Key message: Evidence from randomized controlled trials of efficacy of self-management programs for chronic non-cancer pain suggests little to no improvement in overall, physical, or mental health-related quality of life when compared with usual care among adults.
Introduction
The etiology of many chronic pain conditions is often unclear and is mostly multifactorial; characterized by a complex interaction between biological, psychological, and social factors. Reference Fillingim, Bruehl and Dworkin1 The World Health Organization International Classification of Diseases 11 (ICD-11) regards pain to be chronic if it lasts or recurs for at least three months, persisting past normal healing time, and lacking acute warning physiological signs, is associated with significant emotional distress and/or functional disability, and not explained by a known condition. Reference Smith, Fors and Korwisi2 Chronic pain affects an estimated 20% of individuals Reference Goldberg and McGee3,Reference Gureje, Von Korff and Kola4 and accounts for an estimated 15 to 20% of primary care visits globally. Reference Mantyselka, Kumpusalo and Ahonen5 In the United States of America (USA) alone, using the Medical Expenditure Panel Survey, the annual cost of chronic pain was estimated to be as high as $635 billion a year in 2010 dollars, which was more than the annual costs for cancer, heart disease, and diabetes. Reference Gaskin and Richard6 Chronic pain is therefore of immense public health concern, and estimates suggest a prevalence rate of 5 to 33% for chronic non-cancer pain (CNCP). Reference Reid, Engles-Horton and Weber7
Despite substantially high prevalence, associated morbidity, and deleterious impact of chronic pain, the available evidence indicates that chronic pain is mostly undertreated especially among older adults (65+ years old). Reference Landi, Onder and Cesari8,Reference Sengstaken and King9 Owing to the enormous cost and adverse side effects of many pharmacological pain management agents, Reference Gloth10 the limited efficacy of standard therapies for chronic pain, and the need to maximize the effectiveness of management regiments, Reference Marks, Allegrante and Lorig11 a variety of self-management programs (SMPs) have been proposed and are being developed for the management of chronic pain. Self-management is defined as tasks undertaken by an individual to help them cope and live well with one or more chronic conditions, including motivation of oneself and confidence in dealing with medical, physical, and emotional management of their conditions. Reference Adams, Greiner and Corrigan12 Self-management therefore entails informed tasks and actions to manage chronic conditions effectively. SMPs for CNCP vary in composition but typically include combinations of pain education, tailored exercises, mind and body relaxation, cognitive coping, problem-solving, and communication skills training. Reference Reid, Papaleontiou and Ong13 They also can differ with respect to the mode of delivery (individual or group-based) and duration.
In view of the accumulating evidence and varied conclusions from studies of SMPs for CNCP in adults, we systematically identified, critically appraised, and summarized the findings from randomized controlled trials (RCTs) that compared the efficacy of SMPs for CNCP against usual care, focusing on health-related quality of life (HR-QoL).
Methods
We conducted this rapid systematic review as part of a Systematic Prospective Assessment of Rapid Knowledge Synthesis (SPARKS) project (https://osf.io/fnx36/), and the review was registered with the Open Science Framework (registration: osf.io/tzje2) prior to commencement. The review was conducted in accordance with the World Health Organization guidelines for rapid reviews, Reference Tricco, Langlois and Straus14 and we reported the findings following the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines. Reference Page, McKenzie and Bossuyt15 A knowledge synthesis librarian (NA) designed a literature search strategy for Medline (Ovid), and another librarian peer reviewed the search strategy using the Peer Review of Electronic Search Strategies (PRESS) checklist. Reference McGowan, Sampson and Salzwedel16 The revised search strategy (Appendix 1) was adapted for Embase (Ovid) and Cochrane (CENTRAL) (Ovid). The literature search was first conducted in March 2019 with the search limited to articles published since 2009 in the English language. While the decision to limit to articles published since 2009 was part of the SPARKS methodology of limiting literature to within the last 10 years, it also enabled concentration on more recent SMPs for CNCP as SMPs protocols are still evolving. The searches were updated in August 2021.
