Introduction
There is consistent evidence indicating that traumatic brain injury (TBI) is associated with an increased risk of adverse neuropsychiatric outcomes in adults, including depression, anxiety, posttraumatic stress symptoms, cognitive impairment, personality change, and neurodegenerative disorders (Carroll et al., Reference Carroll, Cassidy, Cancelliere, Côté, Hincapié, Kristman and Hartvigsen2014; Cnossen et al., Reference Cnossen, Scholten, Lingsma, Synnot, Haagsma, Steyerberg and Polinder2017; Fleminger, Reference Fleminger2008; Perry et al., Reference Perry, Sturm, Peterson, Pieper, Bullock, Boeve and Welsh-Bohmer2016; Rogers & Read, Reference Rogers and Read2007; Schwartz, Jodis, Breen, & Parker, Reference Schwartz, Jodis, Breen and Parker2019; van Reekum, Cohen, & Wong, Reference van Reekum, Cohen and Wong2000). One association that has proved more controversial, however, has been the link between TBI and psychosis. Although there are clearly cases of post-TBI psychosis (Fujii & Ahmed, Reference Fujii and Ahmed2002), the extent to which TBI is a reliable population risk factor for psychosis has been debated. In a narrative review of the evidence, David and Prince (Reference David and Prince2005) concluded that it was unlikely brain injury reliably causes psychosis given the published data available at the time. In a subsequent narrative review, Batty, Rossell, Francis, and Ponsford (Reference Batty, Rossell, Francis and Ponsford2013) estimated that psychosis following TBI appears to be three times more prevalent than psychotic disorders in the general population. Looking specifically at the association between TBI and schizophrenia in case–control studies, Molloy, Conroy, Cotter, and Cannon's (Reference Molloy, Conroy, Cotter and Cannon2011) meta-analysis reported a significant association and, through the inclusion of family studies, suggested this effect was larger in those with a genetic predisposition to psychosis.
Notably, however, the studies considered in these reviews largely examined the impact of adult TBI on later psychosis. Although clearly important, studies that focus solely on adult TBI may miss longer-term associations between TBI that occurs before the age of 18 and an increased risk of psychotic disorders or symptoms later in life. The association between pediatric TBI (pTBI) and psychosis is plausible given what we know about risk factors for psychosis in childhood and adolescence. Key developmental models of psychosis, including the psychosis-proneness-persistence-impairment model (Linscott & van Os, Reference Linscott and van Os2013; van Os, Linscott, Myin-Germeys, Delespaul, & Krabbendam, Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009) and the developmental risk factor model (Howes & Murray, Reference Howes and Murray2014; Murray, Bhavsar, Tripoli, & Howes, Reference Murray, Bhavsar, Tripoli and Howes2017), are based on evidence that adverse experiences that impair typical neurodevelopment can maintain normally transient sub-threshold symptoms of psychosis during adolescence and increase the risk of later transition to psychotic disorders (Rubio, Sanjuan, Florez-Salamanca, & Cuesta, Reference Rubio, Sanjuan, Florez-Salamanca and Cuesta2012; Trotta, Murray, & Fisher, Reference Trotta, Murray and Fisher2015). It has been suggested that pTBI could be one such neurodevelopmental risk factor (AbdelMalik, Husted, Chow, & Bassett, Reference AbdelMalik, Husted, Chow and Bassett2003), but this has never been subjected to systematic review and meta-analysis. Although Molloy et al. (Reference Molloy, Conroy, Cotter and Cannon2011) included a subgroup analysis on pTBI cases in their meta-analysis, only three studies were available at the time, indicating a clear need for a more systematic analysis of this issue as new studies have emerged.
Consequently, we conducted a pre-registered systematic review and meta-analysis to determine the association between pTBI and later psychotic disorders or symptoms of psychosis. To the best of our knowledge, this is the first meta-analysis to examine pTBI as a potential risk factor for psychotic disorders or symptoms.
Methods
The present systematic review and meta-analysis was undertaken and reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow and Moher2021).
Eligibility criteria
Participants
We included studies that recruited participants of any age or gender with a diagnosis of pTBI.
