Mental disorders are recognised as contributing significantly to disease burden throughout the world through morbidity rather than mortality (Reference Murray and LopezMurray & Lopez, 1997). In Australia 30% of the disability burden in 1996 has been attributed to mental disorders (Reference Mathers, Vos and StevensonMathers et al, 2000). Information on the global burden of mental disease has prompted calls for therapeutic packages consisting of counselling and pharmaceutical treatment as the main public health response (Reference UstunUstun, 1999). However, effective responses to morbidity and mortality in populations usually proceed from an understanding of causation, and then prevention, rather than relying on mass treatment. In this study we used the cross-sectional Australian National Survey of Mental Health and Wellbeing (Reference Henderson, Andrews and HallHenderson et al, 2000) to investigate associations between socio-economic status, mental disorders and suicide attempts. This study also examines results in terms of social causation and selection models of mental disorders and attempted suicide.
METHOD
Data
The National Survey of Mental Health and Wellbeing unit record data (n=10 641) were obtained from the Australian Bureau of Statistics. This nationally representative survey was conducted in 1997 and sought information on psychiatric disorders, cognitive impairment, common psychological problems, disablement due to mental disorder, and health service use (Reference Henderson, Andrews and HallHenderson et al, 2000). National prevalences of various mental disorders can be estimated from the survey using population weights derived by the Australian Bureau of Statistics (1999). The questionnaire included the computer-administered Composite International Diagnostic Interview, the 12-item General Health Questionnaire and the 12-item Short Form Health Survey, among other instruments (Reference Henderson, Andrews and HallHenderson et al, 2000).
Dependent variables for this study were mental disorders and suicide attempts. Mental disorders selected were substance use disorders, affective disorders and anxiety disorders as defined in ICD–10 (World Health Organization, 1992), derived from a standardised suite of responses to specific questions relating to the past year (ICD–10 codes for each disorder are given in the Appendix). Lifetime history of one or more suicide attempts was also examined as an outcome factor, and was elicited using the question ‘Have you ever attempted suicide?’ after asking the respondent about previous suicidal ideation. The National Survey was a stratified, multistage area sample of private dwellings. Post-stratification survey weights were assigned by the Bureau with each area, gender and age stratum equal to the inverse of the probability of selection for each stratum (Australian Bureau of Statistics, 1999). These person weights were used to calculate nationally representative prevalences, and were normalised (by dividing by the mean weight) to retain the original survey standard errors.
Socio-economic characteristics of survey respondents examined were education level, occupational status, income source and employment status. Demographic predictor variables considered as confounders or effect modifiers were gender, age, urban/rural residence and country of birth. Age groups were defined as 20–29, 30–44, 45–64 and ≥65 years. Urban/rural residence (binary variable) was represented by metropolitan (capital city or other metropolitan centre) and non-metropolitan (all other areas). Country of birth groups as defined by the Australian Bureau of Statistics on the unit record file were ‘Australia’, ‘main English-speaking countries’ and ‘all other’. Both urban/rural residence and country of birth were included as categorical variables in analyses to adjust for potential confounding with socio-economic measures as demonstrated previously (Reference Taylor, Morrell and SlaytorTaylor et al, 1998; Reference Morrell, Taylor and SlaytorMorrell et al, 1999; Reference Andrews, Henderson and HallAndrews et al, 2001; Reference Page, Morrell and TaylorPage et al, 2002). Educational level was coded as an ordinal variable: ‘bachelor degree or higher’ (n=1505), ‘undergraduate diploma’ and ‘associate diploma’ (n=995), ‘skilled vocational qualification’ and ‘basic vocational qualification’ (n=2200) and ‘no higher qualification’ (n=4699). An ordinal occupational status variable (for those employed full- or part-time) was also defined as ‘managers and professionals’ (n=1937), ‘associate professionals, tradespersons, and advanced clerical and service workers’ (n=1865), ‘intermediate clerical, sales, service, production and transport workers' (n=1506) and ‘elementary clerical, sales and service workers, labourers and related workers’ (n=962). A combined education/occupation variable was also created for the employed (n=6270). This was calculated by addition of the categorical education level and occupational status scores, resulting in a new seven-level socio-economic status variable.
Employment status – defined as ‘employed’ (n=6270), ‘unemployed’ (n=328) and ‘not in the labour forc’ (n=2805) – was also examined. Employed persons were those who reported that they had worked in a job in the preceding week; unemployed persons were those who were not employed in the previous week but were actively looking for work. Income source was also examined as a binary variable, as either ‘government benefit’ (n=2794) or ‘all other sources of income’ (n=6606). Analyses of occupation, income source, employment status and the combined socio-economic status variable were restricted to respondents of working age (20–64 years).
