1. Introduction
Although the notion that the onset of psychosis is usually preceded by a “prodromal” phase was first recognized by Mayer-Gross in 1932 [Reference Mayer-Gross and Bunke50], formal PubMed research appeared only about 20 years ago in a pioneering work by Huber et al. (1989) [Reference Huber and Gross44]. Influenced by Mayer-Gross’ observations, Huber first described basic symptoms in the 1960s and initiated the first prospective early detection study in the 1980s [Reference Huber and Gross44]. Since then, there has been an exponential clinical and research interest into the high risk state for psychosis (for a comprehensive and up-to-date conceptual review see Fusar-Poli et al. [Reference Fusar-Poli, Borgwardt, Bechdolf, Addington, Riecher-Rössler and Schultze-Lutter17]). It is now clear that the high risk state (variably termed as At Risk Mental State, ARMS or Ultra High Risk, UHR or Clinical High Risk, CHR) is associated with an increased probability of developing a psychotic disorder – mainly schizophrenia spectrum disorders [Reference Fusar-Poli, Bechdolf, Taylor, Bonoldi, Carpenter and Yung21] – over time, from 18% at six months up to 36% after three years [Reference Fusar-Poli, Bonoldi, Yung, Borgwardt, Kempton and Barale36]. Broadly speaking the high risk state is characterized by the presence of subtresholded psychotic symptoms, cognitive and neurobiological deficits [28,37,31,16] and significant limitations in psychosocial functioning [Reference Addington, Penn, Woods, Addington and Perkins1]. A growing interest in this area has lead to the discussed proposal of including a new high risk diagnostic category in the forthcoming DSM-5 [Reference Fusar-Poli and Yung15]. In such a scenario, the Outreach and Support in South London (OASIS) team has played a pivotal role as one of the first and largest services in the world devoted to the diagnosis and clinical management of potential prodromal psychosis. In about one decade, the OASIS team has become an established model where clinical practice and research are fully integrated in the field of preventative interventions in psychosis. In this article we will present the progresses that have been made since the development of the OASIS service, while recognizing at the same time the future challenges.
2. Methods
2.1. Sample
All subjects with “at risk” signs or symptoms for psychosis referred to the OASIS service for assessment and diagnosis over the past decade (2001–2011) were included in the present analysis.
2.2. Outcome variables
The present study has evaluated the impact of the OASIS service on three outcome measures:
diagnosis of high risk subjects;
clinical management of subjects with an enhanced risk for psychosis;
implementation of a clinical-academic model for ongoing research in the mental health services.
The first outcome was analyzed with respect to the development of local early intervention services, description of the catchment area (number of referrals, psychometric assessment of presenting psychopathology, inclusion and exclusion criteria, differential diagnosis, definition of different high risk subgroups, pathways to care, assessment of social functioning and comorbid diagnoses). The second outcome was analyzed with respect to the logistic demands for the implementation of prodromal services, clinical outcomes relevant to the treatment of high risk patients (case management, focused interventions, transition outcomes, integration with first-episode services, treatment of patients in prison) and economic considerations. The third outcome was analyzed with respect to the development of clinical academic groups, neuroimaging investigations of subjects at risk for psychosis and by discussing other research approaches.
2.3. Statistical analysis
Descriptive statistics included mean and standard deviation for continuous variables and absolute and relative frequencies for categorical variables. Histograms and pies were used to better describe each specific outcomes. Survival curves were calculated by Kaplan-Meier estimates along with the Log-rank test. Data were analyzed with IBM SPSS20.
3. Results
3.1. Diagnosis
3.1.1. Development of early interventions in South London and the Maudsley
The development of the early intervention services in South London and the Maudsley (SLaM) began in 1997, when shortcomings in existing services for young people with first-episode psychosis were first identified by an internally commissioned report in Lambeth called ‘Bridging the Gap’ [Reference Power, McGuire, Iacoponi, Garety, Morris and Valmaggia57]. The first service, the Lambeth Early Onset (LEO) Community Team began operation in January 2000 as an extended hours service from a small clinic near central Brixton [Reference Power, McGuire, Iacoponi, Garety, Morris and Valmaggia57]. As the LEO Community Team was being established a new acute 18-bed adult inpatient unit was commissioned at Lambeth Hospital in 2001, where it is still located. Furthermore, a Crisis and Assessment Team (LEO CAT) was developed in 2002 to target GPs, improve their detection and referral rates, and provide quick access for community based assessments and engagement into the first episode services [Reference Power, McGuire, Iacoponi, Garety, Morris and Valmaggia57]. The OASIS team was developed at the same time (2001) in the Lambeth borough to identify subjects at high clinical risk for psychosis [Reference Broome, Woolley, Johns, Valmaggia, Tabraham and Gafoor7].
3.1.2. Catchment area
The OASIS team is currently covering a wide urban area in South London catering for clients in four different boroughs (Lewisham, Croydon, Lambeth, Southwark). The overall catchment area is of about 1.18 million of citizens (Lewisham 264,500, Croydon 342,800, Lambeth 283,300, Southwark 285,600)(UK government national statistic; http://data.london.gov.uk/datastorefiles/visualisations/atlas/fol10-pop&mig-2010/atlas.html). The OASIS service is fully integrated with the new first-episode services, which have been developed in each of the above boroughs: Southwark Team for Early Psychosis (STEP); Lewisham Early Intervention Service (LEIS); Lambeth Early Onset Psychosis (LEO) and Croydon Outreach Assessment Support Team (COAST) (Fig. 1). The clinical management of these services has undergone a profound change with the development of the new NHS-Institute of Psychiatry Clinical Academic Groups (CAGs) (see the paragraph below here).
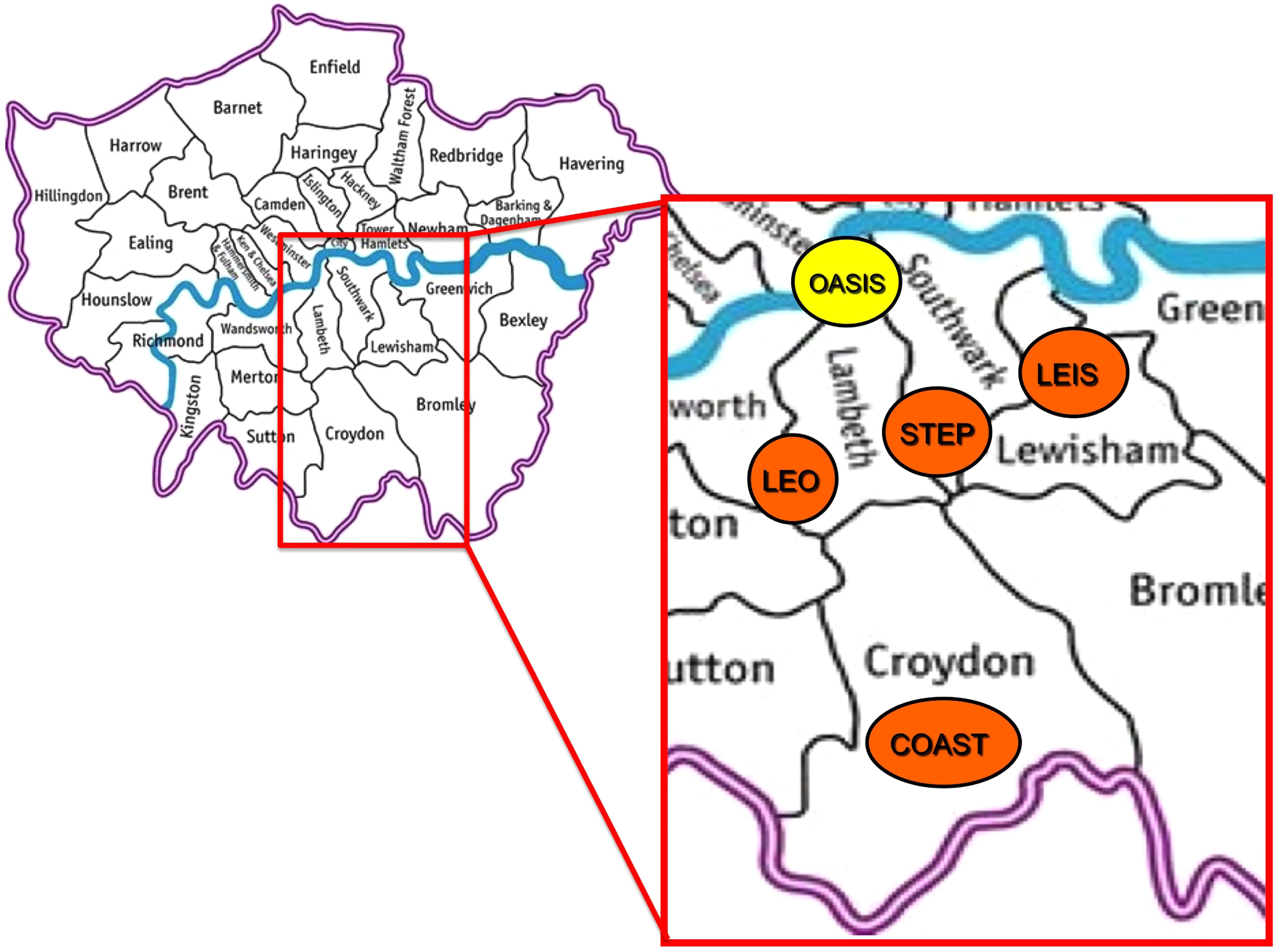
Fig. 1 Early intervention services in South London and Madusley (SLaM, Southwark, Lambeth, Lewisham, Croydon). In yellow prodromal teams, in orange first episode teams. OASIS: Outreach and Support in South London prodromal service; STEP: Southwark Team for Early Psychosis; LEIS: Lewisham Early Intervention Service; LEO: Lambeth Early Onset Psychosis; COAST: Croydon Outreach Assessment Support Team. The inpatient unit for first-episode psychotic patients is not represented.