Exposures
pTBI was defined as an onset of TBI before adulthood (i.e. <18 years old). pTBI could be determined by the age of the study population (e.g. children or adolescents with TBIs) or the time of onset of TBI (e.g. adults with a history of pTBI). We included participants with a diagnosis of pTBI based on validated screening tools, structured clinical interviews, medical records reviews, or clinical diagnosis. TBIs with severity ranging from mild (including concussion) to severe were included. For exclusion, we did not select studies where the occurrence of pTBI could not be determined, and when psychotic disorders or symptoms were not measured. In addition, we did not include studies when exposure to TBI could not be differentiated from other non-TBI conditions within a single group.
Comparators
Studies with and without comparison groups were included, with no exclusion criteria applied.
Outcomes
The main outcome of interest was presence of psychotic disorders or psychotic symptoms based on validated screening tools, psychometric measures, structured clinical interviews, medical records reviews, or clinical diagnosis. Psychotic disorders included schizophrenia and related disorders, whilst psychotic symptoms included psychosis-risk syndromes, psychotic symptoms, and psychotic-like experiences (PLEs). We only included studies where the onset of the psychotic disorder/symptoms occurred after the TBI. We excluded studies reporting only broad neuropsychiatric outcomes (such as behavioral difficulties) without any specific assessment of psychosis.
Types of studies included
We included all peer-reviewed primary studies published in English with no date restrictions. The following types of design were included: randomized or non-randomized controlled trials, retrospective or prospective cohort studies, and case–control studies (including nested case–control and family studies). We excluded meta-analyses, systematic reviews, literature reviews, case reports, case series, qualitative studies, opinion pieces, editorials, comments, newsletters, book chapters, and congress papers.
Information sources and search strategy
The databases of PsycINFO (Ovid) (from 1806 onwards) and MEDLINE (Ovid) (from 1946 onwards) were searched based on the strategy outlined in Table 1 (see Appendix S1 for full search strategy), with the search carried out independently by two reviewers (K.-C. Y., G. R.). Studies were screened according to the above criteria. Prior to the final analysis, searches were re-run on 1 December 2022 to identify any further studies that could be included in the review.
Table 1. Search strategy

Note. ab, abstract; ag, age group; id, key concepts; kw, keyword heading; ti, title.
Study selection process
Following removal of duplicates, two reviewers (K.-C. Y., G. R.) independently screened the titles and abstracts of all the records retrieved. A third reviewer (V. B.) was consulted when a consensus could not be reached. Two reviewers (K.-C. Y., G. R.) independently screened the full-text reports based on the above eligibility criteria, and processes of discussion between the two reviewers and consultation with the third reviewer (V. B.), in the case of disagreement, were held.
Data extraction process
A data extraction excel sheet was developed by one of the reviewers (K.-C. Y.). Two reviewers (K.-C. Y., G. R.) independently extracted study characteristics and outcomes from all the included studies, and data were compared. A third reviewer (V. B.) was consulted when a consensus could not be reached.
Data items
Outcomes
The main outcome was presence of a psychotic disorder or psychotic symptoms including schizophrenia, psychosis, hallucination, paranoia, psychosis-risk syndromes, and PLEs. Diagnoses of schizophrenia, psychosis, hallucination, and paranoia based on the International Statistical Classification of Diseases and Related Health Problems (ICD), the Diagnostic and Statistical Manual of Mental Disorders (DSM), or Feighner et al. (Reference Feighner, Robins, Guze, Woodruff, Winokur and Munoz1972) criteria were used. We also extracted sub-threshold symptoms of psychosis including psychosis-risk syndromes (McGlashan, Walsh, & Woods, Reference McGlashan, Walsh and Woods2010) and PLEs (Lee et al., Reference Lee, Chan, Chang, Lee, Hui and Chen2016). For methods of outcome measurement, validated screening tools and psychometric measures (including Prodromal Psychosis Questionnaire – Brief Child Version [PQ-BC] by Karcher et al. [Reference Karcher, Barch, Avenevoli, Savill, Huber, Simon and Loewy2018]), structured clinical interviews, medical records reviews, and clinical diagnosis were included. Regarding the onset of psychotic disorders or symptoms, anytime time point was eligible (i.e. childhood, adolescence, or adulthood) provided the onset was after pTBI.
