Germany has an estimated 150 000 people with opioid dependence, mainly heroin dependence, among a population of 80 million (Reference Bühringer, Adelsberger and HeinemannBühringer et al, 1997). Less than half (50 000–60 000) at any given time are on opioid maintenance treatment. None the less, the mortality rate only decreased slightly after the widespread introduction of maintenance treatment in the early 1990s (Reference Raschke, Püschel and HeinemannRaschke et al, 2000), which is in accordance with other long-term follow-up studies (Reference Rathod, Addenbrooke and RosenbachRathod et al, 2005). This opened the discussion for modification of maintenance treatment, especially for people who either dropped out or who continued treatment but also illicit opioid use.
A large (n=1969) cohort study was initiated in Switzerland in 1994, and ascertained the feasibility, safety and potential efficacy of offering injectable heroin to people with dependence who were not responding sufficiently to maintenance treatment (Reference Rehm, Gschwend and SteffenRehm et al, 2001). The study showed a high retention rate (70% after 12 months) as well as positive effects with respect to illegal drug use, physical and mental health and social outcomes. However, assessment of the Swiss trial by the World Health Organization was unable to determine if the positive effects were a result of the prescription of heroin, the extensive psychosocial counselling and care, or the combination of both (Reference Ali, Auriacombe and CasasAli et al, 1999). A small randomised controlled trial (n=51) comparing injectable heroin with a standard treatment (mainly methadone maintenance) showed significantly better functioning in those receiving heroin after 6 months (Reference Perneger, Giner and del RioPerneger et al, 1998). However, those people also received additional, mandatory psychosocial care, which may have influenced the results.
In 1998 two randomised controlled trials in The Netherlands assessed the effectiveness of the co-prescription of inhalable (n=375) and injectable (n=174) heroin in people with opioid dependence and chronic resistance to methadone treatment. Results showed that heroin-assisted treatment was feasible, more effective and probably as safe as methadone alone in reducing physical, mental and social problems (Reference van den Brink, Hendriks and Blankenvan den Brink et al, 2003; Reference Blanken, Hendriks and KoeterBlanken et al, 2005). Co-prescription of heroin was cost-effective compared with methadone treatment alone (Reference Dijkgraaf, van der Zanden and de BorgieDijkgraaf et al, 2005). A limitation of these trials was that psychosocial treatments were not standardised and were uncontrolled. Furthermore, the larger of the two trials used inhalable heroin, which is used by the majority (75–90%) of street heroin users in The Netherlands, but not in Germany.
A recent Cochrane review (Reference Ferri, Davoli and PerucciFerri et al, 2005) found that the Swiss and Dutch studies do not allow a definite conclusion to be drawn about the overall effectiveness of heroin prescription because of a lack of comparability. We therefore examined the effectiveness of medically prescribed and supervised heroin injection in an open-label randomised controlled trial in two groups of people with heroin dependence: those not responding sufficiently to methadone maintenance treatment and those currently not in substance misuse treatment. To control for the impact of psychosocial treatment, participants in each group were randomised to one of two types of psychosocial care.
METHOD
Study design
After screening more than 2000 people with heroin dependence, a total of 1032 consenting participants were randomised between March 2002 and December 2003 in seven treatment centres (Hamburg, 401 participants; Frankfurt, 191; Hanover, 132; Bonn, 100; Cologne, 100; Munich, 60; Karlsruhe, 48). Participants were from two target groups: (a) people with heroin dependence who were insufficiently responding to treatment owing to continuous intravenous heroin use (n=492); and (b) people with heroin dependence who were not in treatment in the previous 6 months (n=540). Participants from each target group were randomised into four subgroups according to the type of medication and the type of psychosocial care (Fig. 1), resulting in a 2×2×2 design and eight separate groups. Of the 811 people lost between screening and baseline, 106 (13.1%) did not meet inclusion criteria and the others did not attend for examination. Of the 240 people lost between baseline and randomisation, 1 died (0.4%), 14 (5.8%) were rejected by the expert panels for not meeting study inclusion criteria and the rest did not complete the baseline examination or attend for randomisation. Seventeen patients, 5 previously on methadone and 12 not in treatment, were excluded from analysis because they withdrew their consent after randomisation without initiating study treatment (n=8), because they did not have an independent baseline interview prior to randomisation (n=8), or both (n=1), leaving 1015 patients in the intent-to-treat analysis (n=487 treatment failure, n=528 not in treatment).

Fig. 1 CONSORT diagram. ITT, intent-to-treat.
After giving consent, participants were given an extensive baseline examination. Inclusion criteria were then presented to a local independent expert committee before a final decision for inclusion was made. Then a second consent was necessary before randomisation. Randomisation took place separately for each target group (methadone treatment failure and not in treatment), and treatment allocation was performed using sealed and consecutively numbered envelopes at each study site.
