Drunkenness and alcohol misuse by the male partner are associated with poor mental health and spousal violence among married women in India. Reference Kumar, Jeyaseelan, Suresh and Ahuja1–Reference Varma, Chandra, Thomas and Carey3 Research outside India documents that men's alcohol problems increase the risk of depression in their female partners; Reference Homish, Leonard and Kearns-Bodkin4–Reference Tempier, Boyer, Lambert, Mosier and Duncan6 exceeding the risks associated with women's own alcohol use disorders or spousal violence. Reference Dawson, Grant, Chou and Stinson5 Gender inequities play a key role in women's health, Reference Moss7,Reference Murphy8 including in the impact of spousal violence Reference Varma, Chandra, Thomas and Carey3 but have not been included in studies on partner alcohol use and women's mental health. Similarly, most studies do not include women's own alcohol use and may overestimate associations between partner alcohol use and depression in women. Reference Dawson, Grant, Chou and Stinson5 Thus, an overall limitation of existing research is the lack of simultaneous examination of different psychosocial risk factors and, thereby, a limited understanding of the interrelationships between such factors in women's poor mental health.
Alcohol misuse represents a public health crisis in India that has yet to receive adequate attention. Reference Neufeld, Peters, Rani, Bonu and Brooner9,Reference Benegal10 About 30% of male drinkers in Goa, India's smallest state, 11 use alcohol hazardously. Reference Silva, Gaunekar, Patel, Kukalekar and Fernandes12,Reference D'Costa, Nazareth, Naik, Vaidya, Levy and Patel13 Common mental disorders, a term used to describe non-psychotic affective disorders (depressive and anxiety disorders), Reference Goldberg and Huxley14,Reference Patel, Kirkwood, Pednekar, Weiss and Mabey15 are documented in 6.6% of women aged 18–45. Reference Patel, Kirkwood, Pednekar, Pereira, Barros and Fernandes16 Economic deprivation, poor marital