Two categories of treatment have been shown to be effective in treating panic disorder with or without agoraphobia. One is psychotherapy and the other is pharmacotherapy using antidepressants and benzodiazepines (American Psychiatric Association, 1998; Reference Nathan and GormanNathan & Gorman, 2002). However, it is uncertain whether combining these two forms of treatment confers any additional benefit over and above either treatment alone, both in the short term and in the long term. The primary objective of this systematic review was therefore to review and synthesise evidence from randomised controlled trials that examined the short- and long-term benefits and adverse effects of a combination of psychotherapy and antidepressants compared with either therapy alone for the treatment of panic disorder. A separate review that focuses on the use of psychotherapy in combination with benzodiazepines is in preparation.
METHOD
Inclusion criteria
Randomised controlled trials that compared a combination of psychotherapy and antidepressant pharmacotherapy with either treatment alone for adult patients with panic disorder, with or without agoraphobia, were eligible for inclusion.
We included both individual and group formats of behaviour therapy involving some kind of exposure, cognitive therapy involving some kind of cognitive restructuring, cognitive–behavioural therapy involving elements of both cognitive and behavioural therapy, and other psychological approaches. All commonly prescribed antidepressants were eligible, including tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs).
Studies in which there was irregular use of benzodiazepines or in which benzodiazepines were regularly administered at a constant dosage for long-term users were included, because it was considered that these did not undermine the comparability of the combined therapy with either monotherapy, and because such practices would reflect clinical reality more closely. The effect of this decision was examined in a sensitivity analysis. Studies in which benzodiazepines were combined with antidepressants as part of the study medication were excluded.
Identification of trials
We searched the Cochrane Collaboration Depression, Anxiety and Neurosis Controlled Trials Register (CCDANCTR) with the keywords ANTIDEPRESSANT and PANIC up to April 2003. The CCDANCTR is a study-based register of randomised trials that incorporates the results of group searches of Medline (from 1966), EMBASE (from 1980), CINAHL (from 1982), PsycINFO (from 1974), PSYNDEX (from 1977) and LILACS (from 1982 to 1999), and hand searches of major psychiatric and medical journals, conference proceedings and trial registers. Two additional searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and Medline were also undertaken. No language restrictions were imposed on the search.
Two reviewers examined the titles and abstracts of studies identified by the electronic search, and then checked the full articles for eligibility. To identify further trials, the references cited in these studies and in other review papers were also checked, relevant studies were subjected to SciSearch, and experts in the field were contacted.
Quality assessment and data extraction
Two independent reviewers assessed the methodological quality of the selected studies according to the recommendations of the Cochrane Reviewers’ Handbook 4.2.2 (Reference Alderson, Green and HigginsAlderson et al, 2004), which emphasises allocation concealment (A, low risk of bias; B, moderate risk of bias; C, high risk of bias). We also rated the study as ‘blinded’ when at least one outcome measure was assessed by an independent assessor who was masked to treatment allocation, and ‘unblinded’ when the outcomes were assessed by someone who was aware of the allocated treatment.
In addition, we rated the adequacy of the psychotherapy as ‘good’ when the way in which psychotherapy was actually conducted was examined by a third reviewer by means of audiotapes, etc., and as ‘poor’ when the authors only provided a description of the therapy procedure.
Two reviewers independently extracted data from the original reports using standardised data-extraction forms. Our primary outcome was ‘response’ – that is, substantial improvement from baseline, such as ‘very much or much improved’ according to the Clinical Global Impression scale (CGI; Reference GuyGuy, 1976), a decrease of more than 40% in the Panic Disorder Severity Scale score (Reference Shear, Brown and BarlowShear et al, 1997), and a reduction of more than 50% in panic frequency or the Fear Questionnaire – Agoraphobia sub-scale (Reference Marks and MathewsMarks & Mathews, 1979). Our secondary outcomes included global severity, frequency of panic attacks, phobic avoidance, general anxiety, depression, social dysfunction, patient satisfaction and cost-effectiveness. The total number of drop-outs for any reason was regarded as a proxy measure of the acceptability of treatment. Adverse effects were evaluated by examining the number of drop-outs due to adverse effects.