Treatment duration was 12 months. Treatment in the intervention group consisted of an individually adjusted dose of injectable heroin that was self-administered in an out-patient setting under direct supervision of medical staff, maximally three times a day, 7 days a week, with a maximum single dose of 400 mg and a maximum daily dose of 1000 mg (none to take home). Up to 60 mg of methadone could also be given for take-home night-time use to suppress withdrawal. Treatment in the control group consisted of a minimum daily dose of 60 mg methadone, which could be individually adjusted according to clinical judgement. Participants within both groups were randomised to either group psychoeducation plus individual counselling according to Farnbacher et al (Reference Farnbacher, Basdekis-Josza, Krausz, Böllinger and Stöver2002), or case management and motivational interviewing according to Oliva et al (Reference Oliva, Görgen and Schlanstedt2001). Each of these interventions has been described in manuals, and training of all therapists was conducted prior to the study to minimise site differences. The type of psychosocial care was similar with respect to average intensity of contact, but there was more individual flexibility in the case management group than with the more standardised psychosocial care in the psychoeducation group.
Study population
Inclusion criteria were 23 years old or greater and an ICD–10 diagnosis of opioid dependence of at least 5 years' duration (World Health Organization, 1993). Furthermore, eligibility criteria for the group with methadone treatment failure included continued intravenous use of street heroin (confirmed by urine testing) despite ongoing maintenance treatment of at least 6 months, whereas for the not in treatment group they included regular intravenous use of street heroin (confirmed by urine testing) and confirmed participation in previous drug treatment. Participants needed to have poor physical and/or mental health, with at least 13 symptoms on the Opiate Treatment Index (OTI) Health Scale (Darke et al, Reference Darke, Ward and Zador1991, Reference Darke, Hall and Wodak1992) and/or at least 60 points (standardised T-score) on the Global Severity Index of the Symptom Check-List (SCL–90–R; Reference DerogatisDerogatis, 1983).
People with a pending jail sentence, those who had been abstinent for 2 or more months in the past 12 months and those with a severe physical disorder such as renal or hepatic failure, clinically significant cardiac arrhythmias or chronic obstructive pulmonary disease were excluded, as were pregnant or breast-feeding women.
Assessments and statistical analyses
Baseline assessments were completed by study physicians and independent research assistants before a decision was made on randomisation. Potential study inclusion was based on physician assessment only but had to be confirmed by an independent panel of experts after baseline assessment, which delayed initiation of treatment for an average of 31 days. Study physicians re-assessed people who were approved for randomisation at initiation of treatment, and at 1, 3, 6 and 12 months. Independent assessment by research assistants was performed at 6 and 12 months.
Assessment by the study physician included application of the OTI and SCL–90–R, the composite international diagnostic interview (CIDI; World Health Organization, 1990), and the severity of withdrawal scale (SOWS; Reference GossopGossop, 1990), and a comprehensive physical examination, including electrocardiography, laboratory examinations, echocardiography, abdominal ultrasonography, urine and hair analyses, as well as all serious adverse events. All serious adverse events, defined according to guidelines E2A and E6 of the International Conference on Harmonisation of Technical Registration for Recognition of Pharmaceuticals for Human Use (ICH; http://www.ich.org) were reported to a safety board, which consisted of three independent clinicians, who evaluated all adverse events with respect to safety of the study treatment. The assessment by independent research assistants included administration of the European version of the Addiction Severity Index (EuropASI; Reference Kokkevi and HartgersKokkevi & Hartgers, 1995), and gathering data on criminal behaviour and on subjective aspects of treatment.
In the intent-to-treat analysis, all those randomised were assessed regardless of treatment retention. Data from the baseline and 12-month assessments were used for analysis of the primary outcome measures; the last-observation-carried-forward (LOCF) procedure from data at 6 months was used if data at 12 months were missing. If no data were available for 6 and 12 months, the outcome was coded according to a worst-case analysis (i.e. as a responder in the methadone group and a non-responder in the heroin group).
Two prespecified dichotomous, multidomain primary outcome measures were used. For the primary outcome measure on health, participants were considered responders if they showed at least a 20% improvement and at least 4 points on the OTI Health Scale (physical health) and/or at least a 20% improvement in the GSI (mental health), without a deterioration of more than 20% in the other area of health. For the second primary outcome measure, people were considered responders if they showed a reduction in the use of street heroin with at least 3 of 5 urine samples negative for the drug in the month prior to the 12-month assessment and no increase in cocaine use (hair analysis). If less than 3 urine samples or no hair was available at 12 months, data from urine or hair testing at 6 months were used (LOCF). If these were also not available, data were replaced by self-reported data from the EuropASI. When self-reported data were used, response was defined as a 60% decrease in the number of days with street heroin use and no more than 2 days' increase in cocaine use during the past month. To distinguish between prescribed and illicit heroin, urine samples were tested for papaverine and acetylcodeine, which are common impurities found in street heroin (Reference Paterson, Lintzeris and MitchellPaterson et al, 2005; Reference Rook, Huitema and van den BrinkRook et al, 2006).
