INTRODUCTION
The rapid and appropriate exposure of trauma patients is considered an essential component of the primary trauma survey. 1 , Reference Campbell and Alson 2 It allows early recognition and management of life-threatening injuries. 1 , Reference Campbell and Alson 2 Specifically, haemorrhage has been shown to be a major cause of potentially preventable prehospital trauma deaths.Reference Davis, Satahoo and Butler 3 Close to one-third of these potentially preventable deaths involve extremity injuries that must be rapidly identified and managed with appropriate haemorrhage control techniques.Reference Davis, Satahoo and Butler 3 Ideally, healthcare practitioners should use the most efficient technique to remove patient clothing and complete the primary survey in a timely fashion. Currently, there is no gold standard with regard to technique for clothing removal or acceptable time to trauma patient exposure. A review of the medical literature found only two studies that evaluated techniques to expose trauma patients.Reference Tang, Levy, Harrow and Bingham 4 , Reference Hurtado and Montoya 5 The authors of both of these studies examined the use of trauma shears versus a specific cutting tool designed for clothing removal. The purpose of our study is to compare two specific techniques of clothing removal versus usual practice using standard trauma shears in the management of a simulated trauma patient.
METHODS
Databases including PubMed, Embase, and CINAHL as well as major trauma, emergency medicine, and prehospital care textbooks 1 , Reference Campbell and Alson 2 , Reference Marx, Hockberger and Walls 6 , Reference Tintinalli, Stapczynski and Ma 7 , Reference Asensio and Trunkey 8 were searched for descriptions of clothing-removal techniques. All paramedicine education programs in Canada accredited by the Canadian Medical Association were surveyed to determine if a preferred method of clothing removal was taught to their students. When none of these sources revealed a preferred method, the web-based search engine Google was queried to look for anecdotal evidence of a technique preferred by experienced providers. We discovered one emergency medical services (EMS)-related blog site that promoted an unnamed technique we have since designated the “cut and rip technique” (CAR). 9 A focus group of paramedic instructors at Holland College found this technique to be quick and easy to perform. It was selected as our primary experimental intervention.
Convenience samples of both advanced care paramedic (ACP) students at Holland College (Prince Edward Island) as well as practicing paramedics in PEI were recruited to participate. The Holland College research ethics board approved the study, and informed written consent was obtained. All ACP student participants had previously obtained a diploma in primary care paramedicine (PCP). During their PCP program, students received training on basic assessment, care, and transport of trauma patients. The online learning management program Angel Learning Management Suite (v. 7.4, Blackboard Inc., Washington, DC) “Random Team Generator” function was used to allocate ACP students to either the “cut alone technique” (CAL) or the CAR technique. None of the study investigators participated in the randomization or evaluation of participants. The CAR technique (Figure 1) involves using standard trauma shears to make a starting cut through the thicker cuffed ends of clothing, followed by the use of hands to tear the length of the clothing. Care is taken to stay medial of the pockets when ripping the pants. The CAL technique (Figure 1) involves using standard trauma shears in the usual cutting fashion across the entire length of clothing. Students in each group were given a separate 15-minute didactic presentation on how to perform their respective technique, followed by a live demonstration on a mannequin. Participants were then given an opportunity to perform a practice cut on a single article of clothing.