Analysis
Mental health variables and suicide attempts were examined by socio-economic status (SES) adjusting for demographic variables – age group, country of birth and urban/rural residence using logistic regression:
where p is the probability of having a mental disorder (substance use, affective, anxiety) or suicide attempt, β 1–β4 are regression coefficients for predictor variables (β1, age group; β2, urban/rural residence; β3, country of birth; β 4, SES variable) and k is the constant. Age group, urban/rural residence and country of birth were specified categorically. Analyses were completed separately for men and women.
Adjusted odds ratios from the regression models for levels of each socio-economic status variable were then applied to the unadjusted mental disorder prevalences in the referent group of that variable to produce adjusted prevalences in the comparison groups. Socio-economic status was also entered into the equation as an ordinal (continuous) variable to determine linear trend. From these equations the predicted OR in the lowest socio-economic group, as a ratio to the predicted OR in the highest group, was calculated as a relative index of inequality (Reference Kunst and MackenbachKunst & Mackenbach, 1995).
Probability of a suicide attempt (over a lifetime) was also examined by socio-economic status adjusting for demographic variables and mental disorders, in order to assess the degree to which the socio-economic status variation in suicidal attempts may be explained by mental disorders:
where p is the probability of a lifetime suicide attempt, β 1–β3 are regression coefficients for demographic variables (as above), β4 the coefficient for measures of socio-economic status, β5–β7 coefficients for mental disorders (β5, substance misuse; β 6, affective disorder; β7, anxiety disorder) and k is the constant. Linear trends in the relative index of inequality were calculated as above. In the case of male suicide attempts a curvilinear relationship was apparent. A series of curvilinear models were specified and assessed using goodness-of-fit statistics. An exponential model of the general form y=axb was the best fit to observed data, where a and b are constants, and y and x represent suicide attempts and socio-economic status respectively. PROC GENMOD in the SAS statistical package (version 8.02) was used to analyse and model the data.
RESULTS
A significant increasing linear trend from high to low educational level and occupational status (employed) was evident for substance use disorders (men only), affective disorders (men and women) and anxiety disorders (men and women) (Tables 1 and 2). Adjusting for age, urban/rural residence and country of birth did not significantly reduce the magnitude of these trends. Prevalence rates of affective and anxiety disorders were slightly higher in women than in men.
Table 1 Mental disorders and suicide attempts by education level

| Psychiatric disorder and adjusted variables | Prevalence, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Education level (men) | Education level (women) | |||||||||
| High1 (n=787) | 3 (n=548) | 2 (n=1375) | Low (n=2085) | P 2 | High1 (n=718) | 3 (n=447) | 2 (n=825) | Low (n=2614) | P 2 | |
| Substance use disorders | (n=73) | (n=45) | (n=144) | (n=255) | (n=36) | (n=17) | (n=42) | (n=102) | ||
| Age | 9.3 | 9.3 | 11.7 | 14.4** | <0.001 | 5.0 | 4.4 | 6.0 | 5.3 | 0.701 |
| Age, U/R, COB | 9.3 | 9.5 | 11.7 | 14.7** | <0.001 | 5.0 | 4.4 | 5.9 | 5.3 | 0.693 |
| Affective disorders | (n=20) | (n=14) | (n=64) | (n=98) | (n=32) | (n=32) | (n=56) | (n=224) | ||
| Age | 2.5 | 2.7 | 5.2** | 5.6** | <0.001 | 4.5 | 8.4* | 7.7* | 11.1*** | <0.001 |
| Age, U/R, COB | 2.5 | 2.7 | 5.0** | 5.4** | <0.001 | 4.5 | 8.4* | 7.8* | 11.1*** | <0.001 |
| Anxiety disorders | (n=43) | (n=34) | (n=116) | (n=149) | (n=55) | (n=44) | (n=128) | (n=348) | ||