relationships and gender disadvantage increase and employment decreases risk for postnatal depression in Goan women. Reference Patel, Kirkwood, Pednekar, Weiss and Mabey15,Reference Patel, Rodrigues and DeSouza17 However, the role of partner alcohol use in women's depression has not been systematically assessed. The present study examined associations between various psychosocial risk factors, including demographics, partner alcohol use, partner violence and gender violence-related attitudes and common mental disorders in a community sample of women in Goa (Fig. 1). We hypothesised that a lack of resources (e.g. poor education and unemployment) and gender violence-related attitudes confound the association between partner alcohol use and common mental disorders in women; and that partner violence and partner alcohol-related problems each mediate the association between partner alcohol use and women's poor mental health. As a result of the low prevalence of women's drinking (<5%) in India, Reference Benegal, Nayak, Murthy, Chandra, Gururaj, Obot and Room18 although we assessed women's own alcohol use, we did not include women's drinking in our model.
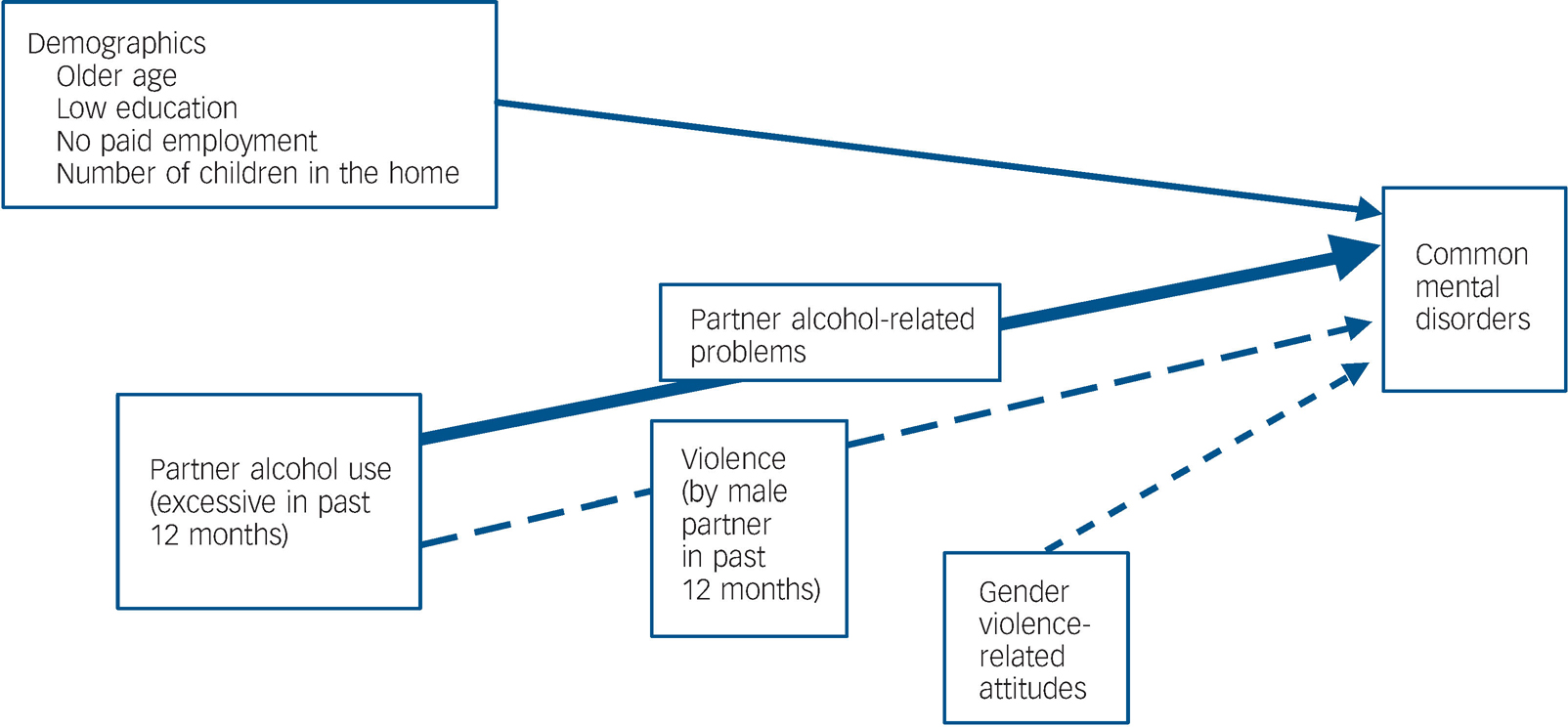
Fig. 1 Hypothesised associations among partner alcohol use, violence and common mental health disorders in women.
Method
Participants
We report data from a population study on alcohol use patterns and sexual risk behaviours conducted in rural and urban areas in Northern Goa, selected purposively to represent the local Goan situation. Given the study's focus on sexual risk, participation was limited to women aged 18–49 years. Respondents were selected in three stages (Fig. 2):
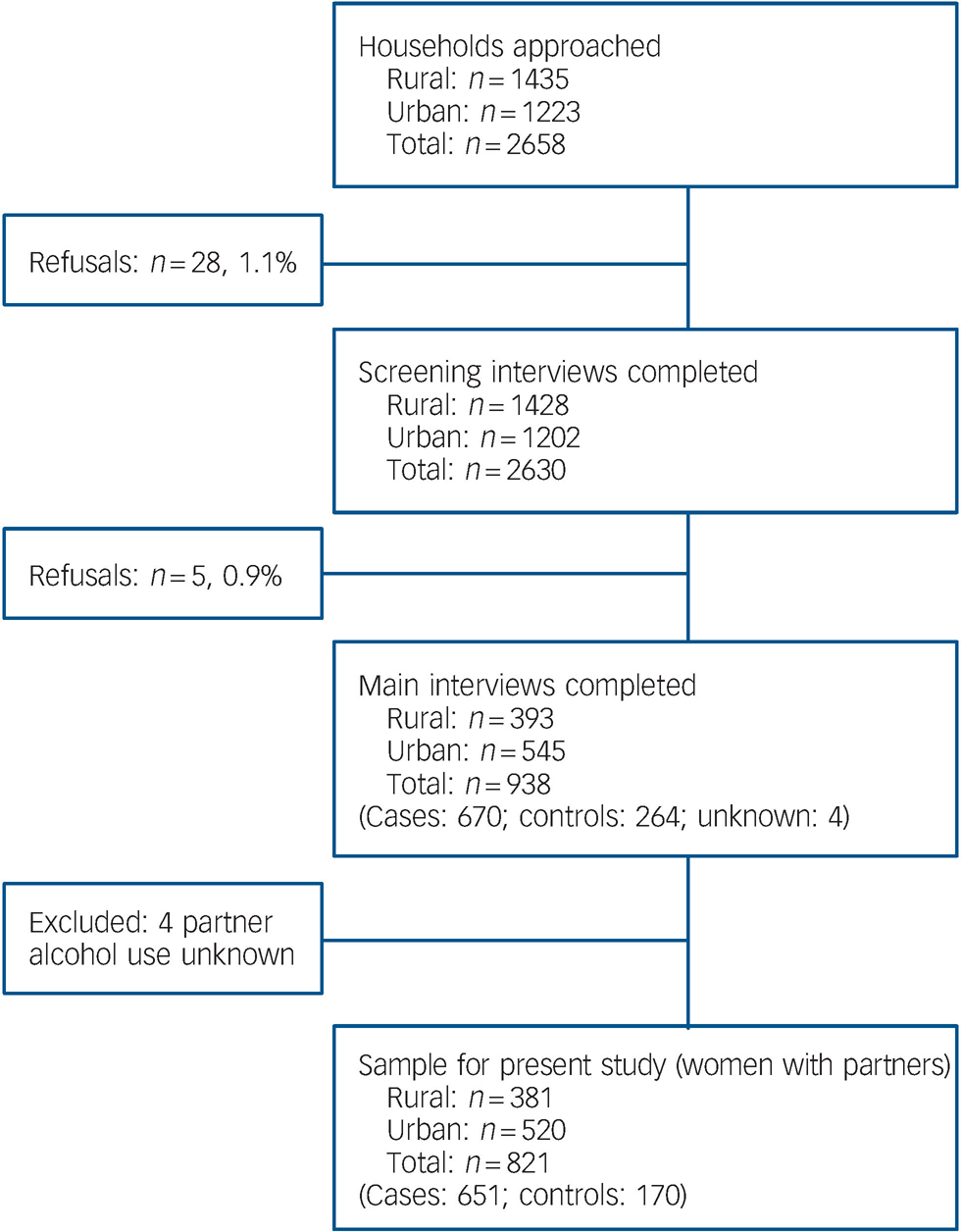
Fig. 2 Study sampling procedure. Cases, woman and/or her partner drank alcohol in the past year; controls, neither woman nor her partner drank in the past year; Unknown, woman reported on her own alcohol use but responded ‘don't know’ or ‘refuse’ to questions on her partner's alcohol use.