Any discrepancies were resolved by consensus between two or, where necessary, between all three reviewers. The decision to include in the meta-analysis studies that did not appropriately conceal allocation, that were ‘unblinded’ or that scored ‘poor’ with regard to adequacy of psychotherapy was examined in sensitivity analyses.
Data synthesis
Data were entered into Review Manager 4.2 (Windows software provided by the Cochrane Collaboration and available at http://www.cc-ims.net/RevMan) and double-checked for accuracy. For dichotomous outcomes, relative risk (RR) and 95% confidence intervals were calculated using a random-effects model, which yields superior results in terms of clinical interpretability and external generalisability compared with fixed-effects models and odds ratios or risk differences (Reference Furukawa, Guyatt and GriffithFurukawa et al, 2002). For continuous outcomes, the standardised weighted mean difference (SMD) and 95% confidence intervals were calculated using a random-effects model.
For dichotomous outcomes, we used intention-to-treat analyses according to the following principle. When data on drop-outs were carried forward and included in the efficacy evaluation using the last-observation-carried-forward method, they were included as such. When drop-outs were excluded from any assessment in the primary studies (e.g. those who never returned for assessment after randomisation), they were considered to be non-responders in both active and comparison groups. The same principles were applied to outcomes after the end of continuation treatment.
Subgroup and sensitivity analyses
To investigate clinical heterogeneity, we planned three a priori subgroup analyses: for types of psychotherapies; for classes of antidepressants; and for patients with or without agoraphobia. Statistical heterogeneity between studies was assessed with the I-squared statistic and the Q statistic. If significant heterogeneity was noted (I 2>30% or P<0.10) (Reference Higgins, Thompson and DeeksHiggins et al, 2003), sources were investigated.
In addition, sensitivity analyses were performed, restricting the data syntheses to studies of higher quality in terms of allocation concealment, blinding, operational diagnosis, adequacy of psychotherapy and control of benzodiazepine co-intervention. Meta-regressions (Reference Thompson and SharpThompson & Sharp, 1999) were also performed to determine whether these variables had a significant effect on the pooled effect sizes.
RESULTS
Description of studies
The electronic search identified 139 studies from CCDANCTR, an additional 164 studies from CENTRAL and 35 studies from Medline. By browsing their titles and abstracts, the two independent reviewers identified 135 articles as possible candidates, and full copies of these articles were obtained. Two independent reviewers then examined the strict eligibility of these papers. As a result of a further reference search, SciSearch and personal contacts, we identified 21 studies which satisfied the strict eligibility criteria. The interrater reliability of the eligibility criteria was found to be 94%. Because two trials provided two comparisons each (Reference Sheehan, Ballenger and JacobsenSheehan et al, 1980; Reference Mavissakalian and MichelsonMavissakalian & Michelson, 1986), there were 23 randomised comparisons involving a total of 1709 participants (Table 1) (a more detailed version of Table 1 is presented as a data supplement to the online version of this paper).
Table 1 Characteristics of the studies included in the review
| Study | Duration (weeks) | Acute-phase interventions | Continuation interventions (weeks) | Naturalistic follow-up | |
|---|---|---|---|---|---|
| Psychotherapy | Antidepressant | ||||
| Azhar (Reference Azhar2000) | 9 | Cognitive—behavioural therapy | Fluvoxamine | None | None |
| Barlow et al (Reference Barlow, Gorman and Shear2000) | 12 | Cognitive—behavioural therapy | Imipramine | 24 | At 6 months after treatment discontinuation |
| Berger et al (Reference Berger, Sachs and Amering2004) | 20 | Cognitive—interpersonal therapy | Paroxetine | None | At 24 weeks (i.e. at end of tapering) |
| de Beurs et al (Reference de Beurs, van Balkom and Lange1995) | 12 | Behavioural therapy | Fluvoxamine | None | At 24 months after trial termination |
| Fahy et al (Reference Fahy, O'Rourke and Brophy1992) | 6 | Cognitive—behavioural therapy | Clomipramine or lofepramine | None | None |
