2.1 Overview of the evidence: skill-mix interventions, professions, care sectors
Worldwide, countries are seeking strategies to strengthen their health workforce to ensure health systems are sustainable and resilient and to reach universal health coverage (World Health Organization, 2016). In Europe, a 2019 expert opinion focused on task shifting, which is one – among several – examples of skill-mix innovations (European Commission, 2019). However, to date, a systematic analysis of skill-mix innovations and their effects on outcomes has been missing. Skill-mix changes have been suggested to be of high relevance to respond to changing patient needs (for example, for patients with chronic conditions and multimorbidity), unequal access to services (for example, for vulnerable groups), skill gaps (for example, in long-term and palliative care) and changes among the health workforce (shortages and maldistribution) (see Chapter 1).
This chapter will synthesize the evidence on skill-mix changes and outcomes for individual patients and populations, health systems and health professionals. Hence, for the purpose of this book, an overview of reviews was conducted on the outcomes of skill-mix changes, and mini case studies were written on country-specific and setting-specific developments. The methods of the overview of reviews are described in Box 2.1. More details on the methodology as well as the mini case studies are provided in Chapter 1.
Box 2.1 Methods of the overview of reviews
A short summary of the methods is provided below, for more details please refer to Chapter 1 and the protocol (PROSPERO Nr. CRD42018090272) (Reference Maier, Kroezen and HartlMaier et al., 2018).
Search strategy and screening: Systematic search conducted in six databases (Embase, MEDLINE, Cochrane CENTRAL, Web of Science, CINAHL, PsycINFO) and Google Scholar, plus snowballing. The search terms covered skill-mix using a broad definition, including all professions, lay workers and informal carers/caregivers. The search strategy was developed in cooperation with a librarian. Skill-mix was defined as changing roles, tasks and/or teamwork in primary care, ambulatory care or at the interface between hospital-ambulatory care settings. Systematic reviews on implementation of skill-mix, barriers and facilitators were also included. The protocol provides a list of all search terms (Reference Maier, Kroezen and HartlMaier et al., 2018). Titles and abstracts as well as full-text versions were screened by a team of researchers, after in-depth piloting and high levels of interrater reliability scores.
Inclusion criteria: Systematic reviews with narrative synthesis and/or meta analyses, any skill-mix intervention with patients-, health system or profession-specific outcomes or implementation, all populations or patient groups, all health professions, lay workers and informal caregivers working in primary care (including ambulatory care settings) or at the hospital–ambulatory care interface.
Exclusion criteria: Systematic reviews with no focus on skill-mix, study designs other than systematic reviews, hospital settings (inpatient), nursing homes, emergency care, non-English languages, reviews published before 2010 (because of the high number of reviews identified and the focus on skill-mix innovations, defined as a novelty).
Analysis: The analysis included the extraction of the findings and a narrative synthesis of the evidence by population group(s) and diseases, following five segments of care (modified from OECD, 2017): health promotion and prevention, acute care, chronic conditions, long-term care and palliative care; and access to health services (for vulnerable groups and in underserved areas). The findings were extracted by a core group of researchers from TU Berlin and Erasmus University into standardized excel files, after pilots and double checks by one researcher to ensure consistency.
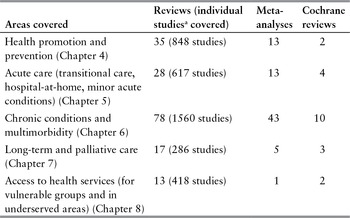
The overview of reviews resulted in a total of 187 systematic reviews, of which 171 focused on skill-mix in (at least) one of the five care segments and included at least one outcome measure on patients or populations, health systems or effects on health professionals (Table 2.1). A total of 29 reviews analysed skill-mix and factors related to implementation and are summarized in the chapter on implementation and policy lessons (Chapter 3). It should be noted that 13 reviews covered skill-mix and outcomes as well as implementation, and so are covered in both this chapter and Chapter 3.
Table 2.1 Skill-mix and outcomes: total number and characteristics of systematic reviews included
| Areas covered | Reviews (individual studiesa covered) | Meta-analyses | Cochrane reviews |
|---|---|---|---|
| Health promotion and prevention (Chapter 4) | 35 (848 studies) | 13 | 2 |
| Acute care (transitional care, hospital-at-home, minor acute conditions) (Chapter 5) | 28 (617 studies) | 13 | 4 |
| Chronic conditions and multimorbidity (Chapter 6) | 78 (1560 studies) | 43 | 10 |
| Long-term and palliative care (Chapter 7) | 17 (286 studies) | 5 | 3 |
| Access to health services (for vulnerable groups and in underserved areas) (Chapter 8) | 13 (418 studies) | 1 | 2 |
Note: a Total number of individual studies includes double or multiple counting if listed in more than one systematic review.
The total number of identified reviews is high, but the numbers vary between the different areas in primary care and for the patient groups covered. Especially rich is the evidence on skill-mix changes for patients with chronic conditions, which includes a total of 78 systematic reviews and is summarized in Chapter 6. Moreover, 43 reviews performed meta-analyses. Two areas that were also well researched are skill-mix changes to improve health promotion and prevention, covered by 35 reviews (Chapter 4), and for patients with acute conditions, covered by 28 reviews (Chapter 5). Two fields were less well covered: long-term and palliative care was covered by 17 reviews (Chapter 7) and skill-mix interventions to improve access to services was addressed by 13 reviews, of which only one focused specifically on rural areas (Chapter 8).
Overall, the review methods including data analysis varied. The majority of the reviews performed narrative analyses of the findings.
For skill-mix changes in chronic care, however, more than half of the reviews (43 of 78 reviews) performed meta-analyses. A total of 21 Cochrane reviews summarized skill-mix interventions and health outcomes across the five areas covered in this volume. Cochrane reviews use a highly standardized, rigorous methodology and have become the reference standard for systematic reviews.