Regarding the major outcome data, we primarily extracted the number of participants experiencing psychotic disorders or symptoms after pTBI. When studies used several methods for reporting the relevant data, we followed a priori defined rules of decision to select corresponding data. (i) When both the raw number of participants experiencing psychotic disorders or symptoms and the calculated statistics (e.g. incidence rate ratios [IRRs]; odds ratio [ORs]) were available, we extracted the raw number. (ii) When descriptive statistics of interval measures of psychotic disorders or symptoms and the calculated statistics (e.g. p values or effect sizes) were available, we extracted the descriptive statistics. (iii) When both non-imputed and imputed data were reported, we chose the imputed. (iv) Lastly, we extracted the set of raw number based on primary analysis of the original study.
Where the required data had not been published (three studies: Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022; Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014; Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002), authors were contacted for the required information (e.g. asking for total number of participants in the exposure group of pTBI. Two authors responded but only one (Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022) could provide the required raw data. The remaining two studies were only included in narrative synthesis but not meta-analysis.
Exposures
We included all TBIs with severity ranging from mild (including concussion) to severe. For methods of measurement, validated screening tools (including the Ohio State University TBI Identification Method [OSU TBI-ID]; Corrigan and Bogner, Reference Corrigan and Bogner2007), structured clinical interviews, medical records reviews, and clinical diagnosis were included. Regarding the major exposure data, we primarily extracted the number of participants experiencing TBI.
Study characteristics
For the characteristics of included studies, apart from the above exposure and outcome data items, we also extracted the (i) year and location of the study, (ii) study design, and (iii) participant characteristics (in the exposure and control groups, if any).
Quality assessment
Two reviewers (KCY & GR) independently assessed the quality of included studies using Kmet, Lee, & Cook's (Reference Kmet, Lee and Cook2004) quality assessment scale. This consisted of a 14-item checklist on a 3-point scale (0 = criteria not met; 1 = partially met; 2 = fully met) generating a summary score (total sum / total possible sum) ranging from 0 to 100, to categorize the low (⩽54), moderate (55–74), and high (⩾75) quality of evidence. The areas of assessment included evaluation of appropriateness of research objectives, study design, sampling methods, recruitment of participants, adoption of measures, sample size, statistical analyses, estimate of variance, control for confounders, results reported, and conclusion drawn. All disagreements were resolved by consensus.
Synthesis methods
We estimated the meta-analytic OR with 95% confidence interval (CI) of psychotic disorders or symptoms associated with preceding pTBI among the included studies using the R package ‘meta’ (Balduzzi, Rücker, & Schwarzer, Reference Balduzzi, Rücker and Schwarzer2019). We computed the I 2 statistic to measure heterogeneity among included studies, and the levels of low, moderate, and high heterogeneity were assigned to I 2 values of 25, 50, and 75% respectively (Higgins et al., Reference Higgins, Thompson, Deeks and Altman2003). We expected a moderate-to-high I 2 value due to methodological heterogeneity, and subsequently we opted to use a random-effects model to estimate pooled estimates using the Paule–Mandel estimator (Paule & Mandel, Reference Paule and Mandel1982) given evidence for its lower risk of bias compared to other methods (Langan, Higgins, & Simmonds, Reference Langan, Higgins and Simmonds2017). We used a funnel plot to test for evidence of publication bias and Egger's test was planned to provide a statistical test of funnel plot asymmetry (Ioannidis & Trikalinos, Reference Ioannidis and Trikalinos2007). Subgroup analyses based on (i) study location, (ii) study design (i.e. case–control study v. cohort study), (iii) type of outcome being measured (i.e. psychotic disorders v. symptoms or sub-threshold symptoms of psychosis), (iv) type of outcome measurement (i.e. clinical diagnosis v. validated/structured method), and (v) time of onset of the outcomes (i.e. childhood/adolescence v. adulthood) were conducted. We followed the suggested guidelines reporting any detections of statistically significant subgroup differences (Richardson, Garner, & Donegan, Reference Richardson, Garner and Donegan2019). Afterwards, we conducted Viechtbauer and Cheung's (Reference Viechtbauer and Cheung2010) outlier and influential study diagnostics and a leave-one-out sensitivity analysis to assess the presence of any overly influential studies in estimating the pooled effect. We also completed a meta-regression to estimate whether study quality was related to study outcome. If the meta-regression was statistically significant, a sensitivity analysis was performed to assess whether the pooled association remained robust after removing studies of low quality.