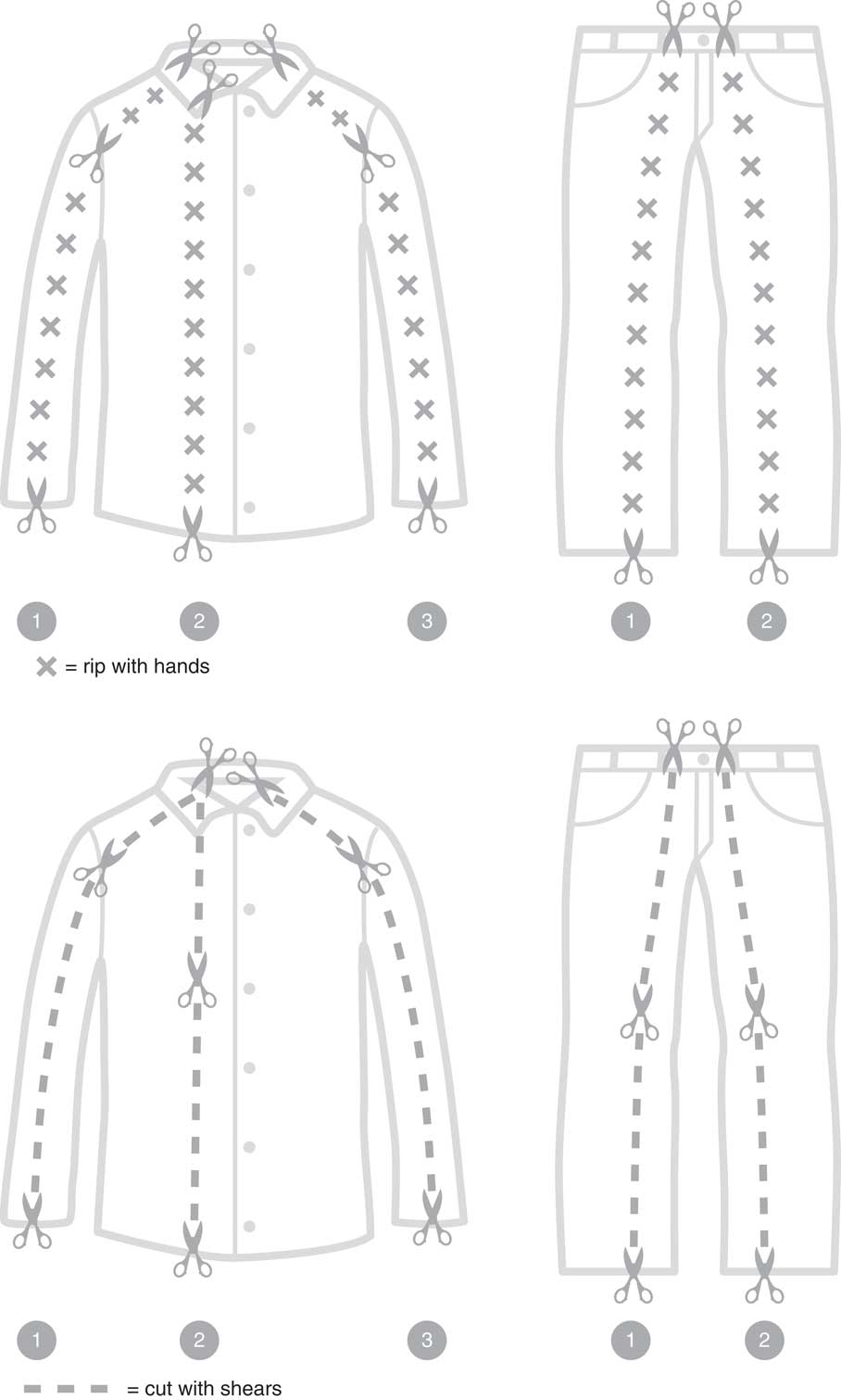
Figure 1 Clothing removal techniques.
Practicing paramedics (both PCPs and ACPs) were recruited for the usual practice (UP) group. These paramedics were asked to remove the simulated patient’s clothing using standard trauma shears and whatever technique they normally would employ when treating a real trauma patient. They received instruction regarding study protocol and were offered a practice cut on a single article of clothing.
For each attempt, an identical full-body adult mannequin (Laerdal MegaCode Kelly) was placed on a standard ambulance stretcher (Ferno Proflex, Megacode, Laerdal Medical Canada Ltd., Toronto, ON). The bottom half of the mannequin was fitted with an identical brand, size, and style of denim/blue jeans (waist size 32 inches and inseam 30 inches). The top half was fitted with evenly distributed medium or large cotton T-shirts, and on top of this a medium or large long-sleeve cotton/polyester button-up shirt (Figure 2). Care was taken to ensure that clothing was similar in style and type and thickness of material. Brand-new identical trauma shears were used for each group (a maximum of eight times for each pair). Trained independent evaluators timed participants using identical timing devices. Timing started from the moment the trauma shears touched the patient’s clothing. Pieces of clothing were sequentially removed from the upper body followed by the lower body so as to follow a standard trauma ABCD approach without obvious external bleeding or injury. Timing ended when the anterior portion of the simulated patient was completely exposed, a log roll was performed to expose the back, and the patient was placed flat on the stretcher again. Times for complete patient exposure plus times for removal of individual articles of clothing were recorded. Following a participant’s attempt, they were asked to fill out a brief survey to collect demographic information, including gender, age, years of practice, and level of certification obtained (PCP or ACP), as well as prior completion of a basic trauma life support course (or equivalent).