| Age | 5.4 | 6.5 | 9.1** | 7.8* | 0.034 | 7.7 | 10.8 | 18.1*** | 16.5*** | <0.001 |
| Age, U/R, COB | 5.4 | 6.5 | 9.2** | 7.9* | 0.032 | 7.7 | 10.8 | 18.2*** | 16.5*** | <0.001 |
| Suicide attempts3 | (n=14) | (n=6) | (n=27) | (n=55) | (n=22) | (n=10) | (n=37) | (n=97) | ||
| Age | 1.7 | 1.2 | 2.1 | 2.9 | 0.028 | 3.1 | 2.2 | 4.8 | 4.3 | 0.070 |
| Age, U/R, COB | 1.7 | 1.3 | 2.2 | 3.0 | 0.018 | 3.1 | 2.2 | 4.9 | 4.4 | 0.059 |
| Age, mental disorders | 1.7 | 1.2 | 1.8 | 2.5 | 0.102 | 3.1 | 2.1 | 4.1 | 3.6 | 0.330 |
| Age, U/R, COB, mental disorders | 1.7 | 1.2 | 1.9 | 2.6 | 0.071 | 3.1 | 2.1 | 4.2 | 3.7 | 0.280 |
Table 2 Mental disorders and suicide attempts by occupational status

| Psychiatric disorder and adjusted variables | Prevalence, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Occupational status (men)1 | Occupational status (women)1 | |||||||||
| High2 (n=1114) | 3 (n=1220) | 2 (n=751) | Low (n=457) | P 3 | High2 (n=824) | 3 (n=645) | 2 (n=755) | Low (n=506) | P 3 | |
| Substance use disorders | (n=83) | (n=165) | (n=91) | (n=63) | (n=37) | (n=35) | (n=40) | (n=25) | ||
| Age | 7.4 | 13.0*** | 11.8** | 12.0** | 0.006 | 4.5 | 5.5 | 5.2 | 5.0 | 0.715 |
| Age, U/R, COB | 7.4 | 13.1*** | 11.9** | 12.6** | 0.002 | 4.5 | 5.6 | 5.2 | 5.1 | 0.603 |
| Affective disorders | (n=39) | (n=44) | (n=32) | (n=16) | (n=46) | (n=50) | (n=59) | (n=48) | ||
| Age | 3.5 | 3.8 | 5.7* | 5.5 | 0.009 | 5.6 | 8.4* | 9.6** | 9.9** | <0.001 |
| Age, U/R, COB | 3.5 | 3.8 | 5.7* | 5.4 | 0.010 | 5.6 | 8.4* | 9.6** | 9.8** | <0.001 |
| Anxiety disorders | (n=67) | (n=82) | (n=44) | (n=37) | (n=63) | (n=74) | (n=97) | (n=84) | ||
| Age | 6.0 | 6.5 | 7.2 | 9.9** | 0.004 | 7.7 | 12.0** | 14.3*** | 16.9** | <0.001 |
| Age, U/R, COB | 6.0 | 6.5 | 7.2 | 9.9** | 0.004 | 7.7 | 12.0** | 14.3*** | 16.8*** | <0.001 |
| Suicide attempts4 | (n=14) | (n=21) | (n=19) | (n=14) | (n=20) | (n=19) | (n=22) | (n=25) | ||
| Age | 1.3 | 2.1 | 2.5* | 3.8*** | <0.001 | 2.5 | 2.4 | 3.2 | 4.6** | 0.002 |
| Age, U/R, COB | 1.3 | 2.1 | 2.5* | 4.0*** | 0.002 | 2.5 | 2.4 | 3.2 | 4.6** | 0.002 |
| Age, mental disorders | 1.3 | 1.9 | 2.2 | 3.1** | 0.004 | 2.5 | 2.1 | 2.8 | 4.0* | 0.017 |
| Age, U/R, COB, mental disorders | 1.3 | 1.9 | 2.3 | 3.4** | 0.002 | 2.5 | 2.1 | 2.8 | 4.0* | 0.015 |
Significant increasing trends from high to low occupational status (men and women) and educational level (men only) were evident for suicide attempts, after adjusting for age, and also after additionally adjusting for country of birth and urban/rural residence (Tables 1 and 2). A similar trend in psychiatric disorders and suicide attempts was evident for the combined education/occupation variable (employed), with increasing prevalences from high to low levels of this combined measure (Figs 1 and 2), except for substance use disorders in women. These data were adjusted for age, urban/rural residence and country of birth. Adjustment for psychiatric disorders reduced to a minor extent the linear trend in suicide attempts by occupational status and by the combined education/occupation variable (employed), in both men and women, and the trend remained statistically significant. A significant curvilinear trend for male suicide attempts for the combined education/occupation variable was evident. Adjustment for psychiatric disorders rendered the trend in suicide attempts by education level non-significant (Table 1), but the effect remained by occupational status (Table 2).

Fig. 1 Mental disorders by socio-economic status based on education and occupation level, in employed respondents aged 20-64 years: (a) men; (b) women. Data adjusted for age, urban/rural residence and country of birth. Odds ratios (OR) of low to high socio-economic status derived from linear regression coefficients; P values represent test for linear trend.