-
(a) a two-staged probability sampling procedure, based on 2004 and 2007 electoral rolls, was used to select households for participation. When no respondents were available or interviews could not be completed for other reasons at the randomly selected household, replacement households, specifically the first house on the right hand side of the house deemed unavailable, were approached;
-
(b) within each of the household, a randomly selected woman completed a screening interview;
-
(c) a subsample of women also completed a second more detailed (main) interview. Overall, refusal rates for both interviews were very low (<2% and <1%).
The main interview oversampled women who reported on the screening interviews that either they or their partner drank at least one whole alcoholic drink in the past year (71.2% of those interviewed, n = 670). There were three reasons for this oversampling: the study focus on alcohol-related health risks; relatively low expected drinking rates among women in Goa; and sexual risks for women being hypothesised as resulting from their partner's alcohol use. Only 2.2% (n = 59) of the 2630 women screened reported drinking alcohol in the past year; 24.6% (n = 648 or 34.9% of those with partners) reported that their partner drank. The remaining sample for the main interviews comprised non-drinking women, either without partners or with partners who were also reported to be non-drinkers in the past year (controls: 28.2%, n = 264).
The majority of 938 women completing main interviews were from randomly selected households (89.6%, n = 837). There were no sociodemographic differences between these women and those from replaced households, except for education. Fewer women from replaced compared with randomly selected households reported less than high-school education (29.5% v. 43.6%, P<0.01). Women from replaced and randomly selected households did not differ in the main outcome variable in the present study, i.e. common mental disorders or studied risk factors, such as partner violence, partner alcohol use and violence-related attitudes. Of women completing main interviews, 825 had partners in the past year. Analyses reported in this paper are limited to the 821 women who provided adequate information on both their own and their partner's alcohol use. Four women who could not provide information on their partner's alcohol use were excluded from the analyses.
Measures
Partner alcohol use
Partner alcohol use was the primary risk factor of interest in the present study and was assessed in screening interviews only for those women with partners in the past 12 months, i.e. either married or living with someone as a couple or never married but engaged or with a romantic partner. Almost all respondents reported one sexual partner in the past 12 months (99.5%, n = 820, 4 were not sexually active in the past 5 years) and only male partners.
Thus, ‘partner alcohol use’ refers exclusively to alcohol use by the male. Women who reported that their partner had at least one full drink in the past year (current alcohol use) were asked to estimate their partner's usual consumption on drinking days, consumption of the equivalent of 60 g of ethanol on any occasion and how often he returned home drunk in the past year. Partner excessive alcohol use was coded as positive when women reported any of the following for their partner: returned home drunk at least once, heavy usual quantity or any heavy drinking in past year. Heavy drinking was defined as the equivalent of 60 g or more of pure ethanol, carefully assessed by beverage-specific drink-size information. Reference Nayak, Kerr, Greenfield and Pillai19
Partner alcohol-related problems were assessed in the main interview for women with drinking partners. Items were modified from those in the US National Alcohol Surveys. Reference Midanik and Greenfield20,Reference Greenfield, Nayak, Bond, Ye and Midanik21 As in recent US studies on partner alcohol use, Reference Dawson, Grant, Chou and Stinson5 these items assessed seven alcohol-related problem areas including threats to health, legal problems, fights, accidents, tension or conflict in the home, financial problems and the woman or her children being physically hurt after or while her male partner was drinking. Respondents reporting one or more problems relating to the partner's alcohol use were coded positive for partner alcohol use problems.
The General Health Questionnaire (GHQ)
The GHQ originally developed in the UK Reference Goldberg and Williams22 and widely used internationally to screen for common mental disorders was used to assess the primary outcome measure of common mental disorders in the main interview. This 12-item measure, previously used in Goa, assesses cognitive and psychological well-being. The GHQ has been demonstrated to be superior to the primary care psychiatric questionnaire for detection of common mental disorders, Reference Patel, Pereira and Mann23 with a score of six or more being associated with an overall correct classification rate of 87% Reference Patel, Araya, Chowdhary, King, Kirkwood and Nayak24 in primary care samples. A score of five or more has been used for common mental disorders with community samples in Goa. Reference Pillai, Andrews and Patel25
Hypothesised confounding and mediating factors assessed included the following.