All analyses were conducted with R (version 4.2.1; R Core Team, 2020) and were conducted on a Linux x86_64 platform. All R code and data for the analyses are available online in the following archive: https://github.com/vaughanbell/pTBI_psychosis_meta-analysis
For any studies that did not yield meta-analyzed results, we planned to conduct a narrative synthesis to assess how the additional studies might affect the interpretation of the overall findings, using ESRC guidelines (Popay et al., Reference Popay, Roberts, Sowden, Petticrew, Arai, Rodgers and Duffy2006).
Results
Study selection
A total of 850 records resulted from searching the PsycINFO (n = 365) and MEDLINE (n = 485) databases. After removing duplicates by Ovid's automatic de-duplication feature, 688 records remained. Seventy records were eligible for full-text screening, of these 60 were excluded. A total of 10 studies were included in this review. See Fig. 1 for PRISMA 2020 flow diagram.

Figure 1. PRISMA 2020 flow diagram for literature search.
Study characteristics
Among the 10 included studies, five adopted case–control designs (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; Deighton et al., Reference Deighton, Buchy, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006; Helgeland & Torgersen, Reference Helgeland and Torgersen2005; Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987) and five adopted cohort designs (Ledoux et al., Reference Ledoux, Webster, Clarke, Fell, Knight, Gardner and Zemek2022; Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022; Massagli et al., Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004; Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014; Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002). Four studies were carried out in the United States (Deighton et al., Reference Deighton, Buchy, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022; Massagli et al., Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004; Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987), whilst the remaining six studies were undertaken in other places including Canada (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; Ledoux et al., Reference Ledoux, Webster, Clarke, Fell, Knight, Gardner and Zemek2022), Denmark (Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014), Finland (Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002), Norway (Helgeland & Torgersen, Reference Helgeland and Torgersen2005), and Sweden (Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006). Five studies measured schizophrenia as an outcome (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006; Helgeland & Torgersen, Reference Helgeland and Torgersen2005; Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002; Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987), four studies measured psychosis (Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006; Ledoux et al., Reference Ledoux, Webster, Clarke, Fell, Knight, Gardner and Zemek2022; Massagli et al., Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004; Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014), and two studies investigated sub-threshold symptoms of psychosis (Deighton et al., Reference Deighton, Buchy, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022). For the method of outcome measurement, six studies adopted clinical diagnosis (Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006; Ledoux et al., Reference Ledoux, Webster, Clarke, Fell, Knight, Gardner and Zemek2022; Massagli et al., Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004; Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014; Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002; Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987), whilst the remaining four studies adopted validated psychometric measures or structured clinical interviews (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; Deighton et al., Reference Deighton, Buchy, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Helgeland & Torgersen, Reference Helgeland and Torgersen2005; Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022). Finally, in terms of the window of interest regarding the onset of a psychotic disorder or psychotic symptom, six studies reported psychotic disorders or symptoms in adulthood (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; Deighton et al., Reference Deighton, Buchy, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Harrison et al., Reference Harrison, Whitley, Rasmussen, Lewis, Dalman and Gunnell2006; Orlovska et al., Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014; Timonen et al., Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002; Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987), whilst the remaining four studies reported childhood and adolescence (Helgeland & Torgersen, Reference Helgeland and Torgersen2005; Ledoux et al., Reference Ledoux, Webster, Clarke, Fell, Knight, Gardner and Zemek2022; Lopez et al., Reference Lopez, Christensen, Foxe, Ziemer, Nicklas and Freedman2022; Massagli et al., Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004). Detailed characteristics of all the included primary studies are shown in online Supplementary Table S1. A summary of included study characteristics are presented in Table 2. Details of the quality assessment ratings are reported in online Supplementary Table S2, with seven studies rated as demonstrating high quality of evidence, one moderate, and two low.