We evaluated the comparative efficacy of SMPs compared with usual care in improving HR-QoL in adults (18+ years old) with CNCP (ICD-11), focusing on English-language publications of RCTs. Trial participants were individuals with CNCP recurring for more than 3 consecutive months. We excluded studies on individuals with chronic cancer-related pain. A SMP must have a reflexive component and addresses an individual’s ability to manage their condition. We included SMPs irrespective of administration modalities, types, and duration. We excluded SMPs that are just educational programs or peer-support groups. Usual care included any educational programs or peer-support groups. The primary outcome was HR-QoL.
Retrieved citations from the literature searches were screened by one reviewer. We documented the number of ineligible citations at the title/abstract screening stage and both the number and reasons for ineligibility at the full-text article screening stage. The reviewer scanned references of all included full-text articles for potential RCTs for inclusion. The reviewer also extracted data from the included RCTs and assessed risk of bias using the Cochrane tool for risk of bias assessment in RCTs. Reference Sterne, Savovic and Page17 Another reviewer checked the extracted data and risk of bias assessments for errors. The two reviewers resolved any discrepancies through discussions or involvement of another reviewer.
The characteristics of the included RCTs and the risk of bias assessments are presented descriptively and in tabular form. To account for different scale measurements of the outcome and potential differences in implementation of scales across RCTs, where appropriate (at least two contributing RCT results), we conducted meta-analysis using an inverse variance, random-effects model and calculated the standardized mean difference (SMD) and associated 95% confidence interval (CI). We assessed and quantified statistical heterogeneity between pooled results using the I 2 statistic. Reference Higgins and Thompson18 Where appropriate (at least ten contributing RCT results), publication bias was assessed using the Egger’s regression test. Reference Sterne, Egger and Smith19 All statistical analyses were implemented in STATA (version 13; Stata Corp. LP, College Station, TX).
Results
From a total of 8,538 retrieved citations, 28 RCTs (29 publications) Reference Ackerman, Buchbinder and Osborne20–Reference Yang, Wei, Ge, Meng and Zhao48 met the eligibility criteria (Figure 1). Relevant characteristics of the RCTs are summarized in Table 1 and Appendix 2. There were five RCTs from Spain, Reference Ariza-Mateos, Cabrera-Martos and Lopez-Lopez22,Reference Izquierdo-Alventosa, Ingles and Cortes-Amador32,Reference Lopez-Lopez, M. and J.36,Reference Molinari, Garcia-Palacios and Enrique40,Reference Rodriguez-Torres, Lopez-Lopez and Cabrera-Martos46 four RCTs from each of Australia, Reference Ackerman, Buchbinder and Osborne20,Reference Bennell, Ahmed and Jull23,Reference Gardner, Refshauge, McAuley, Hübscher, Goodall and Smith29,Reference Nelligan, Hinman, Kasza, Crofts and Bennell43 China, Reference Cheung, Yeung and Suen27,Reference Kwok, Au and Li-Tsang33,Reference Sit, Choi and Wang47,Reference Yang, Wei, Ge, Meng and Zhao48 and the USA, Reference Allen, Somers and Campbell21,Reference Cederbom, Leveille and Bergland26,Reference Fanning, A. and H.28,Reference Morone, Greco and Moore41 two RCTs from each of Canada, Reference Bourgault, Lacasse and Marchand25,Reference Lang, Hendrick and Clay34 Norway, Reference Haugmark, Hagen, Provan and Zangi30,Reference Nøst, Steinsbekk, Bratås and Grønning44,Reference Nøst, Steinsbekk, Bratås and Grønning45 Portugal, Reference Marconcin, Espanha and Teles38,Reference Marconcin, Yazigi and Teles39 and the United Kingdom, Reference Littlewood, Malliaras, Mawson, May and Walters35,Reference Manning, Hurley, Scott, Coker, Choy and Bearne37 and one RCT from each of India, Reference Bhatia, Karvannan and Prem24 the Netherlands, Reference Hutting, Staal and Engels31 and Switzerland Reference Muller, Segerer and Ronca42 . Participants’ inclusion criteria varied across the RCTs especially regarding patient characteristics, pain type, and pharmacological treatments that participants were allowed to be on, or may have received, during the course of the RCTs. The number of participants varied across the RCTs, ranging from 8 to 282. None of the RCTs was funded by industry; 22 RCTs were funded by non-industry sources while six RCTs received no funding.