Demographics
In the screening interview, we assessed age, ethnicity (Goan nativity), religion, marital status and socioeconomic status measures including education, employment, experiencing hunger in the past 3 months because of lack of money or money problems, and household assets including drinking water, toilet facilities, use of non-biomass cooking fuels and ownership of durables (e.g. fan, bicycle, refrigerator or automobile). As in prior Indian surveys, Reference Gwatkin, Rutstein, Johnson, Suliman, Wagstaff and Amouzou26 household asset information was used to compute a standard of living index (SLI) based on principal component analysis. Specifically, the SLI was computed by summing items weighted by their factor loadings. Resultant scores were categorised into quintiles as in other Indian studies on alcohol consumption. Reference Subramanian, Nandy, Kelly, Gordon and Smith27
Women's alcohol and tobacco use
Women's own alcohol and tobacco use were assessed in screening interviews. Respondents were asked if they had ever tasted alcohol or had a drink containing alcohol. Those affirming this were asked if they had a whole drink of any alcoholic beverage in the past 12 months. The Alcohol Use Disorders Identification Test (AUDIT), a 10-item questionnaire developed for international use by the World Health Organization Reference Babor, Higgins-Biddle, Saunders and Monteiro28 and used previously in Goa Reference D'Costa, Nazareth, Naik, Vaidya, Levy and Patel13,Reference Gaunekar, Patel and Rane29 was used to assess hazardous alcohol use. Individual AUDIT items are coded 0 to 4. Given recommendations to use lower scores for women, Reference Bradley, Boyd-Wickizer, Powell and Burman30 a score of six or more indicated hazardous alcohol use. Using items from the Indian National Family Health surveys, 31 respondents were asked if they had used tobacco in any form, including smoking or chewing tobacco, how often and in what amount they used tobacco in the past 12 months.
Partner violence
Experience of victimisation by partner violence was assessed in the screening interview for women with partners. Two questions assessed past 12-month occurrence of partner physical violence (‘Has your partner slapped, hit, kicked, punched you or done something else that did or could have hurt you physically?’) and sexual violence (‘Has your husband/wife/partner had sex with you when you were unwilling or forced you to do sexual things or to have sex?’). These questions, based on the Conflict Tactic Scale, Reference Straus, Hamby, Boney-McCoy and Sugarman32 were adapted from items previously used in studies on partner violence in India. Reference Patel, Kirkwood, Pednekar, Pereira, Barros and Fernandes16,Reference Duvvury, Nayak, Allendorf, Young and staff33 Women reporting either type of violence were coded as positive for partner violence.
Gender violence-related attitudes
Gender violence-related attitudes were assessed in the main interview with a 6-item measure of attitudes regarding partner violence derived from a multisite study on masculinity and violence in India Reference Duvvury, Nayak, Allendorf, Young and staff33 and adapted for use in Goa. These items assessed whether respondents agreed or disagreed with specific conflict areas as reasons that make it acceptable for a man to use force with his female spouse or partner, such as the partner being ‘sexually unfaithful’ and ‘being disrespectful’. Principal components analyses indicated a single factor (58.2% variance; λ1 = 3.49), with high-item factor loadings (0.59–0.88) and good internal consistency (α = 0.85, 0.83) for women's responses. A total score was computed by counting all ‘agree’ responses for those women who answered at least four of the six items. Analyses used a dichotomous variable (agreement with one or more items v. none) based on this total score to indicate attitudes condoning spousal violence by men.
Procedure
Following informed consent procedures, screening and main interviews were administered by women interviewers, in private, in the respondents' homes. Screening interviews took about 15 min to complete (mean = 14.64, s.d. = 4.93); main interviews about 45 min (mean = 48.64, s.d. = 17.88). For almost all respondents (98.8%, n = 927), both interviews were completed on the same day. Study procedures, including the protocol and measures, were approved by research ethics committees at Sangath in Goa, the Public Health Institute in the USA, and the Indian Council of Medical Research.
Analysis
After examining distributions of demographics, self-reported alcohol and tobacco use, victimisation by partner violence and partner alcohol use, bivariate analyses were conducted to identify differences by the presence v. absence of common mental disorders. Significant variables (P<0.01, using a correction for multiple tests) were then entered into logistic regressions with common mental disorders as the outcome. Logistic regression models were first estimated using demographics, violence attitudes and partner violence as covariates. Regression models were specified with appropriate interaction terms to evaluate possible moderating effects of risk factors on expected associations between partner alcohol use and women's mental health.
Mediation effects in the partner excessive alcohol use and common mental disorders were tested, separately for partner violence for all women with partners; and for partner alcohol-related problems for the subset of women with drinking partners. These analyses focused on assessing four criteria for demonstrating mediation effects: Reference MacKinnon34
-
(a) the independent variable (partner excessive alcohol use) must be related to the mediator (partner violence, alcohol problems);
-
(b) the mediator must be related to the dependent variable (common mental disorders);
-
(c) the independent and dependent variable must be related;
-
(d) the association between the independent and dependent variable must be reduced to non-significance when the mediating variable is included in the regression equation.