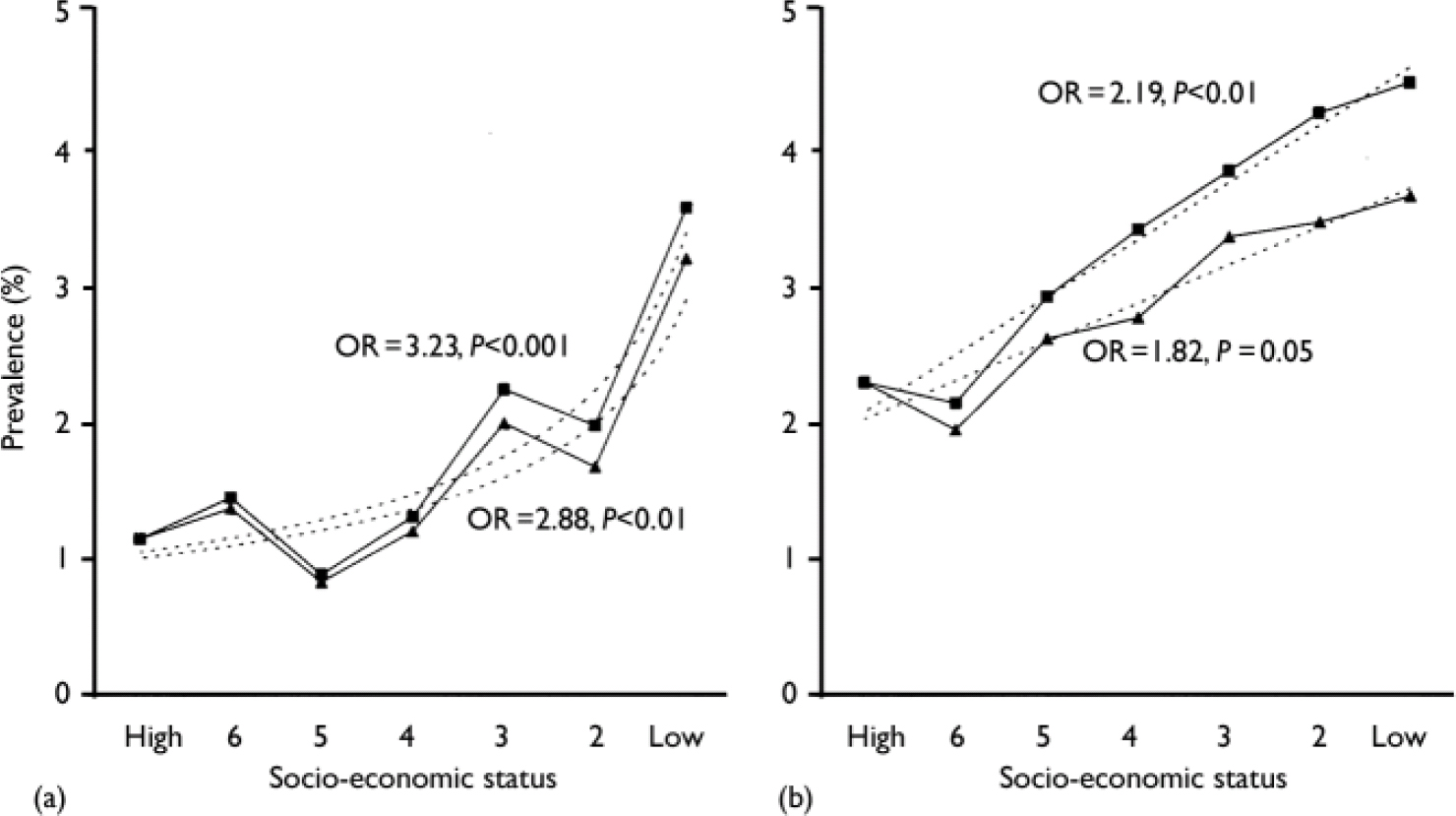
Fig. 2 Suicide attempts by socio-economic status based on education and occupation level, in employed respondents aged 20-64 years: (a) men, (b) women, adjusted for age (▪) and for age, urban/rural residence, country of birth and psychiatric disorder (▴). The curve fit for women is linear; that for men is of the form y=axb (adjusted for age, a=3.4, b=-0.6; adjusted for age, country of birth and urban/rural residence, a=2.9, b=-0.5). Odds ratios (OR) are of low to high socio-economic status derived from regression coefficients; P values represent test for trend.
