Rates of detention in psychiatric hospital have more than doubled in England since 1983 and risen faster than almost anywhere else in Europe during the past decade.Reference Sheridan-Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster1 Detention in hospital is inherently coercive: it is experienced by most patients as such,Reference Sheehan and Burns2,Reference Akther, Molyneaux, Stuart, Johnson, Simpson and Oram3 and 3 months after detention many patients still disagree with the decision to detain them.Reference Priebe, Katsakou, Glöckner, Dembinskas, Fiorillo and Karastergiou4 Involuntary hospital admissions are typically longer and more costly than voluntary admissions. Patients experience only limited improvements in health and social circumstances following detention.Reference Priebe, Katsakou, Yeeles, Amos, Morriss and Wang5 Understanding and addressing the rising rate of detentions is therefore a priority for mental healthcare in England, which prompted the recent Independent Review of the Mental Health Act (MHA Review), which reported in December 2018.6 To support the review, an expert topic group was convened, supported by the National Institute for Health Research (NIHR) Mental Health Policy Research Unit (MHPRU). This group was tasked with exploring why rates of detentions in psychiatric hospital in England have risen since the introduction of the Mental Health Act 1983 (MHA), and most rapidly over the past decade. This work is reported here.
We sought to identify hypotheses for the rise in detentions in England, test their plausibility in relation to available evidence, and then develop an explanatory logic model for the rise in detentions in England between 1983 and 2016. The term ‘detentions’ is used here to include compulsory admissions to psychiatric hospital and detentions of people in psychiatric hospital following a voluntary admission, including civil and forensic MHA detentions, for people of all ages. We excluded uses of the MHA that direct conveyance to a place of safety or to permit short-term detention (72 h or less) for the purpose of assessment only.
Method
The study comprised: (a) generating hypotheses to explain the rising rate of detentions; (b) rapid scoping for evidence relevant to each hypothesis; (c) testing each hypothesis (in so far as data permitted) and rating its plausibility as an explanation for rising rates of detention; and (d) developing an explanatory model of the rising rate of detentions in England.
Hypothesis generation
A list of potential explanatory factors for the rising rate of detentions was generated from three sources.
(a) Reports and literature, chiefly the recent report from the Care Quality Commission7 and the evidence submitted to the MHA Review,6 which included over 50 focus groups with patients and carers, evidence submissions from over 200 mental health organisations, practitioners, patients and carers, and seven public workshops across England.
(b) Consultation with an expert topic group convened for the MHA Review. This comprised eight academics, six of whom were psychiatrists, one a social worker and one a researcher with lived experience. The group included two women and two members of Black, Asian and minority ethnic (BAME) communities, one of whom co-chaired the Mental Health Act Review African and Caribbean Group (MHARAC), which supported the MHA Review.
(c) Consultation with 14 members of the Lived Experience Working Group of the Mental Health Policy Research Unit (MHPRU), all with lived experience as a mental health patient or family carer. All members of this group were adults; the group was demographically varied with respect to age, gender and ethnicity.
Through discussion in the MHA Review topic group, all proposed explanations were considered and clarified into hypotheses where necessary, describing how proposed explanatory factors might contribute to an increase in detentions. Types of information that could support or contradict each hypothesis were agreed.
Evidence gathering
Relevant data sources were sought for variables relating to each hypothesis, with advice from academics with epidemiology, health economic and health services research expertise. We investigated the relationship of each variable to the rising rate of detentions in England through the following process.
First, an ecological study explored the associations over time between national population-level indicators for a range of explanatory variables and the rate of detentions. Where more than one relevant data source was identified for a proposed explanatory variable, the most appropriate variable was selected through discussion in the study team, with priority given to well-established measures used in previous research or national reports, and variables with the most years of data available. Annual data for all explanatory variables were collected from 1983 onwards, where available. Descriptive data from each variable were reviewed to assess whether exposure to the explanatory variable appeared to have changed over time (in the direction compatible with contributing to a rise in detentions). The association between each indicator variable and rates of involuntary hospital admission was assessed using regression analyses. Following guidance,Reference Harrell, Lee and Mark8, Reference Moons9 only indicator variables with at least 10 years of annual data were included in the analyses, to avoid reporting imprecise statistical results based on limited data. Breusch–Godfrey tests were used to identify the presence of serial correlation (in which the model residuals are correlated over time). Such correlation can be present in time series data and can result in biased estimates if inappropriate regression methods are used. When there was evidence of serial correlation, Prais–Winsten regressionReference Prais and Winsten10 was used; otherwise simple linear regression was used. Analyses were performed using Stata version 15 for Windows. The outcome variable in all analyses was annual number of detentions per 100 000 population, derived from publicly available English KP90 detentions data.11 If prevalence of exposure to an explanatory variable was unchanged or was not associated with detention rates in the expected direction, it was considered less plausible as a contributory factor for the rise in compulsory admissions.
Second, available research was scoped by MHPRU researchers (L.S.R., N.L., L.M.) for additional evidence relevant to our hypotheses, including: studies exploring predictors of detention at individual patient, local area or international level, and qualitative literature regarding perceived changes in explanatory factors over time. Relevant literature was identified through: (a) a programme of systematic reviews and data analysis conducted for the MHA Review by the MHPRU.6 These provided a range of types of evidence from quantitative and qualitative research, and included systematic reviews of social and clinical predictors of detention, interventions to reduce detention, qualitative literature on patients’ and carers’ experience of detention, an international comparison of detention rates and factors associated with detention rates, and an analysis of routine health records data regarding the nature of changes over time in patterns of detention in two London National Health Service (NHS) trusts; (b) keyword searching for relevant terms in electronic databases (MEDLINE and PsycInfo); and (c) asking subject experts in the MHA Review topic group, authors of this paper and others (acknowledged at the end of this paper) to identify other relevant literature.
Assessing the plausibility of hypotheses
Findings for each hypothesis were synthesised and summarised. The likelihood of any hypothesised or observed ecological relationship between explanatory variables and rates of detentions being causal in nature was assessed, where applicable and as far as evidence was available, with regard to established criteria for causality,Reference Hill12 including the strength and consistency of associations, their perceived plausibility as causal mechanisms and, where possible, the specificity of relationships to populations at increased risk of detention, and temporality, i.e. evidence that rises in explanatory factors preceded rises in detentions. Hypotheses were then graded by the study team for plausibility as a contributory factor to the rising rate of detentions in England: 0, contradicted by available evidence; 1, lack of evidence or available evidence is ambiguous or mixed; 2, supported by the balance of available evidence. Two factors were considered in grading each hypothesis: evidence for change over time in the direction expected; and evidence, or self-evident face validity, that the hypothesised factor was causally related to risk of detention. Ratings were made initially by the lead authors of this paper (L.S.R, B.L.-E.), then reviewed by all authors and revised if necessary following discussion.
