Introduction
Suicide is one of the main external causes of death worldwide. The world health organization [WHO] has tracked suicide trends over the years and has pointed out the need to act urgently to tackle suicide impact worldwide (WHO, 2014). Thus, in their latest seminal report, the WHO reported that suicide accounted for more than 700 000 deaths in 2019 (WHO, 2023).
Even then, deaths by suicide are just the tip of the iceberg. Other suicide-related behaviors, such as suicidal attempts or ideation (while not strictly a behavior) have much higher prevalence (Nock et al., Reference Nock, Borges, Bromet, Cha, Kessler and Lee2008; WHO, 2014). Previous attempts are one of the most relevant risk factors for death by suicide (Mendez-Bustos, De Leon-Martinez, Miret, Baca-Garcia, & Lopez-Castroman, Reference Mendez-Bustos, De Leon-Martinez, Miret, Baca-Garcia and Lopez-Castroman2013). A recent meta-analysis suggests that one in five people who attempts suicide could repeat it (de la Torre-Luque et al., Reference de la Torre-Luque, Pemau, Ayad-Ahmed, Borges, Fernandez-Sevillano, Garrido-Torres and Ayuso-Mateos2023).
Risk factors for suicidal behavior represent a highly relevant line of work. Considering variables associated with suicidal history, the effect of ideation (at different levels of structuring) and the presence of multiple attempts are well established (De La Garza, Blanco, Olfson, & Wall, Reference De La Garza, Blanco, Olfson and Wall2021; Mendez-Bustos et al., Reference Mendez-Bustos, De Leon-Martinez, Miret, Baca-Garcia and Lopez-Castroman2013). Other psychosocial aspects such as non-suicidal self-injury, trauma, or high impulsivity are also relevant (Daray et al., Reference Daray, Rojas, Bridges, Badour, Grendas, Rodante and Rebok2016; Hawton, Saunders, & O'Connor, Reference Hawton, Saunders and O'Connor2012; Ng, Yong, Ho, Lim, & Yeo, Reference Ng, Yong, Ho, Lim and Yeo2018; Zatti et al., Reference Zatti, Rosa, Barros, Valdivia, Calegaro, Freitas and Schuch2017). Socio-demographic factors have also been studied: with respect to sex, there are more deaths by suicide in men but more attempts in women. Regarding age groups, young people and the elderly represent special risk groups (WHO, 2014).
However, despite knowing these suicide attempt risk factors, the knowledge is not directly transferable to reattempts (Mendez-Bustos et al., Reference Mendez-Bustos, De Leon-Martinez, Miret, Baca-Garcia and Lopez-Castroman2013). Some relevant risk factors in a first attempt may not be so when repeating. Studies in this regard are fewer, and there is a lack of clear evidence on the weight of each risk factor in successive attempts throughout life. In addition, the differences in terms of sample and methodology make it difficult to obtain clear conclusions (de la Torre-Luque et al., Reference de la Torre-Luque, Pemau, Ayad-Ahmed, Borges, Fernandez-Sevillano, Garrido-Torres and Ayuso-Mateos2023).
There are two groups of particularly interesting variables when talking about reattempt. On one hand, those related to the person's own history of suicide. These variables have been associated with the so-called acquired capability for suicide. This concept is related to the habituation to suicide and the fearlessness of death or pain (Klonsky, Saffer, & Bryan, Reference Klonsky, Saffer and Bryan2018). On the other hand, the volitional risk factors. This term refers to those variables that predict the transition from suicidal ideation to suicide attempt in the Integrated Motivational-Volitional Model (O'Connor & Kirtley, Reference O'Connor and Kirtley2018).
Further precise knowledge of how risk factors differ between first attempters and reattempters could help provide more personalized help. The study has two main objectives:
1) Calculate the risk of suicide reattempt in the presence of suicidal history and psychosocial risk factors.
2) Estimate the magnitude of the effect of each risk factor.
Methods
This study followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols 2020 (PRISMA 2020) statement (Page et al., Reference Page, McKenzie, Bossuyt, Boutron, Hoffmann, Mulrow and Moher2021).