A four-factorial logistic regression model was used to assess the effectiveness of heroin-assisted treatment compared with methadone, controlling for the effect of the target group (methadone treatment failure v. not in treatment), the psychosocial intervention (psychoeducation v. case management) and study site (likelihood ratio test). Using a test on interaction between primary outcome and target group (methadone treatment failure or not in treatment), we assessed whether the effect of pharmacological treatment was independent of the target group. The hypothesis would be confirmed if the logistic regression model showed superiority of heroin over methadone for both primary outcome measures (‘health' and ‘illegal drug use’) at the 5% significance level. Statistical analyses were performed using SPSS versions 10 and 11 for Windows.
Calculations of sample size were based on an estimated response rate of 30% in the methadone group and 50% in the heroin group for each primary outcome measure. Based on a one-tailed significance criterion of 0.025 (α) and a β of 0.90 for each primary outcome measure, the total power remained 80% (0.9*0.9) for the study to yield a statistically significant result. Assuming that 10% of the methadone group and 5% of the heroin group would not be reached for assessment at 6 or 12 months, and therefore according to the worst case definition would be considered responders and non-responders respectively, the reduced effect size led to a minimum sample size of 482 for each treatment group (heroin v. methadone).
RESULTS
Sample characteristics
Table 1 shows baseline characteristics of the participants included in the intent-to-treat analysis. Both target groups had severe drug use, health problems and social problems. The group not in treatment had a more severe pattern of drug use and more problems with housing than those with past methadone treatment failure. Of the 487 in the treatment failure group, 387 were previously being treated with methadone (mean dose 90.6 mg/day), 64 with levomethadone (mean dose 56.4 mg/day), 33 with buprenorphine (mean dose 10.7 mg/day), and 3 with dihydrocodeine (mean dose 2080.0 mg/day).
Table 1 Baseline characteristics of 1015 people with heroin dependence who participated in the study

| Methadone treatment failure | Not in treatment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Heroin | Methadone | Total | Heroin | Methadone | Total | |||||
| Male gender, % | 78.5 | 77.2 | 77.8 | 81.4 | 82.2 | 81.8 | ||||
| Age, years: mean (s.d.) | 36.7 (6.5) | 37.1 (6.7) | 36.9 (6.6) | 35.7 (6.8) | 36.0 (6.8) | 35.9 (6.8) * | ||||
| Stable housing, % | 74.8 | 75.5 | 75.2 | 63.7 | 64.2 | 63.9 * | ||||
| Employed, % | 6.1 | 3.7 | 4.9 | 4.1 | 3.9 | 4.0 * | ||||
| Regular drug use, years: mean (s.d.) | ||||||||||
| Heroin | 14.2 (6.2) | 14.4 (6.3) | 14.3 (6.3) | 13.1 (6.4) | 12.8 (6.2) | 13.0 (6.3) * | ||||
| Cocaine | 6.1 (6.9) | 5.9 (6.4) | 6.0 (6.7) | 5.0 (6.4) | 5.3 (6.2) | 5.1 (6.3) * | ||||
| Benzodiazepines | 6.2 (7.8) | 7.3 (7.8) | 6.7 (7.8) | 4.0 (6.0) | 3.8 (6.1) | 3.9 (6.0) * | ||||
| Drug use in past month, days: mean (s.d.) | ||||||||||
| Heroin | 17.1 (10.8) | 17.6 (10.5) | 17.4 (10.7) | 26.8 (6.5) | 26.2 (7.4) | 26.5 (6.9) * | ||||
| Cocaine | 14.7 (11.0) | 14.1 (10.8) | 14.4 (10.9) | 14.7 (11.4) | 16.3 (11.7) | 15.5 (11.5) | ||||
| Benzodiazepines | 18.7 (11.2) | 18.4 (11.5) | 18.6 (11.3) | 13.3 (11.3) | 14.2 (11.4) | 13.8 (11.3) * | ||||
| Intravenous drug use | 19.7 (10.7) | 20.3 (10.5) | 20.0 (10.6) | 26.6 (7.2) | 26.3 (7.5) | 26.5 (7.4) * | ||||
| Alcohol use in past month, days: mean (s.d.) | 10.9 (11.3) | 13.6 (12.2) | 11.9 (11.7) | 12.9 (11.5) | 14.0 (13.1) | 13.4 (12.3) | ||||
| Previous detoxification treatment, % | 88.1 | 90.4 | 89.2 | 82.3 | 80.6 | 81.4 * | ||||
| Previous drug-free treatment, % | 62.6 | 61.1 | 61.8 | 54.6 | 53.0 | 53.8 * | ||||
| Previous maintenance treatment, % | 100.0 | 99.6 2 | 99.8 | 77.8 | 81.5 | 79.6 * | ||||
| Physical health score, mean (s.d.) | ||||||||||
| OTI Health Scale score, mean (s.d.) | 18.8 (5.1) | 18.9 (5.5) | 18.9 (5.3) | 18.7 (5.3) | 19.3 (5.3) | 19.0 (5.3) | ||||
| Body mass index | 23.0 (3.8) | 22.9 (3.8) | 22.9 (3.8) | 22.5 (3.2) | 22.2 (3.1) | 22.4 (3.2) * | ||||
| HIV positive, % | 11.8 | 10.9 | 11.4 | 5.7 | 8.1 | 6.9 | ||||
| HCV positive, % | 82.8 | 85.4 | 84.1 | 78.5 | 78.6 | 78.5 | ||||
| Mental health | ||||||||||
