Depression is the leading global cause of disability among young people aged 15–25 years.Reference Ferrari, Charlson and Norman1 A recent population study of over 600 000 US residents found that depression prevalence was not only greatest among those aged 12–25 years, but had also risen over the past 10 years in this group.Reference Weinberger, Gbedemah, Martinez, Nash and Galea2 Ineffective management of depression can set up a young person for a lifetime of recurrent episodes and associated functional impairments, including academic underperformance and failure to attain adult milestones (e.g. career progression, independent living).Reference Peters AT and Jacobs3
Existing treatments for depression in young people are effective, but have a number of drawbacks. First, psychopharmacological options that constitute front-line depression treatment among adults have lower efficacy and adherence among young people.Reference Cipriani, Zhou and Del Giovane4 Studies have suggested that young people and their parents prefer non-drug treatments for depression.Reference Jaycox, Asarnow, Sherbourne, Rea, LaBorde and Wells5 Unfortunately, psychotherapeutic treatment efficacy is more modest in young people than in adults. One meta-analysis found that effect sizes of cognitive–behavioural therapy (CBT) for depression were 30% smaller for children and/or adolescents than for adults.Reference García-Escalera, Chorot, Valiente, Reales and Sandín6 Another meta-analysis included samples with a mean age of less than 18 years and found that CBT for depression was effective in this population but had a smaller effect size (g = 0.35) than in adults and was no better than other forms of psychotherapy.Reference Weisz, McCarty and Valeri7
Loneliness as a target of treatment
There is a need for innovation in depression treatment, particularly among young people, with an emphasis on strategies that not only improve symptoms, but also reduce the risk of relapse. In seeking to address this need, a growing evidence base has pointed to the role of social and contextual factors in the development and maintenance of depression. In particular, loneliness has been identified as a particularly strong and robust risk factor in the onset, maintenance and relapse of depression.Reference Erzen and Çikrikci8 Loneliness is related to other constructs, such as social isolation, but distinctly captures the subjective absence of meaningful connections to others. Loneliness has probable causal links to mental illness and causes significant distress and impairment in its own right. Although most research evaluating loneliness interventions has been conducted with older people,Reference Masi, Chen, Hawkley and Cacioppo9 loneliness is more common among young people.Reference Mance10
Previous trials of interventions targeting loneliness and its downstream mental health consequences have had mixed success, with a 2011 meta-analysis of loneliness interventions describing their benefit as ‘modest’.Reference Masi, Chen, Hawkley and Cacioppo9 This meta-analysis included 50 studies, and among the 20 randomised trials the average effect size was small (d = −0.19). Another review found that loneliness interventions conducted in group contexts tended to be more effective.Reference Cattan, White, Bond and Learmouth11
In the years since these reviews, Groups 4 Health (G4H) has emerged as a promising intervention for loneliness, with concomitant benefits for depression and general well-being.Reference Haslam, Cruwys, Haslam, Dingle and Chang12,Reference Haslam, Cruwys and Chang13 G4H is a manualised group therapy programme founded on the social identity theoretical framework. It seeks to increase group-based belonging using a combination of educational, psychotherapeutic and behavioural strategies. In a phase 2 randomised controlled trial (RCT) published in 2019 with 120 participants reporting loneliness and mental illness, G4H outperformed treatment as usual in reducing loneliness (d = −1.04) at 4-month follow-up and performed comparably to treatment as usual in reducing depression (d = −0.63).Reference Haslam, Cruwys and Chang13 Two relevant meta-analyses were also published in 2019. The first found a negative association (r z = −0.15) between social identity and depression in 76 (mostly correlational) studies.Reference Postmes, Wichmann, van Valkengoed and van der Hoef14 The second evaluated the efficacy of interventions that build social identity, including G4H.Reference Steffens, Larue and Haslam15 Among the 27 studies identified, 8 included depression as an outcome variable, with an average effect size of g = −0.58. This emerging evidence base suggests that social identity-based interventions, and G4H in particular, show promise in reducing loneliness and depression.
What is not known, however, is how these beneficial effects of G4H on depression compare with best-practice evidence-based treatment for young people: CBT. For G4H to be widely implemented in practice, it needs not only to perform strongly on loneliness relative to treatment as usual, but also to show benefits for depression that are not inferior to gold standard treatment. It is also crucial that the relative benefits of these interventions are assessed over both the short and longer term, because depression tends to follow a relapsing–remitting pattern.
The current study
The overarching aim of this study was to compare G4H with CBT on primary outcomes of loneliness and depression across a 1-year follow-up period. We conducted a phase 3 RCT in which young people were recruited from mental health services and assigned to receive either G4H or a dose-controlled manualised format of group-based CBT. Our hypotheses were as follows.
(a) Hypothesis 1: at programme completion G4H would be superior to CBT in reducing loneliness. This hypothesis would be considered supported if there were evidence of significant improvements in loneliness in the G4H condition (hypothesis 1(a)) and a significant condition × time interaction, such that improvements in loneliness over time were greater for the G4H condition than for the CBT condition (hypothesis 1(b)).