Figure 2 Dressed mannequin.
Statistics
For the primary outcome measure of time to complete patient exposure, we performed a power calculation assuming a clinically significant difference of 30 seconds (SD 7.5) between cutting techniques. We estimated that a total of 24 participants (8 in each group) would provide 92% power to detect half the clinically significant difference. The clinically significant difference was determined by a focus group of 10 experts in emergency medical services across Canada. Participants were evaluated using a per-protocol analysis. Unadjusted analyses using a one-way ANOVA were performed to look for a difference among techniques with regard to total time to patient exposure as well as differences in time to remove a specific item of clothing. Further differences between specific groups in both total time-to-exposure as well as individual pieces of clothing were determined post hoc using Tukey’s pairwise comparisons. All analyses were conducted using Minitab 17 (Minitab Inc., State College, PA).
RESULTS
A total of 24 participants (8 per group) were recruited to participate (see Table 1). One participant (CAL group) was not analyzed due to a violation of the per-protocol analysis. A single participant (UP group) removed the clothing piecemeal, allowing only the total time to removal to be recorded. The student groups (CAR, CAL) were similar in mean age (29, 27), years of practice (1 student >5 years), and male gender (63, 43%). The UP group was older (mean 34), more experienced (63% practice >5 years), and had a higher level of training (63% ACP) but had a similar percentage of males (63%). Clothing removal times are listed in Table 2.
Table 1 Demographics
Table 2 Mean times to remove clothing
* One missing data point.
For the primary outcome measure of time to complete patient exposure, the CAR group outperformed the CAL group by a mean difference of 32 seconds (mean 104 seconds, 95% CI 88–120 vs. 136 seconds, 95% CI 119–154, p=0.02). There was no difference in time to complete patient exposure between either the CAR or CAL groups and the UP group (mean 124 seconds, 95% CI 108–140, p≥0.05). For the secondary outcome of time to removal of individual categories of clothing, CAR was faster than CAL for removal of pants (mean 35 seconds, 95% CI 27–43 vs. mean 54 seconds, 95% CI 46–63, p=0.006). There were no other differences between the three groups. Clothing removal times are listed in Table 2.
DISCUSSION
This study demonstrates that the CAR cutting technique is faster and could save time when assessing a critically ill trauma patient. Although it could be argued that this reduction in delay to exposure may not be clinically relevant for many patients and that full clothing removal is often unnecessary, intuitively it makes sense that rapid patient exposure might reduce time to discovery of life-threatening injury. In the case of a mass-casualty incident, where large numbers of patients must be rapidly assessed and managed, the incremental effect of even brief delays could potentially be catastrophic for some patients. Early intervention may subsequently improve patient outcomes. Standard trauma and critical care teaching emphasizes the importance of early control of external haemorrhage, quick decompression of a tension pneumothorax, and discovery of external signs of potential internal injury (e.g., seatbelt sign). In particular, the use of tourniquets to control extremity haemorrhage has significantly reduced mortality in military settings and been shown to be safe and appropriate in civilian prehospital care.Reference Eastridge, Mabry and Seguin 10 , Reference Scerbo, Mumm and Gates 11 Further, there are other non-trauma scenarios where rapid patient exposure is presumably of benefit, including cardiac arrest, where rapid exposure of the chest may allow earlier defibrillation. Clinical outcomes in cardiac arrest have been shown to be worse with each additional minute of delay to defibrillation.Reference Chan, Krumholz, Nichol and Nallamothu 12
Tang et al.Reference Tang, Levy, Harrow and Bingham 4 compared the use of standard trauma scissors/shears versus a hooked cutting device to remove clothing from a standard mannequin. Our times for removal of a long-sleeve buttoned shirt and pants in both the CAR and CAL groups were much faster than their scissor/shears group. Participants from our CAL group were able to individually remove the long-sleeve buttoned shirt and pants on average 42 and 15 seconds faster. Further, their results showed that participants were able to remove the pants faster than the shirt using scissors/shears, which was the opposite of our CAL group. It is possible that differences in clothing size or material or our standardization of cutting technique in the CAL group created these differences. As our simulated patients were completely exposed, we do not believe that the degree of exposure can explain our faster time. The hooked cutting device was 10 and 16 seconds faster than our CAR technique for both the removal of the shirt and pants respectively. Tang et al.Reference Tang, Levy, Harrow and Bingham 4 state that the timing of clothing removal began as soon as the device touched the clothing and ended when the mannequin was fully exposed, just as in our study. This overall time difference of 26 seconds is less than our selected clinically relevant difference of 30 seconds. The identical participants in the Tang study were used to perform clothing removal in both the experimental and control groups. This potentially adds some bias that could favour the performance of the hooked cutting devices. The disadvantages of hooked cutting devices include their considerable expense compared to standard trauma shears and the requirement for sharpening at regular intervals.