Logic model development
Following guidance,Reference Harries, Hodgson and Noble13 we developed a visual logic model to show how plausible proposed contributory factors (i.e. hypotheses rated as 1 or 2 for plausibility) might contribute to the rising rate of detentions in England and might interrelate. In developing the model, we worked backwards from the final outcome to be explained (the rising rate of detentions) to identify proximal outcomes, mental health service activities, inputs and contextual factors. We differentiated elements of this explanatory model that were supported by available evidence from hypothesised elements with ambiguous or absent evidence. Proposed causal pathways and mechanisms of change in the rate of detentions were illustrated in the model with arrows. An initial draft of the logic model was developed by B.L.-E., informed by a preliminary draft of relevant data tables and evidence reviews (supplementary Appendices 1 and 2, available at https://doi.org/10.1192/bjo.2020.64). This was then discussed with the study co-authors and revised with feedback and reference to additional retrieved evidence in five iterative stages.
Results
Rates of detention in England
Data for the number of detentions in England were not available from NHS Digital before 1988. National detention data collection methods changed from April 2016,11 so data after this point are not comparable with previous data.
The annual rates of detentions per 100 000 population in England from 1988 to 2016 are shown in Fig. 1. Detention rates more than doubled during this period, from 52 to 114 per 100 000 population. A 1-day census of the number of people per 100 000 population detained at year-end each year also rose, from 26.0 in 1998 (the first year for which data are available) to 36.5 in 2016. The rise in the rate of detentions was steepest in the periods 1988–1996 and 2011–2016, plateauing in between. Increases in detentions were greatest at the point of admission. Overall detention rates, and detentions for assessment (section 2 of the Mental Health Act 1983, MHA), rose significantly during the study period. Rates of detention for treatment (s.3 MHA) and use of forensic detentions did not change significantly (supplementary Appendix 1). Use of legal powers by the police to bring people to a hospital-based place of safety (s.135 or s.136 MHA) for assessment – which were not included in our overall detention rate variable – also increased significantly during the study period. Individual patients are not distinguished in government KP90 detentions data, which therefore cannot distinguish to what extent the rise in detentions reflects more people being detained, or the same number of people being detained more frequently. The data also cannot identify in which clinical or demographic groups the rise in detentions occurred.

Fig. 1 Rates of involuntary detentions per 100 000 population in England 1988–2016. Inv hosp, involuntary hospital admissions; s., section of the Mental Health Act 1983; CTO, community treatment order; MHA, Mental Health Act 1983; NHS, National Health Service.
Proposed explanations for the rising rate of detentions in England
Seventeen hypotheses for the rising rate of detentions in England were generated. These are presented in the Appendix (immediately preceding the References), with a brief description of the proposed mechanisms of effect on detention rates. Consistent with previous work7 we have grouped the hypotheses as: social factors, service provision, legal factors and data recording problems.
Available data relevant to each hypothesis are summarised in Table 1, along with results of statistical tests of association with detention rate, where undertaken. Serial correlation was present for all but one indicator variable, so Prais–Winsten regressions were used. Full descriptive data and illustrative graphs showing change over time for each explanatory variable are provided in supplementary Appendix 1. Research evidence regarding the nature of the relationship of each of these factors to detention rates is summarised below and reported fully in supplementary Appendix 2.
Table 1 The relationship of potential explanatory factors to detention rates: exploration of available national data
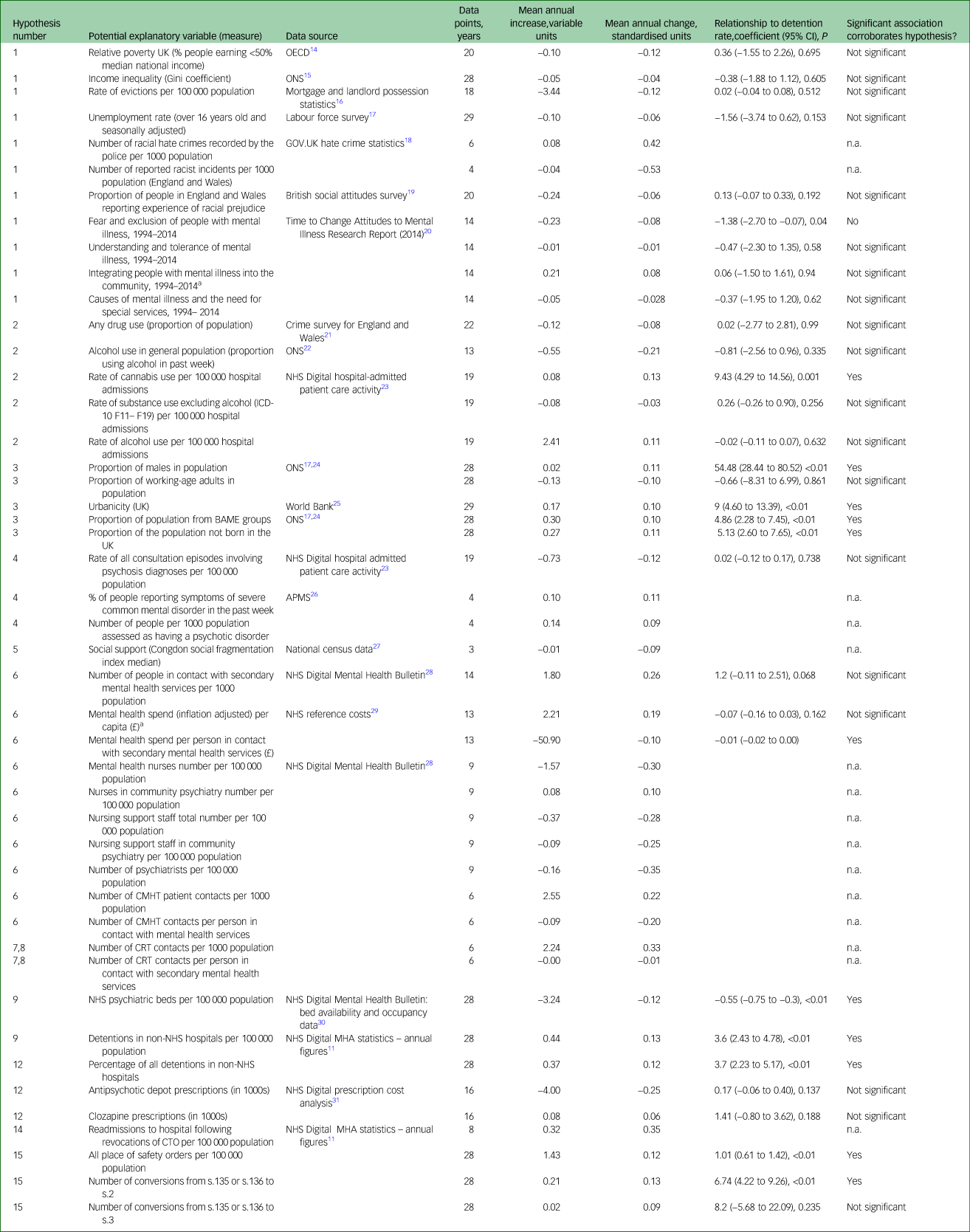
OECD, Organisation for Economic Co-operation and Development; ONS, Office for National Statistics; n.a., not applicable; BAME, Black, Asian and minority ethnic; APMS, Adult Psychiatric Morbidity Survey; NHS, National Health Service; CMHT, community mental health team; CRT, crisis resolution team; MHA, Mental Health Act 1983; CTO, community treatment order; s., section (of MHA).