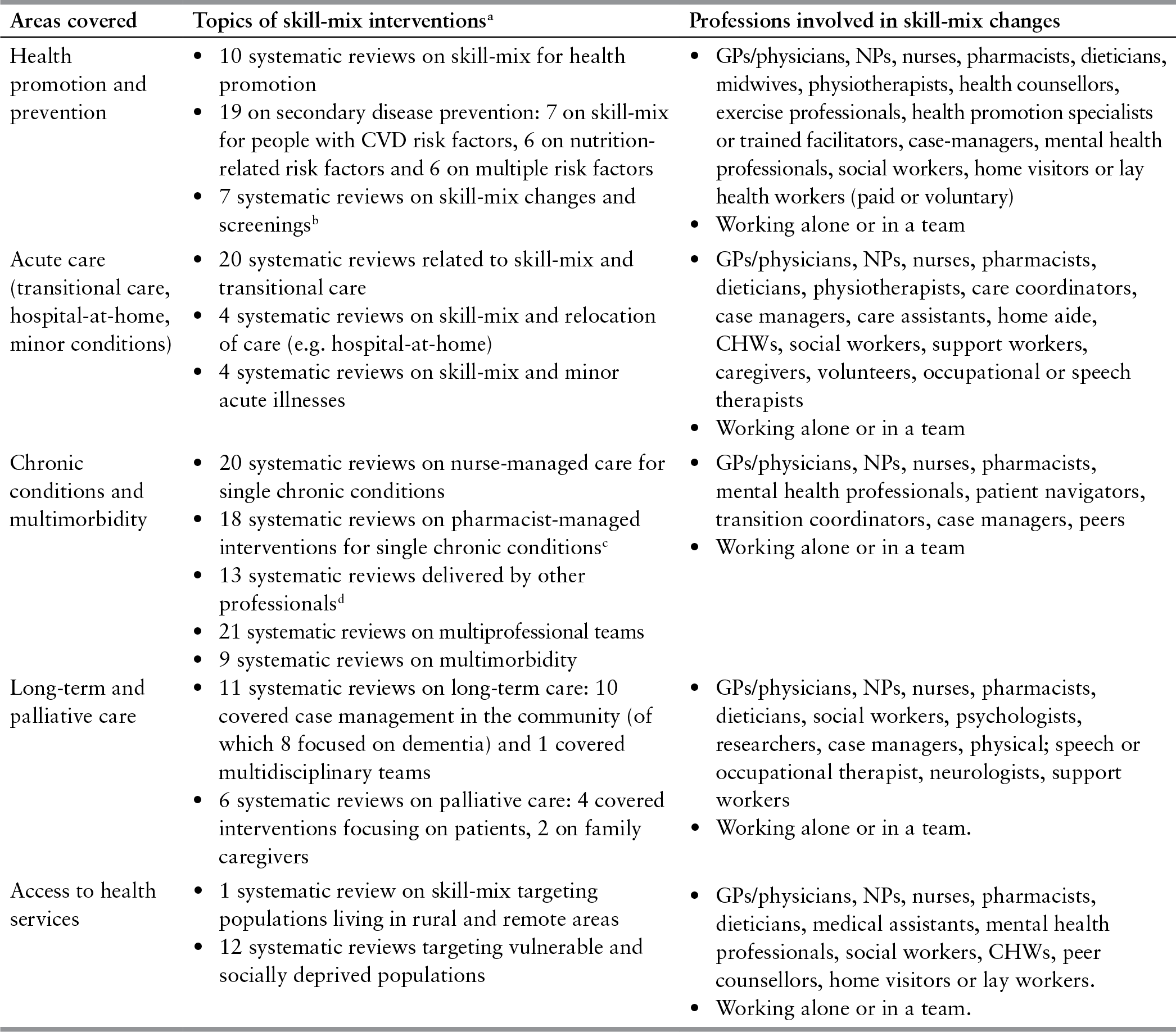
Main topics and themes of the skill-mix interventions
A wide range of different topics and areas were covered not only across, but also within the main five care segments (Table 2.2). Within health promotion and prevention, the largest number of reviews (19 reviews) evaluated skill-mix changes related to secondary prevention for patients with risk factors, followed by 10 reviews on skill-mix aimed at improving the health of healthy populations or population groups (health promotion) and seven reviews on skill-mix and screenings (for example, patient navigator interventions to improve cancer screening uptake and nurse-delivered colorectal and skin cancer screenings) (Chapter 4).
Within acute care (which covers acute conditions, acute episodes of chronic conditions such as stroke and acute myocardial infarction, and minor illnesses), most evidence was available on skill-mix changes aimed at care transitioning between the hospital and ambulatory care interface (20 systematic reviews), followed by four reviews on hospital-at-home and four on minor acute illnesses in ambulatory care settings (Chapter 5).
Skill-mix and chronic conditions was the most researched, particularly for patients with a single chronic condition with the aim to improve the quality of care, self-management and monitoring. The interventions were primarily performed by nurses and pharmacists (20 and 18 systematic reviews, respectively). A total of 21 reviews analysed the effects of multiprofessional teams. Overall, nine reviews specifically analysed skill-mix interventions for patients with multimorbidity (Chapter 6).
On long-term care, of the 11 reviews identified, the majority covered case management for patients with dementia (eight reviews). Palliative care was less often researched, four reviews analysed skill-mix interventions directed at improving outcomes for patients with palliative care needs, whereas two focused on their caregivers (Chapter 7). Finally, 12 reviews were aimed at improving access to services for vulnerable population groups. Yet, perhaps counterintuitively, only one systematic review focused on skill-mix and access in underserved regions (Chapter 8).
Table 2.2 Skill-mix changes in primary and chronic care: professions involved and topics of skill-mix interventions
| Areas covered | Topics of skill-mix interventionsa | Professions involved in skill-mix changes |
|---|---|---|
| Health promotion and prevention |
|
|
| Acute care (transitional care, hospital-at-home, minor conditions) |
|
|
| Chronic conditions and multimorbidity |
|
|
| Long-term and palliative care |
|
|
| Access to health services |
|
|
Abbreviations: CHW: community health worker; CVD: cardiovascular disease; GP: general practitioner; NP: nurse practitioner.
Notes: a Several reviews cover multiple skill-mix areas or several professions and are therefore listed more than once. b One review covers health promotion and screening. c One review covers pharmacist-delivered, nurse-delivered interventions and multiprofessional teams. d One review covers single chronic conditions and multimorbidity.
Professions and informal workers involved in skill-mix interventions
The changing roles of many different health professions and lay workers were evaluated in the systematic reviews. Table 2.2 shows the diversity of professions who were affected by skill-mix changes, ranging from physicians / GPs to home visitors and others, often lay workers with no or limited additional training.
However, when looking at the main providers involved in skill-mix changes, two professions stood out: the highest number of individual studies analysed skill-mix changes involving nurses and pharmacists. For instance, for patients with chronic conditions and multimorbidity, 20 reviews analysed nurse-managed care and 18 reviews analysed pharmacist-managed care (often compared with physician-managed care) for patients with chronic conditions (Table 2.2). In addition, some reviews focused on skill-mix changes targeting (primary care) physicians, physiotherapists, dieticians and physician assistants, among others.