Table 2. Comparison data for probability of psychotic disorders or symptoms following pTBI
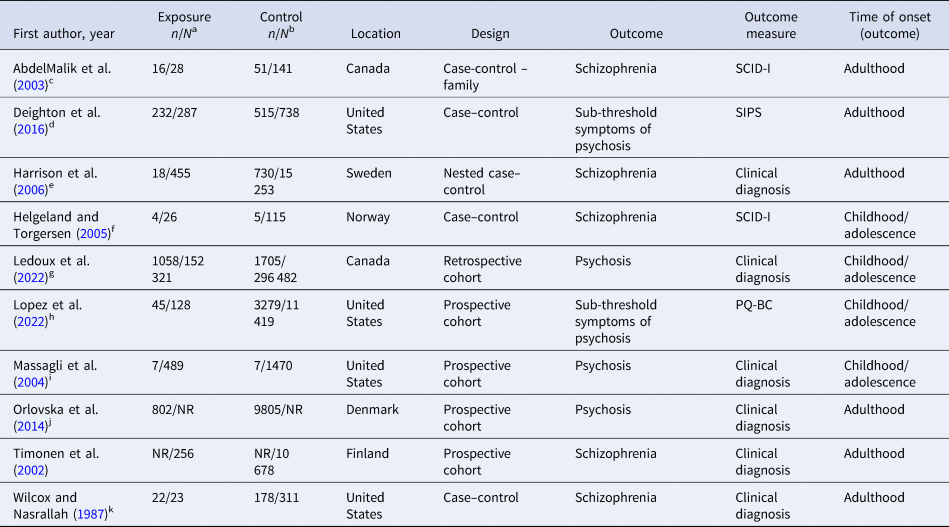
Note. NR, not reported; PQ-BC, Prodromal Questionnaire –Brief Child Version; pTBI, pediatric traumatic brain injury; SCID-I, Structured Clinical Interview for DSM Axis I Disorders; SIPS, Structured Interview for Psychosis-risk Syndromes.
a Exposure n/N = (number of participants in pTBI exposure group having psychotic disorders or symptoms)/(number of participants in pTBI exposure group).
b Control n/N = (number of participants in non-pTBI control group having psychotic disorders or symptoms)/(number of participants in non-pTBI control group).
c TBI in childhood (⩽10 years old) was chosen over throughout adolescence (⩽17 years old) due to primary analysis of the original study.
d Comparison between clinical high risk (CHR) of psychosis and healthy controls (HC) was chosen due to primary analysis of the original study.
e Schizophrenia was chosen over non-affective psychosis due to more precise measurement of psychotic disorder.
f Both concussion and head traumas were chosen and aggregated.
g Raw data on number of participants in relation to psychosis reported in the supplemental materials were used.
h Data provided by the original author.
i 3-year follow-up was chosen due to primary analysis of the original study.
j Hospital contacts for head injury from 0–15 years old were chosen.
k Surgical control was chosen due to primary analysis of the original study.
Synthesis of results
Overall pooled analysis
Among the 10 included studies, raw data from two were either not published or not provided by the original authors after contacts and were therefore excluded from the meta-analysis. Based on eight studies, with a pooled sample size of 479 686 (153 757 in the pTBI group; 325 929 in the control group), there was an overall significant positive association between exposure to pTBI and outcomes of psychotic disorders or symptoms (pooled OR = 1.80, 95% CI 1.11–2.95) with moderate between-study heterogeneity (I 2 = 69%, τ 2 = 0.35, p < 0.01). Figure 2 shows the comparison data and forest plot of the corresponding analysis.

Figure 2. Comparison data and forest plot of odds ratio meta-analysis for psychotic disorders or symptoms.
Subgroup analyses
Subgroup analyses based on study location (p = 0.34), design (p = 0.30), psychotic disorder v. subthreshold symptoms of psychosis (p = 0.48), measurement type (p = 0.77), time of onset (that psychotic disorder/symptoms emerged) (p = 0.62) were all non-significant, suggesting that these variables did not modify the effect of pTBI on the probability of psychotic disorders/symptoms. Forest plots of all the above subgroup analyses are reported in online Supplementary Figs S1–S5.
In the subgroup analysis comparing psychotic disorder with subthreshold symptoms of psychosis, both remained reliably associated with pTBI (psychotic disorder OR = 2.11, 95% CI 1.01–4.37; subthreshold symptoms of psychosis OR = 1.58, 95% CI 1.17–2.13)
Robustness and sensitivity analyses
For the assessment of publication bias, visual inspection of the funnel plot (Fig. 3) appeared to exhibit asymmetry. Egger's test was completed (p = 0.052) although was likely under-powered given 10 studies are considered the minimum for a reliable assessment of publication bias (Ioannidis & Trikalinos, Reference Ioannidis and Trikalinos2007).