a. Linear regression was conducted for this variable, not Prais–Winsten regression, as there was no evidence of auto-correlations.
Social factors
We considered whether the rise in detentions was related to: increased social and economic hardship, reduced social support, demographic change, increasing psychiatric morbidity, and increasing drug and alcohol use in the population.
Internationally, wealthy countries tend to have higher rates of detention.Reference Sheridan-Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster1 However, at individual level, poverty and economic hardship, and lack of social support, are associated with increased risk of detention.Reference Walker, Mackay, Barnett, Sheridan-Rains, Leverton and Dalton-Locke32 The two periods of economic recession in the UK during the study period (1991 and 2008–2009)33 coincide with or immediately precede periods of steepest rise in detentions in England. However, many established markers of economic hardship, including unemployment rate, poverty/relative poverty and income inequality, do not show clear evidence of change nationally over the study period (Table 1). Evidence of reduced informal social support or increased social discord during the study period is also limited: median scores for social fragmentation – an established indicator of informal social support,Reference Congdon34 collected every 10 years through national census data – have changed little. More specific indicators of social discord and discrimination, such as recorded hate crimes and racist incidents, have available data only for recent years and provide an inconclusive picture. Public attitudes to mental illness also appear to be unchanged or to have become more positive, based on available data from 1994 to 2014 (Table 1).
Men, younger adults (age 18–35) and people from Black, Asian and minority ethnic (BAME) groups are at increased risk of detention in England.Reference Weich, McBride, Twigg, Keown, Cyhlarova and Crepaz-Keay35,36 The proportion of the population in England from all BAME groups has more than doubled between 1988 and 2016, as has the proportion of non-UK-born people in the population. The proportion of the population who are male has risen marginally. These rises may contribute to a rise in detentions (Table 1). Conversely, the proportion of the English population who are adults aged 18–35, the highest-risk age group for detentions, has fallen as the number of older adults has increased.
Available data suggest that psychiatric morbidity in England has increased during the study period, consistent with our fourth hypothesis. Adult Psychiatric Morbidity Survey (APMS) data collected every 7 years indicate a consistent rise in prevalence of people with common mental disorders with severe symptoms from 1993 to 2014, and a possible recent rise in prevalence of people with psychosis.26 A clear causal pathway between increased overall psychiatric morbidity and more detentions is lacking, however. The increasing number of people seen in secondary mental health services (Table 1) may reflect increased numbers of people with a severe mental health problem, who are also at risk of detention. Alternatively, however, it could reflect increases in help-seeking or service accessibility, which do not influence rates of detention.
Contrary to our hypothesis, rates of drug and alcohol use in the general population in England have fallen over the past 20 years). However, psychiatric hospital admissions for people with substance use disorders have risen since 2010 (supplementary Appendix 1), with a significant association with detention rate across the whole study period for cannabis use (Table 1). Three potential, not mutually exclusive, explanations for this discrepancy are: (a) drug use has increased among people accessing mental health services, in contrast to the general population; (b) the greater availability of potent drugs, including forms of cannabis such as skunk,Reference Freeman, Groshkova, Cunningham, Sedefov, Griffiths and Lynskey37 and novel psychoactive substances with mental health risksReference Mdege, Meader, Lloyd, Parrott and McCambridge38 has increased the risk of detention among drug users with mental health problems; and (c) changing attitudes among mental health practitioners to risk and safety and perceived treatability have led to more detentions of people with mental health problems who use drugs, independent of changes in patterns of drug use. We lack evidence to definitively support or reject any of these explanations, and the causal association of drug use and detention rates is uncertain (supplementary Appendix 2, section 2).
Service provision
Changes in the availability or quality of (a) in-patient care, (b) community crisis care, (c) longer-term community care, (d) reduced continuity of care during assessment for compulsory admission, (e) staff attitudes to risk and safety and (f) changes in prescribing practice were all considered as potential contributors to the rising rate of detentions.
In-patient care
The rise in detentions has coincided with a dramatic reduction in NHS psychiatric beds in England (Table 1). Plausible mechanisms have been proposed for why reduced bed availability may lead to more detentions.Reference Keown, Weich, Bhui and Scott39 Offer of in-patient admission may be delayed until illness becomes more acute. Relapse and re-detention may be more likely if patients are discharged prematurely because of bed pressures. Patients may not accept voluntary admission if the only available beds are far from home or because levels of disturbance in in-patient wards have increased, as only the most severely unwell, mainly non-consenting patients are admitted. Some psychiatrists report a perceived need to (unlawfully) detain patients who could have been voluntarily admitted, in order to secure prompt access to a bed.40 P.K. and colleaguesReference Keown, Weich, Bhui and Scott39 found that the association between bed reductions and detention rates at local level in England was strongest with a 1-year time lag, i.e. increases in detentions follow bed cuts. This suggests a possible causal relationship.
However, the same study found that a moderate correlation remained between NHS bed reductions and rises in detentions, both contemporaneously and with a time lag in the other direction, i.e. bed reductions following rises in detentions,Reference Keown, Weich, Bhui and Scott39 which less clearly indicates that bed reductions cause detentions. Increasing use of private beds (Table 1) and increasing access to community crisis alternativesReference Lloyd-Evans, Lamb, Barnby, Eskinazi, Turner and Johnson41 may mitigate some pressures caused by NHS bed reductions. A recent systematic review found no studies that had demonstrated a relationship between detention rates and bed occupancy rates, another indicator of pressures on available beds.Reference Walker, Mackay, Barnett, Sheridan-Rains, Leverton and Dalton-Locke32 An even more recent study has reported no significant association between in-patient bed numbers and detention rates in a multivariate model, for the period from 1999 to 2016.Reference Smith, Gate, Ariyo, Saunders, Taylor and Bhu42 Internationally, greater in-patient bed availability is associated with higher, not lower, rates of compulsory admissions.Reference Sheridan-Rains, Zenina, Dias, Jones, Jeffreys and Branthonne-Foster1
Community crisis care
Specialist community crisis care has proliferated in England following the national mandate in 2000 to introduce crisis resolution teams in the NHS Plan,43 and the accessibility of community crisis care may have increased further since 2011.Reference Lloyd-Evans, Lamb, Barnby, Eskinazi, Turner and Johnson41 However, no community crisis service models have been shown to reduce compulsory admissions.Reference Bone, McCloud, Scott, Machin, Markham and Persaud44 Improvements in service quality in crisis resolution teams had no impact on rates of compulsory admissions in a recent English trial.Reference Lloyd-Evans, Osborn, Marston, Lamb, Ambler and Hunter45 Hypotheses that reduced availability or quality of community crisis services has contributed to rising detention rates are not supported by available evidence.