| Fava et al (Reference Fava, Savron and Zielezny1997) | 8 | Behavioural therapy | Imipramine | None | At 24 months after acute-phase treatment |
| Johnston et al (Reference Johnston, Troyer and Whitsett1995) | 17 | Behavioural therapy | Clomipramine | 12 | None |
| Kampman et al (Reference Kampman, Keijsers and Hoogduin2002) | 8 | Cognitive—behavioural therapy | Paroxetine | None | None |
| Loerch et al (Reference Loerch, Graf-Morgenstern and Hautzinger1999) | 8 | Cognitive—behavioural therapy | Moclobemide | None | At 6 months after treatment discontinuation |
| Marks et al (Reference Marks, Gray and Cohen1983) | 14 | Behavioural therapy | Imipramine | 14 | At 6 and 18 months after treatment discontinuation |
| Mavissakalian et al (Reference Mavissakalian, Michelson and Dealy1983) | 12 | Behavioural therapy | Imipramine | None | None |
| Mavissakalian & Michelson (Reference Mavissakalian and Michelson1986)1 | 12 | Behavioural therapy | Imipramine | None | At 6 and 24 months after acute-phase treatment |
| Mavissakalian & Michelson (Reference Mavissakalian and Michelson1986)2 | 12 | Behavioural therapy | Imipramine | None | At 6 and 24 months after acute-phase treatment |
| Oehrberg et al (Reference Oehrberg, Christiansen and Behnke1995) | 12 | Cognitive—behavioural therapy | Paroxetine | None | None |
| Sharp et al (Reference Sharp, Power and Simpson1996) | 12 | Cognitive—behavioural therapy | Fluvoxamine | None | At 6 months after treatment discontinuation |
| Sheehan et al (Reference Sheehan, Ballenger and Jacobsen1980)1 | 12 | Behavioural therapy | Imipramine | None | None |
| Sheehan et al (Reference Sheehan, Ballenger and Jacobsen1980)2 | 12 | Behavioural therapy | Phenelzine | None | None |
| Spinhoven et al (Reference Spinhoven, Onstein and Klinkhamer1996) | 6 | Cognitive—behavioural therapy | Trazodone | None | None |
| Stein et al (Reference Stein, Ron Norton and Walker2000) | 10 | Cognitive—behavioural therapy | Paroxetine | None | None |
| Telch et al (Reference Telch, Agras and Taylor1985) | 8 | Behavioural therapy | Imipramine | 18 | None |
| Wiborg & Dahl (Reference Wiborg and Dahl1996) | 12-15 | Psychodynamic psychotherapy | Clomipramine | 33-36 | At 9 months after treatment discontinuation |
| Zitrin et al (Reference Zitrin, Klein and Woerner1980) | 14 | Behavioural therapy | Imipramine | 12 | None |
| Zitrin et al (Reference Zitrin, Klein and Woerner1983) | 26 | Behavioural therapy | Imipramine | None | At 24 months after treatment discontinuation |
The majority of the participants were women, and their average age was between 30 and 40 years. They had suffered from panic disorder for 5 to 10 years. Only one comparison focused on patients with panic disorder without agoraphobia, whereas 13 comparisons focused on patients with panic disorder with agoraphobia. The other studies were of mixed populations.
The typical length of the acute-phase active treatment was between 8 and 12 weeks. In total, 12 studies administered behaviour therapy that consisted of exposure and/or breathing retraining and/or relaxation exercises. None of the studies used narrowly defined cognitive therapy that relied only on cognitive restructuring. Nine studies administered cognitive–behavioural therapy that consisted of both behaviour and cognitive therapy elements. Two studies were categorised as ‘Other psychotherapies’. One of these used a mixture of cognitive–behavioural therapy and interpersonal psychotherapy (Reference Berger, Sachs and AmeringBerger et al, 2004) and the other used brief psychodynamic psychotherapy (Reference Wiborg and DahlWiborg & Dahl, 1996). With regard to medications that were administered, 14 studies used TCAs (with an average dose of 146 mg/day of imipramine equivalents), 7 studies used SSRIs (average dose 32 mg/day fluoxetine equivalents) and 2 studies used monoamine oxidase inhibitors.
Response was defined in terms of the CGI scale in eight studies, in terms of the Fear Questionnaire Agoraphobia sub-scale in three studies, in terms of panic frequency in two studies, and in terms of other measures in 10 studies. In total, 13 studies reported continuous outcomes of global severity, 15 reported on panic frequency, 20 reported on agoraphobia, 18 reported on general anxiety, 18 reported on depression and 13 reported on social dysfunction. None of the studies reported on patient satisfaction or cost issues.