Article selection criteria
The PICOS (Population, Intervention, Comparison, Outcomes and Study) matrix guided the selection of the units of analysis. Starting with the population, studies with human participants of all ages who had attempted suicide (index attempt) and were admitted to a hospital department due to this attempt, were selected. Regarding intervention, participants had to be assessed with respect to suicidality. In terms of control criteria, studies should have either (a) a control group of individuals who engaged in a suicide attempt without reattempting; (b) a baseline assessment of reattempters in longitudinal studies. Regarding outcome criteria, studies had to include a measure of reattempt risk and information on at least one of these risk factors:
– Those directly related to suicide history: previous suicide attempts (attempts prior to the index one) and suicidal ideation.
– Those that facilitate the transition from suicidal ideation to attempt (whether related to impulse control or exposure to pain): alcohol misuse, drug misuse, non-suicidal self-injury, trauma, or impulsivity.
Finally, regarding study criteria, longitudinal studies (both prospective and retrospective) published in Spanish or English until March 2022 were considered. Studies with cross-sectional measures were discarded.
Search strategy and data extraction
Studies were located following an ascendant approach. The consulted databases were: Web of Science, PubMed, PsycInfo, SCOPUS, CINAHL, and the Cochrane Library. The search was done by combining the following keywords: Suicide attempt and repetition. The exact searches can be found in online Supplementary Table S1 of the supplementary materials.
Found papers were screened, collecting titles, abstracts, and keywords. Next, the papers selected in the first step were read in full, to decide if they were included. An independent peer reviewer endorsed the selection of every paper to be included. In case of discrepancies, they were resolved by discussion.
Relevant data were extracted from each article using a coding manual, made purposely. Data collected from each study covered bibliometric features (i.e. year of publication, country), methodological features of the study (i.e. sample size, mean age of participants, sex ratio), suicide-related features (suicidal ideation, previous suicide history), and other relevant psychological traits (alcohol or drugs misuse, trauma, non-suicidal self-injury, and impulsivity). All risk factors were measured at baseline.
The Newcastle – Ottawa Quality Assessment Scale (NOS) (Wells et al., Reference Wells, Shea, O'Connell, Peterson, Welch, Losos and Tugwell2000) was used to measure the methodological quality of the studies.
Data analysis
Multilevel mixed-effects meta-regression was used to estimate the overall repetition Odds Ratio (OR), derived from pooling risk estimates from each primary study. Heterogeneity among the individual effect sizes was analyzed by means of the Cochran's Q statistic and the Higgins and Thompson I 2 statistic (Higgins & Thompson, Reference Higgins and Thompson2002; Higgins, Thompson, Deeks, & Altman, Reference Higgins, Thompson, Deeks and Altman2003).
Sensitivity analysis was conducted for each of the risk factors separately (the high variability between risk factors in each study prevented combined meta-regression techniques). OR was used as a measure of effect size for the individual factor effect size. The varying effect size estimates (relative risk, hazard ratio, or Cohen's d) from the individual studies were transformed into a common metric (OR).
When the same study included samples with several risk factors, all of them were included. If the study featured treatments, only the control groups were used. Finally, if there were several temporal follow-ups, only the longest one was considered.
The restricted maximum-likelihood estimator was used to estimate overall effect size and variance (under the inverse variance method). The forest plot was used to visually display the individual effect sizes (presented for sensitivity analysis).
Publication bias was studied by means of Egger's regression asymmetry test.
All the analyses were conducted using the software R (R Core Team, 2017) version 4.2.2, with packages meta and metaphor.
Results
The initial search resulted in 11 905 articles. After removing duplicates, 3672 abstracts were screened. Of those, 651 articles were read in full, and 34 papers presented data relevant to the study, jointly presenting 52 different effect sizes. Table 1 shows the characteristics of each of the studies. In cases where a study measured different risk factors, it appears several times, showing in each case the size of the relevant effect. Figure 1 shows the article selection flowchart.