(b) Hypothesis 2: at programme completion, G4H would be as effective as CBT in reducing symptoms of depression (i.e., be non-inferior). This hypothesis would be considered supported if there were evidence of significant improvements in depression in both conditions, with a non-significant condition × time interaction. The non-inferiority margin was a depression change score difference of 2.20 on the 21-item Depression Anxiety Stress Scales (DASS-21) (see protocolReference Cruwys, Haslam, Walter, Rathbone and Williams16 for details of calculation).
(c) Hypothesis 3: the benefits of G4H for loneliness and depression would be sustained at 12-month follow-up. This hypothesis would be considered supported if there were no significant increase in depression and loneliness scores between 6-month and 12-month follow-up in the G4H condition.
Method
Study design
The study was a randomised phase 3 non-inferiority trial with 12-month follow-up. The trial profile is provided in Fig. 1. SPIRIT and CONSORT guidelines were followed. The trial was conducted at two mental health services in South-East Queensland, Australia: a community-based youth mental health service (headspace) and a university-based psychology clinic (University of Queensland clinic). A total of 26 therapy groups were completed (13 of each type). The trial recruited 15- to 25-year-olds because this corresponds to the population mean age of depression onset and peak prevalence.Reference Peters AT and Jacobs3
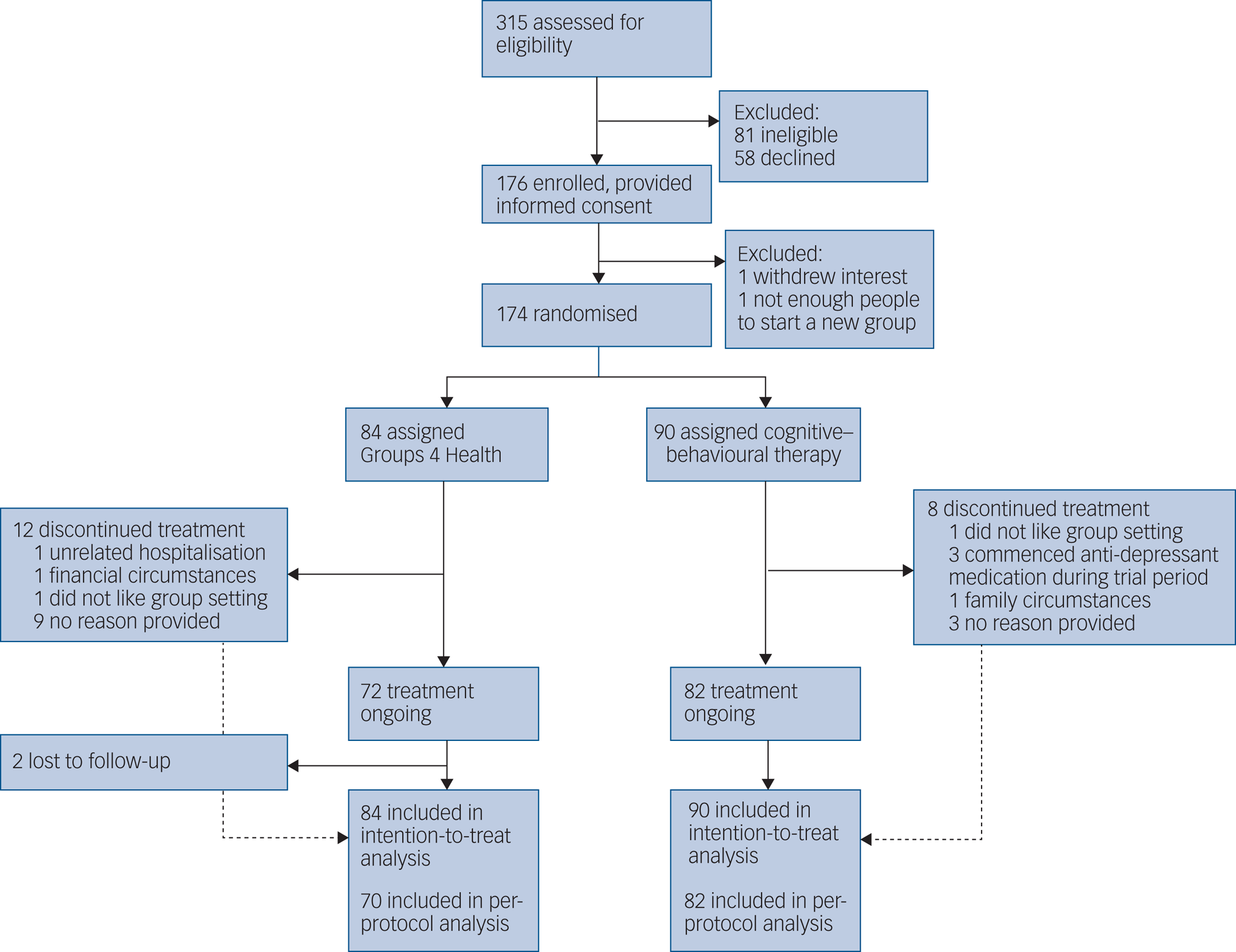
Fig. 1 Trial profile. All 174 randomised participants were invited to participate in the follow-up assessments, and so 17 of the 22 participants who discontinued have outcome data available for inclusion in the intention-to-treat analysis.