Longer-term community care
We have limited evidence about how the quality of care in community services has changed since 1983. Over the past 15 years, the number of patients seen by mental health services has increased substantially, while overall mental health funding has increased only slightly and community mental health service staffing has remained relatively stable. Similar resources, spread across a larger patient group, have therefore led to a reduction in mental health spend per patient in secondary care, and in the number of contacts provided per patient in recent years in some service settings, for example community mental health teams (Table 1).
The extent and quality of community mental health service provision may relate to rates of detentions, although the relationship is complex. Interventions delivered in longer-term community care are best supported by current evidence as promising means to reduce detentions.Reference Bone, McCloud, Scott, Machin, Markham and Persaud44 Weich and colleaguesReference Weich, McBride, Twigg, Keown, Cyhlarova and Crepaz-Keay35 found that higher spending on community mental health teams in England was associated with lower local detention rates, but that health service areas with community teams assessed as lower quality than others also had lower rates of detention. As their reach increases, community mental health services, especially higher-quality teams, may be getting better at detecting the need for detention, but at the same time becoming less able to provide intensive support to individuals where necessary to prevent detentions, as their resources are spread more thinly across a larger patient group. Adult social care spending has fallen since 2010–2011:Reference Bottery, Ward and Fenney46 this could further reduce available support to prevent mental health crises and subsequent detentions.
Changes in prescribing practice
Regarding prescribing practice, reductions in use of clozapine and depot injections were proposed as factors that might increase patients’ risk of relapse and therefore of detention. However, there has been no clear reduction in the prescription of clozapine since 2007.Reference Roberts, Neasham, Lambrinudi and Khan47 National prescription cost data suggest that the number of items of depot antipsychotic medication prescribed has reduced marginally since 2000. However, although the association between depot prescriptions and (reduced) detentions was in the anticipated direction, this association was not statistically significant (Table 1). Furthermore, given variable dosing schedules, fewer prescriptions do not necessarily reflect a reduction in the number of people for whom depot medications are prescribed. Finally, there is some evidence that depot injections may not increase adherence in any case.Reference Sendt, Tracy and Bhattacharyya48
Staff attitudes to risk and safety
Risk and safety are important considerations for mental health staff,Reference Szmuckler and Rose49 and clinicians’ attitudes and responses to risk are highly variable and subjective.Reference Robertson and Collinson50,Reference Stone51 Perceived risk has consistently been identified as the strongest predictor of outcome of assessments for involuntary admission in English studies.Reference Singh, Burns, Tyrer, Islam, Parsons and Crawford52–Reference Wickersham, Nairi, Jones and Lloyd-Evans54 The amendments to the MHA in 2007 extended the reach of coercion in response to perceived risk by broadening legal definitions of mental disorder and treatability, and introducing community coercion through community treatment orders, and has been characterised as reflecting a more general societal preoccupation with risk minimisation.Reference Pilgrim55 Szmukler & RoseReference Szmuckler and Rose49 identify an increasing salience for risk assessment in mental healthcare internationally. It is plausible that increasing focus by mental health staff on risk and safety may have contributed to the rise in detentions since 1983. The increase in detentions for assessment under section 2 of the MHA, rather than treatment under section 3, may be consistent with an increasing willingness by mental health staff to detain people in the context of potential perceived risks, not just established known risks. However, we cannot quantify any such change in attitudes or its impact on detention rates.
Continuity of care
We found little evidence regarding how changes in the continuity of care at MHA assessments may affect the outcome of assessment and thus detention rates. One small study suggests that presence of a community professional, such as the patient's care coordinator, may reduce the risk of a formal assessment for compulsory admission resulting in detention.Reference Wickersham, Nairi, Jones and Lloyd-Evans54 However, we lack information about the extent of any changes over time in the involvement in MHA assessments of practitioners, including general practitioners, who know the patient being assessed.
Legal factors
Three legal factors potentially relevant to detention are: (a) changing legislative approaches to patients who lack decision-making capacity but do not actively object to hospital admission; (b) the introduction of compulsory community treatment; and (c) the police's use of legal powers to bring people with suspected mental health problems to a place of safety for assessment.
Capacity and consent to treatment
Since the Human Rights Act 1998 came into force in England in 2000, enshrining the European Convention on Human Rights, it has been unlawful to admit anyone to psychiatric hospital on a voluntary basis who lacks the capacity to consent to this treatment. This requirement has been reinforced by subsequent English case law, most notably the ‘Bournewood judgment’ in 2004 and the ‘Cheshire West’ case in 2014. Deprivation of liberty safeguards (DoLS) were introduced in 2008 as an addition to the Mental Capacity Act 2005 (MCA): DoLS provide a legal framework for approving in-patient admission and treatment for people who lack decision-making capacity, without using detention under the MHA. It is hypothesised that the rising rate of detentions in England may reflect increasing compliance with human rights law through the application of the MHA rather than DoLS to those who might previously have been admitted voluntarily.
Available research suggests that, prior to the introduction of DoLS, as many as 20% of in-patients were non-objecting and voluntarily admitted, but lacked capacity to consent to admission.Reference Owen, Richardson, David, Szmukler, Haywood and Hotopf56 In 2017–2018, however, fewer than 4000 DoLS applications were completed for patients in psychiatric hospitals,57 i.e. only about 4% of roughly 100 000 admissions per year in total.58 The uncertainty in extrapolating from one small research study's findings is acknowledged, and we do not know whether, in practice, some non-objecting patients who lack decision-making capacity may still be (unlawfully) admitted to hospital voluntarily. However, if detention under the MHA is always now used to admit the remaining non-objecting patients who lack capacity but are not subject to DOLS, this could explain a substantial proportion of the rise in detentions in the past decade.