Table 1. Features of studies
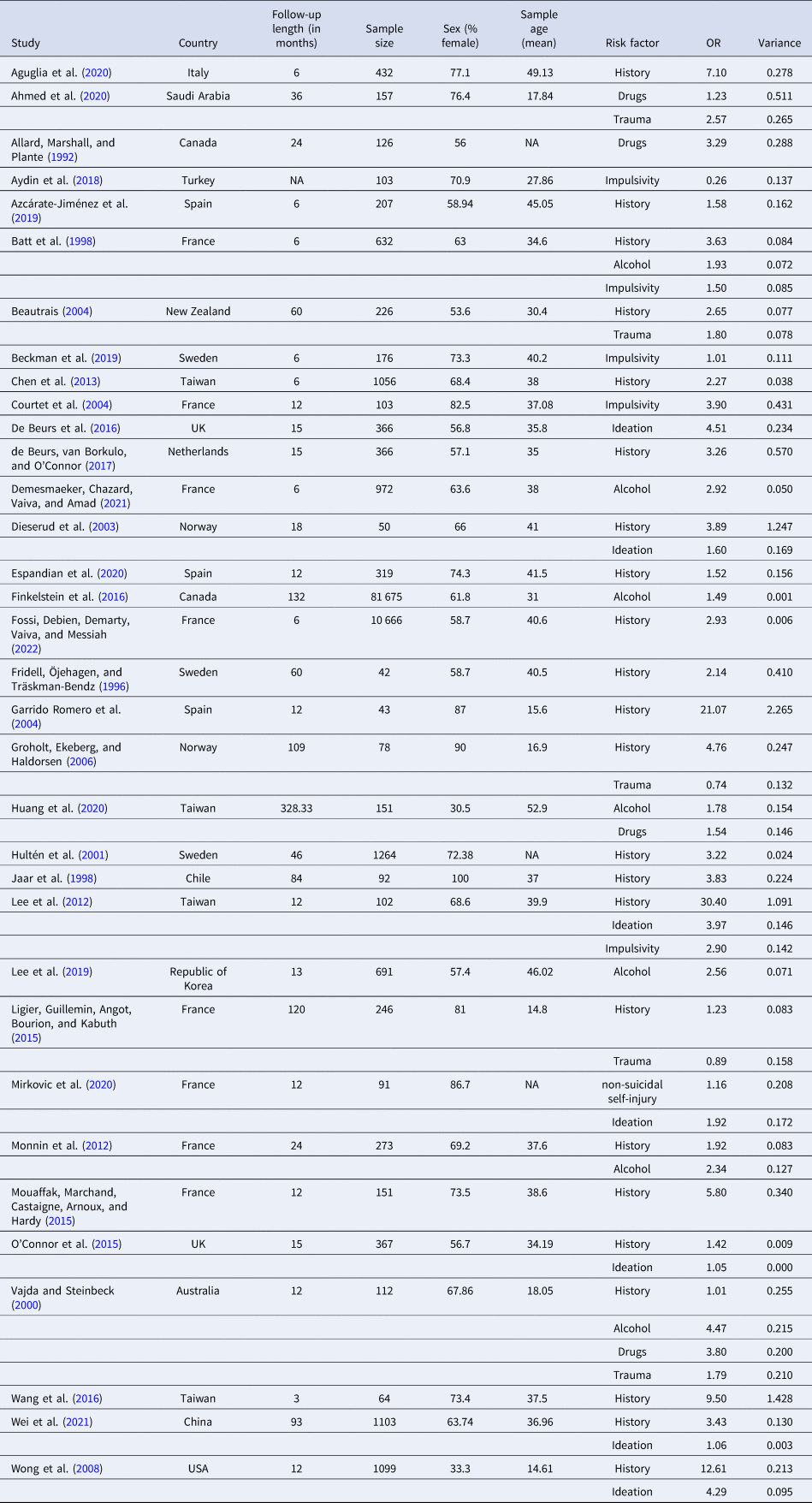
†Country of the correspondence author's affiliation.