The role of community-based workers and other lay health workers (usually with additional training) was evaluated in expanding health promotion and screenings, particularly for vulnerable population groups. Interventions often targeted the patients themselves or their caregivers, and included educational components, coaching and other measures to improve self-management and health literacy skills. This refers to reviews on health promotion (Chapter 4), including lifestyle education, but also in long-term and palliative care including caregiver and patient self-management education interventions (Chapter 7). In addition, skill-mix strategies involving peers and family caregivers were introduced and evaluated for patients with long-term care conditions and at the end-of-life (Chapter 7).
Population groups covered
Patients with chronic conditions were the main target population of skill-mix changes, which is mirrored with the high number and burden of diseases among this population group. In particular, skill-mix changes were frequently introduced and evaluated for patients with cardiovascular diseases, cancer, diabetes and mental health conditions. The population groups covered with regard to health promotion were primarily children, pregnant women, mothers and newborn infants, often with a socially or economically deprived status. Patients with acute care conditions most frequently suffered from stroke, acute myocardial infarction or other acute episodes, usually of chronic conditions. There was comparatively less research evidence on the outcomes of skill-mix interventions for patients specifically with minor acute illnesses, for example, influenza, pharyngitis, small wounds or other minor illnesses. More evidence is needed in these areas, because several countries have introduced skill-mix reforms that also focus on a new division of work, whereby physicians take care of patients with complex conditions and nurses or other professionals provide care for patients with minor conditions.
Interventions aiming at expanding access to health services were mainly targeted to vulnerable population groups, including socially or economically deprived groups. Skill-mix changes aimed at improving long-term and palliative care focused primarily on older people with dementia, Parkinson’s disease, as well as patients with (end-stage) cancer and other conditions at the end of life. The majority of the reviews described the population groups, however, few exceptions existed.
Study designs and country coverage
Most systematic reviews included randomized controlled trials (RCTs), controlled before–after studies, and several also covered cross-sectional study designs, which were conducted in several countries across Europe and North America. Generally, a high number of studies were conducted in the USA and Canada and within Europe, mainly in the United Kingdom, the Netherlands, Belgium, Spain and Sweden. The wide country coverage applies to several skill-mix interventions, including advanced roles for nurses or midwives to improve maternal and child health (in 24 countries; Chapter 4), transitional care-management roles delivered by nurses and pharmacists (15 countries; Chapter 5) and skill-mix models for health screenings (Chapter 4), which has been evaluated in many countries worldwide.
Interestingly, in contrast, the role of community health workers or similar community-based workers with some, albeit limited, training was primarily studied in the USA and much less in Europe. The question arises why this group is less represented in Europe. Some countries have trained peer workers to improve access for vulnerable groups, for example in Australia, Canada, the United Kingdom and the USA. However, their roles and contribution were much less frequently evaluated. Community-based interventions to improve access and facilitate communication involving lay and qualified health workers were often limited to the USA and Canada (Chapter 8).
Summary of research evidence available
In sum, the generally high quantity of research evidence – particularly on chronic conditions and health promotion and prevention – comes at a time when the policy attention is high globally to identify effective strategies to ensure a sustainable health workforce as a prerequisite to achieve or maintain universal health coverage. The high number of systematic reviews alone and the additional research evidence identified illustrate the strong research focus and are matched with a high policy interest in this field on how to strengthen the health workforce to improve access and quality of care (United Nations, 2016; World Health Organization, 2018). Yet, there remain evidence gaps or shortcomings for some areas, including on skill-mix innovations to improve access in rural and underserved areas and in the field of palliative care.
2.2 Evidence on outcomes: what skill-mix interventions are promising?
The following section provides an overview of the main themes of the skill-mix interventions and a snapshot of the evidence on outcomes. Although a full synthesis of the evidence is provided in each of Chapters 4–8, this section will highlight those interventions of particular interest and with promising results. For a full account of all interventions, we refer the reader to the respective chapters.
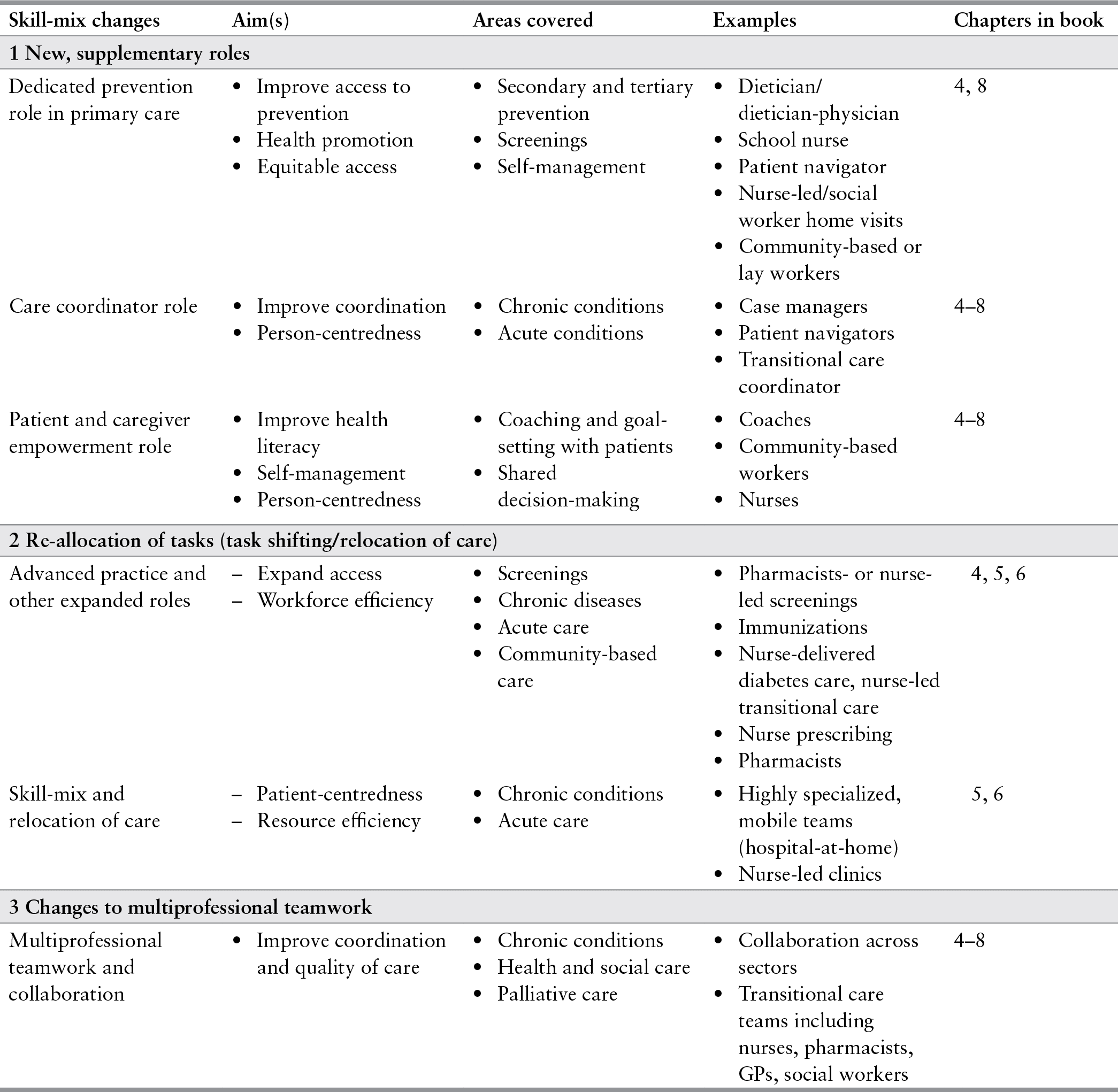
The main skill-mix interventions or models emanating from the literature and country experiences were as follows (Table 2.3):
first, new, supplementary roles for primary care providers,
second, the re-allocation of tasks between providers (involving advanced practice for non-physician providers), and
third, changes to multiprofessional collaboration.