South London is well recognized as having one of the highest rates of psychosis in the UK [Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant46] and one of the highest in the world. There are different reasons underlying the high incidence of psychosis in this area. For example, Lambeth has high proportion of Black and other ethnic minorities residents and the highest proportion of African–Caribbean residents in London. Consistent evidence indicates in the UK African-Caribbeans and Black Africans are at especially high risk for both schizophrenia and mania [Reference Fearon, Kirkbride, Morgan, Dazzan, Morgan and Lloyd14]. South London has a large migrant population [Reference Morgan and Fearon54] and migration has been associated with higher risk for psychosis [Reference Cantor-Graae8]. The unemployment rate in this area is high as well as the proportions of households and homelessness. Social fragmentation, urbanicity and deprivation have all been associated with an elevated risk of developing psychosis in the general population [Reference Allardyce, Gilmour, Atkinson, Rapson, Bishop and McCreadie2]. Fig. 2 summarizes the 2010 deprivation index of the different boroughs in London, illustrating the picture given above here.
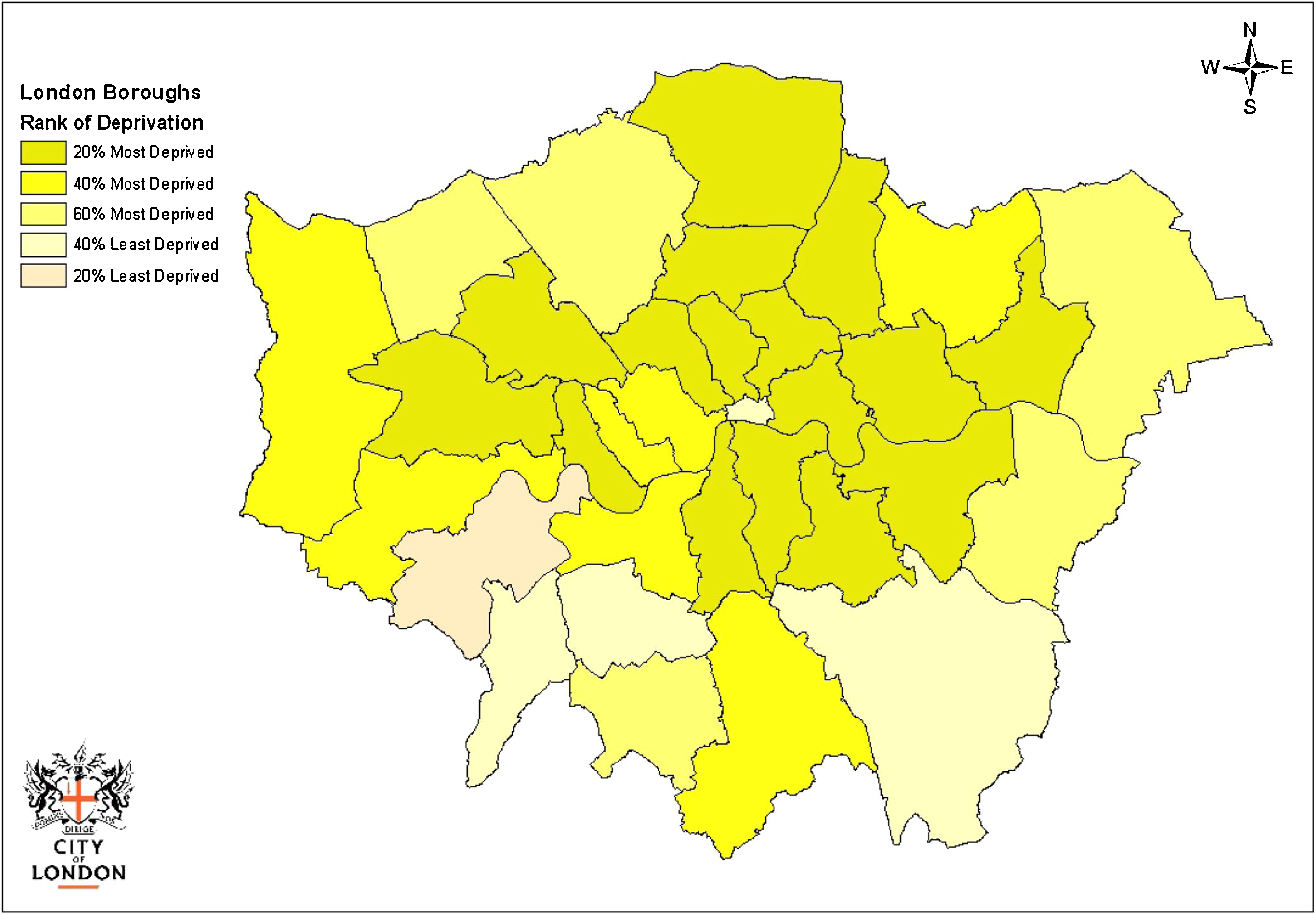
Fig. 2 2010 Deprivation indices for London Boroughs. South London, where the OASIS team is based, is characterized by a high level of social deprivation. Source: Indices of Deprivation, Department of Communities and Local Government, Crown Copyright 2010 http://www.cityoflondon.gov.uk/NR/rdonlyres/F3E4FC12-AF75-4D8E-8BAF-5CA643A5327B/0/DP_PL_DeprivationIndex2010_v2.pdf.
The additional concern is that the proportion of drug use in these areas is quite high. In particular there has been a worrying trend towards the utilization of street cannabis with higher concentration of d-9-tetrahydrocannabinoid, which is the active ingredient increasing the risk of psychosis [Reference Di Forti, Morgan, Dazzan, Pariante, Mondelli and Marques12]. Overall, in the 15–35 age group, the rate of new cases of psychosis is approximately 65/100,000 [Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant46]. The local prevalence of the ARMS is unknown, but if it is correlated with the incidence of psychosis, it is likely to be comparably high.
3.1.3. Referrals and prescreening
Referrals are usually accepted by telephone, mail and fax and can be done by service user's friend, or relatives as well as health professionals. The diagnostic process at the OASIS team includes three steps:
prescreening;
screening assessment;
baseline assessment.
First, the individual referred is contacted by telephone to check the suitability of the referral (pre-screening). The OASIS team is continuously developing educational programmes in liaison with local health and non-health agencies who may encounter people potentially meeting the inclusion criteria. Mental health charities and voluntary organizations, local pastoral and educational services are also informed about the OASIS team. The concept of the potential prodrome or ARMS is unfamiliar to most health care professional such as primary care physicians (GP's), primary care counsellors, college and university counsellors, community mental health teams as well as child and adolescent services. Thus, the educational programme is continuously ongoing and includes informal meetings, presentations and distribution of information materials. Information is also posted on a website (http://www.slam.nhs.uk/our-services/oasis.aspx), and distributed in leaflets and newsletters. This training and educational effort has been effective, as the OASIS team to date has received a total of 1102 referrals (2001–2011, Fig. 3). Furthermore, the referral rate has increased over time, with 235 referrals received in the past year (4.52 referrals/week).