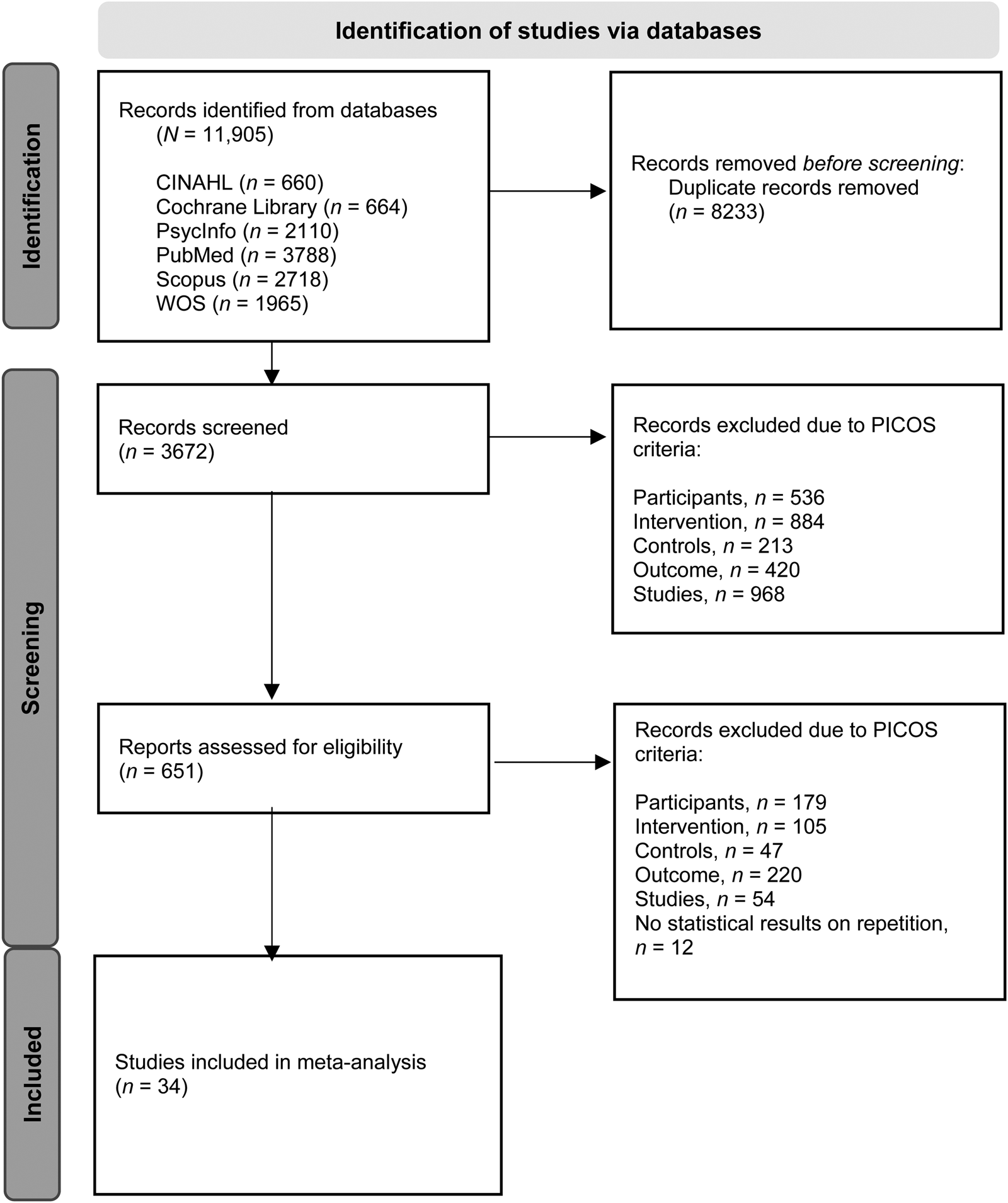
Figure 1. Flow diagram of studies selected for this meta-analysis.
Most studies came from France (23.53%), followed by Taiwan (11.8%), Spain, and Sweden (8.8% in both cases). Almost 60% of the works were published after 2013. The follow-up period ranged from 3 to 328 months (M = 40.40, s.d. = 63.17, Median = 13). The articles considered a total sample size of 103 601 attempters (M = 3047.09, s.d. = 14 009.69, Median = 216.5). The mean age of participants was 34.33 years old (s.d. = 10.29, Median = 37.08).
First, the multilevel mixed-effects model was carried out without introducing moderators (σ 2 = 0.28, OR 2.16, CI95 [1.75–2.68], Z = 7.12, p = < 0.01). High heterogeneity was observed (Q = 652.87, p < 0.01).
Then, regarding the multilevel mixed-effects meta-regression, an analysis was carried out introducing the percentage of women in the sample, the follow-up period, and the mean age as covariates. This model showed a random-effects variance of σ 2 = 0.18; and QM (3) = 3.03, p = 0.39. No covariate showed a significant loading in the model. Egger's regression pointed to the possible existence of bias (Z = 3.17, p < 0.01).
Since the diverse specific risk factors of each sample cannot be included in the same model (each study uses a different one, which would prevent joint analyses), we then opted for sensitivity analysis with the different risk factors.