| GSI standardised T-score: mean (s.d.) | 69.5 (11.0) | 69.7 (9.8) | 69.6 (10.4) | 68.4 (10.9) | 69.5 (10.5) | 68.9 (10.7) | ||||
| Previous suicide attempts, % | 45.8 | 43.5 | 44.6 | 37.4 | 42.2 | 39.7 | ||||
| At least one lifetime psychiatric diagnosis, % 1 | 62.1 | 60.8 | 61.7 | 57.9 | 62.0 | 59.3 | ||||
| Social functioning score | ||||||||||
| GAFS: mean (s.d.) | 53.3 (10.5) | 52.5 (11.9) | 52.9 (11.2) | 54.2 (12.1) | 54.3 (11.5) | 54.2 (11.8) | ||||
| Illegal activities past month, days, mean (s.d.) | 18.8 (11.0) | 18.8 (10.5) | 18.8 (10.7) | 23.3 (9.5) | 22.0 (10.0) | 22.6 (9.8) * | ||||
| Ever convicted, % | 97.1 | 96.2 | 96.6 | 96.6 | 95.3 | 95.9 | ||||
| Ever incarcerated, % | 74.2 | 76.0 | 75.1 | 73.7 | 74.3 | 74.0 | ||||
OTI, Opiate Treatment Index; HCV, hepatitis C virus; GSI, Global Severity Index; GAFS, Global Assessment of Functioning Scale
* P <0.05 methadone treatment failure v. not in treatment
1. ICD–10 diagnosis of schizophrenic (F2), affective (F3), neurotic (F4) or behavioural (F5) disorder
2. One participant did not meet criteria for 6-month maintenance treatment in independent assessment
Availability of outcome data
Follow-up data were available at 12 months for 956 of the 1015 participants (95.1% of the heroin group and 93.2% of the methadone group). Health data were available for 970 patients (497 from the heroin group and 473 from the methadone group, including LOCF and death cases), leaving 45 instances where missing response data had to be replaced according to the worst case strategy. Data on illicit drug use were available for 982 participants (504 from the heroin group and 478 from the methadone group, including LOCF and death cases), leaving 33 instances where missing response data had to be replaced according to the worst case strategy.
Treatment retention
Treatment retention was higher in the heroin group, with 67.2% completing 12-month treatment compared with 40.0% in the methadone group. However, 28.8% of the methadone group did not even initiate study treatment (in contrast to 2.3% of the heroin group). Of those initiating treatment, 68.3% of the heroin group and 56.3% of the methadone group completed study treatment; 11.8% of the heroin group and 24.8% of the methadone group started with an abstinence-based or maintenance treatment after dropping out of the study treatment. The average number of treatment days was 290 days in the heroin group and 195 days in the methadone group. The mean daily dose of heroin was 442 mg with an additional 8 mg of methadone (mean daily dose over all heroin treatment days) – additional methadone was only necessary on 20.6% of heroin treatment days. In the methadone group the mean daily dose was 99 mg methadone.
Treatment effectiveness
In the intent-to-treat analysis, the heroin treatment group showed a significantly greater response than the methadone treatment group with respect to both primary outcome measures (Table 2).
Table 2 Effectiveness of heroin v. methadone treatment for two primary outcome measures
| Heroin | Methadone | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | OR | 95% CI | P | |||
| Intent-to-treat analysis | |||||||||
| Improvement in ‘health’ | 412 | 80.0 | 370 | 74.0 | 1.41 | 1.05–1.89 | 0.023 1 | ||
| Reduction in illegal drug use | 356 | 69.1 | 276 | 55.2 | 1.85 | 1.43–2.40 | <0.001 2 | ||
| Total | 515 | 100.0 | 500 | 100.0 | |||||
| Per-protocol completers analysis | |||||||||
| Improvement in health | 301 | 87.0 | 154 | 77.0 | 2.05 | 1.28–3.27 | 0.003 | ||
| Reduction in illegal drug use | 253 | 73.1 | 103 | 51.5 | 2.64 | 1.80–3.88 | <0.001 | ||
| Total | 346 | 67.2 | 200 | 40.0 | |||||
OR, odds ratio
1. Hosmer and Lemeshow goodness of fit: χ2=2.23, d.f.=8, P=0.973
2. Hosmer and Lemeshow goodness of fit: χ2=11.06, d.f.=8, P=0.198
With respect to the primary outcome measure ‘health’, logistic regression analysis showed no effect of target group (methadone treatment failure v. not in treatment; P=0.320), study centre (P=0.143) and type of psychosocial intervention (psychoeducation v. case management; P=0.269). In addition, no interaction was found between medication group and target group (P=0.544). After adjustment for target group, study centre and type of psychosocial care, the main effect of medication group on the primary outcome measure ‘health’ remained significant (OR=1.54, 95% CI 1.02–2.34, P=0.042).
