Friedman, Olshen and Stone53] and Random Forests (RFs) [Reference Breiman54], on observations with no missing data (N = 14,948; 63.3% VH vs. 36.7% IH). Moreover, we used ordinary logistic regression to compare its predictive power with that obtained through CART and RFs.
First developed by Breiman et al. [Reference Breiman, Friedman, Olshen and Stone53], CART is a flexible tool used to discover hierarchical and complex associations among variables. It is a nonparametric methodology, thus no assumptions are made on the distribution of the predicting variables and it can handle any type of data, numerical as well as categorical. Moreover, compared to traditional statistical methods, CART presents several advantages: (1) the best “splitting” variables are identified automatically at each step of the tree by searching among all available features; (b) it can easily deal with missing data; (c) it is relatively easy to perform, requiring little input from the user; and (d) its results are generally simple for clinicians to interpret [Reference Lewis40]. CART presents a major improvement compared to previous tree-based algorithms, such as Automatic Interaction Detection (AID) and Chi-square Automatic Interaction Detector (CHAID). In CART, the tree can grow until further split is not possible due to the stop criteria, which can be defined a priori. For reasons of parsimony and generalization, we can also remove irrelevant branches by “pruning” in order to find the best potential CART [Reference Steinberg and Colla55].
RFs are a generalization of CART, in which a large number of trees are fitted on resampled versions of the original data and each single CART contributes to the final prediction by choosing the most important predictor.
Our predicted outcome was voluntary/involuntary hospitalization (VH vs. IH). IH was defined as the positive class and VH as the negative one. Socio-demographic, clinical, and procedural characteristics were the predictive variables (23 features; Table 1).
Table 1. Socio-demographic, clinical, and referral process characteristics: subgroups comparisons (N = 25,584).

Note: Effect size: Δsmall effect; ΔΔsmall to medium effect; and ΔΔΔmedium effect.
HoNOS, Health of the Nations Outcome Scale; VH, voluntary hospitalisation; IH, involuntary hospitalization; IQR, interquartile range; Mdn, median; SD, standard deviation.
a Mann–Whitney U test.
b Pearson’s Chi-square.
The three models were first fitted on the 70% of observations chosen randomly from the completely observed sample (training subsample; n = 10,464), and their predictive power was tested on the remaining 30% (test subsample; n = 4,484). For more details on the characteristics of training and test subsamples, please see the accompanying Supplementary Material. Default hyperparameters were used (maximum depth of the model = 30, minimum number of observations per node = 20, complexity parameter (cp) = 0.01, and number of models for RFs = 100). At each node, the split was performed on the variable with the lowest Gini index. Beside predictive accuracy, balanced accuracy and validity area under curve (AUC), other performance statistics were calculated: sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
Due to the large proportion of missing information, which varied between 0 and 23% depending on the variable, and in order to verify the robustness of our results, we performed sensitivity analyses. Missing data were imputed through multiple imputation using chain equations [Reference Sv and Groothuis-Oudshoorn56]. CART and RFs were retested on the imputed data (N = 25,584).
All statistical analyses were performed using IBM SPSS 26 and R 4.0.1 (mice, stat, rpart, and randomForest libraries).
Results
Between January 1, 2013 and December 31, 2017, 25,790 hospitalizations were registered within the four hospitals. Two hundred and six cases were excluded from the analyses since the legal status of the hospitalization was unknown. Of the included 25,584 hospitalizations, 61.7% were voluntary and 38.3% involuntary. The total sample was composed of 51% women, with an average age of 45 years, single (50%), of Swiss nationality (66%) and with a primary diagnosis of schizophrenic (F20–F29; 24%) or depressive disorders (F32–F39; 19%).