Compulsory community treatment
The introduction of community treatment orders (CTOs) in 2008 has been proposed as a potential contributor to the rising rate of detentions, either by lowering the bar for readmission of patients subject to a CTO (through the use of recall to hospital) or by increasing the risk of relapse by facilitating earlier, premature hospital discharge following the index admission leading to the CTO. The use of CTOs in England increased year on year from 2008 to 2016, with the numbers of people readmitted to hospital from a CTO rising correspondingly (Table 1). However, a recent systematic reviewReference Barnett, Matthews, Lloyd-Evans, Mackay, Pilling and Johnson59 provides clear evidence that internationally and in England, compulsory community treatment has no effect on raising or reducing readmission rates. This hypothesis is therefore not supported by available evidence.
Police use of place of safety powers
Police use of legal powers (s.135 or s.136 MHA) to convey someone to a health-based place of safety has risen markedly during the study period. This has led to a corresponding increase in the number of people admitted to psychiatric hospital following use of a police place of safety order (Table 1). It is unknown what proportion of these people might otherwise have been detained via a different pathway, but it is plausible that police are becoming better at identifying people who meet criteria for detention in hospital and bringing them to the attention of health services. Some of those who are now detained via a place of safety order may previously have been arrested or left in public spaces or at home.
Data recording
The Care Quality Commission proposed that more complete reporting of detentions by provider organisations may have led to an artefactual rise in recorded detentions over the study period.7 An analysis of patient records from 2007 to 2016 in six London boroughsReference Oram, Colling, Pritchard, Khondonker, Fonseca de Freitas and Ter-Minassian60 found substantially lower increases in detention rates in these boroughs than those observed nationally. However, the extent of missing data in the routine nationally collected KP90 data on detentions, and whether this has changed over time, are unknown.
‘Double-counting’ in official statistics may contribute to a rise in the recorded rate of detentions. Detention episodes within one provider organisation are reported in the KP90 data used for this paper as a single detention, even if a person is transferred from one form of detention to another during this episode (e.g. transfers from a MHA section 2 detention for assessment to section 3 detention for treatment). However, recorded detentions in the KP90 data are inflated by double-counting of transfers in care, where a patient is moved during detention from one hospital to another run by a different provider organisation.36 This may account for between 12 and 20% of all detentions recorded in the data, and accounts for the big drop in English national detention records in 2017, when a new reporting system was adopted.Reference Congdon34 The increase in the use of private hospitals during the study period is associated with the rise in detentions (Table 1) and suggests that transfers of care during detentions might have increased, leading to more double-counting and an artefactual rise in reported detentions. However, the extent of any such rise over time is unknown.
Development of an explanatory logic model
From the evidence summarised above, and presented more fully in supplementary Appendices 1 and 2, ratings were made regarding the strength of evidence for each proposed hypothesis to explain the rise in detentions (Table 2).
Table 2 Strength of evidence ratings for hypothesised explanations for the rise in detentions
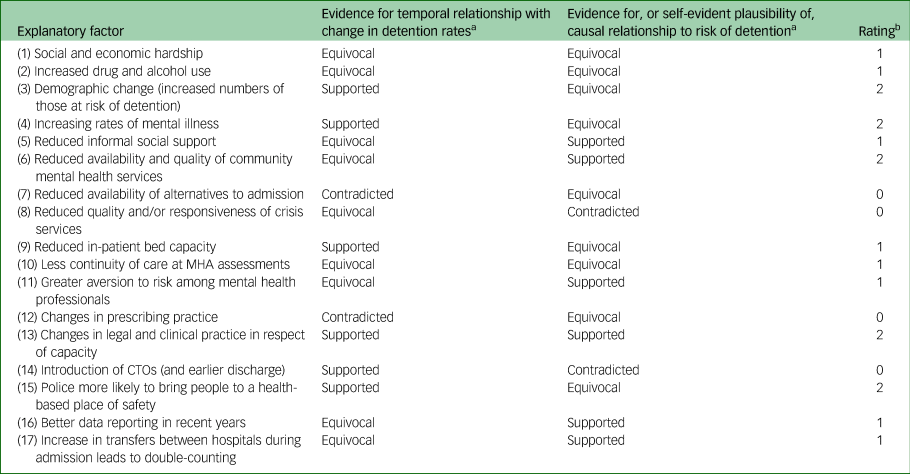
MHA, Mental Health Act 1983; CTO, community treatment order.
a. Contradicted, contradicted by current evidence; equivocal, absent or ambiguous evidence; supported, supported by current evidence.
b. 0, hypothesis is contradicted by available evidence; 1, lack of evidence or available evidence is ambiguous or mixed; 2, hypothesis is supported by the balance of available evidence.
An explanatory logic model was then developed (supplementary Appendix 3). Hypotheses contradicted by available evidence were excluded from the model. Bold and dashed text boxes were used to distinguish components of the model supported by available evidence, and those for which available evidence was ambiguous or lacking. Arrows highlighted possible relationships between components of the model.
Following reviewers’ feedback on the full logic model described in supplementary Appendix 3 and the initial paper draft, we decided to develop a second visual explanatory model for the observed rise in rates of detentions from 2010 onwards. The rationale for this second model is that more data are available for potential explanatory factors in this period. This complementary but simpler and clearer explanatory model distinguishes two overarching pathways to the rise in detentions during this decade: an increase in perceived need for detention; and an increase in actual need. This second model is shown in Fig. 2.