In working-age respondents (20–64 years), significantly higher prevalences of psychiatric disorder and suicide attempts were evident in the unemployed and the ‘not in the labour force’ category compared with those employed (Table 3), and in those receiving government benefit compared with those with other sources of income (Table 4). These differences remained in models after adjusting for age, urban/rural residence and country of birth. The trends in suicide attempts across the categories were lessened but remained statistically significant when adjusted for having a psychiatric disorder, in addition to demographic variables.
Table 3. Mental disorder and suicide attempts by employment status

| Psychiatric disorder and adjusted variables | Prevalence, % | |||||||
|---|---|---|---|---|---|---|---|---|
| Employment status (men)1 | Employment status (women)1 | |||||||
| Unemployed (n=198) | Not in labour force (n=429) | Employed2 (n=3454) | P 3 | Unemployed (n=130) | Not in labour force (n=975) | Employed2 (n=2693) | P 3 | |
| Substance use disorders | (n=50) | (n=52) | (n=401) | (n=15) | (n=43) | (n=136) | ||
| Age | 26.4*** | 17.6* | 11.6 | <0.001 | 10.8** | 5.2 | 5.0 | 0.060 |
| Age, U/R, COB | 26.7*** | 17.9** | 11.6 | <0.001 | 11.1** | 5.3 | 5.0 | 0.046 |
| Affective disorders | (n=21) | (n=39) | (n=130) | (n=19) | (n=104) | (n=203) | ||
| Age | 12.3*** | 10.7*** | 3.8 | <0.001 | 14.6* | 11.9*** | 7.5 | <0.001 |
| Age, U/R, COB | 12.1*** | 10.6*** | 3.8 | <0.001 | 15.0** | 11.8*** | 7.5 | <0.001 |
| Anxiety disorders | (n=30) | (n=60) | (n=226) | (n=32) | (n=179) | (n=319) | ||
| Age | 16.3*** | 15.7*** | 6.5 | <0.001 | 28.7*** | 20.2*** | 11.8 | <0.001 |
| Age, U/R, COB | 16.3*** | 15.7*** | 6.5 | <0.001 | 28.8*** | 20.0*** | 11.8 | <0.001 |
| Suicide attempts4 | (n=13) | (n=15) | (n=68) | (n=12) | (n=57) | (n=86) | ||
| Age | 6.8*** | 4.1* | 2.0 | <0.001 | 10.1*** | 6.0*** | 3.2 | <0.001 |
| Age, U/R, COB | 6.9** | 4.2* | 2.0 | <0.001 | 10.2*** | 6.1*** | 3.1 | <0.001 |
| Age, mental disorders | 4.7** | 3.0 | 2.0 | 0.005 | 7.1* | 5.3** | 3.2 | 0.001 |
| Age, U/R, COB, mental disorders | 4.8 | 3.1 | 2.0 | 0.004 | 7.1* | 5.3** | 3.2 | 0.001 |
Table 4 Mental disorders and suicide attempts by income source

| Psychiatric disorder and adjusted variables | Income source (men)1 | Income source (women)1 | ||
|---|---|---|---|---|
| Government benefit (n=605) | Other source2 (n=3475) | Government benefit (n=1111) | Other source2 (n=2687) | |
| Substance use disorders | (n=116) | (n=386) | (n=74) | (n=119) |
| Age | 23.0*** | 11.1 | 7.1** | 4.4 |
| Age, U/R, COB | 23.8*** | 11.1 | 7.3** | 4.4 |
| Affective disorders | (n=59) | (n=131) | (n=137) | (n=188) |
| Age | 11.5*** | 3.8 | 13.6*** | 7.0 |
| Age, U/R, COB | 11.4*** | 3.8 | 13.5*** | 7.0 |
| Anxiety disorders | (n=86) | (n=230) | (n=228) | (n=302) |
| Age | 14.9*** | 6.6 | 23.0*** | 11.2 |
| Age, U/R, COB | 14.9*** | 6.6 | 22.9*** | 11.2 |
| Suicide attempts3 | (n=29) | (n=67) | (n=69) | (n=86) |
| Age | 5.2*** | 1.9 | 6.3*** | 3.2 |
| Age, U/R, COB | 5.5*** | 1.9 | 6.4*** | 3.2 |
| Age, mental disorders | 3.8** | 1.9 | 4.9* | 3.2 |
| Age, U/R, COB, mental disorders | 3.9** | 1.9 | 5.0* | 3.2 |
The odds ratio of attempted suicide was also significantly higher in those with a mental disorder compared with those without a mental disorder (Table 5). The magnitude of this effect was reduced, although not substantially, after adjustment for demographic factors and each selected socio-economic status variable.