Socio-demographic, clinical, and referral process characteristics: subgroups comparisons
The associations between legal status of the hospitalization and the socio-demographic, clinical and referral process characteristics are presented in Table 1. Globally, the two subgroups differed significantly on all the characteristics with the exclusion of sex, nationality, and secondary diagnosis of addiction. However, only five variables reached an effect size of 0.2 (small to medium effect) and only one exceeded the threshold of 0.3 (medium effect). Indeed, the IH group showed a considerably higher percentage of people affected by organic mental disorders (F00–F09) (χ 2(1) = 1259.9; p < 0.001). Moreover, involuntary patients scored higher on four HoNOS items: overactive, aggressive, disruptive, or agitated behavior (U = 38316000.5; z = −48.5; p < 0.001), cognitive problems (U = 40715055.0; z = −31.5; p < 0.001), problems associated with hallucinations and delusions (U = 41784750.5; z = −35.8; p < 0.001), and the problems with psychotropic medication compliance additional item (U = 34761181.5; z = −32.4; p < 0.001). Finally, a remarkably higher percentage of voluntary patients auto-referred themselves to the hospital (χ 2(1) = 1663.5; p < 0.001).
Predicting factors of involuntary hospitalization
The original data contained a large number of missing values, and only 58% (14,948 out of 25,584) of the observations were complete.
Table 2 shows the predictive statistics produced for the three models on the completely observed test subsample (n = 4,484). The three methods achieved very similar results, with RFs and logistic regression showing slightly better performances compared to CART. Predictive balanced accuracy ranged from 68% for CART to 72% for logistic regression. The three models showed better specificity then sensitivity. Indeed, on the test subsample they were able to correctly classify between 81 and 86% of actual cases of voluntary hospitalization and between 54 and 58% of actual cases of involuntary hospitalization.
Table 2. Comparison of models’ validity.

Note: AUC, Area Under Curve; PPV, Positive Predictive Value; NPV, Negative Predictive Value.
When we fitted a CART on the training subsample (n = 10,464), the resulting tree showed that only three parameters were essential to estimate the probability of being involuntarily admitted to hospital: the HoNOS score on the “Overactive, aggressive, disruptive or agitated behavior” item, who referred the patient to hospital and primary diagnosis (Figure 1).

Figure 1. Classification and Regression Tree to predict involuntary hospitalizations on 70% of observations chosen randomly from completely observed sample (N = 10,464).
Note: VH, voluntary hospitalization; IH, involuntary hospitalization. HoNOS scores: 0 = no problem; 1 = minor problem requiring no action; 2 = mild problem but definitely present; 3 = moderately severe problem; 4 = severe to very severe problem. Referral from: 1 = Patient; 2 = Family/relatives; 3 = General practitioner; 4 = General hospital; 5 = Outpatient psychiatrist; 6 = Psychiatric hospital; 7 = Civil justice/other justice authority; 8 = Other. Primary diagnosis: 1 = F00–F09; 2 = F10; 3 = F11–F19; 4 = F20–F29; 5 = F30–F31; 6 = F32–F39; 7 = F40–F48; 8 = F60–F69; 9 = Other mental disorders; 10 = Other non-mental disorders.
The likelihood of coercion was higher for people with moderate to very severe aggressive behaviors (65%), especially if not auto-referred to hospital (68%). This percentage dropped to 21% when they referred themselves.
Among people showing none up to mild aggressiveness, there was a higher risk of involuntary admission if they were referred to hospital by a general practitioner, a general hospital, a psychiatric hospital or the civil justice (46%). A further increase was recorded if patients were affected by organic disorders (F00–F09), disorders due to alcohol use (F10), schizophrenia (F20–F29), and other non-mental disorders (58%). On the contrary, the odds of being involuntarily hospitalized decreased when the HoNOS score for aggressive behavior was lower than 3 (30%), and the patients referred themselves, or were referred by a family member/relative, an outpatient psychiatrist or others (20%).
When RFs were fitted on the training subsample, the importance of each predictor was estimated based on its mean decrease in accuracy and its mean decrease in Gini coefficients (Figure 2). Based on these results, four factors emerged as the most important in both classifications: who referred the patient, the HoNOS score for “overactive, aggressive, disruptive, or agitated behavior,” primary diagnosis and age. The exclusion of one of these four variables would reduce either the accuracy of the model or its homogeneity.

Figure 2. Mean decrease in accuracy and mean decrease in Gini coefficients (sorted decreasingly) in Random Forests model.
Finally, of the 23 factors included in the logistic regression model, 15 were found to affect significantly the likelihood of being coerced to hospital (Table 3). However, in order to calculate the probability of an individual belonging to the IH group using this model, all the 23 characteristics must be available.
Table 3. Predictors of involuntary hospitalization: logistic regression analysis on 70% of observations chosen randomly from completely observed sample (N = 10,464).