Six studies reported the results at the end of continuation treatment which lasted for between 3 and 9 months. Nine studies followed up the patients 6–24 months after termination of acute-phase and continuation treatments.
With regard to validity, all but four comparisons from three trials (Reference Mavissakalian and MichelsonMavissakalian & Michelson, 1986; Reference Wiborg and DahlWiborg & Dahl, 1996; Reference Berger, Sachs and AmeringBerger et al, 2004) scored B for allocation concealment. In total, 19 studies conducted blinded outcome assessments and four studies were unblinded (Reference Mavissakalian, Michelson and DealyMavissakalian et al, 1983; Reference Spinhoven, Onstein and KlinkhamerSpinhoven et al, 1996; Reference AzharAzhar, 2000; Reference Berger, Sachs and AmeringBerger et al, 2004). The interrater reliability of these two validity criteria was 94% for allocation concealment and 83% for outcome assessment.
Six studies reported that quality control of the psychotherapy was adequate (Reference Zitrin, Klein and WoernerZitrin et al, 1983; Reference de Beurs, van Balkom and Langede Beurs et al, 1995; Reference Fava, Savron and ZieleznyFava et al, 1997; Reference Loerch, Graf-Morgenstern and HautzingerLoerch et al, 1999; Reference Barlow, Gorman and ShearBarlow et al, 2000; Reference Kampman, Keijsers and HoogduinKampman et al, 2002). Four studies acknowledged financial support from pharmaceutical companies (Reference Fahy, O'Rourke and BrophyFahy et al, 1992; Reference de Beurs, van Balkom and Langede Beurs et al, 1995; Reference Sharp, Power and SimpsonSharp et al, 1996; Reference Loerch, Graf-Morgenstern and HautzingerLoerch et al, 1999), and these companies marketed the drugs involved in the trials. Oehrberg et al (Reference Oehrberg, Christiansen and Behnke1995) did not acknowledge financial support from a drug company, but three of the co-authors of that study were company employees.
Psychotherapy plus antidepressant v. antidepressant treatment
Acute-phase treatment
Combining data from 11 studies involving 322 patients in the psychotherapy plus antidepressant arm and 347 patients in the antidepressant arm showed that the combination was 1.24 times (95% CI 1.02–1.52) more likely to produce a response at the end of 2–4 months of acute-phase treatment compared with the antidepressant alone (Fig. 1). There was moderate but statistically significant heterogeneity (P= 0.05, I 2=44.9%). Furthermore, the funnel plot indicated that there was some publication bias, with one small study reporting an extreme result (Reference Telch, Agras and TaylorTelch et al, 1985). Subgroup analyses suggested that there was greater heterogeneity in the ‘other psychotherapies’ category (Reference Wiborg and DahlWiborg & Dahl, 1996; Reference Berger, Sachs and AmeringBerger et al, 2004). When we omitted these studies, limiting the included studies to those that employed behavioural or cognitive–behavioural therapies, the RR remained the same (RR=1.28, 95% CI 1.08–1.52) and there was no longer statistical heterogeneity (P=0.18, I 2=30.5%) or funnel-plot asymmetry.
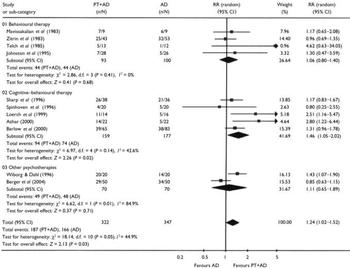
Fig. 1 Psychotherapy plus antidepressant v. antidepressant alone: response at the end of acute-phase treatment. PT, psychotherapy; AD, antidepressant; RR, relative risk.
The superiority of the combination therapy was corroborated by secondary analyses using continuous data. The combination treatment decreased the global severity of the disorder (SMD=–0.36, 95% CI 70.60 to –0.11), depression (SMD=–0.52, 95% CI –0.76 to –0.28) and social dysfunction (SMD=–0.47, 95% CI –0.89 to –0.05).
There were no differences in overall drop-outs or in drop-outs due to side-effects.