The sensitivity analyses focused on specific risk factors are presented below. The most studied risk factor in the literature was the history of suicide prior to the index attempt (k = 23). The effect of suicide attempt history on reattempt was significant (OR 2.85, CI95 [2.19–3.71], Z = 7.78, p = < 0.01). Heterogeneity was significant (Q = 87.14, p < 0.01, I2 = 78.24%).
Regarding studies focused on the presence of active ideation at baseline (k = 7), a significant OR was found (OR 2.05, CI95 [1.24–3.40], Z = 2.78, p < 0.01). Between-study heterogeneity was high (Q = 45.18, p < 0.01, I2 = 97.97%).
Regarding alcohol misuse, seven studies analyzed its role as a risk factor for suicide reattempts. The analysis showed a significant OR for alcohol misuse (OR 2.16, CI95 [1.63–2.86], Z = 5.34, p < 0.01). Heterogeneity was, again, significant (Q = 20.87, p < 0.01, I2 = 61.72%).
The studies that considered other drug use as a risk factor (k = 4) are presented now. The OR for the samples with drug use was also significant (OR 2.29, CI95 [1.33–3.93], Z = 2.99, p < 0.01). In this case, the heterogeneity was not significant (Q = 3.57, p = 0.31, I2 = 20.72%).
Lastly, the effect of trauma was significant when it came to suicide reattempt (k = 5, OR 1.58, CI95 [1.12–2.24], Z = 2.58, p < 0.01). Cochran's Q wasn't significant (Q = 3.36, p = 0.49, I2 = 0%). It should be clear that all the included studies spoke of trauma as a lifetime experience of sexual trauma.
The risk factors that did not show significant results are now discussed. Only one paper studied the relationship between non-suicidal self-injury and suicide reattempt. This precludes the use of meta-analytic techniques. The only study that provided this data was that of Mirkovic et al. (Reference Mirkovic, Cohen, Garny de la Rivière, Pellerin, Guilé, Consoli and Gerardin2020). In their sample, an OR 1.15 was obtained. The effect was not significant.
Five studies focused on the role of impulsivity. The analyses did not show a relevant role for this risk factor (OR 1.28, CI95 [0.52–3.18], Z = 0.54, p = 0.59). Cochran's Q was significant (Q = 26.52, p < 0.01, I2 = 86.69%). A sensitivity analysis was performed eliminating the study by Aydin, Algin, Poyraz, and Kalenderoglu (Reference Aydin, Algin, Poyraz and Kalenderoglu2018) as it was the only one that had an Odds Ratio less than 1. In this way, a significant effect was found (OR 1.80, CI95 [1.04, 3.11], Z = 2.09, p < 0.05). Cochran's Q was not significant (Q = 6.31, p = 0.10, I2 = 53.46%).
The forest plot corresponding to each risk factor can be seen in the supplementary materials (online Supplementary Figs S1 to S6).
Discussion
Risk factors studied in first suicide attempts are partially replicated when we talk about repeat attempts. However, non-suicidal self-injury and impulsivity do not have the same relevance in reattempt. Our meta-analysis also reveals that there are various understudied risk factors in the field of suicide reattempt, for example, non-suicidal self-injury.
This study aimed to find a robust global estimate of the effect of different suicide histories and psychological risk factors on suicide reattempts, and their individual contributions. For this, a robust methodology and a large number of studies were used (k = 34). The extensive initial search has allowed us to obtain results on a wide range of risk factors.
Previous studies showed that an index attempt acts as the key single risk factor for suicide attempt repetition. In this regard, a previous meta-analysis stressed that one in five people will engage in another suicide attempt later in life (de la Torre-Luque et al., Reference de la Torre-Luque, Pemau, Ayad-Ahmed, Borges, Fernandez-Sevillano, Garrido-Torres and Ayuso-Mateos2023). The risk factors studied here can help determine which profiles are more prone to reattempt. Our results indicate that people who present any of the studied risk factors have a double risk of suicide reattempt. The high variability between effect sizes makes it necessary to focus on which specific factors pose a greater risk. As can be seen, not all factors are equally relevant.