Table 5 Odds ratios of suicide attempt with a mental disorder1

| Adjusted for | Men (n=102) | Women (n=166) | ||||
|---|---|---|---|---|---|---|
| Substance use disorder | Affective disorder | Anxiety disorder | Substance use disorder | Affective disorder | Anxiety disorder | |
| Age, COB, U/R | 3.94 | 5.16 | 6.49 | 5.81 | 5.10 | 5.58 |
| Education level, age, COB, U/R | 3.78 | 4.85 | 6.42 | 5.71 | 5.10 | 5.47 |
| Occupational level, age, COB, U/R | 3.78 | 4.85 | 6.17 | 5.87 | 5.05 | 5.42 |
| Income source, age, COB, U/R | 3.56 | 4.26 | 5.81 | 5.42 | 4.76 | 5.21 |
| Employment status, age, COB, U/R | 3.63 | 4.35 | 5.87 | 5.64 | 4.81 | 5.21 |
DISCUSSION
This study examined socio-economic status by 12-month prevalence of common psychiatric disorders (affective, anxiety and substance use disorders) and by lifetime suicide attempts, using individual measures of socio-economic status, as measured by the Australian National Survey of Mental Health and Wellbeing. Significantly increasing gradients in mental disorders by decreasing socio-economic status were found using educational attainment and occupational status (in the employed) for both men and women (age adjusted). These gradients remained after adjusting for demographic variables, with the exception of substance use disorders in women, in whom prevalence was low (relative to men) and little socio-economic gradient was evident. The socio-economic gradient in the prevalence of suicide attempts was statistically significant using occupational status measures in the employed, and remained significant after adjusting for both demographic variables and psychiatric disorders. A similar increasing gradient was found for the socio-economic measure combining both educational and occupational categories (employed). Government benefit as the main income source (v. income from other sources) and unemployed or ‘not in the labour force’ (v. employed) were associated with higher rates of mental disorders and suicide attempts, and these differentials were attenuated but not removed or rendered non-significant by adjustment for demographic variables and mental disorders.
Methodological issues
The socio-economic status gradients found for suicide attempts (after adjusting for mental disorders) could be influenced partly by measurement issues, since mental disorders over the past 12 months are an incomplete proxy for a lifetime (the reference period for suicide attempts), although this is unlikely to be systematically different across the groups being compared. As there is no a priori reason to expect differential underestimation by socio-economic status of lifetime mental disorder v. current mental disorder, it is unlikely that the status trends found would be affected by this. If mental disorders are considered as intermediary between socio-economic status and attempted suicide then they cannot be confounders, and should not be adjusted for in assessing the effects of status on suicide attempts. Also, comorbidity was not considered in the study; however, groups with comorbidity might have a higher risk of suicide attempt, in which case observed effects of single disorders are likely to be an underestimate of the effect of comorbidity.
Although the mental health survey was nationally representative, the instruments used to assess mental condition (defined in terms of ICD–10 categories) were clinical diagnostic questionnaires validated predominantly in clinical samples (Reference Robins, Wing and WittchenRobins et al, 1988; Reference WittchenWittchen, 1994; Reference Peters and AndrewsPeters & Andrews, 1995; Reference Andrews and PetersAndrews & Peters, 1998). The extent to which the known diagnostic efficacy of these instruments (i.e. sensitivity and specificity) in the clinical setting applies to the general population is not clear. However, in general, a diagnostic tool used in a clinical setting tends to be more sensitive and less specific when applied to the general population. The various prevalences of mental health items from the survey for the population strata reported here could conceivably be biased upwards, but the relative differences between strata would not necessarily be biased.
Reliability and validity estimates from studies examining the psychometric properties of the Composite International Diagnostic Interview, the main instrument of the National Survey, do not report subgroup analyses of demographic factors or socio-economic status (Reference Robins, Wing and WittchenRobins et al, 1988; Reference WittchenWittchen, 1994; Reference Peters and AndrewsPeters & Andrews, 1995; Reference Andrews and PetersAndrews & Peters, 1998). However, on face validity one might expect the more educated, higher socio-economic status respondents to be more forthcoming concerning questions on mental and emotional states, which would mean the socio-economic status mental disorder differentials are underestimated. This scenario is not likely as the odds ratios of attempted suicide by mental disability remained similar after adjusting for the various socio-economic measures (along with demographic variables).