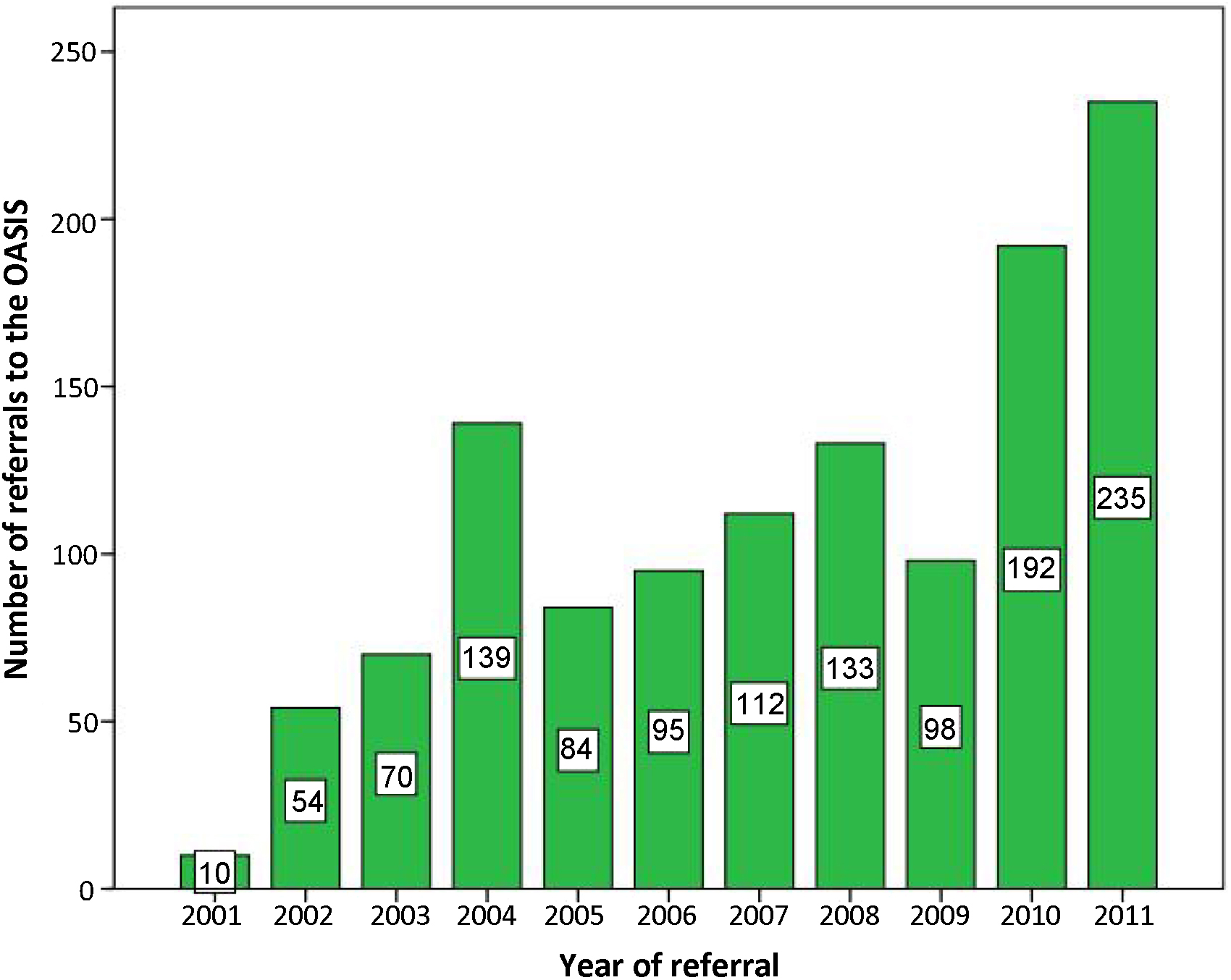
Fig. 3 Number of referrals (n = 1102) to the OASIS team over the past 10 years (2001–2011).
Most of the OASIS referrals (28%) came from GPs, followed by community mental health services or child and adolescent services (18%) and first-episode services (16%)(Fig. 4). Only 11% were self-referrals while other referrers included emergency clinics, relatives or counsellors.
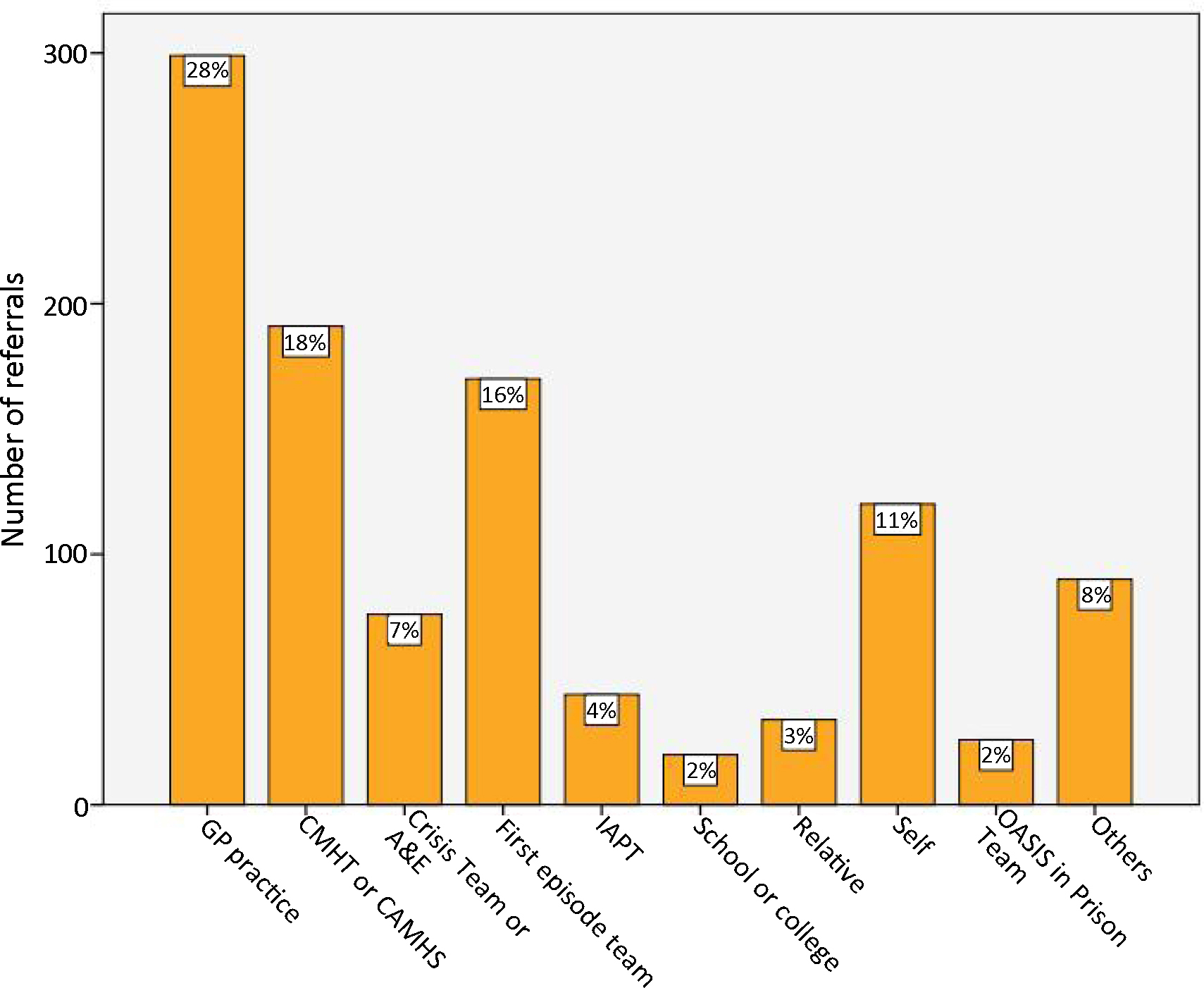
Fig. 4 Sources of referrals to the OASIS team (2001–2011, n = 1102). CMHT: Community Mental Health Teams; CAMHS: Community Adolescent Mental Health Services; IAPT: Improving Access to Psychological Therapies; A&E: Accident and Emergency services.
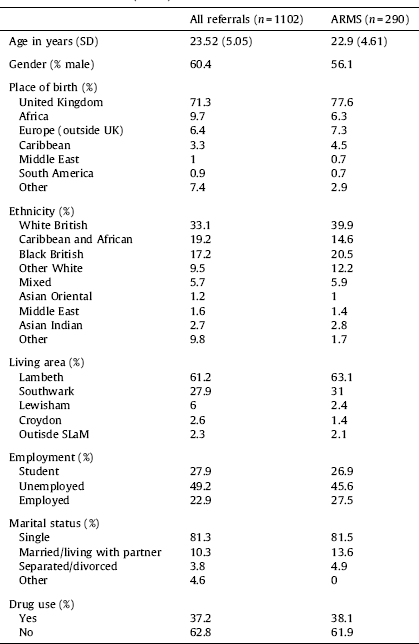
Overall, those referred were predominantly young (mean age 23.5, SD 5.5) males (60.4%). Most of them (71.3%) were born in UK and where from ethnic minorities (white British 33.1%). A substantial proportion of clients was born in African or Caribbean countries (19.2%). Given that OASIS was first set up in Lambeth, the majority of referrals came from this borough (61.2%). About half of the referred clients was unemployed (49.2%) and one third of them (37.2%) admitted using illicit drugs during the pre-screening assessment. The sociodemographic details of the whole cohort are presented in Table 1.
Table 1 Demographic characteristics of 2001–2011 OASIS referrals (column on the left). SLaM, South London and the Maudsley NHS Foundation Trust. The second column on the right shows the demographic characteristics of the subgroup of subjects who met At Risk Mental State (ARMS) after the OASIS assessment.