With respect to the primary outcome measure ‘illicit drug use’, a significant effect of study centre was found (P=0.002), indicating that response rates were not homogenous across centres. Target group (P=0.228) and type of psychosocial care (P=0.369) showed no significant effect. Furthermore, no interaction was found between medication effect and target group (P=0.840). After adjustment for target group, study centre and type of psychosocial care, the main effect of medication group on the primary outcome measure ‘illicit drug use’ remained significant (OR=1.91, 95% CI 1.30–2.79, P=0.001).
Of the 1015 patients included in the intent-to-treat analysis, 546 (346 in the heroin group and 200 in the methadone group) completed the study as defined per protocol. In those 546 participants the response rates were slightly higher than in the intent-to-treat analysis, but the heroin group also showed a significantly greater response than the methadone group (Table 2).
Using a more conservative analysis strategy that defined responders as only those patients responding on both primary outcome measures, the intent-to-treat analysis showed a significantly greater response rate in the heroin compared with the methadone group (57.3% v. 44.8% OR=1.67, 95% CI 1.30–2.14, P<0.001). Using this strategy analysis of the 546 participants completing the study also showed a significantly better response rate for the heroin than the methadone group (63.6 v. 39.5%, OR=2.73, 95% CI 1.88–3.97, P<0.001).
Physical health (OTI Health Scale) showed a significant improvement in both groups, with the greatest improvement observed during the time while preparing for initiation of treatment and the first month of treatment (Fig. 2). The assessment of illicit drug use (according to self-reported data) showed a marked reduction of street heroin use in both groups, but a more pronounced reduction in the heroin group, and a moderate reduction of cocaine use in both groups (Fig. 3). Urine testing at 6 and 12 months for street heroin, as well as weekly urine testing for cocaine, confirms the self-reported data (Fig. 4). Hair analysis for cocaine use confirmed results of urine testing and self-reported data, showing an overall decrease in cocaine use, but especially a decrease in intensive use (from 29.5 to 17.2% of samples in the heroin group and 31.6 to 22.4% in the methadone group).
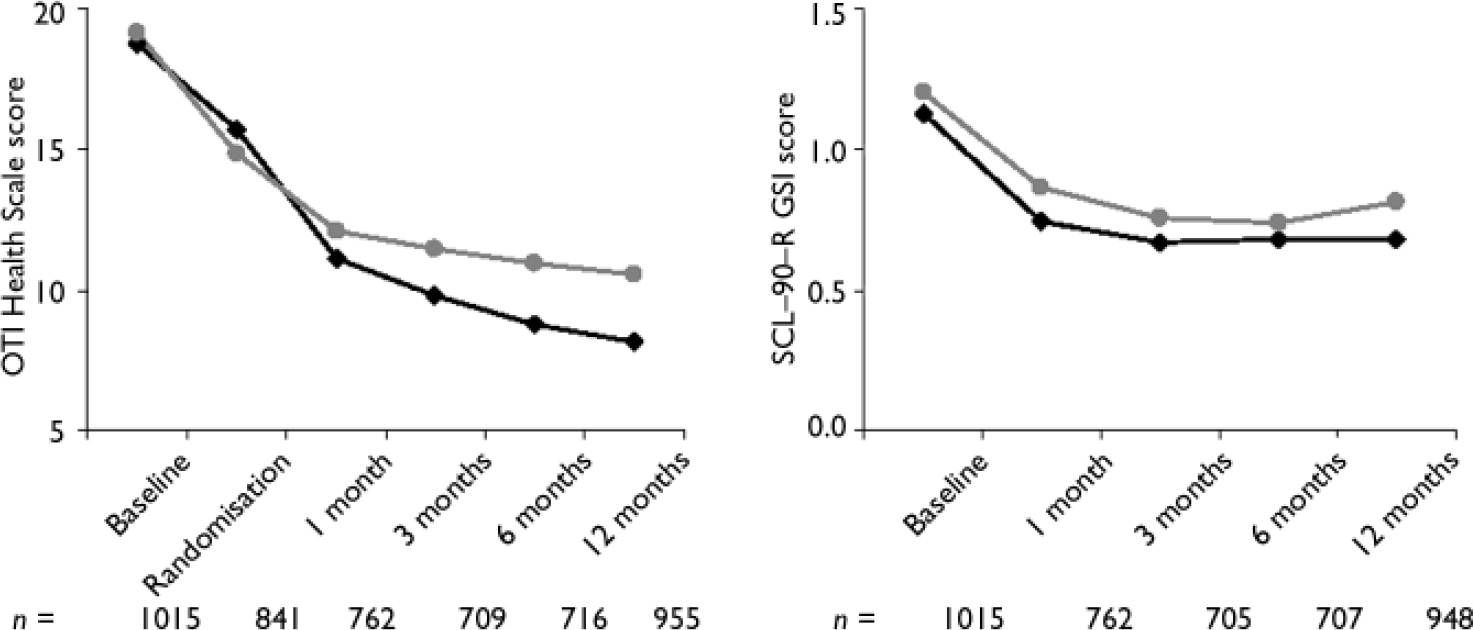
Fig. 2 Assessment of health according to the Opiate Treatment Index (OTI) Health Scale and Global Severity Index (GSI) of the Symptom Check-List (SCL-90-R) during the study period; —♦—, heroin; ![]() , methadone. The SCL-90-R was not administered at randomisation to avoid overlap artefacts, since the SCL-90-R measures symptoms occurring in the past 7 days.