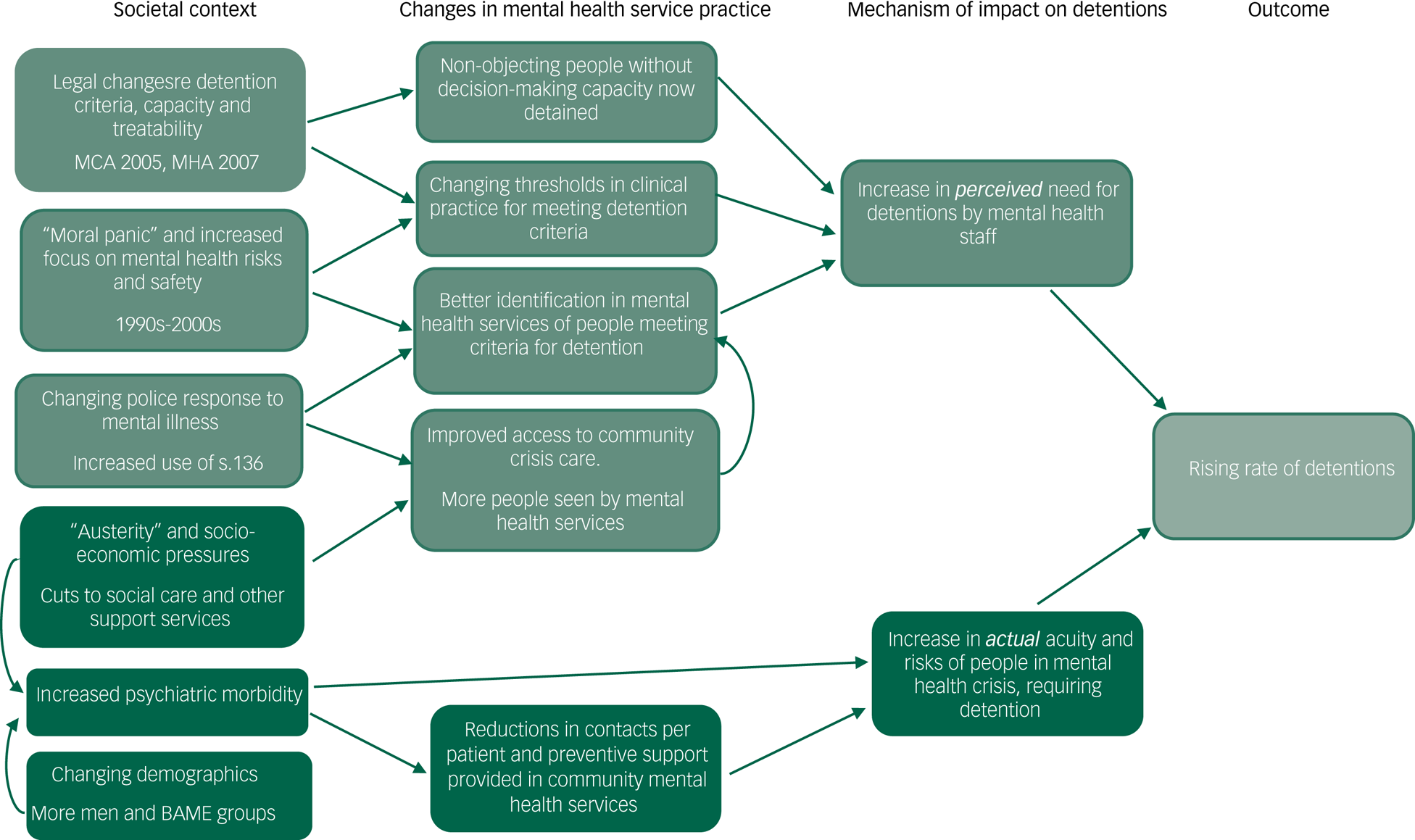
Fig. 2 Two proposed pathways to the rising rate of detentions in England 2011-16: a provisional explanatory model.
Discussion
Main findings
Our explanatory model shows that societal, service-related and legal factors may all contribute to the rise in detentions in England since 1983. Changes in legal approaches to safeguarding the rights of patients who lack decision-making capacity are a probable major contributor to the rapid increase in detentions in this decade. Rising levels of mental illness and demographic change in the population may both contribute. Mental health services and the police may be getting better at identifying people who meet criteria for detention, while in some community mental healthcare settings, increasingly stretched resources may reduce the availability and intensity of the preventive support that can be provided to patients to avert relapse or subsequent detention.
Other factors may be important, but we lack confirmatory evidence. These include: increased exposure of vulnerable groups to economic and social hardship, reduction of available informal social support, changes in drug use among the patient population, changes in public and practitioners’ attitudes to risk and safety, and reduced NHS in-patient bed availability. The reported rise in detentions may have been inflated by the unreliability of available data.
Available evidence suggests that reductions in the availability or quality of community crisis care and the introduction of community treatment orders have not contributed to the rise in detentions. We also found evidence that public fear and exclusion of people with mental illness has decreased in England during the study period, in contradiction to a hypothesis that reduced tolerance of people with mental health problems has driven the rise in detentions.
Strengths and limitations
Our paper collects and appraises the available evidence for and against 17 hypotheses for the rising detention rate, finding evidence to support 4 and reject 3 hypotheses. It thus provides the most comprehensive and informed exploration to date of the rising rate of detentions in England. We identify ten limitations of this paper. First, reported detention rates are based on routinely collected national data that are not wholly reliable. Second, our list of hypotheses to explain the rising rate of detentions may not be exhaustive. For example, the impact on detention rates of changing practices in discharge and transfer of patients with mental health conditions from accident and emergency and general hospitals was raised during the peer review process for this paper. The selection and framing of hypotheses, and ratings of the strength of evidence supporting each hypothesis, will inevitably reflect the perspectives and biases of those involved. Both the MHA Review topic group and the paper's authors comprised a range of mental health stakeholders, but the most represented group in both was academic psychiatrists. Third, because of the breadth of the topic, searches for available evidence were not systematic, and relevant data or research may have been overlooked. Fourth, our evaluation has highlighted hypotheses for which corroborating evidence from explanatory variables is available. However, hypotheses for which we lacked any relevant data to explore associations with detentions may be equally important – for example, changes in attitudes to risk and safety and risk assessment practice among mental health professionals. Fifth, for some hypotheses for which potential explanatory variables were identified, we lacked sufficient data points to allow statistical exploration of their relationship to detention rates. For variables with at least ten data points for which we did conduct analyses, these were not informed by power calculations: potentially important relationships may not have achieved statistical significance. Sixth, identified associations between explanatory variables and detention rates do not determine whether relationships are causal. With the exception of in-patient bed numbers, we were rarely able to establish temporality to inform consideration of the direction of causation in associations. For many hypotheses, additional available research was insufficient to confidently infer or reject causality or establish mechanisms. For example, it is unclear why men and people from BAME ethnic groups are detained more often, and many proposed explanations lack empirical support.Reference Barnett, Mackay, Matthews, Gate, Greenwood and Ariyo61 Seventh, for many of the explanatory variables that we examined, data regarding changes over time were only available at whole-population level, not specifically for those people who are detained, or vulnerable to detention, thus creating risks of ecological fallacies. This may have particularly limited our exploration of the impact of social and economic factors on detention rates. For instance, falls in overall poverty levels in England have not been experienced equally among all demographic groups,62 while the measure of income inequality used in our analyses (the Gini coefficient) has been criticised as being insufficiently sensitive to change.Reference Gastwirth63 We have been unable to locate evidence specifically for people with mental health problems regarding change over time in levels of unemployment, work precarity, disposable income, benefits sanctions, living alone or similar variables, with which to interrogate our hypotheses in more depth. Eighth, we used a single source of data for each population-level indicator used as potential explanatory variables, to allow comparisons of change over time. However, for some indicators, there were changes during the study period in data-reporting methods or acknowledged concerns about data quality, which may limit the validity of comparisons over time. Where identified, these are reported for each variable in supplementary Appendix 1. Ninth, for mental health service provision, staffing and funding, we have relied on available national data for mental health services in general. Specific changes or pressures for children's or older adults’ services may be obscured. Last, we have mainly looked at the relationship between proposed explanatory factors and detention rates individually. We were limited in how far we could explore interrelationships between explanatory factors and cumulative effects of exposure to several factors.