The expansion of new, supplementary roles was implemented particularly to step up health promotion and prevention in primary care and to improve the care for patients with chronic conditions. Task re-allocation was most common in expanding screenings as well as for patients with acute care and chronic conditions. Changes to teamwork and multiprofessional collaboration were commonly introduced for various patient groups and care segments, but most notably for patients with chronic conditions. Moreover, several skill-mix changes were directly aimed at improving the coordination and continuity of care, models included case management roles, patient navigators and transitional care roles. Finally, some skill-mix changes were directly related to new service delivery models aimed at relocating care, for instance hospitals-at-home, requiring new, highly specialized teams.
Table 2.3 Major themes identified: skill-mix innovations
| Skill-mix changes | Aim(s) | Areas covered | Examples | Chapters in book |
|---|---|---|---|---|
| 1 New, supplementary roles | ||||
| Dedicated prevention role in primary care |
|
|
| 4, 8 |
| Care coordinator role |
|
|
| 4–8 |
| Patient and caregiver empowerment role |
|
|
| 4–8 |
| 2 Re-allocation of tasks (task shifting/relocation of care) | ||||
| Advanced practice and other expanded roles |
|
|
| 4, 5, 6 |
| Skill-mix and relocation of care |
|
|
| 5, 6 |
| 3 Changes to multiprofessional teamwork | ||||
| Multiprofessional teamwork and collaboration |
|
|
| 4–8 |
Abbreviations: GP: general practitioner.
Skill-mix changes introducing new, supplementary roles
Dedicated prevention role
New, supplementary roles have been introduced in several countries and regions worldwide with the aim of improving access, especially in the field of preventive care and health promotion. Expanding prevention roles of primary care providers has been increasingly recognized, bringing individual health promotion and prevention closer to and integrated into primary care.
Primary care providers are central in providing individual health promotion and prevention activities, this was also demonstrated by the systematic reviews. In these reviews, they took on supplementary roles to promote healthy diets and physical activity or deliver interventions targeting various risk factors. Nurses, pharmacists, dieticians and GPs performed diet-related health advice in school settings including education and counselling to school children and their parents (Reference Bhattarai, Prevost and WrightBhattarai et al., 2013; Reference Schroeder, Travers and SmaldoneSchroeder, Travers & Smaldone, 2016). Moreover, various professions performed counselling, and provided advice and motivational interviewing to increase physical activity in sedentary adults (Reference Orrow, Kinmonth and SandersonOrrow et al., 2012), among other interventions. Dedicated prevention roles covered various skill-mix interventions across several countries, but the majority of the findings demonstrated a positive effect on prevention-related outcomes. Outcomes included significantly reduced body mass index scores for adults and children, increased dietary intakes of healthy food (for example, vegetables and fruits) and physical activity (Chapter 4).
Home visits were common skill-mix interventions implemented to reach out to specific groups, particularly to vulnerable populations. The professions conducting home visits ranged from qualified professions (including nurses, social workers and midwives) to lay or lower-qualified workers (including community health workers and other lay workers). The tasks performed varied considerably within and across the professions covered. Generally, higher qualified professions also performed more specialized tasks – including with a focus on clinical tasks. Lay workers provided generally no or very limited clinical tasks, but instead focused on providing general information and health advice. The home visits were often tailored to the needs of specific target populations and involved multilingual advice, counselling and referrals, and were sometimes combined with transport services or phone calls. In particular, the multicomponent approaches showed positive effects in terms of expanding access to services.
Innovative skill-mix interventions were targeted towards preventing child maltreatment and reducing health disparities and demonstrated significantly improved patient-related outcomes and significantly reduced health care utilization, such as emergency care use or hospital (re-)admissions (Chapter 4 and Chapter 8). Most studies adding supplementary roles to perform outreach and educational activities showed promising effects towards increasing the access to screening services and earlier treatment (Chapter 8). Cost savings were reported for maternity home visits to prevent child maltreatment (Reference Dalziel and SegalDalziel & Segal, 2012), but were based on estimates and modelling; hence, require more research including costing studies and cost-effectiveness analyses to arrive at a more robust evidence base (Chapter 4).
Care coordinator roles and skills
Many countries have health systems that are fragmented and not well coordinated, particularly for people with chronic conditions and with highly complex care needs. Several skill-mix changes have been introduced establishing new roles to explicitly improve the coordination of care. Two models emerged, either new roles at the interface of hospital and ambulatory care sector, often as a one-off activity; or along the patient pathway as a supporting and coordinating role over a longer period of time. Coordinator roles have been established in many high-income countries, including virtually all European countries; however, the terms used and professions working in these roles vary considerably (care coordinator, case manager, transition coordinator).