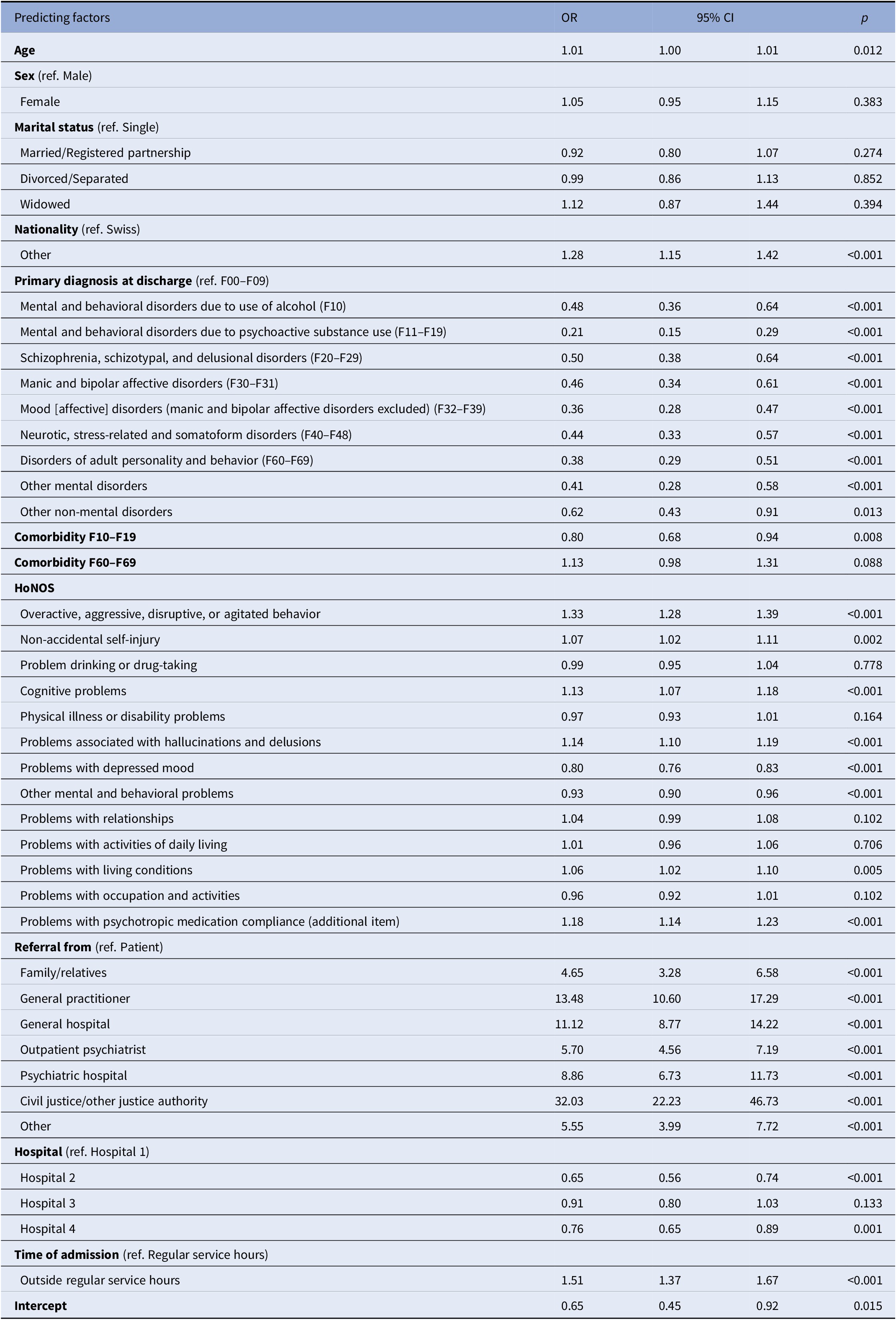
Note: OR, Odds Ratio; CI, Confidence Interval.
Sensitivity analyses
Due to the large proportion of missing information and in order to test the robustness of our results, we fitted both CART and RFs on 100 copies of data completed via multiple imputation. For CART the predictive accuracy on all scenarios ranged from 70 to 72%. The same CART shown in Figure 1 was obtained in 96 out of 100 replications of data completed via multiple imputation. For RFs the predictive accuracy for the 100 multiple imputation data versions varied between 73 and 75%.