Starting with the factors associated with the suicide history itself, the most studied risk factor is the presence of previous attempts. It should be noted that most studies consider the inclusion of a participant after an index attempt, the index attempt is not necessarily the first one. Those who made attempts prior to the index have an increased risk of repetition. This phenomenon could be related to the acquired capacity for suicide raised in the ideation to action framework. The concept of major repeaters could also be relevant (Blasco-Fontecilla et al., Reference Blasco-Fontecilla, Jaussent, Olié, Béziat, Guillaume, Artieda-Urrutia and Courtet2014; Irigoyen-Otiñano et al., Reference Irigoyen-Otiñano, Puigdevall-Ruestes, Prades-Salvador, Salort-Seguí, Gayubo, de Leon and Blasco-Fontecilla2018). Not all studies reported the exact number of lifetime attempts.
The presence of active ideation at the time of the baseline measurement is also a relevant risk factor. From the action ideation models, the part related to ideation is considered relevant (O'Connor & Kirtley, Reference O'Connor and Kirtley2018). Maintaining ideation even after the attempt could lead to new attempts in the future. However, there is some variability in the measures used and even in the concepts measured. Some tests focus on suicidal ideation (e.g. De Beurs, Fokkema, & O'Connor, Reference De Beurs, Fokkema and O'Connor2016; O'Connor, Smyth, & Williams, Reference O'Connor, Smyth and Williams2015) and others on suicidal intent (e.g. Dieserud, Røysamb, Braverman, Dalgard, & Ekeberg, Reference Dieserud, Røysamb, Braverman, Dalgard and Ekeberg2003; Wei et al., Reference Wei, Liu, Zhang, Wang, Chu and Jia2021). It is necessary to systematize these measures to obtain more precise conclusions.
Both alcohol and drug misuse are also a relevant risk factors for suicide reattempts. A previous meta-analysis already found similar results when considering full-blown substance disorders (de la Torre-Luque et al., Reference de la Torre-Luque, Pemau, Ayad-Ahmed, Borges, Fernandez-Sevillano, Garrido-Torres and Ayuso-Mateos2023). This risk factor should not be confused with the involvement of substances during the attempt.
Finally, the presence of trauma was also a significant risk factor for suicide reattempt. It is relevant to point out that the included studies can be interpreted as physical or sexual abuse throughout life (some studies considered only childhood and others lifetime). There may be differential functioning between trauma in adult life and that which occurs during childhood (Zatti et al., Reference Zatti, Rosa, Barros, Valdivia, Calegaro, Freitas and Schuch2017). Studies in this regard seem necessary.
All the factors mentioned have presented the expected relationship. They also coincide with the investigations on first attempts. However, the levels of impulsivity and non-suicidal self-injury did not show a significant role in our study.
Beginning with non-suicidal self-injury, only one study measured the relationship between it and suicide reattempt (Mirkovic et al., Reference Mirkovic, Cohen, Garny de la Rivière, Pellerin, Guilé, Consoli and Gerardin2020). Therefore, meta-analytic analyses could not be carried out. The existing study does not find non-suicidal self-injury as a relevant risk factor. The scarce presence of this risk factor in the studies is striking.
Regarding impulsivity, no significant OR was found when the full sample of studies was used. The literature focused on the first attempts finds that it is a relevant factor (Liu, Trout, Hernandez, Cheek, & Gerlus, Reference Liu, Trout, Hernandez, Cheek and Gerlus2017). In part, these discrepancies could be due to the high conceptual variability associated with impulsivity in the field of suicide (Rimkeviciene, O׳Gorman, & De Leo, Reference Rimkeviciene, O׳Gorman and De Leo2015). In our case, we found studies that considered behavioral impulsivity compared to others that spoke of the impulsivity of the index attempt (the separate analyses were not significant either). When performing the sensitivity analysis, a relevant effect of impulsivity was found. The retrospective nature of the discarded study (Aydin et al., Reference Aydin, Algin, Poyraz and Kalenderoglu2018) could explain this discrepancy. The temporal distance between the measure of impulsivity and the attempt could explain the non-appearance of a relationship (Liu et al., Reference Liu, Trout, Hernandez, Cheek and Gerlus2017).
We can observe that there is a very high heterogeneity of terminology, methodology, and focus of study. Systematizing these aspects could help draw stronger conclusions that help guide future studies.