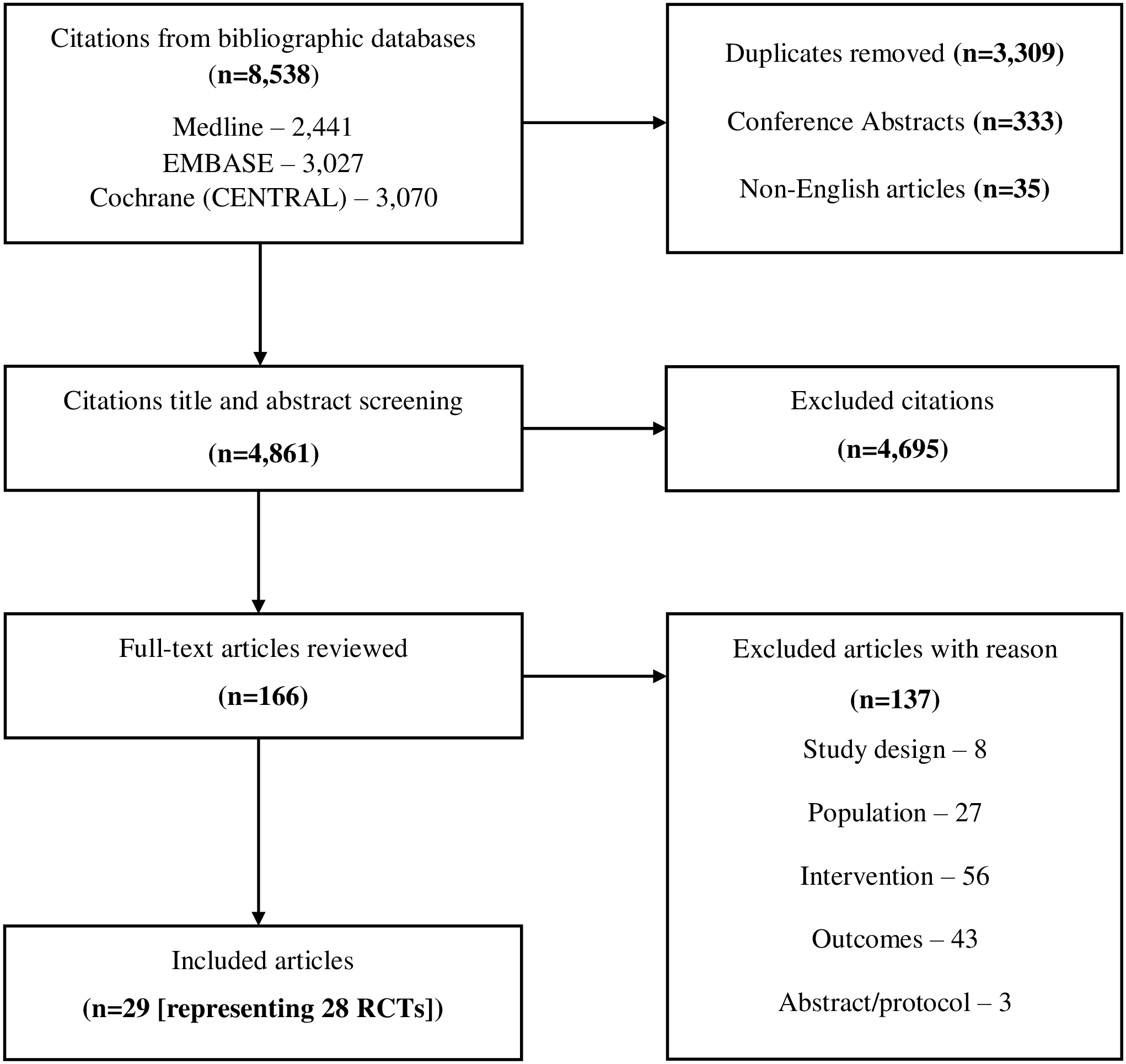
Figure 1: Summary of literature search and screening process (modified PRISMA flowchart).