Continuation treatment
There was considerable statistical heterogeneity (P=0.005, I 2=76.8%). Limiting the studies to behaviour and cognitive–behavioural therapies removed this heterogeneity (P=0.55, I 2=0%) and suggested that the combination therapy was 1.63 (95% CI 1.21–2.19) times more likely to produce a response than antidepressant treatment alone.
After termination of treatment
Figure 2 shows the findings of five studies that reported outcomes after 6–24 months of naturalistic follow-up. Combining outcomes based on 376 participants, the combination therapy was still superior to antidepressant treatment alone (RR=1.61, 95% CI 1.23–2.11). No heterogeneity was noted (P=0.50, I 2=0%).
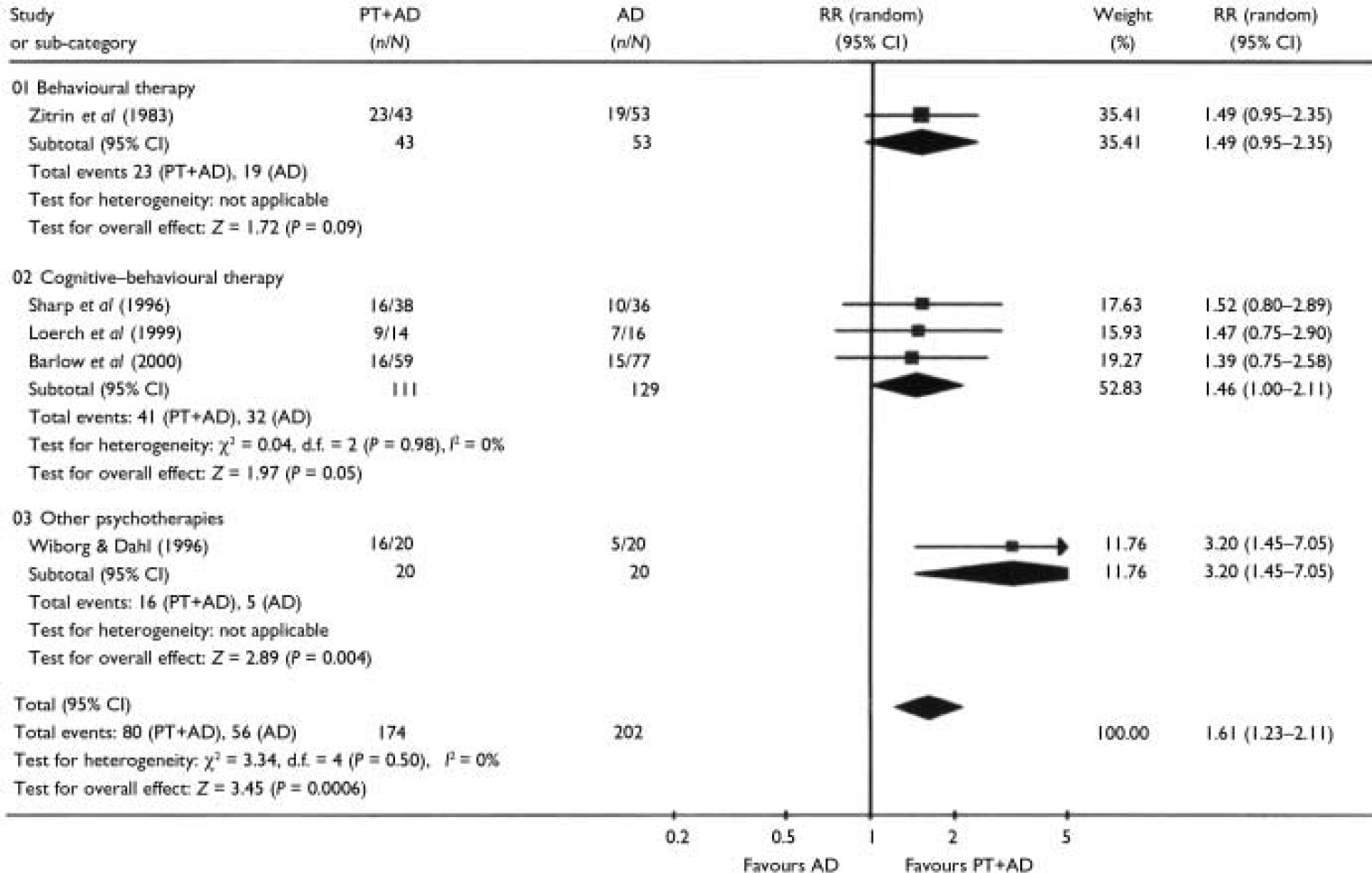
Fig. 2 Psychotherapy plus antidepressant v. antidepressant alone: response after termination of treatment. PT, psychotherapy; AD, antidepressant; RR, relative risk.