3.1.4. Screening and baseline assessments
The initial screening assessment is usually offered at the client's general practice, alternatively at the team base or their home, usually comprising one session. A psychiatrist and/or a clinical psychologist typically assess clients. The age range is of 14–35, consistent with that employed by the Personal Assessment and Crisis Evaluation (PACE) clinic in Melbourne [Reference Yung, Nelson, Stanford, Simmons, Cosgrave and Killackey80]. The assessment is performed through a clinical interview supported by the Comprehensive Assessment of the At Risk Mental State (CAARMS) [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell’Olio77], a semi structured interview designed to assess putative prodromal psychotic symptoms in help-seeking individuals. The scale has a total of 27 items, which can be clustered in seven subscales. The first four items on the CAARMS, which cover attenuated delusions, hallucinations, thought disorder and disorganised speech, are usually summed to give a total score for attenuated ‘positive’ psychotic symptoms and are used to assess the inclusion criteria for an ARMS during the screening assessment. If the client meets ARMS criteria and is taken on by the OASIS team, the remaining scales of the CAARMS are then completed during a subsequent baseline assessment. Since 2008 the OASIS team has been employing a revised and extended version of the CAARMS (CAARMS + COGDIS, see below), which includes additional items from the SPIA scale [Reference Schultze-Lutter, Addington, Ruhrmann and Klosterkötter61]. Level of functioning is evaluated with the Global Assessment of Functioning (GAF) scale [Reference Hall40] and by the Social and Occupational Functioning Assessment Scale (SOFAS) [Reference Goldman, Skodol and Lave38]. The baseline assessment is quite demanding in terms of time and usually takes up to two sessions to be completed (see below).
3.1.5. Inclusion high risk criteria
OASIS inclusion criteria apply to helpseeking subjects only and require the presence of one or more of the following subgroups:
attenuated psychotic symptoms (APS). The APS criterion identifies young people at risk of psychosis due to a subthreshold psychotic syndrome. That is, they have symptoms which do not reach threshold levels for psychosis due to subthreshold intensity (the symptoms are not severe enough) or they have psychotics symptoms but at a subthreshold frequency (the symptoms do not occur often enough);
brief limited intermittent psychotic episode (BLIP), defined as the presence of a psychotic episode of less than seven days which remits spontaneously with no medication or hospitalization;
a trait vulnerability plus a marked decline in psychosocial functioning (Genetic Risk and Deterioration Syndrome [GRD]). The GRD criterion identifies young people at risk of psychosis due to the combination of a trait risk factor and a significant deterioration in mental state and/or functioning: family history of psychosis in first degree relative or schizotypal personality disorder in identified patient;
the fourth group is the cognitive perceptive basic symptoms (BS) group (since 2008). The BS criterion identifies at risk persons on the basis of subtle cognitive and perceptive alterations. Basic symptoms are subjective disturbances of thought processing, language and attention that are distinct from classical psychotic symptoms, in that they are independent of abnormal thought content [Reference Schultze-Lutter60]. Basic symptoms were originally assessed using the Bonn Scale for the Assessment of Basic Symptoms (BSABS) [Reference Klosterkötter, Huber, Wieneke, Steinmeyer and Schultze-Lutter47] and, more recently, the Schizophrenia Proneness Instrument, Adult Version (SPI-A), which allows a frequency-based severity rating of basic symptoms. These instruments inventory focus on self-perceived cognitive and perceptual changes, ultimately clustered in two partially overlapping subsets relating to the COPER (ten cognitive-perceptive basic symptoms) and the COGDIS criteria (the nine cognitive basic symptoms that are the most predictive of later psychosis) [Reference Schultze-Lutter, Klosterkötter, Picker, Steinmeyer and Ruhrmann62]. The revised version of the CAARMS employed at the OASIS includes these 9-COGDIS items from the SPIA scale: Inability to divide attention (A.8.4) from the Cognitive-Attentional Impediments (B, ATTENT) subscale; thought interference (C.1.1), blockages (C.1.4), disturbance of receptive (C.1.6) and expressive (C.1.7.) speech from the Cognitive Disturbances (C, COGNIT) subscale; thought pressure (C.1.3), unstable ideas of references (C.1.17), from the Disturbances in Experiencing the Self and Surroundings (D, SELF) subscale; disturbances of abstract thinking (C.1.16), captivation of attention by details of the visual fields (C.2.9) from the Optional (O) subscale. As indicated on the SPIA scale, severity score should be at least 3 for at least two basic symptoms in the past three months.
For all the four groups above here the additional requirement is that the symptoms should be present in the past year with a 30% drop in GAF score from premorbid level, sustained for a month and within the past 12 months or SOFAS score less than 50 for the past 12 months or more.
3.1.6. Exclusion criteria
OASIS exclusion criteria are:
history of frank psychotic episodes;
previous exposure to antipsychotic agents;
current substance dependence;
deficits in general intelligence (IQ < 70);
neurological disorders or any medical condition;
clients not help-seeking or withdrawing their willingness to be followed by the service;
age range outside than 14–35.
Inclusion and exclusion criteria are discussed in the clinical meeting with the team and a decision is made trough consensus.
3.1.7. Differential diagnosis
Of the 1102 referrals received from 2001 to 2011, 271 were not assessed because one of the following reasons: having been screened out due to living outside of the boroughs served by SLaM NHS Foundation Trust, being outside of the age range of the service, or the patient's refusal to undergo the assessment or recurrently failing to meet with the team. Among the 831 subjects who were assessed, 290 of them (35%) received a diagnosis of an ARMS (ARMS intake in 2011 was of 7 ARMS/month)(Fig. 5). Of interest, about 32% of the subjects who were referred because of putative prodromal symptoms were already frankly psychotic at the time of their referral to the team (Fig. 5). More importantly, almost all the subjects referred to the OASIS team met at least one diagnostic criteria for some psychiatric disorder. All subjects who did not meet ARMS criteria had at least an alternative psychiatric diagnosis (only in less than 4% there was no evidence of psychiatric disorders).
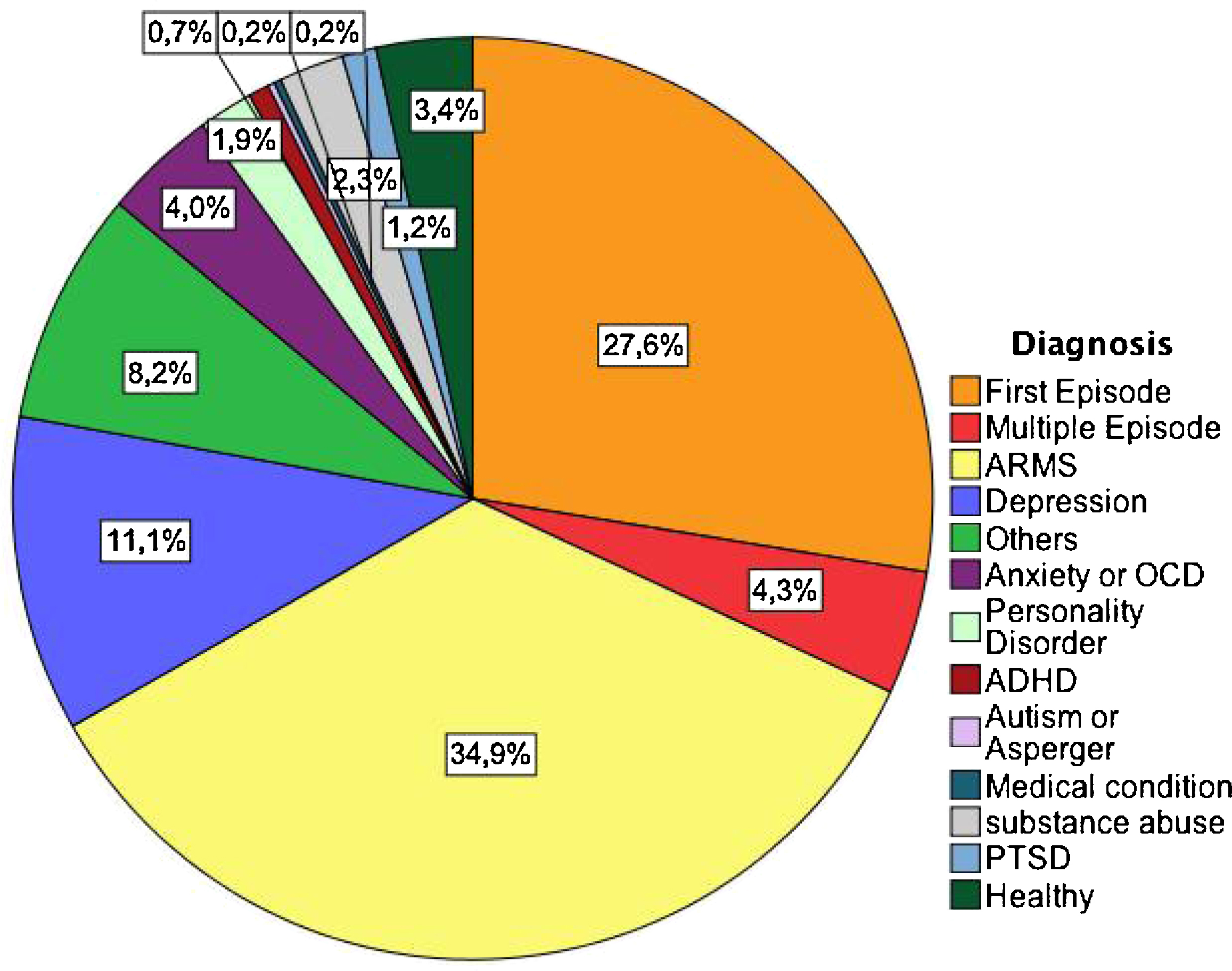
Fig. 5 Differential diagnoses of the 831 subjects who underwent the OASIS assessment between 2001–2011. ARMS: At Risk Mental State; OCD: Obsessive Compulsive Disorder; ADHD: Attention Deficit Hyperactivity Disorder; PTSD: Post-Traumatic Stress Disorder.