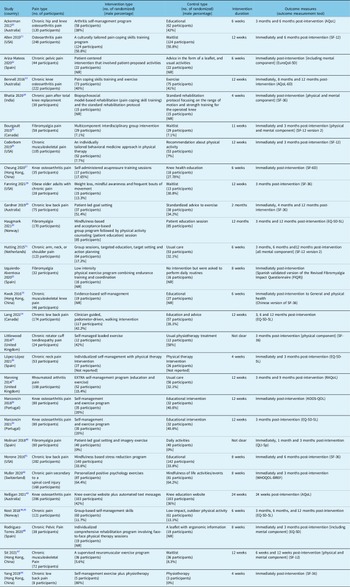
Table 1: Summary characteristics of the included RCTs
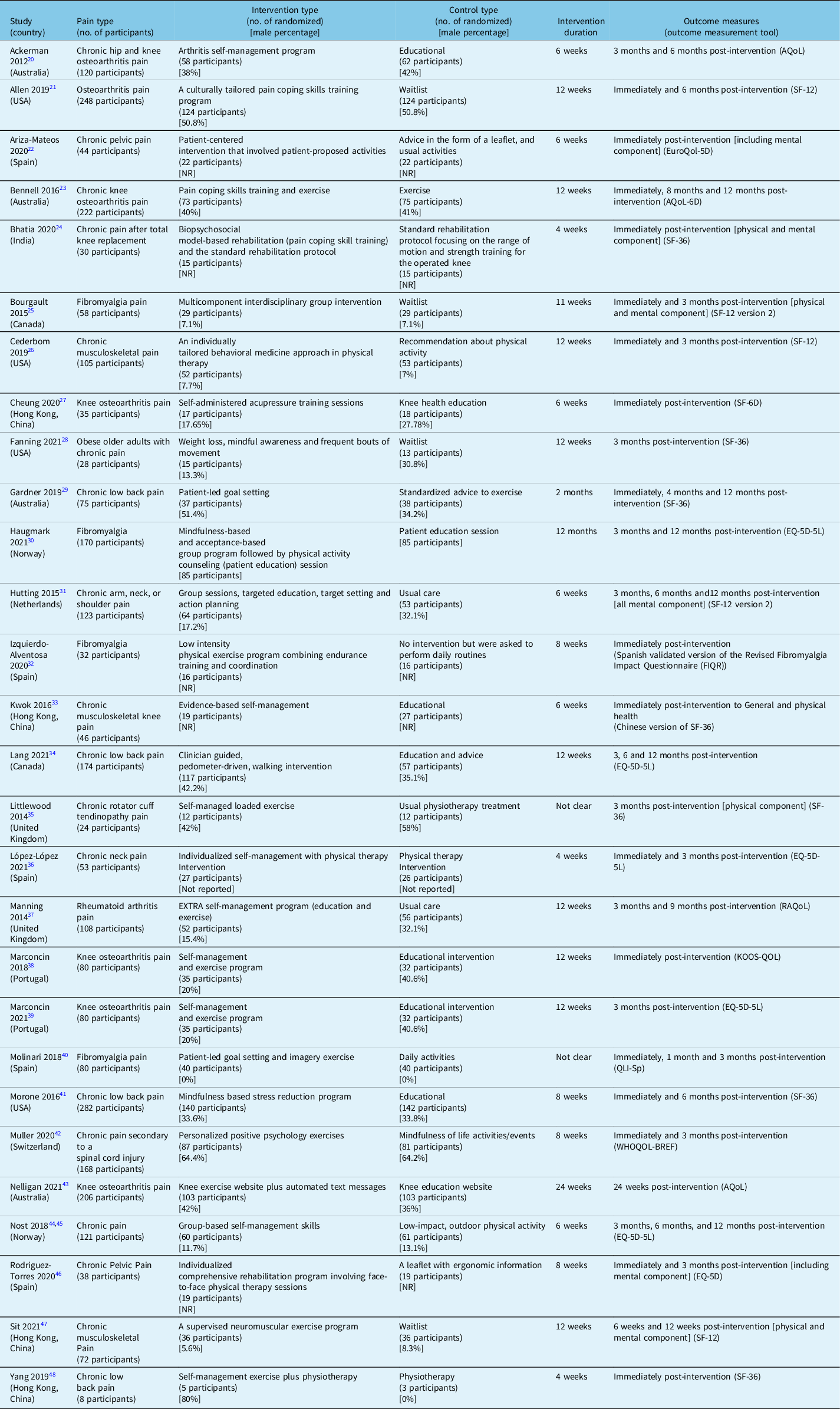
AQoL = assessment of quality of life scale; EQ-5D = Euro quality of life 5 dimensions scale; FIQR = revised fibromyalgia impact questionnaire; KOOS-QoL = Knee injury and osteoarthritis outcome score for quality of life; QLI-Sp = Spanish version of quality of life index scale; RAQoL = rheumatoid arthritis quality of life scale; SF-6D = Short-Form Health Survey 6 Scale; SF-12 = Short-Form Health Survey 12 Scale; SF-36 = Short-Form Health Survey 36 Scale; WHOQOL-BREF = World Health Organization quality of life; NR = not reported.