For these reasons, our proposed explanatory logic model has limited empirical support. It does not offer certainty, but does illustrate likely and possible contributory factors to the rising rate of detentions in England between 1983 and 2016. We have looked specifically for evidence to explain the rise in detentions in England during this time period: our explanatory model may have less validity for other countries and time periods.
Implications for research
This study was limited by the limited information available from routine data about detentions in England. The complete KP90 data held by NHS Digital, which allowed us to compare rates of detention over time, could not yield answers to basic questions regarding in which clinical or demographic groups the rise was occurring. Better routine data are required. The change by NHS Digital in 2016–2017 to collecting complete data about detentions at individual patient level26 may address this need to some extent over time. The development of local NHS systems that allow researchers to access detailed, anonymised records for all patients using local secondary mental health servicesReference Fernandes, Cloete, Broadbent, Hayes, Chang and Jackson64 also enables more sophisticated understanding of risk factors for detention and changes over time.
Our study highlights numerous areas where further research is needed regarding the relationship of potential explanatory factors to rates of detention, especially for social and economic factors, and attitudes to risk and safety.
Public health research indicates that increasing psychiatric morbidity in England may be a result of increasing social deprivation,Reference Barr, Kinderman and Whitehead65 and that specific social and administrative measures may also influence mental health outcomes: for instance, increases in ‘fitness for work’ tests being associated with more suicides.Reference Barr, Taylor-Robinson and Stucker66 We need a clearer and more nuanced understanding of the extent of exposure to social and economic stressors among people with mental health problems, how this may change over time and how, if at all, it relates to changes in rates of detention.
Practitioners’ attitudes to risk and safety are variable and highly important regarding decisions to detain,Reference Sendt, Tracy and Bhattacharyya48–Reference Stone51 but changes over time in clinical culture and practice are not easily evaluated empirically. More qualitative research to understand the nature and extent of practitioners’ biases and group-level stigma has been called for, to aid understanding of the rise in detentions and the disproportionately high rates of detention for people from BAME groups.Reference Barnett, Mackay, Matthews, Gate, Greenwood and Ariyo61 A better understanding of what drives clinicians’ decision-making regarding detention is desirable, as is development and evaluation of interventions to improve the quality of risk assessment and encourage appropriate positive risk-taking.
In this context, three elements of the legal processes for detention are priorities for further research. First, there is a need to understand the causes and consequences of the specific rise in the use of section 2 of the MHA for assessment, rather than section 3 for treatment. Although this may simply be an appropriate response to more new people requiring detention,Reference Oram, Colling, Pritchard, Khondonker, Fonseca de Freitas and Ter-Minassian60 the MHA Review expressed concerns that section 2 is being ‘overused’,6 either through a growing perception that it is less restrictive than a detention for treatment, or because it can be easier to complete, as does not require a place of treatment to be identified. Exploration of patient-level data is desirable regarding circumstances and rates of conversion from assessment and treatment sections, and their relationship to subsequent readmission rates. Second, research is required to understand clinicians’ decision-making processes in using MHA or MCA DoLS processes to detain patients who are not objecting to admission but lack decision-making capacity, and how this choice affects patients’ experiences and outcomes. Third, research is needed to understand the circumstances in which patients are discharged from detention following appeal to a tribunal. This may help identify uses of detention that were unwarranted or avoidable, and how these may contribute to the rising detention rate.
Implications for policy and practice
There is considerable uncertainty about many of our proposed explanations for the rise in detentions in England. Furthermore, interventions might help to reduce detentions, even if they are unrelated to the reasons for the rise: for example, improving community crisis care. For these reasons, implications from our study for policy and practice should be proposed with caution. However, we suggest three areas of priority for reducing detentions.
First, an increase in detentions appears to have been an unintended consequence of legislation and English case law regarding safeguarding the rights of non-objecting patients who lack decision-making capacity and require hospital admission. Clear guidance and training are required for practitioners regarding assessment of capacity and when detention under the MHA is indicated rather than use of DoLS provisions under the MCA. Sufficient staff, appropriately trained in both processes, are required to ensure that the most appropriate course of action can be used in each case.
Second, the past decade has seen a large increase in the number of people treated by secondary mental health services (in addition to the expansion of psychological services in primary care), and a corresponding reduction in the amount of care offered to each individual patient in some service settings. This appears to have been a de facto change in mental healthcare over the past decade rather than one explicitly planned in policy. Within any level of total investment, achieving the optimal balance between breadth and depth of care involves weighing many different aims and priorities. Consideration should be given by policy planners and commissioners to the share of healthcare funding provided to mental health services, and to the potential effect on detention rates of spreading mental health resources increasingly widely, and thus away from the high-need, low-number group of patients most vulnerable to detention.
Third, our study shows that not all the rise in detentions in England necessarily relates directly to mental health service provision: wider societal factors may be equally important to address. Potential contributory factors such as increasing psychiatric morbidity and social deprivation and inequalities require a broader public health and governmental response. More attention to the potential mental health impact of wider social policy is desirable.
Lived experience: commentary by Stephen Jeffreys and Stella Branthonne-Foster
Collectively, we have personal experience of community and in-patient mental health services. We commented on drafts of this paper but did not contribute to the design and scope of the project.
The authors highlight gaps in detentions data: lack of individual-level data and failure to differentiate between frequent individual detentions and detention of more people, plus limited monitoring of Equality Act 2010 protected characteristics.
The paper suggests that detaining more patients lacking capacity, who were previously admitted informally, is a major factor. However, this hypothesis relates only to the second period of steepest rise in detentions. Furthermore, it would be interesting to specifically examine child and adolescent mental health services data for similar trends.
The children and young people's landscape is vastly different from that of their adult counterparts and needs specific consideration. We regret that data on children and young people are merged into the overall national data-set; it is important to note the differences in services (both in-patient and community), and the needs and presentations of under-18s. We anticipate that absence of these data obscures factors specific to that age group.
The biggest increases in detention rates have coincided with two periods of recession, but the authors were unable to demonstrate the impact of austerity or find data specific to those with mental health problems. We suggest widening this investigation to encompass other and more intangible factors associated with austerity and neoliberal ideology, such as individualism, cuts in local services and financial uncertainty. As there has also been a substantial increase in demand on community mental health teams, this work should not be limited to rates of detention.
The paper reveals that MHA section 2 detentions have increased, with section 3 figures remaining stable. Are hospitals discharging patients more quickly and perhaps too quickly owing to pressure on beds, are they finding swifter methods of support and treatment, or are more people being detained under the MHA unnecessarily?
Supplementary material
Supplementary material is available online at http://doi.org/10.1192/bjo.2020.64.