New roles focusing on the transition, specifically from hospital to ambulatory care, were mostly referred to as transition coordinators, navigators or various terms related to discharge management. These roles were central for patients with often severe or multiple conditions who were close to discharge and they were aimed at improving the continuity of care from hospital to ambulatory care. Examples are provided in Chapter 5. Skill-mix interventions often comprised multiple components including discharge planning, patient education, medication reconciliations and sometimes home visits. These roles were primarily performed or led by nurses, including advanced practice nurses and other specialized nurses, pharmacists or sometimes social care workers. The new roles actively managed the early transitioning of care to the ambulatory setting. Introducing new roles in transitional care overall showed positive effects on at least one patient-related or health-system-related outcome. However, whereas patient satisfaction, patients’ knowledge about the disease and self-management improved, findings on mortality and health-system-related outcomes, such as readmissions and service utilization, showed mixed results (Chapter 5).
To improve the coordination of care and patient centeredness over a longer period of time, new roles in care coordination – in particular case manager roles – were undertaken. These roles were most frequently performed by nurses and/or pharmacists depending on different country and care contexts. Case management roles focused on patients with chronic diseases, with major acute conditions or with long-term care needs, in particular patients with dementia. More detailed information is provided in Chapter 5 (acute care), Chapter 6 (chronic care) and Chapter 7 (long-term and palliative care). For patients with mental health problems, interdisciplinary care coordination showed significant improvements in mental health outcomes (Chapter 6).
Introducing case management in the community setting for long-term care patients and their caregivers showed some improvements, nonetheless, the evidence remains mixed for most outcome parameters (Chapter 7). Patients with dementia showed reduced feelings of isolation and embarrassment of the condition after case management roles were introduced that focused on counselling, coordinating, monitoring, assessing and educating. Yet, evidence on other outcomes such as mortality, depression and functional status remained inconclusive (Reference Backhouse, Ukoumunne and RichardsBackhouse et al., 2017; Reference Goeman, Renehan and KochGoeman, Renehan & Koch, 2016; Reference Khanassov and VedelKhanassov & Vedel, 2016; Reference Khanassov, Vedel and PluyeKhanassov, Vedel & Pluye, 2014; Reference Pimouguet, Lavaud and DartiguesPimouguet, Lavaud & Dartigues, 2010; Reference Reilly, Miranda-Castillo and MaloufReilly et al., 2015). The reasons for these mixed, and therefore inconclusive results, are unknown and may be influenced by multiple factors: the intervention itself and differences in the intensity of the interventions, the different roles and professions involved. It may also be related to the fact that the severity of the condition (for example, dementia) has less potential for improvements in clinical outcome measures than if compared with case management skill-mix interventions for patients with acute or stable chronic conditions.
Patient navigator roles were widely implemented and researched, encompassing different tasks such as coordinating, discharge planning, educating and follow up. The patient navigator role was evaluated for cancer patients (Chapter 6), for whom the new role originally emerged. Patient navigators were also introduced for patients with acute conditions and to facilitate the access to screenings, especially for vulnerable population groups (Chapter 5 and Chapter 8). Patient navigators were shown to be health professionals with professional education, but they sometimes also involved former patients/peers, community health workers or other lay workers with some training acting as navigators through the system, particularly for vulnerable groups.
Patient navigators were particularly crucial in overcoming language barriers for vulnerable patients with limited language proficiency. Improved uptake of screenings and completion of diagnostics illustrated the positive impact of patient navigation for vulnerable patients (Chapters 4 and 8). Moreover, community health workers acting as patient navigators to improve chronic disease management showed significant positive effects regarding health outcomes for disadvantaged patients (Chapter 8).
Skill-mix to empower patients and caregivers
Empowering patients and their caregivers in the self-management of their conditions has received policy attention over the past decade as a cost-effective strategy to support self-care and person-centred care of people. Several skill-mix interventions have specifically targeted patient self-management and empowerment. Skill-mix interventions result in extended roles and new tasks, for example, providing (tailored) educational activities, motivational interviewing or coaching, consultations and self-management skills trainings. In the systematic reviews, these services were primarily provided by nurses, pharmacists or peers for patients with single chronic conditions. Overall, these interventions fostering patient autonomy in the care process showed positive effects on several health outcomes including on blood pressure and glycated haemoglobin (HbA1c) levels (Chapter 6).
Introducing peer educators was another common skill-mix intervention. Peer educators are “peers”, defined as other patients usually with the same condition, often with no health profession-specific background but with extensive knowledge on the disease and having received additional, short trainings to serve as peer educators. The advantage is that they have often had a similar experience as patients in the health system. Peer educators, who have regular contact with patients, have been shown to positively impact health or peer-related outcomes (Chapter 6). For example, a peer support model for diabetes patients, which comprised face-to-face management, peer coaching and phone-based support, showed improvements in blood pressure, body mass index and physical activity, among other positive health-related outcomes (Reference Dale, Williams and BowyerDale, Williams & Bowyer, 2012).
For vulnerable groups, community health workers, peer counsellors or professionals with various other backgrounds emerged as a common intervention across the systematic reviews resulting in primarily positive outcomes for patients. Lay and community-based workers focused on education and navigation assistance, usually collaborating with other health professionals (Chapter 8). Interventions delivered by community health workers, who worked alongside other professionals such as nurse case managers and psychologists, showed significant improvements in the management of chronic diseases including positive effects on blood pressure levels and cardiovascular disease risk reduction (Reference Kim, Choi and ChoiKim et al., 2016). Similarly, lay health workers and peer counsellors assisting mothers and their children with low socioeconomic status through home visits, reminders, education and the facilitation of meetings indicated reduced child mortality and morbidity. Additionally, the interventions increased the uptake of immunization rates as well as the likelihood for women to seek care for childhood sicknesses (Reference Lewin, Munabi-Babigumira and GlentonLewin et al., 2010).
Interventions to support and strengthen patients and their caregivers in long-term care encompassed assessing the specific needs, planning of support interventions, monitoring, coaching and counselling (Chapter 7).
Pain management targeted at patients in palliative care and their family caregivers covering different components such as face-to-face education and follow ups demonstrated significantly improved medication adherence; yet, showed mixed results on caregivers’ knowledge, for example, about pain management.