Psychotherapy plus antidepressant v. psychotherapy
Although the comparison of psychotherapy plus antidepressant with psychotherapy alone is theoretically different from the comparison of psychotherapy plus antidepressant with psychotherapy plus placebo (Reference Hollon and DeRubeisHollon & DeRubeis, 1981), our meta-analytical summaries were remarkably similar for the acute phase and follow-up evaluations. We therefore report here the aggregated results of trials comparing psychotherapy plus antidepressant with psychotherapy alone and psychotherapy plus placebo.
Acute-phase treatment
Combining data from 19 comparisons involving 592 patients in the psychotherapy plus antidepressant arm and 665 patients in the psychotherapy arm demonstrated that the combination was 1.16 times (95% CI 1.03–1.30) more likely to produce a response at the end of acute-phase treatment than psychotherapy alone (Fig. 3). The test for heterogeneity was not significant.

Fig. 3 Psychotherapy plus antidepressant v. psychotherapy alone: response at the end of acute-phase treatment. PT, psychotherapy; AD; antidepressant; RR, relative risk. 1. Comparison A of two from this study; 2. comparison B of two from this study.
The same superiority of the combined therapy was noted with regard to the global severity (SMD=–0.43, 95% CI –0.60 to –0.26). When different aspects of panic disorder were examined, the combination therapy was found to be significantly superior with regard to reduction in phobic avoidance (SMD=–0.31, 95% CI –0.49 to –0.12), general anxiety (SMD=–0.41, 95% CI –0.59 to –0.23), depression (SMD=–0.39, 95% CI –0.59 to –0.20) and social dysfunction (SMD= –0.36, 95% CI –0.61 to –0.11).
Although the two arms did not differ in terms of overall drop-out rates, drop-outs due to side-effects were much more frequent in the combined therapy arm (RR=3.01, 95% CI 1.61–5.63).
Continuation treatment
For as long as the treatments were continued, the advantage of the combination therapy appeared to persist, as the response rate at the end of continuation treatment still favoured the combination therapy (RR=1.23, 95% CI 1.00–1.51), and the global severity was significantly lower in the combination arm (SMD=–0.65, 95% CI –0.97 to –0.33).
After termination of treatment
In total, 658 patients from nine studies were assessed 6 to 24 months after discontinuing treatment (Fig. 4). Neither the response rate nor the global severity measure differed significantly between the two arms, which suggests that any advantage of the combination therapy disappeared over time.