Gender differences in reporting mental and emotional factors may also explain part of the higher prevalence of mental disorder and suicide attempt in women than in men. A number of studies have attributed higher self-reported levels of physical and psychiatric morbidity in women (but lower mortality) to socio-cultural factors associated with gender roles (Reference Gijsbers van Wijk, van Vliet and KolkGijsbers van Wijk et al, 1991; Reference Popay, Bartley and OwenPopay et al, 1993; Reference CourtenayCourtenay, 2000). Differential severity of mental disorder (rather than simply prevalence) by gender may also influence the results. Certainly, women showed a stronger association of substance use disorder with suicide attempts than men, and men tended to show stronger associations between suicide attempts and anxiety disorders than women, despite the higher prevalences of substance use disorder in men and anxiety disorder in women.
Social causation of mental disorder
Two common explanations for the relationship between illness and socio-economic status are first, that excess mental illness reflects social causation, in that social and economic circumstances determine the mental health outcome; and second, that the association reflects social selection, in that people who are mentally ill descend the social scale because of their illness (or if at the bottom of the scale, cannot rise) and their mental condition is produced by other factors. Both explanations have been suggested in relation to socio-economic status (Reference Dohrenwend, Levav and ShroutDohrenwend et al, 1992).
The use of cross-sectional data in our study limits conclusions as to whether social causation or selection is operating. However, by restricting many analyses to those in employment, people with severe mental disorder (which precludes working) are excluded. For social selection to be the dominant explanation of the relationships described here, mental health characteristics (or their precursors) would need to operate in a way that precisely graded employed respondents into the hierarchical educational and occupational categories analysed. Furthermore, for suicide attempts to be a consequence of mental disorders exclusively, which also led to socio-economic status stratification, the National Survey would have had to underestimate significantly the presence of mental disorder in groups of low socio-economic status (differentially), since adjustment for mental disorders did not eliminate the significantly higher prevalence of suicide attempts in lower-status groups compared with higher status groups.
The broad education and occupation categories used in this analysis as measures of socio-economic status are generally achieved in young adulthood for most respondents, and prior to the measured mental disorder (past 12 months), establishing an implicit sequence of socio-economic status preceding mental illness. On the other hand, current or recent mental illness could also be a proxy for prior mental disorder or antecedent mental conditions in childhood and adolescence which could have affected educational and occupational attainment. However, no major sociological theory or paradigm posits mental disorder as a major determinant of social position. Social class and status in Australia (as elsewhere) is generally accepted as deriving from formal education, occupational status and ownership and inheritance of productive wealth (Reference EncelEncel, 1970).
The more prominent effect of occupational status compared with education for suicide attempts may be because occupational status reflects to a greater extent the current material conditions of life (income and wealth, employment stability, job control) than does education. Greater effects of adjustment for mental disorders in logistic models of suicide attempts between employed and not employed, and government benefit v. other income sources, were found compared with adjusting for these effects in the analysis of occupational status in the employed. This suggests that some in the most disadvantaged categories (unemployed, receiving government benefit) are there because of mental illness; but this is not the whole story. The consistently higher prevalences of mental disorder and attempted suicide in the unemployed compared with those not in the labour force suggests the occurrence of additional or higher prevalences in those who are unemployed of factors associated with mental illness. Findings from a previous study of a cohort of Australian youth also support a social causation hypothesis, in that psychological disturbance was shown to increase in young people without psychological morbidity following a transition from employment to unemployment, and a corresponding decrease of psychological morbidity following a transition from unemployed to employed (Reference Morrell, Taylor and QuineMorrell et al, 1994).
Although international comparisons of depression show variations between low-income and high-income groups in developed countries (e.g. Finland, Germany, the Netherlands and the USA), in developing countries (e.g. Ethiopia and Zimbabwe) similar differentials in depression are also noted (World Health Organization, 2001).
It is unlikely that socio-economic differentials in mental disorder in such varying contexts are the result of a consistent selection process operating for mental health status, and more likely that they are the consequence of socio-economic circumstances of life. Particularly in developing countries, where deprivation in those of lower socio-economic status is more absolute than relative and where social mobility is limited, it is unlikely that the differential prevalence of depression by socio-economic status is due to social selection rather than social causation.
Mental disorders, attempted suicide and socio-economic status
Other Australian studies using data from the National Survey have examined employment status and educational level in relation to reported mental disorders and suicide attempts (Reference Pirkis, Burgess and DuntPirkis et al, 2000; Reference Andrews, Henderson and HallAndrews et al, 2001). Both these studies found higher prevalences of mental disorder (Reference Andrews, Henderson and HallAndrews et al, 2001) and suicide attempts (Reference Pirkis, Burgess and DuntPirkis et al, 2000) in lower v. higher socio-economic status groups using logistic models adjusting for age, marital status, ethnicity and urban/rural residence. However, age-adjusted and multivariate models considered such socio-demographic factors as confounders only, and did not consider mental disorders as intermediaries between socio-economic status and suicide attempts.