Skill-mix on re-allocation of tasks and new division of work
Many reviews analysed skill-mix and the re-allocation of tasks resulting in a new division of work between health professionals. Most prominent was the model of advanced practice providers (such as advanced practice nurses, as well as pharmacists in advanced practice roles). Other models covered the re-allocation of tasks from health professions (physicians, nurses, pharmacists) to lower qualified assistants (medical assistants, nursing assistants) or from health professionals to lay workers or patients. This new division of work usually involved task-shifting, whereby specific tasks or roles are shifted from higher to lower educated professions (European Commission, 2019). The overarching aim of task-shifting is to expand access to services, with increased workforce efficiency, work flows and/or other parameters. Task shifting covered at least two professions or workers, and usually occurred as forms of collaboration.
Advanced practice roles among nurses, pharmacists and other professions
Skill-mix models in the literature frequently analysed the effects of advanced practice roles of nurses or pharmacists, performing an expanded set of tasks, traditionally provided by physicians or other health professionals. Other professions covered were physiotherapists or dental hygienists working in expanded roles. Advanced roles ranged from introducing advanced practice providers, with a considerably expanded scope-of-practice (for example, advanced practice nurses including nurse practitioners with usually at least a Master’s degree; or pharmacists) to the expansion of a limited set of additional tasks, such as for nurses or dental hygienists. This practice was found across almost all different care segments in the overview of reviews. In health promotion and prevention, advanced practice nurses (for example, nurse practitioners) or professional nurses performed screenings and skin cancer assessments and examinations.
For instance, nurses in advanced practice roles delivering skin cancer screening showed higher sensitivity to identify malignant lesions compared with physicians or general and expert dermatologists (Reference Loescher, Harris and Curiel-LewandrowskiLoescher, Harris & Curiel-Lewandrowski, 2011). Nurse-delivered colorectal cancer screenings detected higher rates of adenomas, and were shown to result in lower costs compared with physician-led services (Reference Joseph, Vaughan and StrandJoseph, Vaughan & Strand, 2015). This is one example whereby nurse-led screenings were associated with reduced costs; however, to date the evidence on nurse-led screenings on costs is scarce and requires more cost-effectiveness studies (Chapter 4).
The highest number of reviews focused on task shifting and a new division of work for chronically ill patients. Nurses and pharmacists took on considerably advanced roles, which had traditionally been performed by physicians. One model was nurse-led care, defined as nurses leading the treatment and care process for a defined group of patients, like with diabetes. Nurse-led care included a wide range of different components such as prescribing of medicines, management of medication adherence, disease management or education. Models ranged from delivery either autonomously or in collaboration with other health professionals, usually with physicians. Nurse-led care for single chronic diseases indicated better or equivalent health outcomes compared with usual care (mainly physician-provided), in particular for titration and medication adherence (Reference Parker, Maresco-Pennisi and CliftonParker et al., 2016; Reference Shaw, Mcduffie and HendrixShaw et al., 2013), yet, nurse-led care revealed insufficient evidence for health system outcomes and cost effectiveness. Inconclusive findings were demonstrated for multimorbidity (Chapter 6).
Pharmacists in expanded roles took over tasks from physicians such as health screenings, immunizations and monitoring medication adherence. Pharmacists delivering care for patients with chronic conditions were shown to positively influence cardiovascular disease outcomes such as blood pressure in several systematic reviews (Reference Blalock, Roberts and LauffenburgerBlalock et al., 2013; Reference Cheema, Sutcliffe and SingerCheema, Sutcliffe & Singer, 2014; Reference Fazel, Bagalagel and LeeFazel et al., 2017; Reference Greer, Bolduc and GeurkinkGreer et al., 2016; Reference Morgado, Morgado and MendesMorgado et al., 2011; Reference Nkansah, Mostovetsky and YuNkansah et al., 2010; Reference Tan, Stewart and ElliottTan et al., 2014; Reference Van Eikenhorst, Taxis and Van Dijkvan Eikenhorst et al., 2017). Moreover, evidence showed improvements in medication adherence for patients with hypertension (Reference Blalock, Roberts and LauffenburgerBlalock et al., 2013; Reference Cheema, Sutcliffe and SingerCheema, Sutcliffe & Singer, 2014; Reference Morgado, Morgado and MendesMorgado et al., 2011) and demonstrated reduced hospitalization, emergency department visits and costs for pharmacist-led chronic care (Reference Entezari-Maleki, Dousti and HamishehkarEntezari-Maleki et al., 2016; Reference Manzoor, Cheng and LeeManzoor et al., 2017).
Skill-mix interventions and task shifting practices were also identified for (minor) acute illnesses where pharmacists, physiotherapists and mid-level dental care providers had extended the scope of practices (Chapter 5). In the United Kingdom, pharmacy-based minor ailment consultations suggested less costly services than usual care delivered by GPs and an overall satisfaction among patients, GPs and pharmacists (Reference Paudyal, Watson and SachPaudyal et al., 2013). Positive effects regarding health outcomes were also reported for mid-level dental providers such as dental hygienists delivering care (Dasanayake et al., 2012; Reference Wright, Graham and HayesWright et al., 2013).
Skill-mix and relocation of care
The relocation of care settings comprised hospital-at-home, nurse-led clinics if provided in a new setting and palliative care at home interventions. Hospital-at-home services are defined as highly specialized services at patients’ homes for individuals who would usually require hospitalization for their condition. Three systematic reviews including two Cochrane Reviews assessed hospital treatment at home by various health professionals in highly specialized teams (Reference Gonçalves-Bradley, Iliffe and DollGonçalves-Bradley et al., 2017; Reference Qaddoura, Yazdan-Ashoori and KabaliQaddoura et al., 2015; Reference Shepperd, Cradduck-Bamford and ButlerShepperd et al., 2017). One Cochrane review analysed home services delivered by a specialist respiratory nurse (Reference Jeppesen, Brurberg and VistJeppesen et al., 2012). Positive or no effects were reported for mortality rates across the reviews and mixed results were shown for readmission and patient outcomes. However, no negative outcomes were reported, suggesting that hospital-at-home may be a safe model of care provision, for instance for patients with acute respiratory conditions, provided that the professions are adequately trained, possess the right skills and perform close monitoring (Chapter 5).
Nurse-led cardiac clinics suggested a positive impact on the quality of care for patients with chronic conditions. Studies demonstrated that nurse-led clinics provided equivalent or better care compared with usual care or clinics run by other health professionals. To illustrate, significant improvements were found for mortality rates and equivalent effects for self-reported mental or physical health and hospitalization episodes compared with usual care (Reference Al-Mallah, Farah and Al-MadaniAl-Mallah et al., 2016; Reference Schadewaldt and SchultzSchadewaldt & Schultz, 2010). Similarly, nurse-led clinics for patients with multimorbidity indicated equivalent care compared to other clinics (Reference Clark, Smith, Taylor and CampbellClark et al., 2011) (Chapter 6).