3.1.8. ARMS subgroups
Within the ARMS, the vast majority met the APS criterion (70%) followed by APS + GRD (11%) and BLIP (9%). The proportion of each soubgroup is depicted in Fig. 6, while the sociodemographic characteristics of the ARMS are detailed in Table 1.
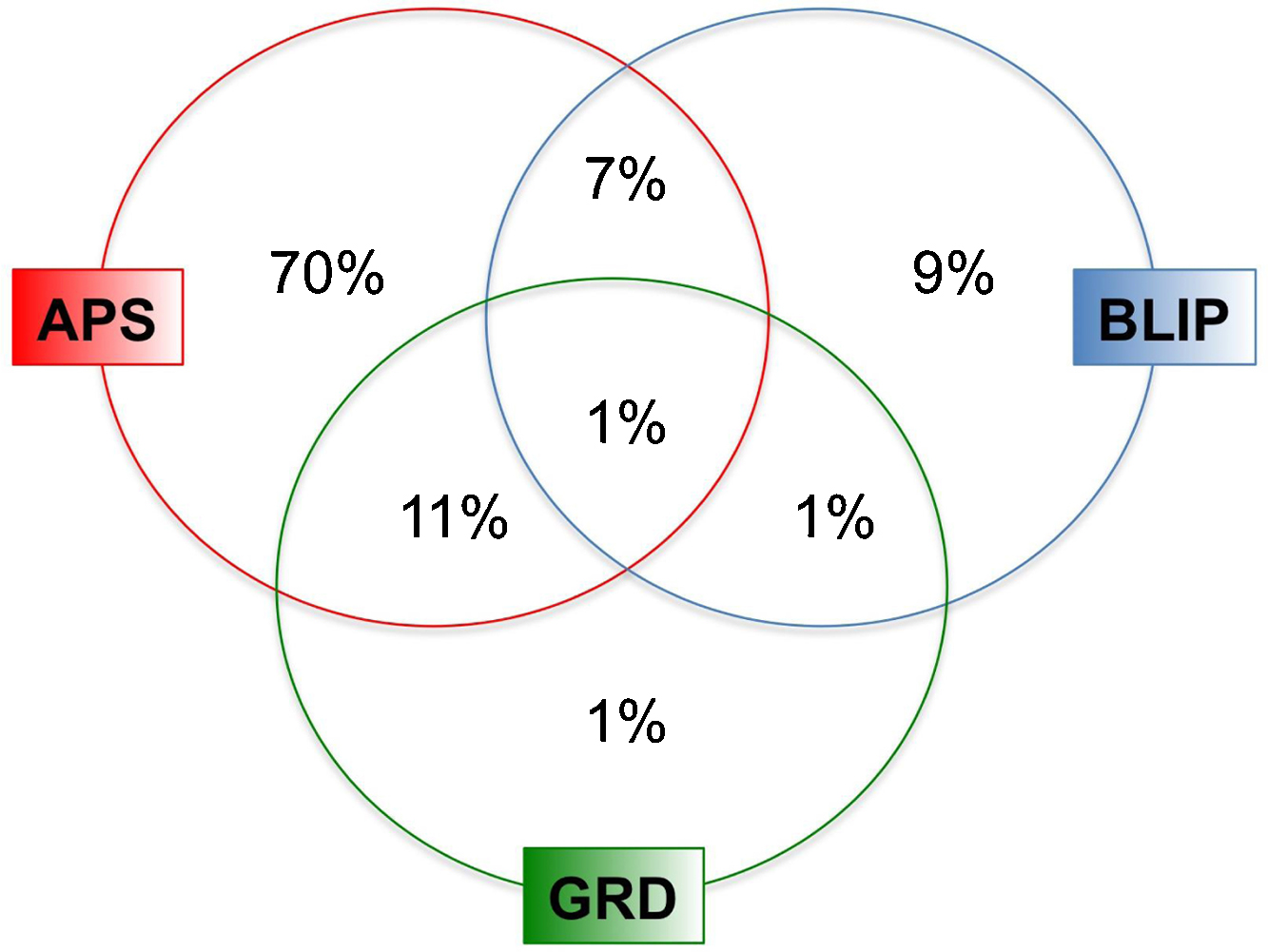
Fig. 6 ARMS subgroups in the OASIS team 2001–2011 (n = 290). The basic symptoms group is not represented as it was added only in the most recent years. APS: Attenuated Psychosis Syndrome; BLIP: Brief Limited Intermittent Psychotic Episode; GRD: Genetic and Deterioration Syndrome.
3.1.9. Pathways to care
Of the 290 ARMS clients, 28% was referred by the GPs, 11% was self-referred, 18% was referred by a community adult/adolescent mental health service, 16% was referred from a first-episode team and the remaining ones were was referred from counsellors, from the OASIS in prison team, or from other charity or voluntary agencies.
3.1.10. Social functioning
The experience of at risk symptoms per se is associated with a marked impairment in psychosocial functioning [Reference Velthorst, Nieman, Linszen, Becker, de Haan and Dingemans71], which appears as a core feature of the prodromal state [Reference Seidman, Giuliano, Meyer, Addington, Cadenhead and Cannon63]. Social impairment plays a significant role in the etiopathology of the disease onset and is an independent predictor of longitudinal outcome [Reference Fusar-Poli, Byrne, Valmaggia, Day, Tabraham and Johns29] being resistant to treatment, pharmacological and psychosocial [Reference Cornblatt, Carrión, Addington, Seidman, Walker and Cannon9]. It is also reflected by a considerably decreased subjective quality of life [58,5]. Clients of the OASIS team are more likely to live in communal establishments or at home with their parents than the local population [Reference Fusar-Poli, Byrne, Valmaggia, Day, Tabraham and Johns29]. The OASIS patients show also higher rates of unemployment than the general population [Reference Fusar-Poli, Byrne, Valmaggia, Day, Tabraham and Johns29].
3.1.11. Presenting symptoms and diagnostic comorbidities
In addition to APS symptoms, help-seeking people who meet criteria for ARMS usually present with other clinical concerns. Many have comorbid diagnoses, in particular anxiety, depression, and substance use disorders that are clinically debilitating [80,74]. High levels of negative symptoms, significant impairments in academic performance and occupational functioning, and difficulties with interpersonal relationships as well as substantially compromised subjective quality of life [Reference Bechdolf, Pukrop, Kohn, Tschinkel, Veith and Schultze-Lutter5] are often observed [1,80,71,49]. The diagnosis of comorbid conditions at the OASIS team is usually performed during the baseline assessment (Fig. 7). The SCID-1 and SCID-2 are used both to assess any co-morbid diagnoses. Quantitative measures of psychopathology are further obtained using the Hamilton Depression and Anxiety scale and the PANSS. Most of the ARMS had at least one comorbid diagnosis, mainly relating to anxiety and depressive domains, in line with recent evidence in high risk samples [Reference Fusar-Poli, Nelson, Valmaggia, Yung and McGuire22].