, methadone. The SCL-90-R was not administered at randomisation to avoid overlap artefacts, since the SCL-90-R measures symptoms occurring in the past 7 days.
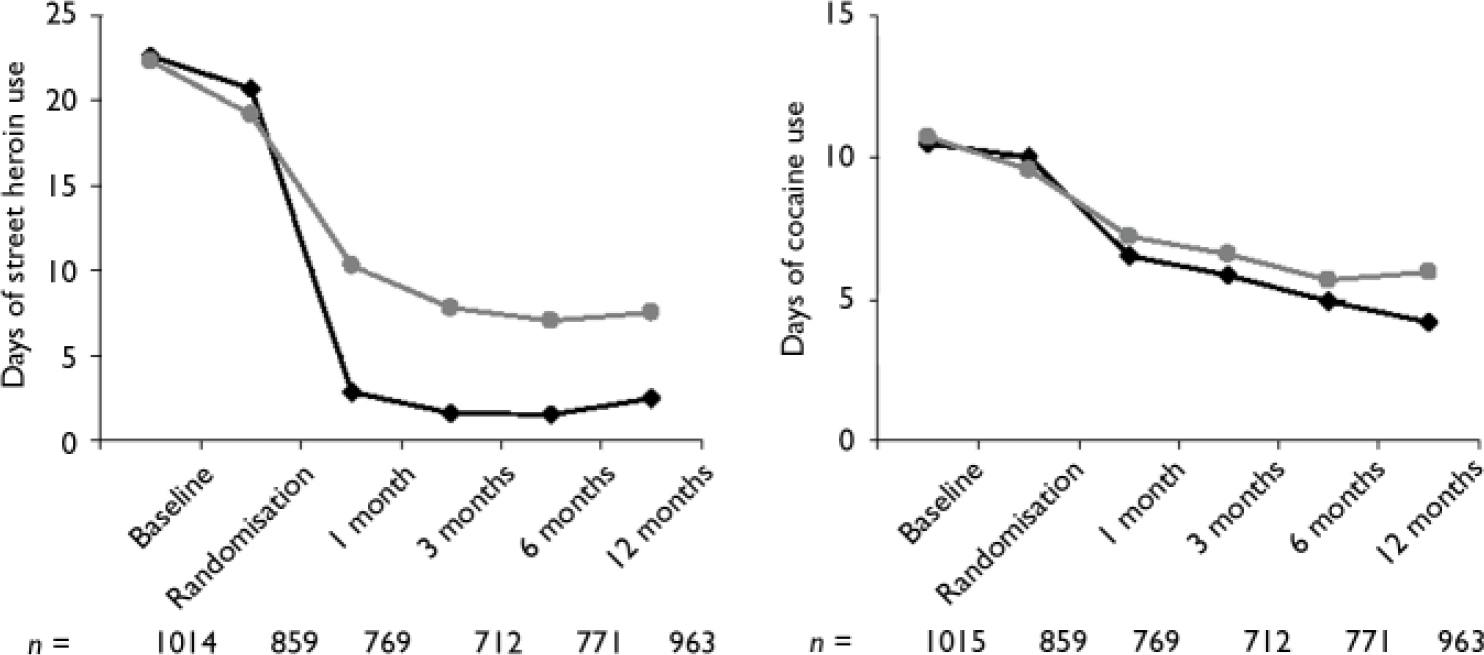
Fig. 3 Change in street heroin and cocaine use in the past 30 days (self-reported data); —♦—, heroin; ![]() , methadone; self-reported data were collected by the attending physician, whenever possible missing values were completed with data from independent interviews.
, methadone; self-reported data were collected by the attending physician, whenever possible missing values were completed with data from independent interviews.