Figure 3. Funnel plot of standard error by odds ratio in meta-analysis.
No studies were identified as outliers but one study (Wilcox & Nasrallah, Reference Wilcox and Nasrallah1987) was identified as excessively influential using Viechtbauer and Cheung's (Reference Viechtbauer and Cheung2010) outlier and influential diagnostics. A leave-one-out sensitivity analysis showed that removing Wilcox and Nasrallah (Reference Wilcox and Nasrallah1987) reduced the pooled estimate although the association between pTBI and psychosis outcomes remained reliable (OR = 1.52, 95% CI 1.08–2.14). The removal of one study altered the estimate to the non-significant range, namely Massagli et al. (Reference Massagli, Fann, Burington, Jaffe, Katon and Thompson2004) revised estimate (OR = 1.74, 95% CI 0.9997–3.04).
A meta-regression analysis indicated that the quality of evidence summary score predicted the association between pTBI and psychotic disorders/symptoms, albeit weakly (random-effects estimate = −0.037, 95% CI −0.06 to −0.01, p = 0.003). Consequently, we completed a sensitivity analysis removing studies with evidence rated as low quality and recalculating the pooled estimate. The revised pooled estimate (see Fig. 4) remained significant with narrower CIs suggesting a more accurate estimate (OR = 1.43, 95% CI 1.04–1.98) and slightly reduced heterogeneity (I 2 = 64%, τ 2 = 0.10, p = 0.02).

Figure 4. Comparison data and forest plot of odds ratio meta-analysis for psychotic disorders or symptoms – sensitivity analysis by the removal of studies with low quality of evidence.
Narrative synthesis including additional studies
Two cohort studies were not included in the meta-analysis due to insufficient data, namely Orlovska et al. (Reference Orlovska, Pedersen, Benros, Mortensen, Agerbo and Nordentoft2014) and Timonen et al. (Reference Timonen, Miettunen, Hakko, Zitting, Veijola, von Wendt and Räsänen2002). Orlovska et al. reported that, compared with individuals without hospital contact for head injury, those exposed to head injury between ages 0 and 5 years had higher rates of schizophrenia spectrum disorders (adjusted incident rate ratio [aIRR] = 1.35, 95% CI 1.18–1.54). In addition, differing effects of head injury at 6–10 years (aIRR = 1.33, 95% CI 1.16–1.50) and 11–15 years (aIRR = 1.86, 95% CI 1.66–2.07) were observed. In Timonen et al., although the original analysis focused on the association between preceding pTBI and the broad outcomes of mental disorders, Molloy et al. (Reference Molloy, Conroy, Cotter and Cannon2011) contacted the original authors and reported no association between pTBI and the subsequent development of schizophrenia (OR = 1.1, 95% CI 0.41–2.96) although the wide CIs indicate that the estimate would carry less weight in estimating an overall effect.
Discussion
We conducted a systematic review and meta-analysis to estimate the association between pTBI and psychosis, including both frank psychotic disorders and psychotic symptoms. Based on a pooled sample size of 479 686, it was found that pTBI was associated with an increased probability of psychotic disorders and symptoms, with moderate between-study heterogeneity. Regarding the robustness of findings, the estimated association passed robustness tests for study quality, outliers, and excessively influential studies, although the removal of one would have reduced confidence in a reliable association in a leave-one-out sensitivity analysis. This reflects the fact that the lower bound of the CI for the pooled estimate was only marginally above one and therefore confidence in the reliability of this estimate must be taken cautiously. Two studies were identified in the systematic review which could not be included in the meta-analysis, and these studies reporting conflicting results. However, given the characteristics of these additional studies, we consider that including them would have moderately increased our confidence in an association between pTBI and psychosis. Consequently, we conclude that this analysis provides additional evidence for an association between pTBI and psychosis. However, concerns remain about the long-run reliability of this estimate and new studies will be crucial in deciding this issue.