Written informed consent was obtained from all participants. For young people aged under 16 who wished to participate, parental consent was also sought in accordance with the organisational policy of the healthcare services where the group therapy was taking place. The authors assert that all procedures complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures were approved by the Brisbane Metro South Human Research Ethics Committee (HREC/18/QPAH/54), ratified by the University of Queensland Human Research Ethics Committee (#2018000420), and were prospectively registered on the Australian New Zealand Clinical Trial Registry (ACTRN12618000440224) on 27 March 2018. The published study protocol is available.Reference Cruwys, Haslam, Walter, Rathbone and Williams16
Participants
Participants were 174 young people seeking mental healthcare. Table 1 shows baseline characteristics of the sample. The sample ranged in age from 15 to 25 years, with an average of 18.94 years (s.d. = 1.96); 131 participants were female (75%) and 43 were male (25%).
Table 1 Baseline characteristics of the intention-to-treat population of 15- to 25-year-oldsa
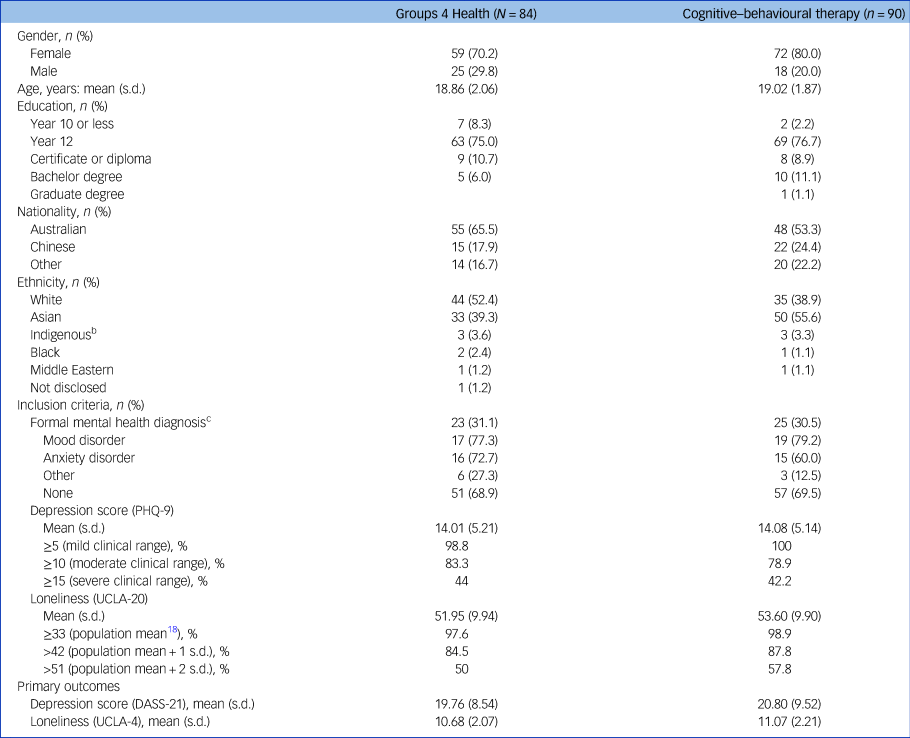
PHQ-9, 9-item Patient Health Questionnaire; UCLA-4, 4-item UCLA Loneliness Scale; DASS-21, 7-item depression subscale of the 21-item Depression Anxiety Stress Scales.
a. T-tests (for continuous variables) and chi-square tests (for categorical variables) indicated no baseline differences between conditions were statistically significant (Ps > 0.135).
b. This category included people identifying as Aboriginal Australian, Torres Strait Islander and/or Maori.
c. People were prompted to skip this question if they did not wish to disclose, and more than 10% of the sample did so. Percentages provided here are a proportion of those who responded to this question, which likely underestimate the true proportion of participants with a formal diagnosis.
Individuals were invited to participate in the trial if they were subjectively experiencing low mood and loneliness. Inclusion criteria were: (a) aged 15–25 years and (b) English speaking, at a sufficient level to understand and engage with group discussions, with the presence of at least one of the following: (c) depressive symptoms of at least mild clinical impairment on the 9-item Patient Health Questionnaire (PHQ-9 score ≥5)Reference Spitzer, Kroenke and Williams17 or (c) a mental health condition diagnosed by a health professional (e.g. major depressive disorder) or (d) elevated loneliness on the 20-item UCLA Loneliness Scale (UCLA-20 score ≥40, approximately 1 s.d. above the mean for 16-year-oldsReference Shevlin, Murphy and Murphy18).
Exclusion criteria were: (a) receiving other concurrent evidence-based treatment for depression (psychopharmacological or psychological), (b) severe suicide ideation, (c) severe psychological symptoms that would interfere with ability to participate (e.g. psychotic episode, substance dependence/intoxication) and (d) severe neurological condition or intellectual impairment that would limit capacity to engage with the intervention. Participants were monitored by group facilitators for changes that might affect their eligibility (e.g. commencing adjunct treatment, suicidality).
Recruitment used a variety of strategies. Staff at each service were provided with referral information and directed individuals to the trial, particularly where they would otherwise be placed on a treatment waiting list. Postcards and posters were displayed at each service and also used to advertise the trial within the community and on university campuses to increase the representativeness of the sample from the intended population, rather than just those presenting to healthcare services.Reference Weisz, McCarty and Valeri7
To improve retention and data quality, participants were offered incentives for completing assessments at programme completion (Au$15 voucher), 6 months (Au$50) and 12 months (Au$50). Those who were enrolled in undergraduate psychology at the university where the trial was taking place were offered course credit.