Discussion
The main aim of this study was to identify predicting factors of involuntary hospitalization using ML models. For this purpose, we analyzed our data using CART and RFs, and compared their predictive power with traditional logistic regression.
Our results showed that the performances of the three methods were very similar. CART showed the lowest predictive balanced accuracy (68%) but the most parsimonious model, allowing to estimate the probability of being involuntarily admitted to hospital with only three checks (aggressive behaviors, who referred the patient to hospital and primary diagnosis). Thanks to his binary structure, CART provided a prompt view of the most relevant predictors of involuntary admission and of their non-linear interactions. RFs and logistic regression achieved slightly higher results (71 and 72%), but at the cost of an increased complexity and a depleted practical feasibility of their models. In RFs, the mean decrease in accuracy and the mean decrease in Gini coefficients provided information about the importance of each variable and its impact on the accuracy and homogeneity of the model. However, nothing can be disclosed on how these factors interacted and affected each other. Logistic regression also made statistical interplay between risk factors difficult to model and interpret [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Lemon, Roy, Clark, Friedmann and Rakowski39,Reference Lewis40]. Moreover, more than 20 parameters had to be taken into account in order to estimate the probability of an individual to belong to the IH group.
The three models showed a greater ability to correctly classify real cases of voluntary hospitalization than to detect real cases of involuntary hospitalization. This result calls into question their actual use in real life and what margin of error should be considered ethically acceptable when dealing with a topic as sensitive as the use of coercion. Further research is mandatory to improve the sensitivity of the models.
The CART identified aggressive behaviors as the strongest predictor of coercion. People with moderate to very severe level of aggressiveness, especially if not auto-referred, showed the highest risk of involuntary hospitalization. Interestingly, the few aggressive patients who referred themselves had a low probability of compulsory admission. This suggests that, beside aggressiveness and agitation, uncooperativeness played a key role during the hospitalization process. RFs and logistic regression also identified aggression as one of the most important factors. Considering that in Switzerland dangerousness is not a prerequisite for involuntary admission but is only required to keep in hospital a voluntarily admitted person who wants to leave the institution, this finding cannot be considered as a mere consequence of the legal requirements in force. Several previous studies have already highlighted the key role of aggressive behaviors as a risk factor of coercion [Reference Silva, Golay and Morandi15,Reference Hustoft, Larsen, Auestad, Joa, Johannessen and Ruud17,Reference Luo, Chen, Zhong, Guo, Li and Cai18,Reference Canova Mosele, Chervenski Figueira, Antonio Bertuol Filho, Ferreira de Lima and Calegaro20,Reference Di Lorenzo, Vecchi, Artoni, Mongelli and Ferri21,Reference de Jong, Oorschot, Kamperman, Brussaard, Knijff and van de Sande23,Reference Kalisova, Raboch, Nawka, Sampogna, Cihal and Kallert32,Reference Günther, Kirchebner and Lau41,Reference Hotzy, Theodoridou, Hoff, Schneeberger, Seifritz and Olbrich44,Reference Abderhalden, Needham, Dassen, Halfens, Fischer and Haug57]. Aggressiveness may also affect the likelihood of being involuntarily admitted because it often requires the involvement of the police, which has been found to be another important risk factor of involuntary admission [Reference Hustoft, Larsen, Auestad, Joa, Johannessen and Ruud17,Reference Canova Mosele, Chervenski Figueira, Antonio Bertuol Filho, Ferreira de Lima and Calegaro20,Reference Hotzy, Theodoridou, Hoff, Schneeberger, Seifritz and Olbrich44]. Perceived risk of danger to self or others has been found to be crucial in professionals’ decisions on involuntary admissions [Reference Wynn, Myklebust and Bratlid58,Reference Lepping, Steinert, Gebhardt and Rottgers59]. However, an accurate prediction of serious violence is very complex [Reference Feiring and Ugstad60–Reference Szmukler and Holloway62]. The use of a structured risk assessment during the admission process and the first days of treatment should be fostered [Reference Abderhalden, Needham, Dassen, Halfens, Haug and Fischer63–Reference Rotvold and Wynn65]. Furthermore, the implementation of interventions and tools able to improve patients’ empowerment and participation in decision-making during psychiatric crisis, such as Joint Crisis Plan [Reference Henderson, Swanson, Szmukler, Thornicroft and Zinkler66], should also be promoted in order to enhance cooperation, reduce the risk of aggressive behaviors and consequently reduce the use of coercion. Finally, dealing with aggression can be extremely challenging and stressful for staff [Reference Husum, Bjørngaard, Finset and Ruud67]. A large number of referring physicians felt threatened by their patients when facing psychiatric emergency situations [Reference Hotzy, Marty, Moetteli, Theodoridou, Hoff and Jaeger68]. Thus, specific training programs on communication skills, management of aggressiveness and de-escalation techniques should be provided to all professionals involved in the referral process [Reference Abderhalden, Needham, Dassen, Halfens, Haug and Fischer63,Reference Blair, Woolley, Szarek, Mucha, Dutka and Schwartz64,Reference Ulrich, Bogren, Gardiner and Lundin69–Reference Hamrin, Iennaco and Olsen71].
