To the Editor—Hyperbaric oxygen therapy (HBOT) is a noninvasive treatment that involves breathing pure oxygen in a pressurized room or tube.Reference Gesell 1 HBOT can be used for chronic wound-healing problems, soft-tissue infections, gas gangrene,Reference Goldman 2 and as an emergency treatment for diving decompression sicknessReference Vann, Butler, Mitchell and Moon 3 or carbon monoxide poisoning.Reference Buckley, Juurlink, Isbister, Bennett and Lavonas 4 Multiplace hyperbaric therapeutic chambers can accommodate several patients at once, allowing contact among patients who may be infected or colonized.
Prevention of cross infection is mainly based on hand hygiene and on the use of alcohol-based hand rubs (ABHRs), which have proven effective in reducing nosocomial infections.Reference Pittet, Hugonnet and Harbarth 5 However, in hyperbaric conditions, fire is the main danger and the most feared riskReference Sheffield and Desautels 6 , Reference Simini 7 because people cannot quickly leave the chamber during a session. Flash fire associated with the use of alcohol-based antiseptic agent has already been described.Reference Bryant, Pearce and Stover 8 Thus, the use of ABHR during HBOT sessions is not recommended. The alternative to hand rubbing is simple hand washing with mild soap, but these soaps generally contain flammable substances (such as glycerin) that should also be avoided inside the chamber. 9
There are no specific recommendations for preventing infection in hyperbaric chambers. Moreover, safety measures reinforce the difficulty of implementing infection prevention recommendations in daily practice. To address these issues, we made an inventory of infection control practices in French HBOT chambers.
We sent a questionnaire to 18 hyperbaric medicine units in France. This survey concerned environmental and medical equipment cleaning (ie, frequency and products used for the cleaning of surfaces and disinfection of breathing circuit components) and infection control precautions. The last part of the survey concerned additional precautions in place according to the patient profile (eg, tracheotomy, carrying multidrug-resistant bacteria, or immunosuppressed) and the existence of specific procedures in the unit for patients requiring additional precautions (ie, contact or airborne precautions).
Between September 2014 and February 2015, we collected 16 completed questionnaires (89% response rate). Environmental disinfection management among HBOT units was quite variable (Table 1); there was heterogeneity in the maintenance frequencies of the different surfaces of the chamber although the products used for cleaning were generally the same. Overall, 87% of units declared they used a cleaner combined with a disinfectant. These cleaning products were not always appropriate to the hygiene recommendations (eg, disinfection products for medical devices were used for the maintenance of soil and surfaces) or to safety instructions related to the hyperbaric conditions (eg, products containing alcohol were used for the disinfection of surfaces).
TABLE 1 Environmental Cleaning Management of Hyperbaric Chambers and Treatment Modalities Depending on Patient Type
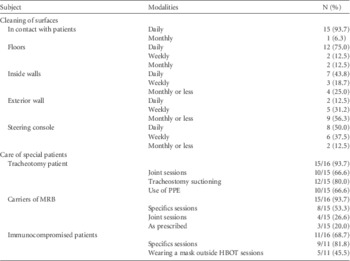
NOTE. PPE, personal protective equipment; MRB, multidrug-resistant bacteria; HBOT, hyperbaric oxygen therapy.
Most chambers (63%) were equipped with a sink. In these chambers, hand hygiene was achieved by simple hand washing using mild soap (30%), using ABHR (30%), using either of these two techniques (30%), or by washing hands with an antiseptic soap (10%). For those without sinks, hand hygiene was performed using ABHR or by simple washing outside the box, and in some cases professionals wore gloves. Practitioners wore professional attire, and in 56% of cases, specific recommendations were given to patients regarding their dress. In 75% of the HBOT units responding, cotton outfits were recommended, and synthetic fabrics and makeup (fats) were disapproved. Disinfection of oxygen masks was performed by soaking the mask in a disinfection solution in 94% of units, but the frequencies of disinfection varied among facilities: every day (50%), every week (19%), or at the end of the treatment cycle (12.5%). Most chambers were used to care for tracheotomy patients, carriers of multidrug-resistant bacteria, or immunocompromised patients. Patients were cared for during specific sessions or in joint sessions with other patients. Two units reported refusing patients who had tuberculosis, chickenpox, or methicillin-resistant Staphylococcus aureus respiratory infection. No unit reported an outbreak linked to an HBOT session.
This study highlights the fact that environmental cleaning management, disinfection of medical equipment, and application of hygiene precautions are highly variable among HBOT chambers. Some professionals believe that the use of ABHR in hyperbaric chambers is not dangerous, whereas others strictly forbid their use. Maintaining a clean and safe healthcare environment is an essential component of infection prevention and control. Likewise, it is very important to know the infection status (colonized or infected) of patients to prevent cross transmission.
Patients under airborne precautions should not undergo HBOT treatment because the risk of transmission of infection by this route is too difficult to control. The same safeguard applies to patients under droplet precautions. Specific sessions should be organized for patients under contact precautions. If postponement of the treatment is not possible, care inside the chamber should be limited, and the chamber should be cleaned immediately after the session. However, these precautions should not delay the treatment of patients in life-threatening emergencies.
The diversity of practices reported illustrates the difficult position of hyperbaric practitioners who must balance prevention of infection with safety practices. These difficulties extend to the safety of medical devices used in hyperbaric chambers, such as defibrillation units, which have been associated with a risk of sparks and fire, for example.Reference Kot 10
Following this study, the French Society of Hyperbaric Medicine and the French Society for Hospital Hygiene decided to develop specific guidelines for infection control in therapeutic hyperbaric chambers.
Acknowledgments
The authors are grateful to the French therapeutic hyperbaric chamber practitioners for their contribution to the study.
Financial support: No financial support was provided relevant to this article.
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.