The results of this study are also consistent with other examinations of psychological disturbance and measures of socio-economic status, specifically employment and occupational status (Reference Weich and LewisWeich & Lewis, 1998). A consistent inverse relationship between socio-economic status and psychopathology has been noted, based on aggregate socio-economic indices and on individual measures of education, occupation, income level and employment status (Reference Kohn, Dohrenwend, Mirotznik and DohrenwendKohn et al, 1998). Significant socio-economic status trends have been found in conditions such as schizophrenia, anxiety disorders, antisocial personality disorders, depression (among women) and substance use (among men) (Reference Kohn, Dohrenwend, Mirotznik and DohrenwendKohn et al, 1998). Previous studies have also shown aggregate measures of low socio-economic status to be positively associated with suicide attempts (Reference Hawton, Harriss and HodderHawton et al, 2001), and studies using individual socio-economic measures have shown similar relationships of higher suicide attempts with lower income (Reference GoodmanGoodman, 1999), unemployment (Reference Ostamo, Lahelma and LonnqvistOstamo et al, 2001) and lower educational level (Reference Beautrais, Joyce and MulderBeautrais et al, 1998).
We conclude that the higher rates of mental disorder and suicide attempts in lower socio-economic status groups compared with higher-status groups in Australia is not explained by measurement bias or confounding, and is most likely to be a consequence of social causation in view of the magnitude, consistency and dose–response trends of the findings, and their sociological plausibility (analogous to ‘biological plausibility’ in epidemiological studies). The significant socio-economic status relationship with suicide attempts after adjusting for mental illness suggests a direct (independent) relationship between status and suicide attempts. This does not exclude some social selection effect of mental disorder into ‘unemployed’ and ‘government benefit’ categories, for example, but adjustment for mental disorder in our study only attenuated slightly the trend for higher suicide attempts in lower v. higher occupational categories in analyses restricted to those employed.
The implication of these findings is that mental disorder and suicide attempts are not just individual phenomena to be considered only within a paradigm that prescribes diagnosis and treatment as a response. Mental disorder (particularly depression) and suicide attempts are also a consequence of material life circumstances, and these circumstances are much more difficult to contend with for people at the lower end of the social spectrum. Beyond mental health services and pharmacotherapy, social and economic responses are needed to reduce relative disadvantage. Programmes enhancing perceived life prospects through improved employment opportunities and job security could have an effect on suicide attempts and mental antecedents just as much as – if not more than – improved mental health facilities. The trends in mental disorder and suicide attempts across socio-economic status categories found in this study indicate also that these phenomena are relevant to the middle classes as well as to the most disadvantaged – that is, to the majority of the population.
APPENDIX
ICD-10 codes used in defining prevalences of selected mental disorders
Substance use disorder
F10.1, F11.1, F12.1, F13.1, F15.1, F10.2, F11.2, F12.2, F13.2, F15.2.
Affective disorder
F30.0, F30.1, F30.2, F31, F32.0, F32.1, F32.2, F32.00, F32.01, F32.10, F32.11, F33.00, F33.01, F33.10, F33.11, F33.2, F34.1.
Anxiety disorder
F40.0, F40.00, F40.01, F40.1, F41.0, F41.00, F41.01, F41.1, F42.0, F42.1, F42.2, F43.1.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Mental disorders and suicide attempts are not merely individual phenomena to be considered within a paradigm that prescribes diagnosis and treatment as a response.
-
▪ Results suggest that lessening social and economic disparities would lower the prevalence of both mental disorders and suicide attempts.
-
▪ Substance use disorders were less prevalent in women than in men and showed little relationship with socio-economic status.
LIMITATIONS
-
▪ As the study design was cross-sectional, causal inferences between socio-economic factors, mental disorders and suicide attempts are limited and need to be considered in relation to the strength of associations, their likely temporal sequence and supporting evidence from longitudinal studies.
-
▪ As lifetime mental disorder prevalence was not surveyed, lifetime suicide attempt prevalence was related to 12-month prevalence of mental illness.
-
▪ Investigations of comorbid diagnoses were not undertaken.
Acknowledgement
This study was funded by the National Health and Medical Research Council, Project Grant 107322.










eLetters
No eLetters have been published for this article.