The compositions of SMPs examined in the RCTs varied and were mostly focused on a pain type and included pain coping skills, activity management, healthy living, goal setting, and stress reduction. However, they were comparable in terms of their overarching types, and the associated usual care comparators were mainly educational or daily activities. There was however substantial variability in the method of application of the SMPs. Duration of intervention ranged from 4 weeks to 12 months. Follow-up after completion of the intervention ranged from one to 12 months.
Ten measurement scales for HR-QoL were identified. These were the AQoL (assessment of quality of life scale), Reference Ackerman, Buchbinder and Osborne20,Reference Bennell, Ahmed and Jull23,Reference Nelligan, Hinman, Kasza, Crofts and Bennell43 EQ-5D (Euro quality of life 5 dimensions scale), Reference Ariza-Mateos, Cabrera-Martos and Lopez-Lopez22,Reference Haugmark, Hagen, Provan and Zangi30,Reference Lang, Hendrick and Clay34,Reference Lopez-Lopez, M. and J.36,Reference Marconcin, Yazigi and Teles39,Reference Nøst, Steinsbekk, Bratås and Grønning44–Reference Rodriguez-Torres, Lopez-Lopez and Cabrera-Martos46 FIQR (revised fibromyalgia impact questionnaire), Reference Izquierdo-Alventosa, Ingles and Cortes-Amador32 KOOS-QoL (Knee injury and osteoarthritis outcome score for quality of life), Reference Marconcin, Espanha and Teles38 QLI-Sp (Spanish version of quality of life index scale), Reference Molinari, Garcia-Palacios and Enrique40 RAQoL (rheumatoid arthritis quality of life scale), Reference Manning, Hurley, Scott, Coker, Choy and Bearne37 SF-6D (Short-Form Health Survey 6 Scale), Reference Cheung, Yeung and Suen27 SF-12 (Short-Form Health Survey 12 Scale), Reference Allen, Somers and Campbell21,Reference Bourgault, Lacasse and Marchand25,Reference Cederbom, Leveille and Bergland26,Reference Hutting, Staal and Engels31,Reference Sit, Choi and Wang47 SF-36 (Short-Form Health Survey 36 Scale), Reference Bhatia, Karvannan and Prem24,Reference Fanning, A. and H.28,Reference Gardner, Refshauge, McAuley, Hübscher, Goodall and Smith29,Reference Kwok, Au and Li-Tsang33,Reference Littlewood, Malliaras, Mawson, May and Walters35,Reference Morone, Greco and Moore41,Reference Yang, Wei, Ge, Meng and Zhao48 and WHOQOL-BREF (World Health Organization quality of life) Reference Muller, Segerer and Ronca42 . None of the RCTs was judged to be at a low risk of bias (Figure 2).

Figure 2: Risk of bias assessment of the included RCTs. RCTs = randomized controlled trials.