In relating the above findings to the field, our results raise the feasibility of potential causal associations between pTBI and psychosis. Developmental models of psychosis suggest that pTBI could be a plausible risk factor for psychosis, given that the full spectrum of pTBI (from mild pTBI to severe brain injury) has established effects on neurodevelopment (Emery et al., Reference Emery, Barlow, Brooks, Max, Villavicencio-Requis, Gnanakumar and Yeates2016; Goh et al., Reference Goh, Looi, Goh, Sultana, Goh, Lee and Chong2021), and events that have an adverse impact on neurodevelopment are known risk factors for psychosis (Howes & Murray, Reference Howes and Murray2014; Murray et al., Reference Murray, Bhavsar, Tripoli and Howes2017). Our meta-analytic results seem to suggest the role of pTBI as a risk factor for psychosis. However, reverse causality or shared risk factor pathways are also possible. Brain injuries have been hypothesized to be more common in young people who have a higher risk for psychosis, as they may already show subtle premorbid difficulties such as motor coordination leading to a higher risk for accidental injuries (AbdelMalik et al., Reference AbdelMalik, Husted, Chow and Bassett2003; David & Prince, Reference David and Prince2005). Furthermore, psychotic symptoms, including in people without frank psychosis, are associated with higher rates of early-life bullying (Catone et al., Reference Catone, Marwaha, Kuipers, Lennox, Freeman, Bebbington and Broome2015; Valmaggia et al., Reference Valmaggia, Day, Kroll, Laing, Byrne, Fusar-Poli and McGuire2015), suggesting a possible reverse or reciprocal association between psychotic spectrum phenomena and acquired brain injury through victimization violence. A well-designed prospective cohort study would be needed to reliably identify relationships between pTBI, psychotic symptoms, and any potential confounders and/or mediators.
Nevertheless, given the concordance between the findings reported here and developmental models of psychosis (Howes & Murray, Reference Howes and Murray2014; Murray et al., Reference Murray, Bhavsar, Tripoli and Howes2017), this may suggest that history of pTBI may be a useful addition when taking a history of patients with psychosis and that public health that prevent pTBI may have longer-term benefits for lifetime mental health.
A strength of this study is the use of systematic procedures to comprehensively search for eligible studies. We also included sensitivity analyses to ensure robustness of the findings. In addition, we pre-registered the review to reduce the risk of bias. Moreover, the meta-analysis is available online as a computational notebook with an open dataset, to enhance openness and reproducibility.
However, we note several limitations of this study. The first is that the included studies are heterogeneous in terms of their measured outcomes design (case–control v. cohort), outcome (symptoms v. disorder), outcome measure (clinical diagnosis v. validated measure), and life-stage of measured psychosis outcome (adulthood v. childhood/adolescence). Our subgroup analyses found no evidence for difference of association between subgroups. We note the potential for low statistical power to make identifying associations within subgroups difficult, given than subgroups typically included 3–4 studies. However, the heterogeneity of studies reflects the fact that many were not primarily designed to assess the association with pTBI and psychosis spectrum phenomena, and more focused and better design studies are clearly needed. Inspection of the funnel plot indicated a potential for publication bias which could have reduced the accuracy or the direction of the estimate. In addition, studies either did not report severity of brain injury, or did not distinguish between severity, meaning it was not possible to examine whether there was a ‘dose–response’ relationship between TBI and later psychosis, a potentially important consideration when examining evidence for causality. We also note that we solely included studies published in English, and listed in primarily English language databases, potentially missing some potentially useful evidence.
Based on the above discussions, it is recommended that future research focus on specifically assessing the association between pTBI and psychosis spectrum phenomena. In addition, to rule out the possible reverse association, a well-designed prospective cohort study would be needed to reliably identify relationships between pTBI, psychotic symptoms, and any potential confounders and/or mediators. Additionally, future studies specifying the type of TBI (e.g. due to accidents or other sources), and location and type of injury, would enhance our understanding of the presence/absence of an etiological relationship between pTBI and psychosis. Lastly, future reviews should consider including non-English language databases.
In conclusion, our systematic review and meta-analysis reports evidence for a positive association between pTBI and subsequent outcomes of psychotic disorders or symptoms but with caveats regarding our confidence in the long-term reliability of this association as new evidence emerges.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723002878.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.