Indeed, referral process was identified as the second most important predictive factor in our decision tree. For people with lower levels of aggression, there was an increased risk of compulsion if they were referred to hospital by a general practitioner, a general hospital, a psychiatric hospital, or the civil justice. On the contrary, non-aggressive patients referred by themselves, by their relatives or by a psychiatrist were less likely to be involuntarily admitted regardless of diagnosis. Referral was also recognized as a strong predictor of coercion in both RFs and logistic regression. A previous study had already highlighted the association between physicians’ qualifications and coercion rates, showing that limiting the right to require involuntary admission to psychiatrists could reduce the use of compulsion [Reference Eytan, Chatton, Safran and Khazaal16]. Another study in Zurich, Switzerland, showed that referring general practitioners found it more difficult to apply legal criteria for involuntary admission and to assess its necessity [Reference Marty, Jaeger, Moetteli, Theodoridou, Seifritz and Hotzy72]. GPs also provided the lowest quality commitment certificates [Reference Kieber-Ospelt, Theodoridou, Hoff, Kawohl, Seifritz and Jaeger73,Reference Jager, Ospelt, Kawohl, Theodoridou, Rossler and Hoff74]. In Cologne, Germany, Schmitz-Buhl et al. [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13] found that the risk of involuntary treatment of patients with suicidal and self-harm behavior was higher in the two psychiatric hospitals that also showed a higher proportion of referrals from general emergency units. This result should call into question the organization of the on-call system in the canton of Vaud, which, despite the local high provision of psychiatrists (0.73/1,000 inhabitants), has been so far carried on solely by general practitioners. It is also worth to mention that psychiatric emergency services are not fully developed in the canton. More efforts should be made to enhance the psychiatric training of primary care physicians, who are often called outside regular service hours and in general emergency services to provide support and assess patients with mental health crisis.
The paramount need to develop trainings that improve the clinical knowhow and the aggressiveness management skills of all professionals involved in the admission process was also one of the recommendations that emerged from the EUNOMIA study for good clinical practice on involuntary hospitalization [Reference Fiorillo, De Rosa, Del Vecchio, Jurjanz, Schnall and Onchev75].