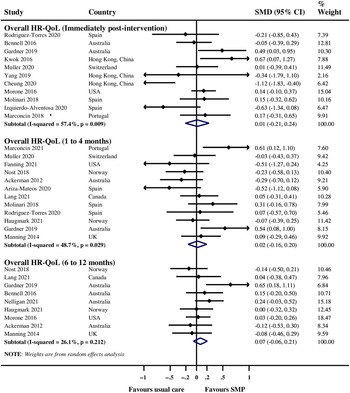
Meta-analysis of SMPs Compared with Usual Care for Overall HR-QoL
There was no evidence of a significant improvement in overall HR-QoL immediately post-intervention (SMD 0.01, 95% CI −0.21 to 0.24; I 2 57%; 11 RCTs; Egger’s test p 0.21; 979 participants), one to four months post-intervention (SMD 0.02, 95% CI −0.16 to 0.20; I 2 48.7%; 12 RCTs; Egger’s test p 0.41; 1,160 participants), and six to twelve months post-intervention (SMD 0.07, 95% CI −0.06 to 0.21; I 2 26.1%; 9 RCTs; 1404 participants) with SMPs compared with usual care (Figure 3). There was no evidence of a significant improvement in overall HR-QoL immediately post-intervention among individuals with fibromyalgia, knee osteoarthritis pain, and low back pain (Appendix 3); one to four months post-intervention among individuals with fibromyalgia, low back pain, and pelvic pain (Appendix 4); and 6 to 12 months post-intervention among individuals with knee pain and low back pain (Appendix 5).

Figure 3: Meta-analysis of SMPs compared with usual care for overall HR-QoL. SMD = D standardized mean difference; SMP = self-management program; HR-QoL = health-related quality of life.
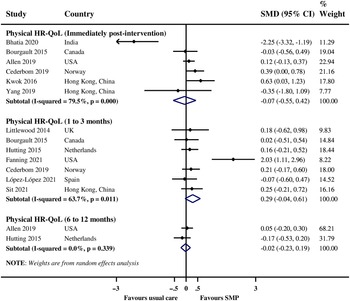
Meta-analysis of SMPs Compared with Usual Care for Physical HR-QoL
There was no evidence of a significant improvement in physical HR-QoL immediately post-intervention (SMD −0.07, 95% CI −0.55 to 0.42; I 2 79.5%; 6 RCTs; 495 participants), one to three months post-intervention (SMD 0.29, 95% CI −0.04 to 0.61; I 2 63.7%; 7 RCTs; 457 participants), and six to twelve months post-intervention (SMD −0.02, 95% CI −0.23 to 0.19; I 2 0%; 2 RCTs; 365 participants) with SMPs compared with usual care (Figure 4). There was a paucity of data to enable stratified analysis by pain type and further exploration of the observed high heterogeneity in the pooled analyses.

Figure 4: Meta-analysis of SMPs compared with usual care for physical HR-QoL. SMD = D standardized mean difference; SMP = self-management program; HR-QoL = health-related quality of life.
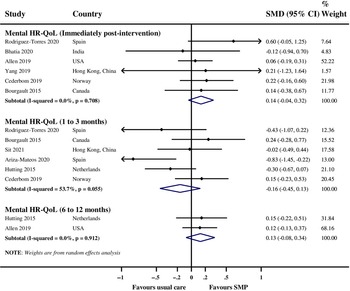
Meta-analysis of SMPs Compared with Usual Care for Mental HR-QoL
There was no evidence of a significant improvement in mental HR-QoL immediately post-intervention (SMD 0.14, 95% CI −0.04 to 0.32; I 2 0%; 6 RCTs; 487 participants), one to three months post-intervention (SMD −0.16, 95% CI −0.45 to 0.13; I 2 53.7%; 6 RCTs; 434 participants), and six to twelve months post-intervention (SMD 0.13, 95% −0.08 to 0.34; I 2 0%; 2 RCTs; 365 participants) with SMPs compared with usual care (Figure 5). There was a paucity of data to enable stratified analysis by pain type and further exploration of the observed high heterogeneity in the pooled analysis for one to three months post-intervention.

Figure 5: Meta-analysis of SMPs compared with usual care for mental HR-QoL. SMD = D standardized mean difference; SMP = self-management program; HR-QoL = health-related quality of life.