Randomisation and masking
To reduce expectation effects, the non-inferiority focus of the trial was emphasised to participants (e.g. ‘We are investigating whether both treatments are equally effective’). After providing informed consent, participants were assigned to a numbered therapy group. Once a minimum number of participants had been recruited to commence a group (five people), the group (and all participants in it) was randomly allocated to G4H or CBT. Randomisation was conducted via a computer-generated random number in a 1:1 ratio.
Trial managers conducted group assignment and were not masked. Participants were masked to allocation until after they had confirmed their attendance. All other researchers were masked to allocation. Assessment at follow-up time points was conducted via an online questionnaire which was identical for all participants, to reduce experimenter bias. Invitations to complete the assessments were identical across conditions and were sent via email and SMS. Statistical analysis was conducted by the lead author without knowledge of allocation (i.e., the meaning of the condition codes (1 for G4H; 2 for CBT) was only provided after hypothesis testing was complete). All authors had access to the data and project files via a shared university drive. To ensure that masking was maintained, the non-masked trial database was password protected with access only possible for trial managers.
Procedures
Group facilitators were provisional psychologists completing a professional psychology graduate programme. In addition to their standard training in supportive counselling, risk assessment, and group therapy, all facilitators were provided with focused training to run the manualised programme that they were delivering (G4H or CBT), and 1 h/week supervision by a clinical psychologist with expertise in G4H or CBT. Adherence to the manualised programme was maintained via direct observation, weekly supervision, recorded focus groups with participants and facilitators after programme completion, and a validated anonymous questionnaire completed by facilitators after each session.Reference Haslam, Cruwys, Haslam, Dingle and Chang12,Reference Haslam, Cruwys and Chang13
Groups 4 Health
Groups 4 HealthReference Haslam, Cruwys, Haslam, Dingle and Chang12 is a psychotherapeutic programme that seeks to reduce loneliness by building group-based belonging. It is delivered in groups of five to eight people and comprises five sessions of approximately 75 mins each. Session content is informed by social identity theorising. Participants first learn about the importance of social connectedness and group-based belonging for health (session 1). They are then guided to develop a visual ‘social identity map’ to gauge current group belonging (session 2), before developing goals and plans for engaging with existing groups (session 3) and for joining new groups (session 4). These are delivered weekly, before participants meet 1 month later to review their progress and goals (session 5).
Cognitive–behavioural therapy
The comparison condition was dose-controlled manualised group-based CBT for depression: the Blues Program.Reference Stice, Burton, Bearman and Rohde19 Minor manual adaptations were made to match the timing and amount of face-to-face contact to that provided in G4H: the 6 × 60 min format was adapted to a 5 × 75 min format. A meta-analysis found that the Blues Program was at least as effective as CBT of longer duration, and better in reducing depression symptoms among high-risk young people than several active comparator interventions.Reference Stice, Shaw, Bohon, Marti and Rohde20
Follow-ups
Assessments were completed at eight time points: baseline (T 0), after each of the five intervention sessions (weekly for 4 weeks; T 1–T 4) and then 1 month later at programme completion (T 5) then at 6 months (T 6) and 12 months (T 7). All randomised participants were invited to complete assessments at all time points, including those who discontinued (see below).
Outcomes
Primary outcomes
The primary outcomes were depression symptom severity, measured using the 7-item depression subscale of the 21-item Depression Anxiety Stress Scales (DASS-21),Reference Henry and Crawford21 and loneliness, measured using the 4-item UCLA Loneliness Scale (UCLA-4).Reference Hays and DiMatteo22
Secondary outcomes
Additional outcome and process variables were measured at only four time points (T 0, T 5, T 6 and T 7). Secondary outcomes were social anxiety, general practitioner visits, well-being, life satisfaction, self-esteem and subjective physical health. Process measures were multiple group membership, group compatibility, social identification as a person with a mental illness, group cohesion, therapy group identification and service identification. Full details of these measures are provided in the protocol;Reference Cruwys, Haslam, Walter, Rathbone and Williams16 analyses are not reported here owing to space constraints.
Assessment of safety and adverse events
Facilitators monitored participant well-being in session and via assessment data. The protocol allowed facilitators to provide brief ad hoc supportive counselling as needed without compromising participant eligibility. Facilitators reported all concerns about participants to their supervisor for case management. Any severe decline in mental health would render participants ineligible for the trial, leading to referral for more intensive mental health treatment, and be recorded as an adverse event. No adverse events were recorded.
Statistical analysis
Full justification of our approach to analysis is provided in the protocol.Reference Cruwys, Haslam, Walter, Rathbone and Williams16 Two mixed-model repeated-measures (MMRM) models were used to test hypotheses: one to predict loneliness (Fig. 2) and one to predict depression (Fig. 3). Each model had a nested structure which included fixed effects for time point (level 1), condition, and their interaction, random intercepts for participant (level 2) and random intercepts for therapy group (level 3).