The last predictive factor identified by the CART was primary diagnosis. Among people with lower levels of aggressive behaviors and referred to hospital by a general practitioner, a general hospital, a psychiatric hospital or the civil justice, a higher risk for involuntary admission was registered if they were affected by organic disorders (F00–F09), disorders due to alcohol use (F10), schizophrenia (F20–F29), and other non-mental disorders. The logistic regression model upheld the strong predictive power of organic disorders, showing that they significantly increased the risk of being involuntarily admitted compared to all other diagnoses. New alternative treatments should be developed to better meet the special needs of this particular population. Indeed, several studies have already confirmed the relevance of this diagnosis as well as of the diagnosis of schizophrenia in predicting the risk of coercion [Reference Luciano, Sampogna, Del Vecchio, Pingani, Palumbo and De Rosa3,Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13–Reference Silva, Golay and Morandi15,Reference Hotzy, Hengartner, Hoff, Jaeger and Theodoridou19,Reference de Jong, Oorschot, Kamperman, Brussaard, Knijff and van de Sande23,Reference Singh, Burns, Tyrer, Islam, Parsons and Crawford25,Reference Myklebust, Sorgaard and Wynn26,Reference Lay, Nordt and Rossler28,Reference Cougnard, Kalmi, Desage, Misdrahi, Abalan and Brun-Rousseau30,Reference Thomsen, Starkopf, Hastrup, Andersen, Nordentoft and Benros33,Reference Karasch, Schmitz-Buhl, Mennicken, Zielasek and Gouzoulis-Mayfrank43,Reference Lay, Kawohl and Rossler76]. Less conclusive are instead the findings concerning disorders due to alcohol use. Some earlier studies had found that being affected by substance abuse disorders, included alcohol, increased the odds of involuntary admission [Reference Luciano, Sampogna, Del Vecchio, Pingani, Palumbo and De Rosa3,Reference Lay, Nordt and Rossler28] while others showed a diminished risk for this population [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13]. Finally, the increased risk associated with other non-mental disorders was not confirmed in the existing literature, according to which this diagnosis would have no impact on the likelihood of being involuntarily admitted [Reference Silva, Golay and Morandi15]. The heterogeneity of the diagnostic categories included in this node makes it difficult to draw conclusions on which preventive measures should be fostered for this subgroup of patients. More homogeneous and therefore more informative subgroups could be obtained by including other parameters in the model.
Even though our main findings are mainly in line with previous studies, we cannot exclude that their representativeness might be affected by specific area-related characteristics, such as the local rate of involuntary admission, the specific regulation in place and, the local mental health organization and availability. According to the Swiss Health Observatory data, in 2016 the canton of Vaud was the canton with the highest rate of involuntary hospitalization in Switzerland, followed by Zurich and Geneva [Reference Schuler, Tuch and Peter48]. With 2.3 involuntary admission per 1,000 inhabitants, the canton of Vaud also ranked above most European countries, along with Germany and Austria [Reference Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster6]. Moreover, contrary to the majority of other Swiss cantons, in the canton of Vaud only some specific categories of medical doctors (general practitioners, psychiatrists, pediatricians, and on-call doctors) are allowed to order an involuntary inpatient treatment. Furthermore, as mentioned above, lack of capacity to consent to treatment and imminent danger, which are required in most countries, are not essential in Switzerland in order to admit someone involuntarily. Finally, model results could also be affected by the important variations existing among cantons and countries in term of psychiatric beds provision and community service development. Therefore, further national and international studies are needed to confirm the generalizability of our model.
Strengths and limitations
The main strength of this study is the large sample size. Thanks to the available routinely collected data, we were able to include in the study all psychiatric admissions occurred between 2013 and 2017 in the canton of Vaud, Switzerland. The second main strength lies in the innovative methodologies deployed to analyze a large amount of data, without a priori selection of variables. The use of CART allowed us to overcome some of the main limitations of traditional statistical methods [Reference Schmitz-Buhl, Gairing, Rietz, Haussermann, Zielasek and Gouzoulis-Mayfrank13,Reference Lemon, Roy, Clark, Friedmann and Rakowski39,Reference Lewis40], providing a parsimonious and feasible hierarchical model with comparable predictive power.
Two main limitations should be reported. First, because of the retrospective nature of the study, only available routinely collected data could be included in our predictive models. Several important factors could not be taken into account. The introduction of these parameters into the models could have further improved their performances, especially their sensitivity. The second shortcoming was the large number of missing values in the original data. To overcome this limitation, sensitivity analyses were performed on 100 copies of data completed via multiple imputation. The results of both CART and RFs on the imputed data were almost identical to those obtained on the original data, confirming the robustness of our models.
Conclusion
This study confirmed the essential role of aggressiveness, referral, and diagnosis as predictors of coercion. Identifying risk factors of involuntary admission is essential in order to efficiently target the development of professional training, preventive strategies, and alternative interventions. ML methodologies offer new effective tools to achieve this goal, providing accurate yet simple models that could be used in clinical practice.
Acknowledgments
The authors would like to thank the hospitals’ management and data managers for their collaboration.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supplementary Materials
To view supplementary material for this article, please visit https://doi.org/10.1192/j.eurpsy.2021.2220.








Comments
No Comments have been published for this article.