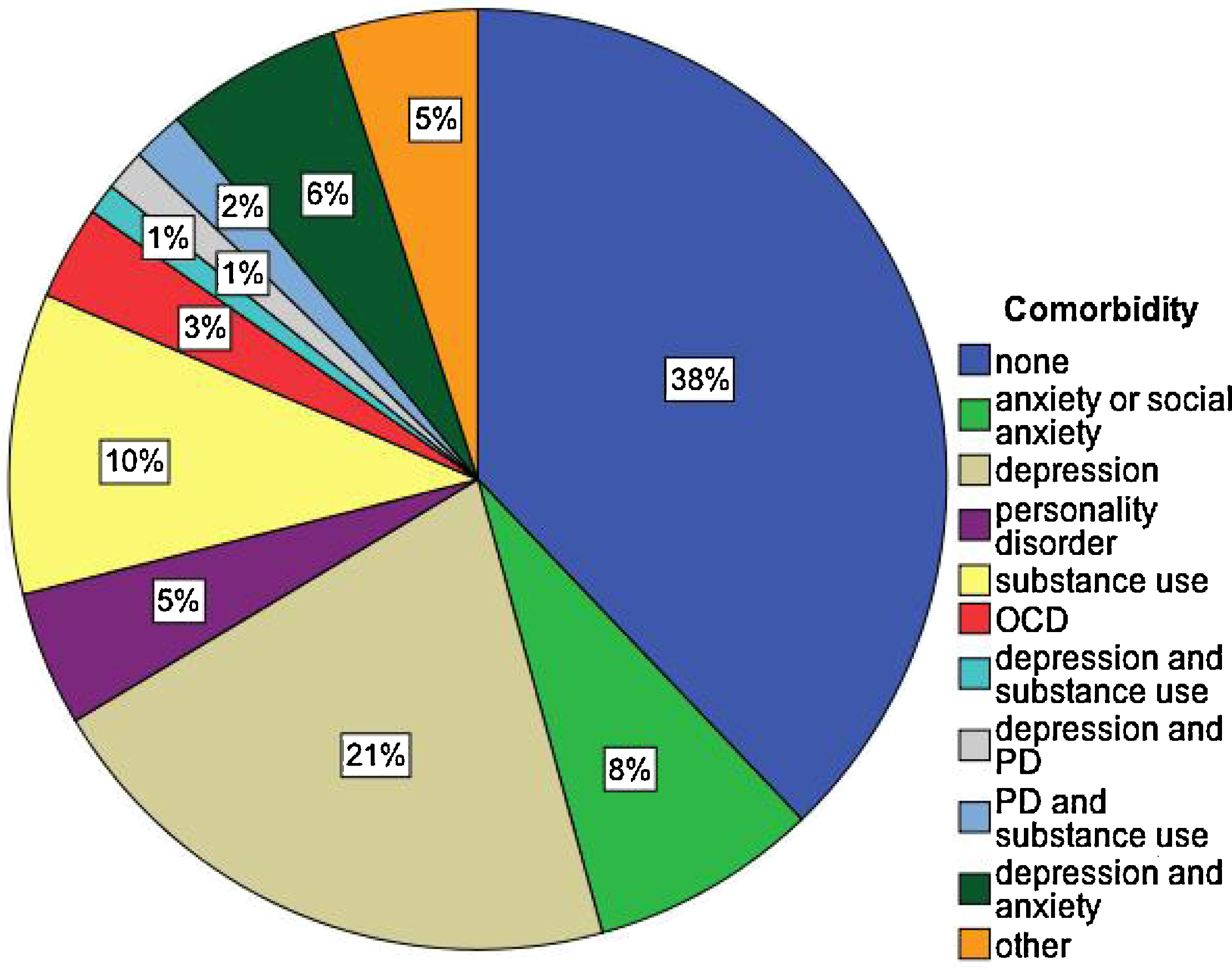
Fig. 7 Early intervention services in South London and Madusley (SLaM, Southwark, Lambeth, Lewisham, Croydon). In yellow prodromal teams, in orange first episode teams. OASIS: Outreach and Support in South London prodromal service; STEP: Southwark Team for Early Psychosis; LEIS: Lewisham Early Intervention Service; LEO: Lambeth Early Onset Psychosis; COAST: Croydon Outreach Assessment Support Team. The inpatient unit for first-episode psychotic patients is not represented
3.2. Treatment
3.2.1. Logistical demands
The overall screening assessment of the OASIS team is quite demanding. The initial screening assessment, taking place over a session of 2 hours, involves a psychiatrist and/or a clinical psychologist. The subsequent baseline assessment involves two sessions of two hours each to complete all the CAARMS subscales (2 hours), an assessment of life events and a neuropsychological assessment (2 hours). The OASIS service currently consists of one part-time consultant psychiatrist, two psychiatrists, three clinical psychologists, a team-leader, and a team administrator. Thanks to the integrated research programme, the team also benefits from a number of clinical research workers, clinical psychologist trainees and psychatrists in training. After the OASIS assessment (i.e. pre-screening, screening, baseline) the clients are taken on by the OASIS team for a period of two years at a frequency determined by their clinical needs. Assessment is repeated at one year and before discharge.
3.2.2. Case management
During the 2-year follow-up all the OASIS patients are offered case management. Clinicians in the OASIS service form supporting relationships with the patients, address distress, identify treatment targets such as anxiety, depression, sleep disturbance and substance abuse, provide a perspective for patient and family, and support the patient in social and role function [Reference McGlashan, Addington, Cannon, Heinimaa, McGorry and O’Brien51].
3.2.3. Focused interventions
In addition to case-management, all patients are usually offered a specific course of psychological interventions. The clinical psychologists at the OASIS team are trained to use cognitive behavioural therapy (CBT) and offer up to 24 sessions. Repeated psychometric measures and discussion with the clinical team are used to map the response to the treatment and the needs of the patients. Most of the OASIS clients (63%) did receive some CBT: as single first-line therapy (33%) or in co-therapy with antidepressants (11%) [Reference Fusar-Poli, Valmaggia and McGuire25] or antipsychotics (19%) [Reference O’Connor, Sota, Cortesi and Fusar-Poli56] (Table 2). Low-dosages antipsychotics, more frequently Quetiapine 25-200 mg are allowed when patients complained of persistent attenuated psychotic symptoms impacting their overall functioning and subjective quality of life.
Table 2 Focused interventions in the OASIS team (n = 290, 2001–2011).
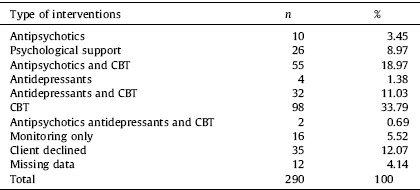
CBT: Cognitive Behavioural Therapy.
3.2.4. Transition outcomes
In general, there is an acceptance within the field that the definition of “psychosis” is somewhat arbitrary [Reference Yung, Nelson, Thompson and Wood81]. The intensity, frequency and duration of psychotic experiences in ARMS subjects appear to vary along continua, and defining transition involves making a quantitative distinction between a symptom severity that corresponds to one of two categories (psychosis and non-psychosis) [73,55]. The standard psychotic criteria are based on the DSM-III-IV or ICD-10 criteria for schizophrenia and other psychotic disorders. DSM defines brief psychotic disorder as an illness lasting from 1 day to 1 month, with an eventual return to the premorbid level of functioning. Under these criteria psychosis can be diagnosed if one psychotic symptom occurs for one day so this threshold is generally lower than the CAARMS, which have longer duration criteria [Reference Fusar-Poli and Van Os19]. The OASIS criteria used are based on the definition given by Yung et al, [Reference Yung, Phillips, McGorry, McFarlane, Francey and Harrigan75] the CAARMS criteria. The CAARMS criteria require the occurrence of at least one fully (positive) psychotic symptom (variably assessed on the hallucination scale, unusual thought content/suspiciousness scale, suspiciousness, conceptual disorganization scale) several times a week for over one week [Reference Yung, Phillips, Yuen, Francey, McFarlane and Hallgren76]. At the time of the writing of the present manuscript, of the 290 OASIS clients, 44 subjects (15.2%) developed a psychotic episode over the 2-year follow-up time (an ongoing research project is monitoring the transition outcomes of ARMS up to 10 years since their initial assessment). The last transition to psychosis was observed after 1242 days, while the mean time to transition was of 375 days (Fig. 8). The transition rates declined over the recent years and this phenomenon has already been observed in other established prodromal services [Reference Yung, Yuen, Berger, Francey, Hung and Nelson79]. Possible causes of the apparent decline in transition rate include:
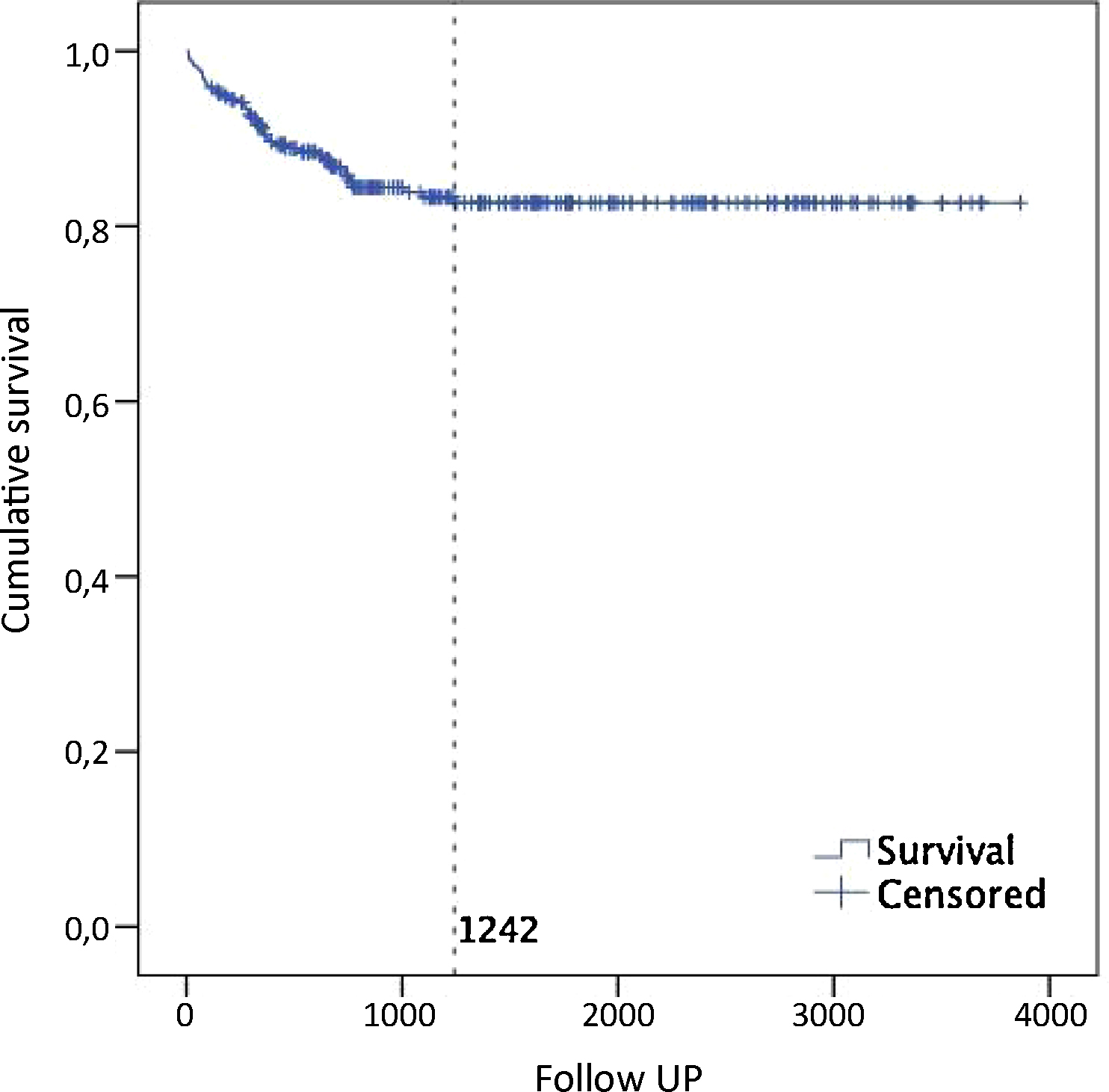
Fig. 8 Kaplan Meier survival estimate of transition to psychosis up to 10 years in 290 ARMS subjects. The last transition was observed after 1242 days (dotted line). The mean time to transition was of 375 days (CI95% from 280 days to 470 days, median 313 days).