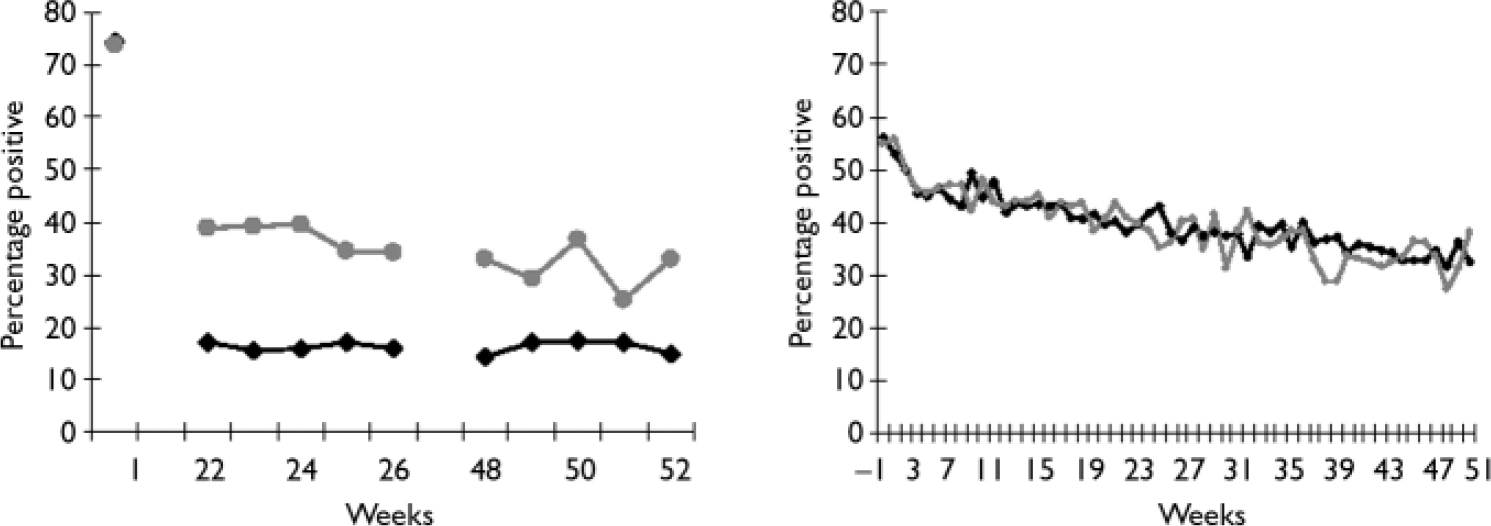
Fig. 4 Testing of urine samples for street heroin (left) and cocaine (right) during the study period; —♦—, heroin; ![]() , methadone.
, methadone.
Safety
A total of 315 serious adverse events were reported during the 12-month study period: 177 among 124 participants in the heroin group and 138 among 88 participants in the methadone group (Table 3). In 58 instances (32.8%) in the heroin group, the adverse event was possibly, probably or definitely related to the study medication, whereas in the methadone group this occurred less often (15 serious adverse events, 10.9%).
Table 3 Serious adverse events in intent-to-treat population during 12-month study period
| Heroin | Methadone | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Events | 177 | 100 | 138 | 100 | 315 | 100 | |||
| Possibly related to heroin or methadone | 34 | 19.2 | 8 | 5.8 | 42 | 13.3 | |||
| Probably/definitely related to heroin or methadone | 24 | 13.6 | 7 | 5.1 | 31 | 9.8 | |||
| Possibly/probably/definitely related to heroin or methadone | 58 | 32.8 | 15 | 10.9 | 73 | 23.2 | |||
| Related to intravenous application | 41 | 23.2 | 41 | 13.0 | |||||
| Treatment days until occurrence of event possibly/probably/definitely related to study medication | 2572 1 | 6501 2 | 3382 | ||||||
1. 149 350 cumulative treatment days in heroin group
2. 97 500 cumulative treatment days in methadone group
Of the 58 adverse events possibly, probably or definitely related to the heroin medication, 41 occurred within a few minutes of injection, 31 of these events were related to respiratory depression, in most cases associated with unreported concomitant illicit benzodiazepine use, whereas 10 were related to an epileptic seizure. Considering the longer average length of per-protocol treatment in the heroin compared with the methadone group (149 350 v. 97 500 cumulative treatment days), a serious adverse event that was possibly, probably or definitely related to the study medication occurred 2.5 times more often (every 2572 v. 6501 treatment days in the heroin and methadone groups respectively). There were 12 deaths (5 in heroin group, 7 in methadone group) in the 12-month study period for the intent-to-treat population. Of these only 5 occurred while the participant was using study medication and none were possibly, probably or definitely related to the study medication (3 in heroin group: 1 spleen rupture after falling, 1 intoxication with illicit methadone 1 owing to pneumonia and myocarditis; 2 in methadone group: 1 ruptured aneurysm, 1 reason unknown but no methadone in days before death).
DISCUSSION
Main findings
This randomised controlled trial found that heroin-assisted treatment of people with severe opioid dependence and treatment resistance more effectively improved health and reduced illicit drug use than methadone maintenance treatment. The main effect of heroin-assisted treatment on each primary outcome measure was seen within the first few months of treatment, and became more pronounced over the following months, thus indicating the necessity of long-term treatment to increase health benefits. The high response rates in the methadone group indicate that a well-structured treatment with trained therapists using standardised and clinically relevant psychosocial interventions can lead to positive outcomes even in a group that has previously responded poorly to methadone treatment. The confirmation of the positive results in the heroin group in the per-protocol analysis is of importance because a positive outcome in the methadone group was expected owing to a low retention rate (highly selected group) but remained significantly below the positive outcome in the heroin group.
These positive effects of heroin-assisted treatment should be weighted against the higher rate of serious adverse events which appear to be associated with the route of administration of opioids and are not unexpected. However, the controlled clinical setting for heroin treatment, with a required 30 min stay after intravenous injection, allows adverse events to be easily managed clinically, unlike when street heroin is injected in uncontrolled and unhygienic settings. No fatalities occurred that were possibly, probably or definitely related to the study medication in either group. The rate of serious adverse events was higher than in the Dutch study (Reference van den Brink, Hendriks and Blankenvan den Brink et al, 2003), which may be because in the latter study heroin-assisted treatment was supplementary to methadone maintenance treatment.