We eliminated one individual from analysis due to a protocol violation. This individual performed what we describe as the “razor” technique, which involves running an open pair of shears up the material without moving the blades to cut. While this is a very effective method, it does not seem to work well with dull shears. Since we wanted to find a technique that would perform well with any pair of shears, regardless of age, we chose not to evaluate this technique. Inclusion of the individual in the final analysis removes the statistically significant difference (p=0.07, ANOVA) and decreases the mean time to clothing removal in the CAL group by 5 seconds (mean 131, 95% CI 114–148). Other techniques of clothing removal have been anecdotally described by practicing paramedics. For instance, the “undertaker” technique involves removal of a jacket by making a single cut line up the back of the jacket and then pulling the arms of the jacket anteriorly to remove it in one piece (similar to how an undertaker might place a jacket on a corpse, but in reverse fashion). Some paramedics bunch the neck and bottom of a T-shirt in one hand to make a single cut along the front. Interestingly, we found that the UP group of experienced paramedics used a combination of techniques including both the CAL and CAR techniques. A number of practicing paramedics also ripped the buttons of the long-sleeve shirt to save time. We specifically asked the CAR and CAL groups to not do this.
Unexpectedly, one participant in the CAR group had a total time that was greater than 6 of 7 individuals in the CAL group and 34 seconds longer than any other person in their own group. The evaluator noted that this individual struggled with hand coordination in performing the rips. Although recursive partitioning failed to demonstrate that this individual was a statistical outlier, we feel that this is a clinical outlier. When this individual is removed from the analysis, the average time for the CAR technique decreases by 7 seconds to 97 seconds and the difference between the CAR and UP group becomes statistically significant (p=0.003, 95% CI 82–112).
Unfortunately, the CAR technique may not work with all materials. We successfully tested the technique on a number of other materials, including fleece, a cotton knit sweater, and a cotton sweatshirt. The technique was not tested on leather or other thicker materials where its effectiveness may be lost.
LIMITATIONS
There are a number of limitations present in this study. The total number of participants was low; however, we exceeded the minimum sample size derived by a power calculation. Although the paramedic students had an opportunity to practice the CAR technique once, the evaluators found that some participants struggled with hand coordination. With further practice, their technique may have improved and thus the overall benefit of the technique is potentially underestimated. It is also possible that practicing paramedics with more experience would have been able to perform the CAR technique more efficiently. Used items of clothing were employed to dress the mannequins. Unfortunately, there were slight differences in the material between the shirts, and it is possible that some shirts were easier to cut than others. We did ensure that shirts were evenly distributed by size among groups and believe that any subtle differences in materials would only make our time to remove the clothing more realistic. Simulated models also have important differences that limit comparisons to real-life patient care. Real patients vary in physical characteristics, body movement, express preferences, and experience pain and emotional distress. Further, the presence of body fluids, hazards including glass and other debris, and immobilization techniques may limit the effectiveness of any clothing-removal technique. Finally, the use of a crossover design may have provided certain advantages to this study. By using individual participants as their own control, the influence of confounding variables may have been reduced and additional comparisons would have been created using the same number of participants. However, using this design in the UP group may have inadvertently biased participants toward a specific technique over their usual practice.
CONCLUSIONS
In conclusion, the CAR technique was the fastest and was significantly faster than the CAL method to remove clothing from a standard trauma mannequin. Practitioners should consider using the CAR method to remove clothing from a critically ill patient. Future studies should compare the CAR technique with specific cutting tools.
Acknowledgments
AS contributed to development of study concept and design, data collection and analysis, critical revision, and approval of submission. TJ and BN contributed to study design, data collection, critical revision, and approval of submission. PA contributed to study design, analysis of data, critical revision, and approval of submission. The authors would like to thank Henrik Stryhn, PhD, for his statistical support in both study design and data analysis, and the Holland College Department of Applied Research for funding to purchase used clothing.
Competing interests: None to declare.