treatment of high risk patients preventing or delaying the psychosis onset;
a lead time bias, that is, earlier detection resulting in transitions seemingly occuring later;
a dilution effect, that is more “false positives” who are not really at risk being referred to high risk services, possibly as a result of these services and their intake criteria becoming more well known [Reference Yung, Yuen, Berger, Francey, Hung and Nelson79].
Of all the clients with an ARMS, there were only few cases of serious self-harm but there were no completed suicides. The longitudinal outcomes of the OASIS patients and the clinical predictors of psychosis transition have been comprehensively addressed in separate papers [29,11].
3.2.5. Integration with first episode services
As mentioned above about a third (32%) of the individuals assessed by the OASIS team were already psychotic at the time of their initial assessment with the team. The OASIS team therefore was not only successful in identifying people with an ARMS but also in identifying people with a first episode of psychosis. Thanks to the close links with the local first episode teams these subjects were taken on by a few days minimizing the impact of untreated psychosis (DUP).
3.2.6. OASIS in prison
In the last two decades the UK government has encouraged for prisoners to receive the same range and quality of services as they would in the community. From 2009 onwards the OASIS team has been working in a local prison to develop a screening instrument for ARMS in a prison setting. This study established the need for an early intervention service in prison [Reference Jarrett, Craig, Parrott, Forrester, Winton-Brown and Maguire45]. In 2011 we received funding to roll-out the OASIS in Prison team which in parallel to the community OASIS team provides an intervention package aiming at the prevention of psychosis. Treatment starts in prison and prisoners are seen by the standard OASIS team upon release. If this innovative approach proves as beneficial as our pilot work suggests, it will lead to a fundamental reorganisation of mental health services in the prison setting with a bigger emphasis on prevention and early intervention.
3.2.7. Economic considerations
The economic impact of the OASIS team has been evaluated using a modelling approach. Based on the OASIS data we performed one of the first economic studies of an early detection service [Reference Valmaggia, McCrone, Knapp, Woolley, Broome and Tabraham69]. A decision model approach was applied to compare the costs associated with the OASIS team versus the cost of treatment as usual for people presenting with a first episode of psychosis without having had prior contact with specialized mental health services. The model was run for two years. During the first year, early detection was more expensive than care as usual as the OASIS patients were receiving care that would not be matched by care as usual. However, over the two years period the OASIS team produced significant savings mainly associated with the prevention of transition to psychosis and the benefits associated with a short duration of untreated psychosis [Reference Valmaggia, McCrone, Knapp, Woolley, Broome and Tabraham69]. A recent review of the economic impact of early detection and early intervention concluded that the data available for early detection is preliminary and that studies of the long term outcome of early detection and the associated potential economic are required [Reference Valmaggia, McGuire, Fusar-Poli, Howes and McCrone70]. This type of study is currently being carried out at the OASIS team.
3.3. Research at the OASIS team
3.3.1. Clinical Academic Groups (CAGs): advanced model for integrated research
Recently, the mental health services in South London and The Maudsley underwent a profound restructuring with the advent of the new Clinical Academic Groups (CAGs) for integrated research. Integrated research aims at coordinating research programmes (audits, students research) between the NHS and the Institute of Psychiatry (King's College London). In particular, the clinical-academic partnership has been developed to improve lasting legacy of a “research culture” within the clinical teams: feedback results to the teams to inform clinical practice, to inform service development, clinical decision making and foster innovation. Furthermore, an innovations “component” is developed within services/pathways, where new ideas and questions are welcomed, and turned into researchable projects. The aim of the new CAGs is also to obtain funds within the pathway to allow growth and implementation of innovations and ultimately to lead large-scale translational research projects that will shape clinical practice and health policy.
3.3.2. Neuroimaging in the ARMS
The OASIS team is closely linked to the Department of Psychosis Studies, Institute of Psychiatry, led by professor Philip McGuire. The OASIS-IoP team is one of the most active research groups in the field of neuroimaging studies of the pre-psychotic phases of psychoses. The Department of Psychosis currently hosts a number of national and international neuroimaging grants aimed at clarifying the neurobiological correlates of an impending risk of psychosis. A detailed discussion of the potentials and limits of imaging studies in the ARMS is out of the scope of the present paper. However, a large number of OASIS-IoP imaging studies has uncovered significant alterations in the structure [28,31,16], function [26,27,32,33], connectivity [Reference Crossley, Mechelli, Fusar-Poli, Broome, Matthiasson and Johns10] of the brain [Reference McGuire, Howes, Stone and Fusar-Poli52]. The OASIS-IoP research team has also been the first to show that the ARMS is associated with neurochemical alterations [34,30,35,18,20] of subcortical dopaminergic neurotransmission. The most important imaging studies performed at the OASIS team and published in the top impact-factor psychiatric journals are summarized in Table 3.
Table 3 Neuroimaging studies published by the OASIS-IoP team in the top impact-factor psychiatric journals (updated up to dec 2011).
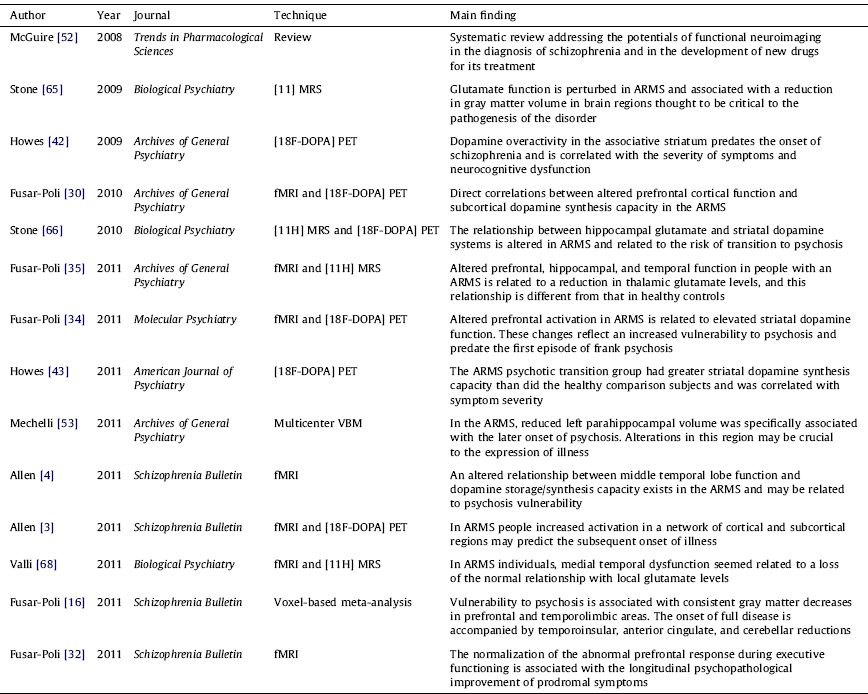
ARMS: At Risk Mental State; DOPA: Dopamine; MRS: Magnetic Spectroscopy; PET: Postitron Emission Tomography; VBM: Voxel Based Morphometry; fMRI: functional Magnetic Resonance Imaging.
3.3.3. Other research at the OASIS team
The OASIS researchers also investigated psychopathological dimensions in subjects with an ARMS using factor analysis and found that both the negative and the cognitive dimension scores were significantly associated with transition to psychosis during subsequent follow up [Reference Demjaha, Valmaggia, Stahl, Byrne and McGuire11]. In close collaboration with colleagues in Australia we have also recently submitted a paper which examines the structure of the ARMS using latent class analysis in a large sample (n = 315) and which found that ARMS who scored highest on all items of the CAARMS, had the lowest GAF score and were unemployed were also characterized by the highest transition rate to psychosis (Valmaggia et al. submitted to Psychological Medicine).