Meta-analysis of SMPs Compared with Usual Care by HR-QoL Measurement Scale
There was no evidence of a significant improvement in overall, physical or mental HR-QoL except for a marginally significant improvement in overall HR-QoL immediately post-intervention measured using the SF-36 (SMD 0.31, 95% CI 0.01 to 0.61; I 2 32.8%; 4 RCTs; 411 participants) and in mental HR-QoL one to three months post-intervention measured using the EQ-5D scale (SMD −0.64, 95% CI −1.08 to −0.19; I 2 0%; 2 RCTs; 82 participants) (Table 2).
Table 2: Meta-analysis of SMPs compared with usual care for HR-QoL by measurement scale type

SMPs = self-management programs; HR-QoL = health-related quality of life; AQoL = assessment of quality of life scale; EQ-5D = Euro quality of life 5 dimensions scale; FIQR = revised fibromyalgia impact questionnaire; KOOS-QoL = Knee injury and osteoarthritis outcome score for quality of life; QLI-Sp = Spanish version of quality of life index scale; RAQoL = rheumatoid arthritis quality of life scale; SF-6D = Short-Form Health Survey 6 Scale; SF-12 = Short-Form Health Survey 12 Scale; SF-36 = Short-Form Health Survey 36 Scale; WHOQOL-BREF = World Health Organization quality of life.
Discussion
We conducted a rapid review to summarize the evidence from RCTs of SMPs compared with usual care for CNCP in adults. We found no evidence of a significant improvement in overall HR-QoL irrespective of pain type nor in physical and mental HR-QoL with SMPs compared with usual care among adults irrespective of SMP intervention duration and the duration of follow-up prior to assessment. While our findings provide some insights into the efficacy of SMPs for HR-QoL in adult individuals with CNCP, we advise cautious interpretation of the findings as the SMPs and the comparator usual care differed substantially and participants’ inclusion criteria varied across the RCTs, in particular, regarding patient characteristics, pain type, and pharmacological treatments that participants may have received during the course of the RCTs, including medication use and adherence. Further, other chronic diseases from which the study participants may also be suffering may have differed across the RCT populations. Moreover, all included RCTs were classified as having some concerns or at high risk of bias.
The general notion is that SMPs are likely effective for CNCP especially in targeted specific (homogeneous) patient populations. While the assessed pain was mostly of musculoskeletal type in most of the included RCTs, we found no evidence of significant improvement in overall HR-QoL among patients with fibromyalgia, knee pain, low back pain, and pelvic pain. While we were unable to compare the efficacy of SMPs in subpopulations (e.g., by gender, age, opioid use) and to explore the influence of characteristics of the included RCTs on the pooled effect estimates due to a lack of data, the observed non-significant improvement in HR-QoL for SMPs when compared with usual care in adults with CNCP may be due to the differences and a lack of uniformity in the compositions and applications of SMPs. This is likely made worse by variability in the characteristics of the included RCTs and adherence (compliance) to SMPs by participants across the RCTs. It was difficult to determine a specific SMP or a stand-alone approach to an SMP from this review. It was also difficult to assess the true efficacy of the SMPs, considering their differing composite nature and a lack of a standard definition. While factors that may predict HR-QoL outcomes in CNCP using SMPs are not yet established, various strategies to enhance an individual’s ability to manage their chronic health condition to support efficacy of SMPs in chronic conditions have been proposed by the Registered Nurses’ Association of Ontario (RNAO), with recommendation of nurses involvement throughout care and that nurses establish a written agenda for appointments in collaboration with individuals and family and that this may include review of clinical data, experiences with SMP, medication, barriers and stressors, and action planning and continued education. 49 RNAO argues that with the use of SMPs, individuals need to work in collaboration with nurses and other healthcare professionals and assume greater responsibility for healthcare decisions. 49 Such an approach, particularly identification and removal of barriers and stressors, may improve HR-QoL with use of SMPs in CNCP.
