To the Editor—Tracking and monitoring antimicrobial prescribing, which includes documentation of the indication for use, is 1 of the 7 Core Elements of Antimicrobial Stewardship Programs set forth by the Centers for Disease Control and Prevention (CDC). 1 Requiring a question for indication in the computerized physician order entry (CPOE) allows for increased transparency and communication among patients and all members of the healthcare team; it also enhances mindful prescribing, medication safety, and understanding of antimicrobial use.Reference Schiff, Seoane-Vazquez and Wright 2 Thus, on September 20, 2016, a mandatory selection of antimicrobial indication as an empiric or pathogen-directed therapy or as a prophylaxis was implemented for all prescribers within the Cleveland Clinic Health System (CCHS), which comprises an academic medical center, 8 community hospitals in Northeast Ohio, and 1 community hospital in Florida. Given the role of antimicrobial indication as a measurement of prescribing patterns and a guide for future stewardship activities, validation is important and necessary to ensure accurate selection of indications by the end users of the electronic medical record (EMR). We sought to describe the accuracy of prescriber-entered antimicrobial indications at CCHS and to describe the prevalence of indications for antimicrobial use on both a health-system and hospital levels.
Through retrospective chart review, data were collected to validate indications of non–order-set antimicrobials administered to patients over a 24-hour period on October 19, 2016, and to describe the prevalence of indications for antimicrobial use over a 1-month period in October 2016. Antimicrobials in order sets had preselected indications in the EMR. Empiric indications consisted of orders to treat possible infection syndrome with unknown pathogen, pathogen-directed indications for treatment of known infection and pathogen, and prophylaxis to prevent infection. The accuracy of prescriber-entered indications was evaluated using information in the EMR available to the prescriber at the time of order entry, including identification of a pathogen by in-house microbiology lab or as described in transfer records, if applicable, and review of physician progress notes describing an intention to prescribe the antimicrobial for prevention of an infection.
Between October 1 and October 31, a total of 39,312 antimicrobials were ordered at CCHS: 20,843 for empiric therapy (53%), 12,338 as prophylaxis (31%), and 6,131 for pathogen-directed therapy (16%). On October 19, there were 899 non–order-set antimicrobial orders: 567 for empiric therapy (63%), 150 as prophylaxis (17%), and 182 as pathogen-directed therapy (20%). During this 24-hour validation period, prescriber-entered indications for antimicrobial orders were validated for 728 of 899 (81%) of all orders, including for 87% of empiric, 91% of prophylaxis, and 52% of pathogen-directed indication. The largest discrepancy in the selection of indications was noted in pathogen-directed orders; 82 of 182 orders classified as pathogen-directed (45%) were validated as empiric therapy, according to the predetermined definitions. No significant difference in proportion of validated indications was detected among the academic medical center and community hospitals, with the exception of 2 outliers, for which the majority of discrepancies arose from antimicrobials ordered in the emergency department. When stratified by prescriber type, the proportion of validated indications was 82% for physicians (394 of 479), 80% pharmacists (69 of 86), and 78% advanced practice providers (166 of 212). The prevalence of indications varied by agent (Figure 1). A significant percentage of vancomycin and piperacillin/tazobactam was used empirically across CCHS as well as on a hospital-specific level.
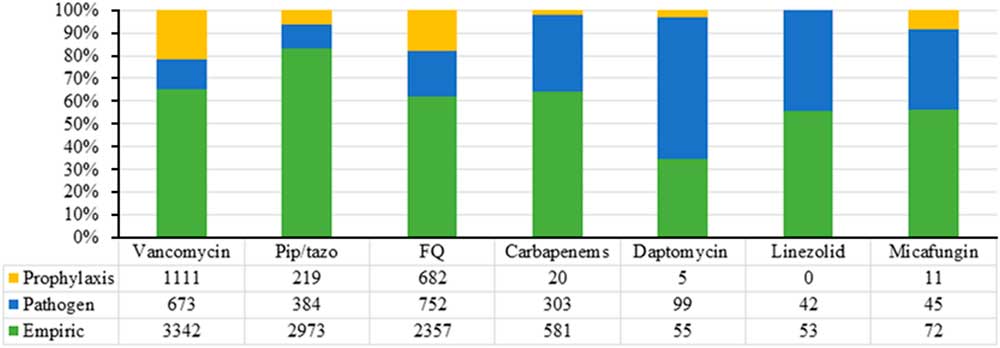
FIGURE 1 Prevalence of indications of selected antimicrobials across CCHS.
Validation is needed to reliably assess the impact of stewardship activities targeted to optimize antimicrobial use. The accuracy of prescriber-entered antimicrobial indications was evaluated previously in a retrospective study that analyzed a random sample of 50 orders, of which the indications of 100% of prophylaxis orders were accurate and the indications of 86% of treatment orders were accurate.Reference Patel, Esterly, Scheetz and Postelnick 3 Through an expanded sample size of 899 non–order-set antimicrobial orders from hospitals in the academic and community settings, we also found that most prescriber-entered indications were accurate and that accuracy was comparable among different prescriber types and hospital settings. Using antimicrobial order indications, we further characterized the epidemiology of antimicrobial prescribing within CCHS over 1 month, during which empiric antimicrobial use was the most prevalent, followed by prophylaxis and pathogen-directed, a trend consistent with national level data.Reference Kelesidis, Braykov and Uslan 4 Given its overall high accuracy, prescriber-entered antimicrobial indication for use will continue to be utilized as an important data point for the design, direction, and monitoring of future stewardship initiatives. Additional education on accurate documentation of indication will be provided at select facilities to ensure the quality and integrity of data used to track and monitor antimicrobial use.
ACKNOWLEDGMENTS
Financial support: No financial support was provided relevant to this article.
Potential conflicts of interest: All authors report no conflicts of interest relevant to this article.