As the OASIS team only sees help-seeking individuals we explored the levels of illness insight in ARMS and found that is impaired [Reference Lappin, Morgan, Valmaggia, Broome, Woolley and Johns48]. In a further investigation we compared individuals who were referred to OASIS but either failed to attend for assessment (‘non-attenders’), or disengaged after assessment (‘disengagers’), with individuals who were engaged and managed by the service (‘help-seekers’). Over one fifth of those referred to services for people at high risk of psychosis do not attend or engage. However, many of this subjects require mental health care, and a substantial proportion has, or will later develop, psychosis. A more assertive approach to assess individuals who are at high risk of psychosis but fail to engage may be indicated [Reference Green, McGuire, Ashworth and Valmaggia39]. We also [Reference Fusar-Poli, Byrne, Valmaggia, Day, Tabraham and Johns29] studied the impairment in psychosocial functioning in the pre-psychotic phases showing that they play a significant role in the etiopathology of the disease onset. Compared with a demographically-matched general population, the ARMS were more likely to live in communal establishments or at home with their parents and had higher rates of unemployment. Baseline unemployment and living in a communal establishment were associated with an increased risk of developing a psychotic episode within the following two years.
4. Discussion
Despite the great burden of work undertaken over the past decade, the OASIS team is facing some crucial challenges. For example, there is recent concern across available literature for the putative “high number” of false positives who are not actually at risk of psychosis, with a declining transition risk observed over the recent years [Reference Yung, Nelson, Thompson and Wood82]. We feel these concerns are overstated. Comparatively, the predictive value of high risk diagnostic criteria should not be considered so low: the yearly conversion risk from mild cognitive impairment to dementia is 12% per year [Reference Fusar-Poli and Borgwardt24], and conversion from prediabetes to diabetes is about 11% per year [Reference Tabak, Herder, Rathmann, Brunner and Kivimaki67]. The biggest limitation is that the number of individuals in the community meeting ARMS criteria remains unknown [Reference Schimmelmann, Michel, Schaffner and Schultze-Lutter59] so the available instruments are not indicated for screening in the general population [Reference Yung, Stanford, Cosgrave, Killackey, Phillips and Nelson78]. Even less is known about the outcome among the group of ARMS subjects who do not convert to psychosis as a few studies only provided characteristics of those subjects who did not develop psychosis [Reference Simon, Velthorst, Nieman, Linszen, Umbricht and de Haan64]. At the psychopathological level, some discussion is emerging around the fact that the CAARMS transition criteria are too weighted towards positive psychotic symptoms [Reference Fusar-Poli and Borgwardt23]. As a result, the ARMS subjects who develop severe negative symptoms or functional impairments (but not severe positive symptoms) can still be categorized as not having made a transition [Reference Yung, Nelson, Thompson and Wood81]. Furthermore it is unclear whether the OASIS participants who will not develop any psychotic disorder will convert to another mental disorder. For example, there is new emerging evidence indicating that bipolar disorders are preceded by a prodromal phase with distinct psychopathological features [Reference Bechdolf, Nelson, Cotton, Chanen, Thompson and Kettle6]. Another recent study indicated that higher psychotic experiences significantly increased the risk of later hospitalization for psychiatric disorders other than schizophrenia spectrum disorders [Reference Werbeloff, Drukker, Dohrenwend, Levav, Yoffe and van Os72]. Consequently it is becoming clear than transition to psychosis versus clinical remission are only some of the possible outcomes, the others being persistence of ARMS symptoms and development of bipolar, depressive, personality or substance abuse disorders (Fig. 9).
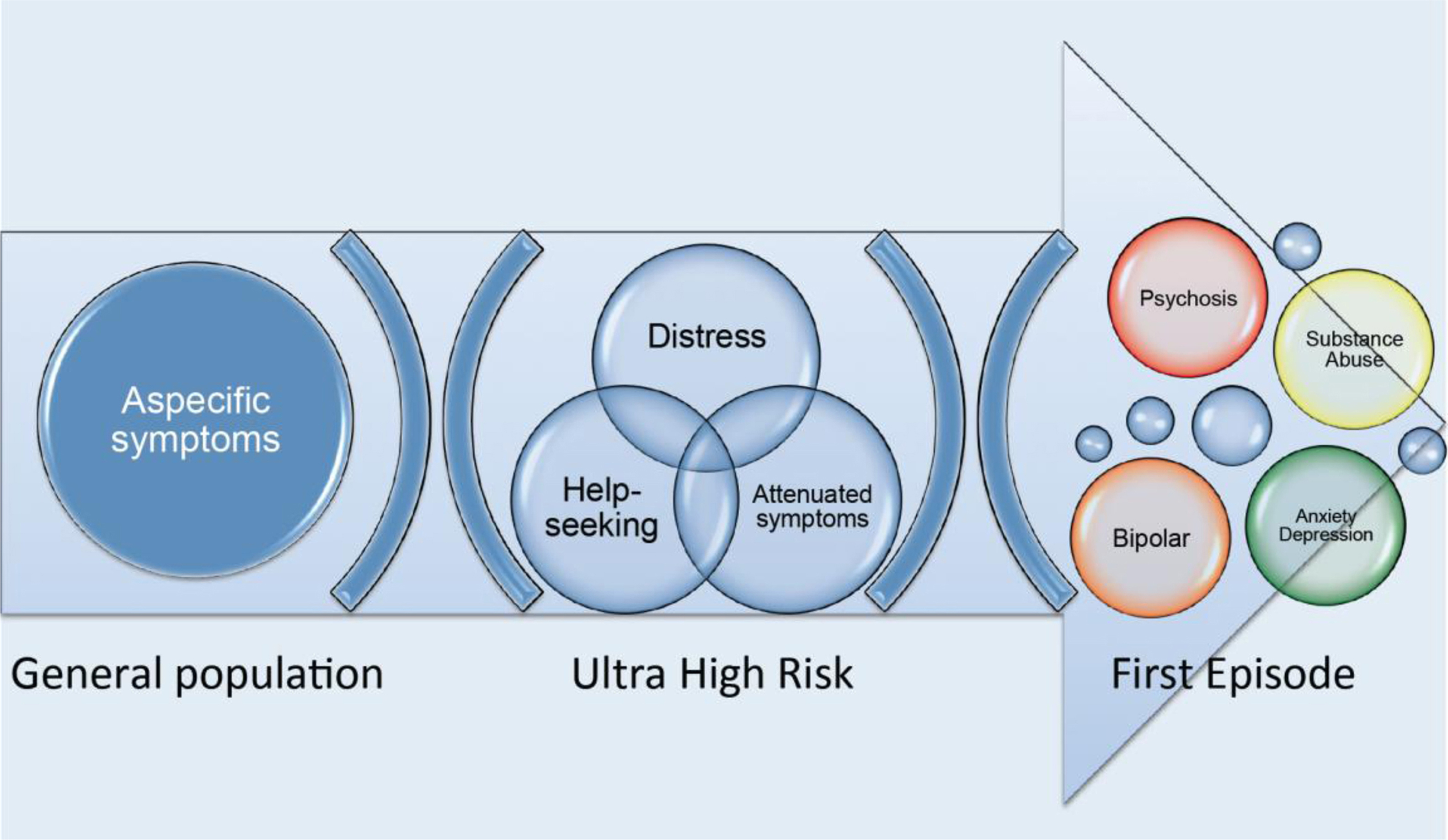
Fig. 9 Vulnerability to psychosis is present as a continuum in the general population as aspecific psychotic-like experiences. The clinical high risk state for psychosis is defined when distress and disability trigger help-seeking behaviours in presence of specific signs or symptoms (attenuated psychotic symptoms). The longitudinal course of the high risk state may include outcomes other than psychotic disorders such as the development of bipolar disorders, anxiety or depressive disorders, substance abuse or clinical remission.
At the level of treatments, there are no established interventions for reducing the ARMS symptoms or preventing psychosis and urgent large-scale research is needed. The specific concern is of unnecessary treatment [82,13], in particular with antipsychotics (which may have significant effects on the brain [26,41]). In the lack of any evidence based treatment, the safest approach is recommended (usually psychological interventions). On the other hand, future research is urgently required to better stratify the different levels of risks within the OASIS samples and thus tailor specific treatments accordingly. A number of exploratory studies are under progress to address the safety and efficacy of active interventions in this group of patients.
5. Conclusions
With more than one thousands referrals in a decade, the OASIS service represents one of the largest and most established prodromal psychosis services in the world. The burden of research evidence and the translational impact on the clinical practice support the OASIS as a leading model for the development of similar services worldwide.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
Our special thanks go to the staff and service users of OASIS. We acknowledge the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry King's College London; the Guy's and St Thomas’ Charitable Foundations; and the South London and Maudsly Charitable Trust for their financial support. Dr Valmaggia was supported by a NARSAD Young Investigator Award, by a Peggy Pollack Research Fellowship from the Psychiatry Research Trust.















Comments
No Comments have been published for this article.