While there is a substantial number of published systematic reviews on SMPs for varied CNCP, Reference Du, Yuan, Xiao, Chu, Qiu and Qian50–Reference Elbers, Wittink, Pool and Smeets52 summary of the evidence regarding HR-QoL is lacking. A review by Mann and colleagues of SMPs for chronic pain that met Lorig and Holman’s definition of SMPs Reference Lorig and Holman53 concluded that SMPs are efficacious in improving mental health and HR-QoL outcomes in individuals with chronic pain. Reference Mann, LeFort and VanDenKerkhof54 However, this was a descriptive review, and as such, not appropriate for determining efficacy. Another review by Turk and colleagues considered integrated interdisciplinary rehabilitation programs with cognitive restructuring with an emphasis on promotion of self-management, self-efficacy, resourcefulness, and activity versus passivity, reactivity, dependency, and hopelessness. Reference Turk, Wilson and Cahana55 The authors concluded that the available interventions provided minimum improvements in physical and emotional functioning. However, this was also a descriptive review and not appropriate for determining efficacy. Further, Guzman and colleagues assessed the efficacy of outpatient psychophysical treatments from RCTs of patients with disabling chronic low back pain, and while the authors reported that a few RCTs assessed the effect on quality of life, they concluded that less intensive outpatient psychophysical treatments did not improve pain, function, or vocational outcomes when compared with non-multidisciplinary outpatient therapy or usual care. Reference Guzman, Esmail and Karjalainen56
We searched a limited number of bibliographic databases given that this was a rapid review although conducted systematically, and while it is possible that we may have missed potentially relevant RCTs as a result, we searched the three main bibliographic databases that are highly relevant to the review topic, and we carefully negotiated efficiencies into our approach. However, we included only English-language publications and therefore may have missed some relevant non-English publications. In keeping with rapid review expectations, only one reviewer selected studies for inclusion in the review, which poses the potential for erroneous omission and selection bias, although this process was conducted by an experienced reviewer. Nevertheless, the reviewer scanned references of all included full-text articles for potential RCTs for inclusion, and while only the reviewer extracted data and assessed risk of bias of the included RCTs, another reviewer checked the extracted data and risk of bias assessments for errors. Notwithstanding these potential limitations, the search strategies employed in this rapid review were developed by a highly skilled knowledge synthesis librarian and peer reviewed by another skilled knowledge synthesis librarian using the PRESS checklist. This approach strengthened the appropriate identification of potential literature for inclusion. Our findings answer important clinical questions that may be of help to clinicians in considering SMPs for CNCP and making informed CNCP management decisions for their patients.
Conclusions
There is a lack of evidence from RCTs that SMPs are efficacious in improving overall, physical, and mental HR-QoL in adult individuals with CNCP compared with usual care. A lack of uniformity in the composition and application of SMPs and in the compared usual care require that future research should focus on standardization of SMPs for CNCP and adopting uniformity in the usual care comparator. Further, the risk of bias concerns across the available body of evidence require that better planned/conducted RCTs are needed to confirm the conclusions from this present review. Future research should also consider exploring the administrative and health systems supports that may be needed to support the delivery of SMPs as the knowledge may enhance the efficacy of SMPs for CNCP.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/cjn.2022.261
Acknowledgements
We thank Dr Andrea C. Tricco and Ms. Nazia Darvesh of the Knowledge Synthesis Team, Li Ka Shing Knowledge Institute of St. Michael’s Hospital for their support and coordination of the study.
Funding
This work was supported by the Canadian Institutes of Health Research (CIHR) Project Grant for Systematic Prospective Assessment of Rapid Knowledge Synthesis (SPARKS).
Disclosures
The authors do not have any relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants, or patents received or pending, or royalties.
Statement of Authorship
Methodology (GNO, NA, LW, JG, AH, BM & AMAS); Data acquisition (GNO, OLTL, VKR, NA, NAY & AMAS); Formal analysis (GNO); Interpretation (GNO, LW, JG, AH, BM & AMAS); Validation (GNO & AMAS); Draft manuscript (GNO); Manuscript revisions (GNO, OLTL, VKR, NA, NAY, LW, JG, AH, BM & AMAS); Final approval for submission (GNO, OLTL, VKR, NA, NAY, LW, JG, AH, BM & AMAS); Accountability (GNO & AMAS)
Submission Declaration
The authors declare that this work has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere including electronically in the same form, in English or in any other language, without the written consent of the copyright holder.