Data availability
The data supporting the findings of this study are available within the article (and/or its supplementary materials).
Funding
This paper presents independent research commissioned and funded by the National Institute for Health Research (NIHR) Policy Research Programme, conducted through the NIHR Policy Research Unit in Mental Health (PR-PRU-0916-22003). The views expressed are those of the authors and not necessarily those of the NIHR, the Department of Health and Social Care or its arm's length bodies, or other Government Departments. S.P.S. is part-funded by the NIHR Collaboration for Leadership in Applied Health Research and Care West Midlands (NIHR CLAHRC WM).
Acknowledgements
Dr Gareth Owen, Professor Paul McCrone and Joe Botham from King's College London helped to identify relevant data or research papers for some of the evidence summaries in this paper. We thank Stephen Jeffreys and Stella Branthonne-Foster, both members of the Lived Experience Working Group in the National Institute for Health Research (NIHR) Mental Health Policy Research Unit, for their commentary on this paper.
Author contributions
B.L.-E., C.M., S.S. were members of the Working Group for the Independent Review of the Mental Health Act 1983. B.L.-E., C.M., S.S., D.C.-K., P.K. and S.P.S. were members of the expert topic group on understanding the rising rate of detentions, which supported the Independent Review of the Mental Health Act. The topic group was chaired by S.W., and topic group members helped generate and refine study hypotheses. B.L.-E., S.W., C.M., S.S., S.J. and L.S.-R. designed the study. J.K. advised on relevant data sources. L.S.-R., L.M., N.L. and B.L.-E. extracted data, scoped relevant research papers and drafted hypothesis summaries for supplementary Appendix 2. L.S.-R. conducted data analyses, with advice from R.J.. B.L.-E. and L.S.-R. drafted the manuscript. All authors (L.S.-R., S.W., C.M., S.S., P.K., D.C.-K., S.P.S., R.J., J.K., L.M., S.B.-F., S.J., B.L.-E.) helped interpret findings, revise the manuscript and approved the submitted version.
Declaration of interest
B.L.-E., C.M., S.S. were members of the Working Group for the Independent Review of the Mental health Act 1983. B.L.-E., C.M., S.S., D.C.-K., P.K. and S.P.S. were members of the expert topic group on understanding the rising rate of detentions, which supported the Independent Review of the Mental Health Act. S.W. chaired the topic group.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjo.2020.64.
Appendix
Proposed hypotheses for the rising rate of detentions in England since 1983
We hypothesised the following 17 potential contributory factors to the rising rate of detentions, listed here with possible mechanisms for the hypotheses (how might exposure to the hypothesised risk factors cause or modify the risk of detention?)
Social factors
(1) Social and economic hardship: increased exposure to social stressors leads to more frequent relapses in the patient population and/or increase in rates of people developing a mental illness, leading to more detentions (social stressors could include: poverty, unemployment, social inequality, benefits sanctions, exposure to discrimination or hate crime).
(2) Increased drug and alcohol use: increased substance misuse leads to increased risk of relapse in the patient population and/or increased rates of mental illness.
(3) Demographic change (increased numbers of those at risk of detention): some demographic groups are at higher risk of detention than others (i.e. men, people from BAME groups and young adults age 18–35): if the proportion of the population from these groups increases, we would expect higher rates of detention.
(4) Increasing rates of mental illness: a proportion of those with mental illness become so unwell that detention is required: higher rates of mental illness lead to more detentions.
(5) Reduced informal social support: the absence of informal support (and perhaps the increase in people living alone) leads to higher rates of relapse; it also makes delivery of community-based crisis care difficult, and admission more likely; bed pressures result in the eventual need for detention.
Service factors
(6) Reduced availability and quality of community mental health services: reductions in the reach (number of patients seen) by community mental health ongoing care services leads to reduced capacity to prevent detentions. Reductions in the quantity and quality of care provided to current patients (possibly due to reduced investment in community mental health services) lead to increased rates of relapse, leading to more detentions.
(7) Reduced availability of alternatives to admission: reduced availability of less restrictive community alternatives to admission leads to more compulsory admissions for patients not prepared to go into hospital.
(8) Reduced quality and/or responsiveness of crisis services: later intervention, or the lack of home treatment services, will result in more patients needing to be admitted.
(9) Reduced in-patient bed capacity: lack of availability of beds (evidenced by reduction in bed numbers or increased bed occupancy rates) means that patients have longer to wait for a bed and are therefore more unwell at the time of admission; or are detained when voluntary admission was possible, in order to secure a bed; or are discharged prematurely to free beds, leading to more frequent relapse and re-detention.
(10) Less continuity of care at Mental Health Act (MHA) assessments: assessment of risk may be more conservative (and overestimated) by professionals who do not know the patient.
(11) Increased focus on safety and risk among mental health professionals: section 12 doctors and approved mental health professionals (AMHPs) have become more likely to detain patients with a risk and clinical presentation that would not have led to detention in the past, owing to changes in professional culture and attitudes to patient safety and risk management.
(12) Changes in prescribing practice: reduced use of depot medication over time has led to reduced medication adherence, resulting in more relapses and subsequent detentions. Reduced use of clozapine over time has led to more relapses and subsequent detentions.
Legal factors
(13) Changes in legal and clinical practice in respect of patients who lack decision-making capacity: following the Bournewood judgment (HL v. UK [2004] ECHR 471) in 2004, non-objecting patients who lack decision-making capacity, who might previously have been admitted to hospital informally, must now be subject to a ‘lawful process’, i.e. detention under the Mental Health Act 1983 or the Mental Capacity Act 2005 deprivation of liberty safeguards (DoLS).
(14) Introduction of community treatment orders (CTOs) (and earlier discharge): (a) there is a lower threshold for CTO recall than for admission following an MHA assessment, so CTO patients are recalled to hospital who would not otherwise have been detained, leading to an increase in compulsory admissions since introduction of CTOs in 2008; (b) CTOs are used as a means of facilitating early (premature) discharge, leading to frequent relapse and recall/readmission.
(15) Police more likely to bring people to a place of safety under section 135 or 136: increasing mental health awareness and use of MHA sections 135 and 136 by the police lead to patients being brought to a place of safety and subsequently detained, who would previously have been arrested or left at home/in public places and not have ended up detained through other routes.
Data-recording factors
(16) Better data reporting in recent years: over time, service providers are submitting more complete data returns regarding detained patients, so underreporting of detentions in official statistics reduces.
(17) Increase in transfers between hospitals during admission leads to double-counting: increasing bed pressures lead to an increase in transfers between hospitals for patients during a detention (out-of-area NHS placements and use of private hospitals), leading to increased double-counting of detentions in KP90 data.








eLetters
No eLetters have been published for this article.