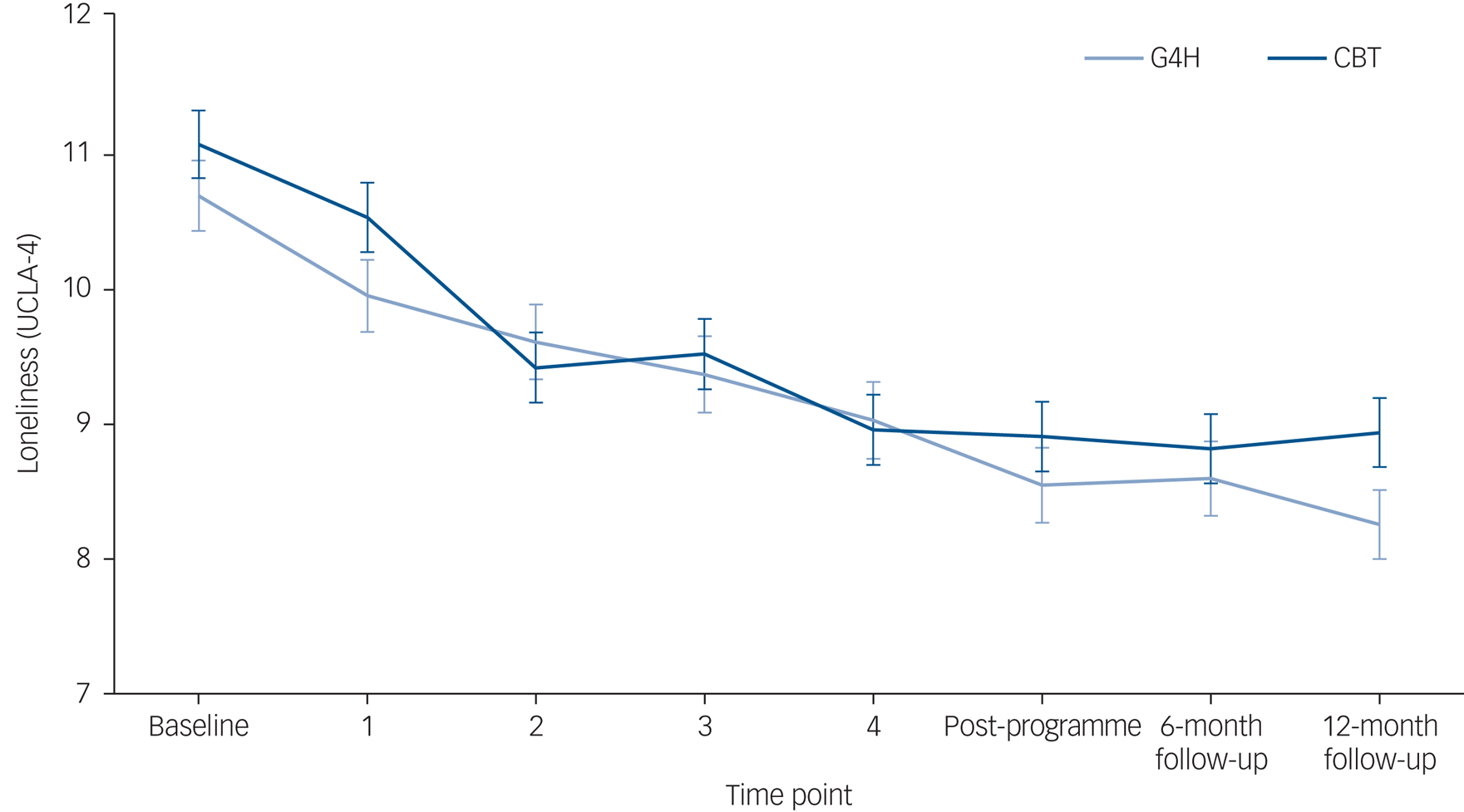
Fig. 2 Change in loneliness over time. UCLA-4, 4-item UCLA Loneliness Scale; G4H, Groups 4 Health; CBT, cognitive–behavioural therapy.