This study confirms in a large sample the positive effects of heroin-assisted treatment reported from uncontrolled (Reference Rehm, Gschwend and SteffenRehm et al, 2001) and controlled (Reference Perneger, Giner and del RioPerneger et al, 1998; Reference van den Brink, Hendriks and Blankenvan den Brink et al, 2003) trials for people resistant to methadone treatment. These data also show that heroin-assisted treatment can be helpful for those with heroin dependence currently not in treatment. It should be noted, however, that many of the latter group have an extensive treatment history and their baseline characteristics were similar to the methadone patients. The use of two structured psychosocial interventions in each treatment condition suggests that the observed differences between the methadone and heroin groups were not the result of differences in psychosocial treatment.
Another methodological strength of the study is the conservative analysis strategy, using a worst case strategy for all missing data not replaced by LOCF. Considering the nature of this group of patients, the high rate of adherence, with 12-month data for most participants, strengthens the interpretation of the results. Despite a general preference for other methods such as direct likelihood analysis or multiple imputation for missing data, in this study these methods would have reproduced differences in distribution of missing values, whereas the LOCF procedure allowed only data collected after 6 months to replace missing data and mirrors more actual treatment effects. Considering the high drop-out rate in the methadone group, a LOCF procedure leads to more results of patients still in treatment, therefore favouring the overall results of the methadone group.
Limitations of the study
Given the nature of the medication under study, a double-blind design was not possible (Reference Bammer, Dobler-Mikola and FlemingBammer et al, 1999). Furthermore, the response rates for the primary outcome measure ‘health’ were much higher for both groups than expected, so that the extent of improvement defined as a response may have been too low. Therefore, a sensitivity analysis using the worst case strategy and a 40% improvement as a definition of response was performed, in order to better compare the results with the Dutch study (Reference van den Brink, Hendriks and Blankenvan den Brink et al, 2003). This showed that lower response rates were observed, but the response rate for the heroin group remained significantly higher than that for the methadone group (75.7% v. 68.0%, OR=1.48, 95% CI 1.12–1.96, P=0.006). Even an increase in the minimal improvement to 50% did not change the result of a significantly more positive effect of heroin treatment (69.5% v. 58.6%, OR=1.63, 95% CI 1.26–2.13, P<0.001). The analysis with a single response criterion – those participants responding on both primary outcome measures – allows for an easier comparison with and confirmation of the Dutch results. However, the analysis of separate response criteria has the advantage of allowing a more differentiated analysis of effects.
Another aspect that needs to be discussed is the improvement in the month between baseline and initiation of treatment with study medication, especially with respect to physical health. This improvement is probably the result of a combination of regression to the mean and treatment between baseline assessment and randomisation. Considering the very poor health status of the sample at baseline, for ethical reasons physical and/or mental health problems had to be attended to even before initiation of study treatment. However, since randomisation took place thereafter, treatment prior to randomisation and possible improvements do not bias the observed differences between the two medication conditions (heroin or methadone) after 12 months' treatment. None the less, if the response criteria for physical health were defined using the OTI score at initiation of treatment as the baseline, 77.1% of the heroin group and 69.2% of the methadone group would have been defined as responders for the primary outcome measure ‘health’, with a significant difference (OR=1.50, 95% CI 1.13–1.99, P=0.005).
The rather low retention rate in the methadone group could be considered a further limitation. The high drop-out rate in the methadone group is probably a result of the disappointment at not being randomised into the heroin group. However, a large portion of those dropping-out took up other treatments, so that the limiting effect of the low retention rate is minimised in a randomised intent-to-treat analysis.
A final limitation is that not all data on illicit drug use were based on objective urine or hair analysis, self-reported data were also included. However, studies have shown self-reported data to be accurate, reliable and valid, provided that confidentiality is ensured and no sanctions are connected to the answers (Reference Rounsaville, Rounsaville, Tims and HortonRounsaville, 1993).
Implications
This large multicentre study confirms the results of the Swiss (Reference Rehm, Gschwend and SteffenRehm et al, 2001) and Dutch (Reference van den Brink, Hendriks and Blankenvan der Brink et al, 2003) studies and therefore addresses the limitations pointed out by the Cochrane review (Reference Ferri, Davoli and PerucciFerri et al, 2005) by providing strong further evidence of the efficacy of prescribed heroin in the treatment of people with opioid dependence who have not profited from other forms of treatment. Considering the higher rate of serious adverse events, heroin prescription should remain a treatment of last resort for people who are currently or have in the past failed at maintenance treatment.
Acknowledgements
We thank patients and staff who participated in the study, as well as the Safety and Advisory Boards for their advice and support. The trial was commissioned and funded by a joint working group of the German Ministry of Health, the seven participating cities and the states of Hessen, North Rhine-Westphalia and Lower Saxony.










eLetters
No eLetters have been published for this article.