Gender-specific weights that adjusted for design-related biases were applied to the data. These weights sequentially adjusted for sampling procedures, village or area population size and age distribution information from the electoral rolls, number of gender-specific adults aged 18–49 in the household, non-response and undersampling of women non-drinkers with non-drinking partners. Weights were capped when outside ‘rule of thumb limits’ to reduce unstable estimates as a result of divergent weights and rescaled to separately represent urban and rural sample sizes.
Results
A total of 79 women scored five or more on the GHQ, suggesting a 8.2% prevalence rate of common mental disorders among 18- to 49-year-old women with partners in North Goa. Some women were unable to provide specific information and answered ‘don't know’ to items on their partner's alcohol use. Thus, the number of women providing data on each partner alcohol use pattern item varied (512 to 625); 804 women provided enough information for partner excessive alcohol use to be coded. Based on women's reports, the prevalence of any partner alcohol use (n = 821) and excessive alcohol use (n = 804) were estimated as 35.7% and 9.7% respectively. Less than 10% of the 188 women whose partner's drinking met excessive alcohol use criteria reported less than monthly occurrence of a single pattern of excessive use alone (i.e. returning home drunk: 9.6%, n = 18; heavy drinking: 3.2%, n = 6). Most of these women (n = 15) could not provide information on the other two drinking patterns used to estimate excessive alcohol use.
Increasing age, not having completed high school and lack of paid employment increased risk for common mental disorders (online Table DS1). The number of children in the home was protective. Urbanicity, ethnicity, number of own children, standard of living and religion were not associated with women's common mental disorders. Less than 5% (n = 38) had consumed any alcohol in the past 12 months and less than 1% (n = 3) reported any hazardous alcohol use. No differences were found by common mental disorders for women's own alcohol use or tobacco (including daily) use (not shown in Table DS1). Table 1 reports partner alcohol use, partner violence and violence-related attitudes by mental disorder. Any partner alcohol use did not increase risk for mental disorders, but partner excessive alcohol use and partner violence increased the risk for such disorders approximately three- (odds ratio (OR) = 2.8, 95% CI 1.3–5.7) and fourfold (OR = 4.41, 95% CI 1.9–9.9) respectively. With the exposure rate of 9.7% and the associated odds ratio for mental disorders of 3.1, a population attributable fraction of 17.5% (95% CI 3.4–31.6%) was estimated for partner excessive alcohol use. Reference Kahn and Sempos35
Table 1 Past 12-month partner alcohol use, partner violence and violence-related attitudes and associations with common mental health disorders among women with partners (n = 821)a

| Total sample % (n) | Common mental health disorders % (n) (n = 79) | Odds ratio (95% CI) | P | |
|---|---|---|---|---|
| Partner alcohol use b | ||||
| Any use by partner in past 12 months | 0.62 | |||
| No | 64.3 (179) | 61.1 (13) | ||
| Yes | 35.7 (642) | 38.9 (66) | ||
| Any excessive alcohol use by partner (n = 804) | 2.76 (1.34-5.68) | 0.004 | ||
| No (includes non-drinking partners) | 90.3 (616) | 79.2 (38) | ||
| Yes | 9.7 (188) | 20.8 (37) | ||
| Any alcohol-related problem (n = 614, drinking partners only) | 4.62 (1.79-11.93) | 0.001 | ||
| No | 72.2 (425) | 40.0 (22) | ||
| Yes | 27.2 (189) | 60.0 (40) | ||
| Alcohol-related problems, excluding tension in the home (n = 614) | 6.75 (2.58-17.65) | < 0.001 | ||
| No | 78.1 (462) | 40.0 (23) | ||
| Yes | 21.9 (152) | 60.0 (39) | ||
| Relationship c | ||||
| Any violence by male partner (n = 791) | ||||
| No | 95.8 (714) | 84.3 (54) | 5.51 (2.28-13.32) | < 0.001 |
| Yes | 4.2 (77) | 15.7 (20) | ||
| Gender violence-related (condoning) attitudes (n = 810) | 2.77 (1.48-5.15) | 0.001 | ||
| No | 52.3 (422) | 30.0 (26) | ||
| Yes | 47.7 (388) | 70.0 (52) |
Prior to multivariate analyses, a principal components factor analysis of all variables significantly associated with common mental disorders was conducted. A condition number of 0.19 (minimum to maximum eigenvalue ratio: 0.43/2.84) suggested a lack of substantial collinearity among covariates. Partner excessive alcohol use remained a significant predictor for women's mental disorders (Table 2) when demographics (model 1) as well as violence-related attitudes (model 2) were entered simultaneously in separate models, with associated odds ratios of roughly four. When partner violence was entered with demographics (model 3), partner excessive alcohol use became less influential (P = 0.07). Unlike age and education, lack of paid employment and number of children in the home remained significant in all multivariate models. Violence-related attitudes remained significant in all multivariate models, increasing odds of mental illness by approximately three (OR = 2.92, 95% CI 1.38–6.19). No interaction effects were found for sociodemographic factors and partner excessive alcohol use.