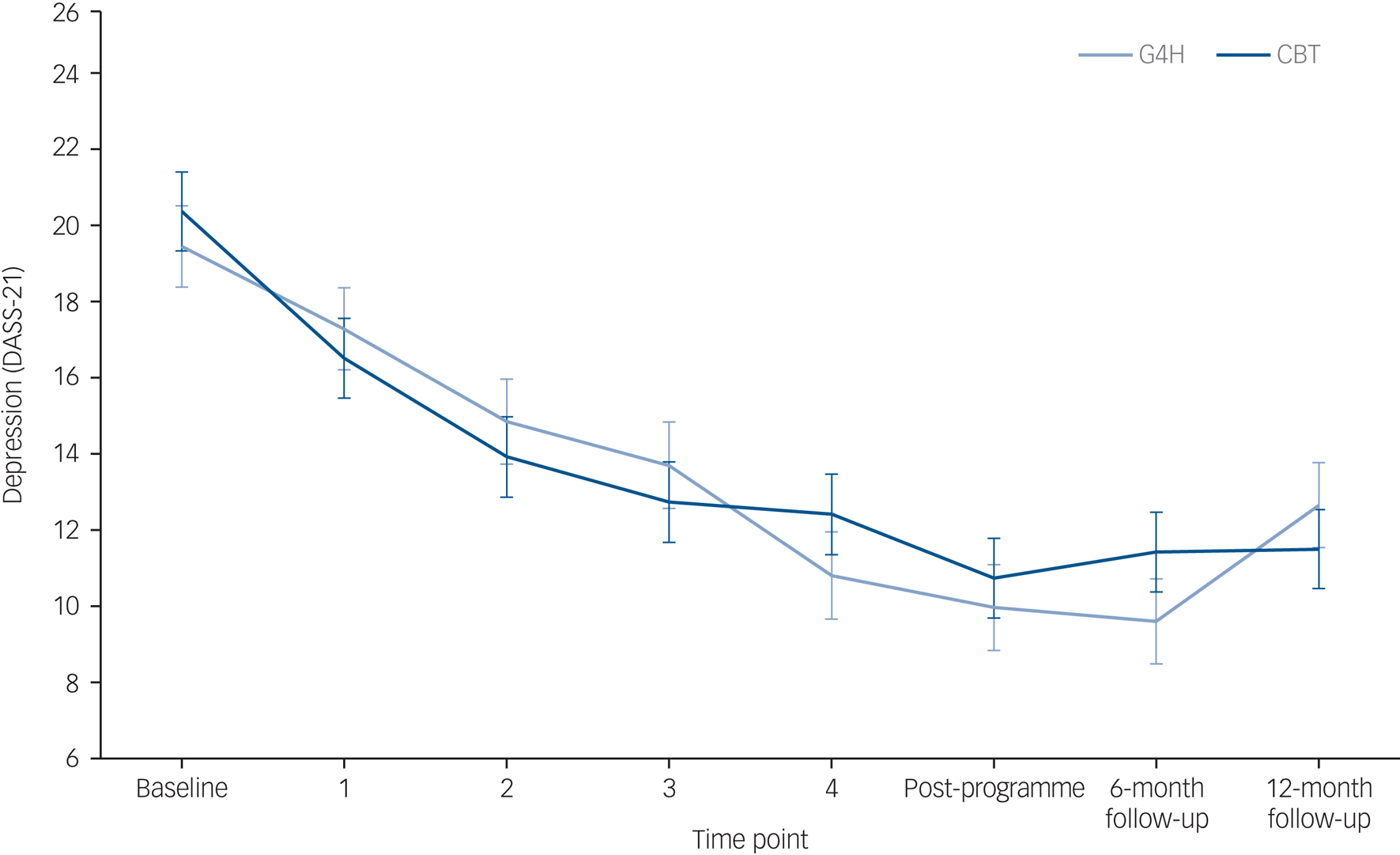
Fig. 3 Change in depression symptom severity over time. DASS-21, 7-item depression subscale of the 21-item Depression Anxiety Stress Scales; G4H, Groups 4 Health; CBT, cognitive–behavioural therapy.
Follow-up planned contrasts using estimated marginal means were calculated as appropriate, with correction for multiple comparisons using the multivariate t-distribution. Analyses were conducted in R (v.3.4.0) on macOS, supported by packages lme4 and emmeans.
Time point was treated as a categorical variable, with patterns of interaction assessed not only for linear but also for non-linear patterns (up to the 6th degree). This was because the time between follow-ups in the experimental design was non-linear and the duration of treatment was T 0–T 5 only. The analyses were therefore sensitive to non-linear symptom change (e.g. if a treatment led to large initial improvements and symptoms subsequently stabilised).
Missing data were managed using full information likelihood maximisation, which is readily implemented in MMRM to honour the intention-to-treat principle.Reference Molenberghs, Thijs and Jansen23 This approach utilises all available data for all participants. Overall, retention was high throughout the trial. Among the full (intention-to-treat) sample, the median and modal number of time points completed in both groups was eight (i.e., complete data). Similarly, the median and modal number of therapy sessions attended was five (i.e., full attendance) in both groups. In total, 173 participants had at least two time points of data, and 169 participants completed at least one of the three follow-up time points (T 5, T 6 and T 7). Time point T 5 had the lowest sample size, with 155 respondents. An a priori power analysis estimated that 67 people per condition would be needed to have 0.80 power to detect the hypothesised effect with an alpha level of 0.05. All time points met this criterion.
Per-protocol analyses were also conducted. These excluded participants who did not meet eligibility criteria throughout the trial period, were not randomly assigned, did not complete the intervention according to the protocol or who were missing data at either baseline (T 0) or follow-up (T 5, T 6 and T 7). This led to the exclusion of 22 participants who did not attend at least three of the five sessions (n = 17), who commenced adjunct treatment (n = 3) or did not complete any of the follow-up time points (n = 2). The likelihood of discontinuation did not differ between the G4H and CBT groups (χ2(1) = 2.38, P = 0.123).
Results
Hypothesis testing
Full details of analyses are provided in the supplementary Appendix available at https://doi.org/10.1192/bjp.2021.128.
Hypothesis 1(a) predicted significant improvement in loneliness in the G4H condition. Contrasts were specified to evaluate this within the G4H condition from baseline to programme completion (t(1086) = −7.96, P < 0.0001, d = −0.91), to 6-month follow-up (t(1085) = −7.85, P < 0.0001, d = −0.89) and to 12-month follow-up (t(1084) = −9.12, P < 0.0001, d = −1.07). Each of these analyses was significant, supporting hypothesis 1(a).