The study has some limitations to be mentioned. First, only published articles were consulted. Second, there could be publication bias that affected the results. Third, it was necessary to group many studies with definitions or measures of constructs that were not exactly the same (although equivalent). This could have masked some differences present, although attempts have been made to control for it using sensitivity analyses. Also, some variables were only considered in very few studies, making it difficult to draw strong conclusions. Given the variability between studies, analyses could not be carried out by taking different risk factors together. Finally, the heterogeneity between effect sizes was not completely covered by moderators in analysis. Specifically, there are relevant variables not studied in this work, such as diagnoses (for an in-depth work on this topic, consult the work of de la Torre-Luque et al., Reference de la Torre-Luque, Pemau, Ayad-Ahmed, Borges, Fernandez-Sevillano, Garrido-Torres and Ayuso-Mateos2023).
Not all people who made a first suicide attempt will reattempt. The presence of multiple previous attempts is the most relevant risk factors for suicide reattempt. There is a relevant overlap between the variables that facilitate the transition from suicidal ideation to act and those present in the reattempt. However, variables widely considered important in first suicide attempts are not so decisive when reattempting (i.e. impulsivity and non-suicidal self-injury). This study allows us to further define the risk profile for patients with several suicide attempts, which may facilitate the development of more effective interventions and preventive strategies.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724000904
Acknowledgements
The following are members of SURVIVE: Beatriz Rodriguez-Vega, Patricia Diaz-Carracedo, Veronica Fernandez-Rodrigues, Elvira Lara, Itziar Leal-Leturia, Mireia Vazquez, Irene Canoso-Garcia, Lorenzo Bracco, Pilar Saiz, Teresa Bobes-Bascaran, Diego Palao, Narcis Cardoner, Anabel Cebria, Purificacion Lopez-Peña, Lide Rementeria, Benedicto Crespo-Facorro.
Funding statement
This study was supported by the Instituto de Salud Carlos III-FIS research grants (PI16/00187, PI19/00236, PI19/00569, PI19/00685, PI19/00941, PI19/00954, PI19/01027, PI19/01256, PI19/01484, PI20/00229), co-funded by the European Regional Development Fund (ERDF) ‘A Way to Build Europe’ integrated into the Plan Nacional de I + D + I and cofinanced by the ISCIII-Subdirección General de Evaluación y confinanciado por la Unión Europea (FEDER, FSE, Next Generation EU/Plan de Recuperación Transformación y Resiliencia_PRTR); the Instituto de Salud Carlos III; the CIBER of Mental Health (CIBERSAM); and the Secretaria d'Universitats i Recerca del Departament d'Economia i Coneixement (2021 SGR 01358), CERCA Programme / Generalitat de Catalunya as well as the Fundació Clínic per la Recerca Biomèdica (Pons Bartran 2022-FRCB_PB1_2022); the Government of the Principality of Asturias (grant ref.: PCTI-2018-2022 IDI/2018/235);. It was also supported by a FPU grant (FPU20/01651) from the Spanish Ministry of Universities and a Universidad Complutense de Madrid Predoctoral contract for research staff in training (CT82/20-CT83/20).
Competing interests
IG has received grants and served as consultant, advisor, or CME speaker for the following identities: ADAMED, Angelini, CasenRecordati, Esteve, Ferrer, Gedeon Richter, Janssen Cilag, and Lundbeck, Lundbeck-Otsuka, Luye, SEI Healthcare Viatris outside the submitted work. She also receives royalties from Oxford University Press, Elsevier, Editorial Médica Panamericana. AGP has received grants from or served as a consultant, advisor, or CME speaker for the following entities: Almirall, AstraZeneca, Bristol-Myers Squibb, Cephalon, Eli Lilly, Glaxo-Smith-Kline, Janssen-Cilag, Ferrer, Johnson & Johnson, Lundbeck, Merck, Otsuka, Pfizer, Sanofi-Aventis, Servier, Shering-Plough, Solvay, the Spanish Ministries of Science and Innovation (through CIBERSAM) and of Science (through the Carlos III Institute of Health), the Basque Government, the Stanley Medical Research Institute, and Wyeth. VPS has been a consultant to or has received honoraria or grants from AB-Biotics, AstraZeneca, Bristol-Myers-Squibb, CIBERSAM, FIS- ISCIII, Janssen Cilag, Lundbeck, Otsuka, Servier, and Pfizer. The remaining authors declare that they do not have any conflict of interest to disclose.