Table 2 Associations between partner excessive alcohol use and women's common mental health disorders in multivariate analyses controlling for significant covariates (n = 767)a

| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Age | 1.43 | 0.93-2.18 | 0.10 | 1.37 | 0.88-2.12 | 0.16 | 1.32 | 0.82-2.12 | 0.25 | 1.32 | 0.82-2.12 | 0.25 |
| Did not complete high school | 1.95 | 1.05-3.62 | 0.04 | 1.95 | 0.64-2.50 | 0.50 | 1.34 | 0.65-2.77 | 0.42 | 1.34 | 0.65-2.77 | 0.42 |
| No paid employment | 3.14 | 1.35-7.33 | 0.008 | 2.64 | 1.11-6.28 | 0.03 | 5.63 | 1.78-17.80 | 0.003 | 5.63 | 1.78-17.80 | 0.003 |
| Children in the home | 0.40 | 0.24-0.66 | < 0.001 | 0.34 | 0.20-0.58 | < 0.001 | 0.34 | 0.19-0.60 | < 0.001 | 0.34 | 0.19-0.60 | < 0.001 |
| Partner excessive alcohol use | 3.79 | 1.73-8.30 | 0.001 | 4.41 | 1.96-9.89 | < 0.001 | 2.29 | 0.85-6.21 | 0.10 | 2.64 | 0.93-7.33 | 0.07 |
| Condoning violence | 2.64 | 1.32-5.29 | 0.01 | 2.92 | 1.38-6.19 | 0.005 | ||||||
| Any partner violence | 5.82 | 1.78-18.99 | 0.004 | 7.15 | 2.03-25.11 | 0.002 | ||||||
Partner violence as mediating the association of partner excessive alcohol use with mental disorders
The first criteria for mediation by partner violence (Table 3) was met, as partner excessive alcohol use was a significant predictor of partner violence (OR = 28.71, 95% CI 11.49–71.70) even when demographic factors were used as controls. Partner violence was significantly associated with common mental disorders (OR = 9.12, 95% CI 3.24–25.7) and partner alcohol use with common mental health disorders (OR = 4.09, 95% CI 1.78–9.39), thus satisfying the second and third criteria for mediation.
Table 3 Tests of mediation effect of partner violence in the association between partner excessive alcohol use and women's common mental health disorders among women with partners (n = 776)

| Criteria 1 (excessive use predicting violence) | Criteria 2 (violence predicting common mental health disorders) | Criteria 3 (excessive use predicting common mental health disorders) | Criteria 4 (including violence in predicting common mental health disorders from excessive use) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Age | 1.20 | 0.64-2.26 | 0.57 | 1.35 | 0.86-2.12 | 0.19 | 1.38 | 0.88-2.16 | 0.16 | 1.36 | 0.86-2.14 | 0.18 |
| Did not complete high school | 1.55 | 0.64-3.77 | 0.33 | 2.19 | 1.14-4.22 | 0.02 | 2.23 | 1.17-4.27 | 0.02 | 2.14 | 1.11-4.14 | 0.02 |
| No paid employment | 0.67 | 0.28-1.68 | 0.41 | 5.35 | 1.85-15.46 | 0.002 | 5.05 | 1.81-14.10 | 0.002 | 6.13 | 2.06-18.27 | 0.001 |
| Children in the home | 1.17 | 0.60-2.28 | 0.65 | 0.40 | 0.24-0.68 | 0.001 | 0.42 | 0.25-0.70 | 0.001 | 0.39 | 0.23-0.67 | 0.001 |
| Partner excessive alcohol use | 28.71 | 11.49-71.70 | < 0.001 | 4.09 | 1.78-9.39 | 0.001 | 2.29 | 0.85-6.21 | 0.100 | |||
| Partner violence | 9.12 | 3.24-25.70 | < 0.001 | 5.82 | 1.78-8.99 | 0.004 | ||||||
Introducing partner violence into the logistic regression equation resulted in a reduction of more than a third (41.1%, 95% CI 33.3–49.9%) from 1.41 (s.e. = 0.43) to 0.83 (s.e. = 0.51) in the beta for partner excessive alcohol use to non-significance (P = 0.10). Thus there was at least a partial mediation effect for partner violence in associations between partner excessive alcohol use and women's common mental health disorders. This mediation effect remained even when women's violence-related attitudes (not hypothesised to be associated with partner excessive alcohol use) were included in models with a reduction of 38.5% (95% CI 31.7–46.7%) from 1.56 (s.e. = 0.44) to 0.96 (s.e. = 0.53) in the beta for partner excessive alcohol use to non-significance (P = 0.07). No interaction effects were found for partner violence and partner excessive alcohol use.