Hypothesis 1(b) predicted that improvements in loneliness would be greater in the G4H condition than in the CBT condition. To assess this, the interaction term between time and condition was examined. Although the linear interaction was not significant (t(1083) = 0.51, P = 0.613), the quadratic interaction was significant (t(1090) = 2.12, P = 0.034), thus supporting hypothesis 1(b). This indicated a non-linear trajectory of recovery that differed between the two groups. Underpinning this significant interaction, simple comparisons indicated that although loneliness decreased steeply between T 0 and T 2 in both the CBT and G4H conditions (t CBT(1077) = 6.61, P < 0.001; t G4H(1085)= 4.02, P = 0.002), loneliness then stabilised in the CBT condition between T 2 and T 7, but continued to improve in the G4H condition (t CBT(1078) = 1.94, P = 0.524; t G4H(1086) = 4.86, P < 0.001). The absolute difference between groups in loneliness at T 7 was −0.679 (95% CI −1.43 to 0.07), t(67.4) = −1.81, P = 0.075. There are no formal guidelines for clinically meaningful change on the UCLA-4. However, previous research has treated a change of 2 points on the UCLA-20 (3.3%) as clinically significant and this would correspond to a change of 0.4 points on the UCLA-4. By this benchmark, the difference of 0.68 between G4H and CBT groups (0.69 in the per-protocol analysis) at T 7 would be considered clinically meaningful.
Hypothesis 2 predicted that G4H would be non-inferior to CBT in improving depression symptom severity, conceptualized as a change score difference that was both non-significant and less than 2.20 at all follow-up time points. Supporting hypothesis 2, all seven planned contrasts between T 0 and each other time point were non-significant (Ps > 0.143), and at no time point did the difference exceed 2.2 (the largest was 2.12 for the T 0 versus T 7 comparison). The absolute difference between groups in depression at the 12-month follow-up was 1.176 (95% CI −1.94 to 4.29), t(61.7) = 1.18, P = 0.453.
Hypothesis 3 predicted that the benefits of G4H for loneliness and depression would be sustained over time. Supporting hypothesis 3, planned contrasts indicated no significant change in loneliness between programme completion and 6-month follow-up (t(1080) = −0.17, P > 0.999) or between 6- and 12-month follow-up (t(1079) = −1.24, P = 0.912). Similarly, for depression, there was no significant change in the G4H condition between programme completion and 6-month follow-up (t(1085) = 0.34, P > 0.999) and limited evidence of change between 6- and 12-month follow-up (t(1079) = −2.84, P = 0.087).
Per-protocol analyses
All hypothesis testing was repeated using only the subsample (n = 152) who completed the programme in accordance with the trial protocol. All of the findings were replicated and each hypothesis supported (see full details in the supplementary Appendix).
Discussion
This non-inferiority RCT compared Groups 4 Health (G4H) with dose-controlled group cognitive–behavioural therapy (CBT) across a 12-month follow-up. Loneliness improved significantly in both conditions, with G4H showing a slight advantage at 12-month follow-up. Depression improved comparably in both conditions. The reason for the different patterns in loneliness and depression outcomes in the two groups is not clear. However, on theoretical grounds, this could tentatively be attributed to the explicit focus on social group connection in G4H (but not in CBT) and on depression in CBT (but not in G4H).
Meta-analytic evidence shows that depression treatments are typically less effective for young people than for adults.Reference Cipriani, Zhou and Del Giovane4,Reference García-Escalera, Chorot, Valiente, Reales and Sandín6 However, few extant treatments target loneliness, which is a key risk factor in the onset, maintenance and development of depression.Reference Erzen and Çikrikci8 Interventions that do target loneliness have limited efficacy and focus almost exclusively on older people.Reference Masi, Chen, Hawkley and Cacioppo9 Promising interventions that address this lacuna focus on building group-based belonging in accordance with a social identity theoretical framework.Reference Haslam, Cruwys, Haslam, Dingle and Chang12 Indeed, recent meta-analysis showed that social identity-based interventions of this form had effect sizes for depression that rivalled those of established treatments.Reference Steffens, Larue and Haslam15
Extending this line of research, the present phase 3 trial is the first to evaluate a social identity intervention against another evidence-based treatment for loneliness and depression. This represented a conservative test of G4H, given that its efficacy has been attributed, at least in part, to the group-based nature of the intervention (which the CBT condition also had) and that it targets depression symptoms only indirectly (while the CBT condition targeted these symptoms directly). This trial found that both G4H (d = −0.71) and CBT (d = −0.91) were effective in reducing depression symptoms. At no time point were there significant differences between conditions for depression, and all numeric differences were smaller than the non-inferiority margin of 2.20. The effect sizes, particularly for CBT, were greater than the average reported in previous meta-analyses.Reference García-Escalera, Chorot, Valiente, Reales and Sandín6,Reference Weisz, McCarty and Valeri7 This may be partly attributable to the controlled setting of the trial, including the manualised nature of the treatments, monitoring of facilitator adherence and the group delivery format (as explained further below).