While the number of systematic reviews on palliative care at patients’ homes was small, effects on pain management through interventions mostly delivered by teams or in collaboration showed improved pain-related outcomes. Palliative teams were composed of nurses, psychologists and researchers and targeted patients and their caregivers in palliative care. Improved caregiver satisfaction and lower caregiver burden were reported for implementing case managers and multidisciplinary collaboration models. Additionally, health system outcomes such as hospital admission and length of stay and profession-specific outcomes including communication and service relationships suggest positive impacts of palliative care delivered at patients’ homes (Chapter 7).
Changing teamwork and collaboration
Skill-mix interventions involving teamwork and collaboration were identified across all care segments included in the study, ranging from health promotion, prevention to long-term and palliative care. Teamwork took various forms, for example, multiprofessional teams, shared care whereby two professionals worked closely together sharing tasks, as well as networks of care providers and multiprofessional clinics.
Skill-mix interventions involving multiprofessional teams for chronic conditions and multimorbidity evaluated different ways of collaboration such as consultation liaison, joint care coordination or shared care performed by various professions, and was compared with usual care generally provided by physicians alone (Chapter 6). For consultation liaison involving collaborative care between physicians and specialists, moderate positive effects on physical health outcomes was demonstrated (Reference Foy, Hempel, Rubenstien and SuttorpFoy et al., 2010; Reference Mitchell, Burridge and ZhangMitchell et al., 2015). There was evidence that collaborative care involving mental health specialists and primary care providers improved mental health outcomes, patient satisfaction and quality of life (Reference Archer, Bower and GilbodyArcher et al., 2012; Reference Coventry, Hudson and KontopantelisCoventry et al., 2014). Reduced utilization of inpatient care and other health care services was shown for other multiprofessional care models such as primary care provider networks (Reference Carter, Riverin and LevesqueCarter et al., 2016) and multiprofessional cardiac clinics (Reference Gandhi, Mosleh and SharmaGandhi et al., 2017). Collaborative care targeting patients with multimorbidity showed improved adherence to medication and health outcomes; but, little or no evidence on cost savings.
Overall, the reviews suggest that multiprofessional care models can have a positive effect for patients with mental health problems and multimorbidity (Chapter 6).
Skill-mix interventions provided by multiprofessional teams were frequently reported for transitional care and early discharge planning. For instance, transitional care teams focused on care transitioning across different care settings including the inpatient/ambulatory interface and different phases of life (paediatric to adulthood). The evidence on transitional care involving various professions demonstrated positive effects on selected patients and health system outcomes; however, not all reviews and underlying studies differentiated between multiprofessional and single-profession interventions (Chapter 5)
In long-term care, multiprofessional community mental health teams and collaborative models were evaluated. Multiprofessional community mental health teams were composed of mental health nurses, social workers, psychologists, consultant psychiatrists and GPs. The mental health teams provided intensive care management and team diagnosis.
Multiprofessional collaboration models included interventions such as shared care plans and joint decision-making. Although the evidence was limited because it covered only a few studies, introducing multiprofessional teams for long-term conditions such as mental health or Parkinson’s disease were suggested to improve quality of life and function and mobility rates. Intensified collaboration among health professionals delivering care for patients in palliative care also demonstrated positive effects on patients and their caregivers, but was limited to few individual studies (Chapter 7).
2.3 Strength of the evidence and limitations
The overview of reviews has synthesized a considerable body of evidence on the different skill-mix interventions (for example, addition of new roles in prevention, task-shifting and new division of work in chronic care, multiprofessional teams) which have been evaluated across various countries. However, the evidence base differed across the care segments.
The outcome measures were clustered into three main categories – patient-related, health system and profession-specific. A large number of reviews reported outcomes on patients (individual health outcomes), but outcomes on health systems, costs and the professions themselves remained scarce. There was considerable heterogeneity in the outcome measures across the systematic reviews. A high number of reviews performed meta-analyses related to single chronic conditions, but in all other areas covered, the number of meta-analyses was considerably smaller and mostly narrative syntheses were performed, because of the heterogeneity of the outcome measures. The variations between outcome measures across individual studies limited their comparability. Several skill-mix interventions were multicomponent and sometimes included non-skill-mix-related changes, which limits the attribution of causality.
The study faces several limitations. First, only systematic reviews published as of 2010 were included. One reason is that the study aimed to cover skill-mix innovations, defined as a novelty in its widest sense, including the time dimension of publication. An additional reason was the feasibility of conducting the overview of reviews. It needs to be noted that there may have been systematic reviews published before 2010 on skill-mix interventions that may have been missed, although the likelihood is estimated to be low. Second, individual studies were not covered; RCTs in particular or other study designs that were recently published may have been missed. Third, although many of the included systematic reviews described the professions involved in the skill-mix interventions and how their roles changed, several reviews did not sufficiently describe the professions, their roles and tasks covered in the intervention group, particularly when it involved teams. Instead terms like “various professions”, “multidisciplinary teams” or “care teams” were applied. Another limitation of the reviews and underlying studies was that the comparator groups were rarely described in detail. Therefore, professions as well as the specific roles and tasks covered often remained insufficiently reported; the comparison groups were sometimes simply referred to as “usual care”. One additional limitation was that the education of the professionals was rarely described, which is essential with regards to implementation considerations.
The findings need to be interpreted in light of these limitations. However, this study is the first of its kind that synthesized the evidence of skill-mix changes on individuals, health systems and professions, covering all health professions as well as lay workers and informal caregivers in primary and ambulatory care settings. It shows that there are several promising skill-mix models to improve the quality of care and access to services.
2.4 Transferability of the findings
Some skill-mix changes work well for a defined population group, in a specific country or setting, but not in others. Assessing the transferability of a proven skill-mix intervention is therefore critical. At the same time, the question of transferability is highly complex and context specific. This volume does not suggest that an innovation can or should be easily replicated without considering how it can fit different contexts and needs. Instead, it suggests that decision-makers identify the different existing skill-mix strategies that have been identified to address a specific health need, skills gap or workforce challenge and evaluate which elements could work in the specific setting and context.