Partner alcohol-related problems
The most frequent past year partner drinking-related problems reported by women with drinking partners were increased tension at home (23.0%), financial problems (15.7%) and threat to his health (12.4%). Fewer than 10% reported partner drinking-related fights (7.3%) or that they or their children were physically hurt by a drinking partner (8.8%). Partner alcohol use-related accidents (0.6%) and legal problems (0.4%) were infrequently reported. Overall, 27% of women with partners (n = 189) reported at least one partner alcohol use-related problem. Excluding increased tension in the home as an alcohol-related problem due to possible reverse causality (tension owing to the woman's depression or emotional distress) did not alter the percentages of women reporting partner alcohol-related problems who were positive for common mental health disorders (Table 1).
Partner alcohol-related problems as mediating the association of partner excessive alcohol use with common mental health disorders
Mediation effects for partner alcohol-related problems in the partner excessive alcohol use and women's common mental health disorders association were tested with the 597 respondents with drinking partners who provided complete data on problems (Table 4). The first criteria for mediation was met as partner excessive alcohol use was a significant predictor of partner alcohol-related problems (OR = 13.45, 95% CI 6.39–28.33). Partner alcohol use problems were significantly associated with mental disorders (OR = 4.65, 95% CI 1.61–12.97) and partner alcohol use with common mental health disorders (OR = 3.87, 95% CI 1.41–10.62), thus satisfying the second and third criteria.
Table 4 Tests of mediation effect of partner alcohol-related problems in the association between partner excessive alcohol use and common mental health disorders among women with drinking partners (n = 597)

| Criteria 1 (excessive use predicting alcohol problems) (n = 597) | Criteria 2 (alcohol problems predicting common mental health disorders) (n = 597) | Criteria 3 (excessive use predicting common mental health disorders) (n = 804) | Criteria 4 (including alcohol problems in predicting common mental health disorders from excessive use) (n = 597) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Age | 0.94 | 0.56-1.57 | 0.80 | 1.10 | 0.55-2.21 | 0.79 | 1.09 | 0.54-2.19 | 0.81 | 1.09 | 0.54-2.19 | 0.81 |
| Did not complete high school | 3.24 | 1.54-6.80 | 0.002 | 1.55 | 0.55-4.39 | 0.41 | 1.84 | 0.67-5.06 | 0.24 | 1.52 | 0.53-4.30 | 0.43 |
| No paid employment | 0.66 | 0.31-1.40 | 0.28 | 1.95 | 0.66-5.79 | 0.23 | 1.95 | 0.65-5.81 | 0.23 | 2.11 | 0.70-6.39 | 0.18 |
| Children in the home | 0.97 | 0.54-1.75 | 0.93 | 1.22 | 0.56-2.66 | 0.62 | 1.23 | 0.56-2.68 | 0.60 | 1.26 | 0.38-2.79 | 0.57 |
| Partner excessive alcohol use | 13.45 | 6.39-28.33 | < 0.001 | 3.87 | 1.41-10.62 | 0.009 | 2.23 | 0.69-7.24 | 0.18 | |||
| Partner alcohol-related problems | 4.57 | 1.61-12.97 | 0.004 | 3.01 | 0.90-10.09 | 0.07 | ||||||
Introducing partner alcohol-related problems into the model resulted in 40.7% reduction (95% CI 31.1–51.5%), from 1.35 (s.e. = 0.52) to 0.80 (s.e. = 0.60), in the coefficient for partner excessive alcohol use to non-significance (P = 0.18). This mediation effect was significant even when tension in the home related to the partner's alcohol use was excluded from partner alcohol-related problems (not shown in tables) with a 65.9% (95% CI 54.8–76.5%) reduction to 0.46 (s.e. = 0.65), in the coefficient for partner excessive alcohol use to non-significance (P = 0.48). Thus, at least partial mediation effects were found for partner alcohol-related problems in the partner excessive alcohol use and women's common mental health disorders association. Interactions between partner excessive alcohol use and partner alcohol-related problems were not significant.
Discussion
Prevalence of common mental disorders in women
There was a prevalence of 8.2% for common mental health disorders among adult women aged 18–49 in our study population in Goa, India. Our findings are consistent with those previously reported from another study in North Goa that reported a prevalence of 6.6% in women assessed by diagnostic interviews. Reference Patel, Kirkwood, Pednekar, Pereira, Barros and Fernandes16 Together, these data suggested a higher prevalence for common mental health disorders compared with that for other negative health outcomes among Goan women, such as sexually transmitted infections which is estimated at roughly 4%, Reference Patel, Weiss, Mabey, West, D'Souza and Patil36 and this underscores the importance of a better understanding of risk factors for mental illness among women in Goa.
Risk factors for women's common mental disorders
Excessive partner alcohol use increased the risk for mental health disorders above and beyond significant sociodemographic risk factors, including older age, poor education, fewer children in the home and lack of paid employment, with an associated population-attributable fraction of 17.5%. Partner violence and partner alcohol-related problems mediated the association of partner excessive alcohol use with women's common mental health disorders. Attitudes condoning male spousal violence were independently associated with mental health problems in women.