The trial yielded several other novel findings. First, previous treatment efforts for loneliness have had mixed success.Reference Masi, Chen, Hawkley and Cacioppo9 This is the strongest evidence to date for the benefit of G4H, with effect sizes much greater than the average of current interventions (d = −1.07 versus −0.19). The effect size of G4H for loneliness in the present trial was almost identical to that found in the phase 2 trial,Reference Henry and Crawford21 further increasing our confidence in its efficacy. Furthermore, few loneliness intervention studies provide evidence of sustained benefit over time. Here, we found evidence that benefits for loneliness were sustained a year later. This is consistent with both our predictions and with a key goal of G4H, which is to develop skills to build and maintain group-based belonging, including during life transitions and times of stress.Reference Haslam, Cruwys, Haslam, Dingle and Chang12 This is particularly pertinent in the context of the COVID-19 pandemic, which has raised the profile of loneliness, not only in terms of its prevalence and its effects on mental health, but also the limited evidence base on which we can intervene to address it.Reference Jetten, Reicher, Haslam and Cruwys24
Second, this trial provides the first evidence of the efficacy of depression-focused CBT in reducing loneliness (d = −0.89). Although these benefits for loneliness were not as large or sustained as those with G4H, they were larger than average effect sizes for other loneliness-focused interventions. Importantly, though, this trial utilised a group-based format of CBT. Therefore, these benefits may be attributable to the group environment as much as to the content of the intervention itself. Indeed, previous studies have indicated that loneliness interventions are most effective when delivered in a group format.Reference Cattan, White, Bond and Learmouth11 Furthermore, CBT is more effective for depression when people feel a sense of belonging with their therapy group.Reference Cruwys, Haslam and Dingle25 These results thus speak to the value of group-based delivery of psychotherapy, not only to the value of CBT.
Strengths and limitations
This trial had many strengths: (a) it had a well-powered design and high rate of retention, (b) it included an active dose-controlled comparison group, (c) it recruited from real-world health services across public and private sectors and (d) it assessed outcomes over a long follow-up period against reliable and valid measures. However, like all studies, it also had limitations. In particular, it was not possible to mask participants or facilitators to their assignment once the groups had commenced. To reduce demand characteristics related to this, the non-inferiority focus of the trial was emphasised at all times.
Future research
Having established the efficacy of G4H, future research needs also to evaluate its effectiveness, particularly when delivered by health professionals with minimal researcher oversight. It will also be important to establish its scalability in large implementation trials and adaptability for remote delivery. Acceptability and feasibility of the intervention in a wide variety of healthcare contexts is yet to be established. Although attrition from this trial did not differ significantly between groups, further investigation of the rate and reasons for treatment drop-out in G4H is warranted. The group-based delivery format of G4H, and its suitability for delivery by trainees, mean that the intervention is likely to be a cost-effective alternative to treatment as usual. However, this too will be important to establish quantitatively in a formal cost-effectiveness evaluation.
Clinical implications
This study has implications for clinical practice, patient care and policy. Its findings suggest that a clinical focus on loneliness is warranted in treatment of depressed young people. Importantly, this also aligns with the lived experience of young people, who often identify a social trigger for the onset of their first depressive episode and typically prefer an active, skills-based approach to treatment.Reference Jaycox, Asarnow, Sherbourne, Rea, LaBorde and Wells5 However, as the evidence presented here illustrates, loneliness-oriented interventions are likely to be most effective when they draw on the established science of social relationships embodied by the social identity framework. Indeed, this framework holds promise for the improvement of clinical interventions more broadly – an opportunity that is yet to be fully realised. Crucially, the two interventions compared here both achieved large effect sizes for depression and loneliness despite both being brief, group-based and manualised; this makes them more resource-efficient than treatment as usual. Depression typically has a remitting–recurring course and causes substantial impairment in functioning for young people. The efficacy of group-based G4H and CBT suggests that policymakers should prioritise efforts to make them accessible for young people.
Acknowledgements
We are grateful for the funding and support provided for this trial by Australian Rotary Health and the National Health and Medical Research Council. The trial would not have been possible without the generous support of our group facilitators, the staff at headspace and the University of Queensland clinic, and all the young people involved in the trial. Sarah V. Bentley, Genevieve A. Dingle and Jolanda Jetten co-authored Groups 4 Health and were essential to its development. Victoria Gore-Jones and Francis Dark assisted in the early stages of the trial development and implementation.
Supplementary material
Supplementary material is available online at http://dx.doi.org/10.1192/bjp.2021.128.
Data availability
The data that support the findings of this study are available from the Open Science Framework: https://osf.io/gbk83/.
Author contributions
T.C. led the grant, oversaw the trial, did the statistical analyses and wrote the first draft of the report. C.H. provided conceptual input at all stages of the grant and project, and led the design of the intervention and the training of facilitators. J.A.R. and E.W. were the trial managers. S.A.H. provided conceptual input and led grants that supported programme development. Z.C.W. provided expertise on protocol development and analyses. All authors provided critical feedback on the report.
Funding
This research was funded by Australian Rotary Health and the National Health and Medical Research Council (#1173270).
Declaration of interest
T.C., C.H. and S.A.H. are the developers of the Groups 4 Health programme, and the University of Queensland holds its associated intellectual property. These authors have an academic, rather than commercial, interest in the programme, with training offered at cost and additional funds directed to ongoing programme development and evaluation.








eLetters
No eLetters have been published for this article.