Bearing this in mind, some skill-mix models have been shown to work well in multiple contexts and been associated with positive health outcomes. This includes introducing new, dedicated prevention and health promotion roles for nurses or pharmacists in ambulatory care and community settings (Chapter 4). Expanding the roles and scope-of-practice for nurses and pharmacists to care for patients with chronic conditions (also referred to as task shifting) was found to be effective in a large number of different countries and contexts (Chapter 6). Expanding the roles for nurses, midwives or community-based workers to reach out to women and their children also shows a promising skill-mix model in several countries (Chapter 8). Introducing a care coordinator function, particularly at the hospital-to-community transitioning interface and for patients with high needs, shows promise, but it remains unclear by which profession and what level of intensity is required for which patient groups (Chapter 5). There remains insufficient evidence for which exact roles and tasks should be performed by what profession and the educational needs required to develop the new skills and roles. Finally, on effective teamwork and outcomes, the evidence remains limited.
Decision-makers can use the evidence synthesis to understand what skill-mix model involving which profession(s) and interventions has worked for what population group in which countries. Yet, when considering implementation of a skill-mix change, assessment of several transferability and implementation questions is critical:
First, has this model been evaluated in the country, at minimum in pilots or small-scale programmes? Will new changes be externally evaluated?
Second, are the skill sets of the concerned profession(s) available or are other professions or workers better suited to perform these roles in a specific setting? Are there sufficient professionals to ensure going to scale within the planned time period? Is additional education and training a requirement to ensure that the new roles can be performed with good quality?
Third, what are the regulatory mechanisms and oversight requirements to ensure patient safety?
Fourth, how is financing and payment impacting on the new roles?
And finally, what communication strategies are effective to inform and involve patients, other health professions, managers and other key stakeholders to ensure the transfer and piloting of new skill-mix models and their evaluation.
Hence, the transfer and implementation of a specific skill-mix intervention is not only influenced by the governance and organization of a health system. Profession-specific regulatory mechanisms also play an important role, the educational system, the influence of the stakeholders involved and the political force field. These factors are critical for generating an inducive environment to support the implementation of skill-mix innovations and reforms. These factors influencing the implementation process will be addressed in Chapter 3.
2.5 Conclusions
The main skill-mix interventions identified in the overview of review focused on new, supplementary roles, new division of work (task shifting and relocation of care) and teamwork (multiprofessional teamwork and collaboration). Several examples for innovative skill-mix changes have demonstrated a positive impact on the quality of care or on the access to health services. Examples are as follows: (i) establishing a dedicated prevention role for population groups or individuals with at-risk factors; (ii) task shifting and new division of work in teams whereby nurses or pharmacists take up clinical tasks from physicians and take over certain patient groups; (iii) care coordinator roles (for example, case managers, transitional care coordinators) for patients with chronic or acute conditions and multiple needs; (iv) patient navigator roles or peers to educate, enhance health literacy and empower individuals, particularly vulnerable groups.
Although the overall body of evidence on skill-mix is remarkable, there remain several research gaps. Except for nurses and pharmacists, the evidence on other professions involved in skill-mix changes and outcomes is less well established. There is considerable evidence across many countries that task shifting between physicians and nurses or pharmacists can lead to equivalent or improved quality of care. Yet, the evidence on costs is mixed and inconclusive. There is generally a scarcity of research on skill-mix changes and effects on health systems and costs. Very limited high-quality evidence is available on the effects of skill-mix changes on the professions themselves. Evidence on teamwork and division of work is mixed. Implementation research is required to evaluate the new roles individually and as part of teams to demonstrate health outcomes, team effectiveness and satisfaction, as well as cost-effectiveness.
What can be concluded from the existing research, however, is as follows: dedicated prevention and health promotion roles performed by qualified health professionals showed promising results on patients’ lifestyle, physical activity and diet. The prevention role often reached out into communities. Some models also included home visits, undertaken by health professionals themselves or in collaboration with lay health workers or peers. The evidence suggests that skill-mix changes focusing on establishing a specific, dedicated prevention role can improve health outcomes, particularly if integrated in primary health care or communities. Often the focus was on vulnerable population groups, which required tailored services. However, determining which profession should undertake this role is highly country and context specific. Countries should step up such a new role to maximize health gains for individuals and population groups and integrate these new roles in communities and health systems.
In addition, promising skill-mix changes are care coordinator roles at the hospital–ambulatory care interface for acute, high-needs patients or in ambulatory care. They were prominent for various patient groups, including for patients with single chronic conditions, multimorbidity, acute episodes of care and long-term and palliative care needs. Case management interventions yielded mixed results, due to the heterogeneity of patient groups, conditions and outcome measures. For patients with cancer or at risk of developing cancer, patient navigation interventions overall showed promising results on patients’ health and access to services, particularly for socioeconomically disadvantaged individuals, migrants or other vulnerable groups. Introducing and training peers and lay health workers to empower patients and their caregivers were innovative interventions that contributed to improved patient outcomes across various care segments. Advanced roles of nurses and pharmacists were most frequently evaluated for task shifting and were found across all care segments in the systematic reviews. Additionally, extended scopesof-practice of physiotherapists and dental mid-level providers were also among the interventions. Most of the reviews covering new division of work showed generally positive patient and health-system-related outcomes if professionals were trained and possessed the right skills.
Skill-mix interventions involving teamwork and collaboration were identified across all care sectors. The interventions were manifold and ranged from multiprofessional teams to networks of primary care providers and clinics. Models covered either various health professions within ambulatory care or across sectors. Positive results were particularly reported for multiprofessional interventions for mental health care in collaboration with primary or other health professionals.
For policy-making, the study shows that there is cross-country evidence demonstrating that skill-mix changes have been widely implemented in Europe and beyond. The trend in many countries from solo physician practices to group practices and multiprofessional health centres has also reinforced new skill-mix developments. However, instead of transferring interventions from one country context to another with no consideration given to transferability, policy-makers should identify and evaluate what skill-mix changes best suit their specific context, population or patient group and intended health aim(s). In terms of which profession(s) to perform new roles to step up prevention, care coordination and the quality of chronic condition treatment, most countries equipped nurses and/or pharmacists with additional training and responsibilities, which showed at least equivalent quality of care. For other interventions, for example for long-term care, additional health workers and caregivers were trained to perform these roles. The aim was to make better use of the skills of nurses, pharmacists and other providers, but the evidence base on other professions is less strong. Each country should consider in its specific context which profession in which team configuration is most suited to provide preventive services, care coordination or other services that can improve access and quality of care for specific patient groups. Critical for implementation is how to integrate these new roles in the communities and health systems, close to the population group(s) targeted and identify how to strengthen the professionals’ capacity and training needs so as to perform these roles effectively.