Kendler and colleagues Reference Kendler, Kessler, Neale, Heath and Eaves37 have noted the multifactorial nature of depression, highlighting the role of stressful life events and negative interpersonal relations. Previous North American studies demonstrated an association between men's alcohol-related problems and depression reported by wives. Specifically, risks associated with male partners’ alcohol use problems for women's depression have been shown to present an additive burden to women's mental health, exceeding those associated with women's own alcohol use disorders or domestic violence. Reference Homish, Leonard and Kearns-Bodkin4,Reference Dawson, Grant, Chou and Stinson5 Indeed, alcohol-related marital problems predict subsequent depression in women. Reference Tempier, Boyer, Lambert, Mosier and Duncan6 These, studies, however, did not control for partner violence or examine its mediating role in men's alcohol use problems and women's anxiety and depression. An important contribution of our study is the ‘unpacking’ of the link between partner alcohol use and mental illness in women. Partner violence and problems related to the partner's alcohol use, such as financial and health problems and interpersonal fights explain at least some of the increased risk for depression in women who report excessive alcohol use by their partner.
The role of gender attitudes
Consistent with existing research, Reference Patel, Kirkwood, Pednekar, Pereira, Barros and Fernandes16 our findings indicate that gender disadvantage increases risk for common mental health disorders in women. Our study is unique in measuring women's attitudes regarding the acceptability of men's use of violence against their female partners. Women's attitudes condoning male partner violence remained associated with mental illness even when other risk factors were controlled for. Acceptability of violence against women is associated with male domination and gender inequity. Reference Costin and Schwartz38,Reference Nayak, Byrne, Martin and Abraham39 Attitudes condoning male violence may, thus, reflect broader gender inequities and a culture of valuing men over women. Reference Murphy8 Women condoning male violence may view themselves as less valuable and, thereby, having fewer choices than men. Given that gender norms have an impact on health behaviours in men and women, Reference Courtenay40 women's perceptions of being subordinate to men may extend to perceptions of having few options to cope with distress, including that related to men's violence. This could increase ‘learned helplessness,’ setting the stage for clinical anxiety and depression. Reducing gender inequity improves women's health. Reference Backhans, Lundberg and Månsdotter41 Hence, understanding women's own views of their world, health behaviours and choices are critical steps to addressing gender inequities and improving women's health. Reference Moss7
Study limitations
Our study's limitations include possible underestimates of partner excessive alcohol use and alcohol-related problems as these are based on women's reports. Alternatively, our definition of partner excessive alcohol use, which included any occurrence of heavy drinking or drunkenness, may appear too broad and overestimate excessive alcohol use by partners. However, the large majority of partners meeting excessive alcohol use criteria (90%) were reported to usually drink heavily or repeatedly (at least monthly), to drink heavily, or return home drunk in the past year. Our high-response rates (less than 1% refusals for the main interview) significantly reduced selection biases. Nevertheless, recall biases in reporting partner violence, including stigma-related under-reporting, cannot be ruled out. Although past-year partner violence represents a significant and current stressful life event for women, other stressful events such as experiencing childhood or prior adult victimisation were not assessed. Childhood neglect and abuse as well as adult victimisation increase risk for depression in women. Reference Hedtke, Ruggiero, Fitzgerald, Zinzow, Saunders and Resnick42 The possibility of reverse causality must also be considered in interpreting associations reported in a cross-sectional survey.
Implications of findings and related recommendations
Despite these limitations, our findings have important implications for women's mental health that extend beyond the geographical location of the study. Male partner violence and alcohol-related problems are widespread across diverse cultures. Reference Garcia-Moreno, Jansen, Ellsberg, Heise and Watts43,Reference Rahav, Wilsnack, Bloomfield, Gmel and Kuntsche44 Hence, partner alcohol use problems and partner violence must be routinely assessed to prevent and treat common mental disorders in women. Likewise, interventions for male heavy drinkers need to address partner violence and the female partner's health.
The amelioration of negative gender-related beliefs such as condoning male violence and subordination of women is also essential for improving women's health. Barriers to screening for partner violence and partner alcohol use such as stigmatisation of victims of violence Reference Nayak45 and acceptance of male violence and heavy drinking by men can be addressed within healthcare settings via mandatory screening and intervention policies. Integrating violence prevention and intervention programmes into already existing healthcare systems, in particular, helps increase women's access to needed services. At the community level, social deterrents for partner violence and heavy drinking are necessary to reduce poor health outcomes in women.
In resource-scarce environments, such as in India and other low and middle-income countries, coping with the difficulties presented by alcohol misuse for users and their families present a particularly significant challenge. Screening, Brief Intervention and Referral to Treatment (SBIRT) systems for alcohol-related problems Reference Stockwell46 could be implemented in primary care and community outreach settings, and adequate, accessible resources for brief intervention developed as indicated. Reference Rehm and Greenfield47 Future research should evaluate the impact of alcohol-related interventions in promoting recovery from common mental disorders in women with partners who drink.
Acknowledgements
We thank staff at Sangath and community members of the selected areas of Goa for assistance with data collection.









eLetters
No eLetters have been published for this article.