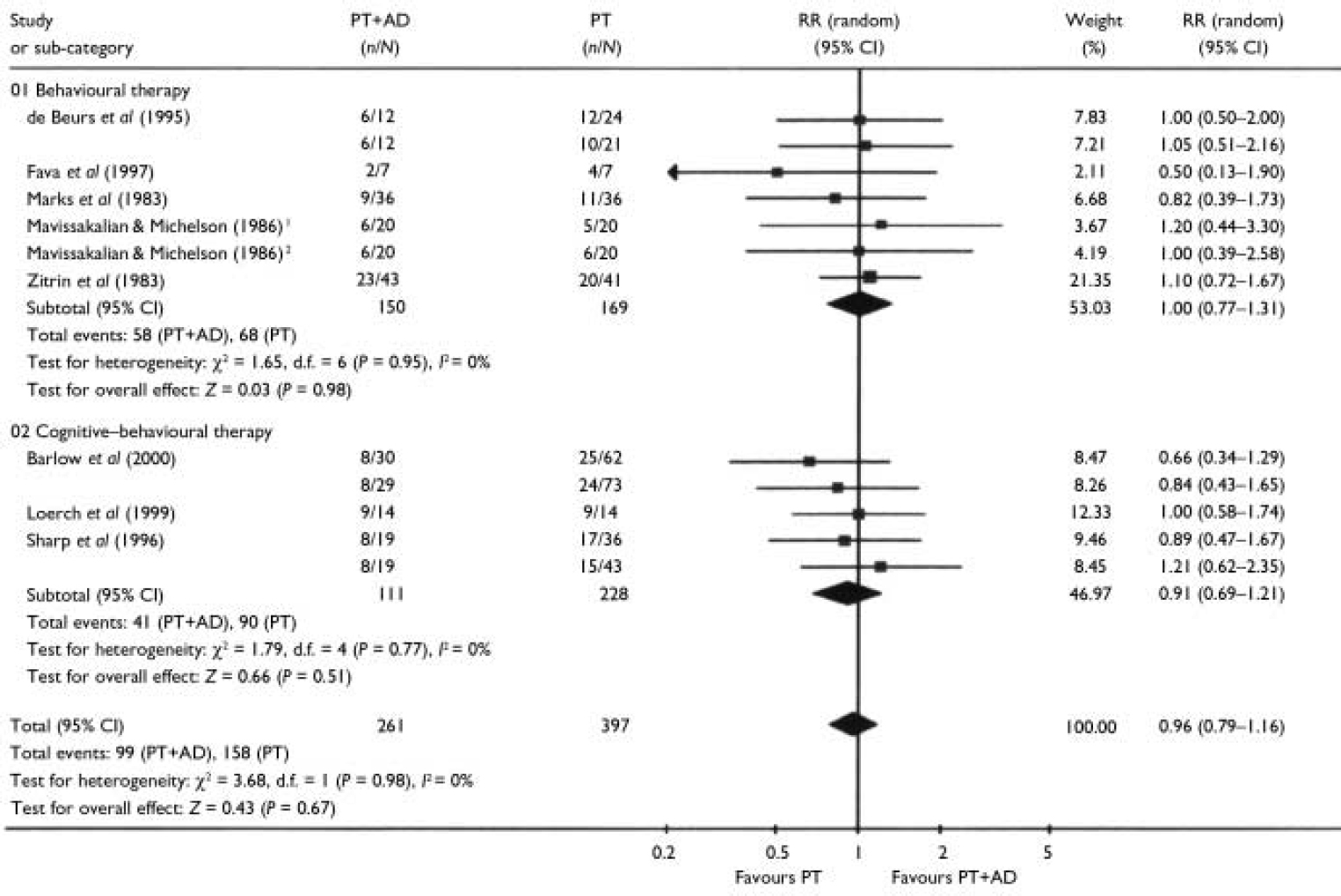
Fig. 4 Psychotherapy plus antidepressant v. psychotherapy alone: response after termination of treatment. PT, psychotherapy; AD, antidepressant; RR, relative risk. 1. Comparison A of two from this study; 2. comparision B of two from this study.
Subgroup and sensitivity analyses
Types of psychotherapy
For all the outcomes during the acute-phase or continuation treatments or after termination of treatment, the confidence intervals of the pooled estimates of the effectiveness of behaviour therapy and cognitive–behavioural therapy overlapped to a significant degree (Figs 1, 2, 3, 4). Pooling these two types of psychotherapy together seldom resulted in significant heterogeneity. The only exception was the ‘other psychotherapies’ category for the comparison of psychotherapy plus antidepressant with antidepressant treatment alone. The results of these studies were sometimes directionally different from those of the other studies in which behavioural or cognitive–behavioural therapies were administered, and combining them often resulted in significant heterogeneity.
Classes of antidepressants
We performed a meta-analysis of 14 studies in which TCAs were used and 7 studies in which SSRIs were used. The pooled estimates of the effect size of these two meta-analyses were very similar both to each other and to the overall results in terms of response or global severity (Table 2).
Table 2 Subgroup analyses for different classes of antidepressants and for patients with and without agoraphobia
| Overall | TCA | SSRI | Patients with agoraphobia | Patients without agoraphobia | |
|---|---|---|---|---|---|
| Combination v. antidepressant | |||||
| Acute phase | |||||
| Response1: RR (95% CI) | 1.24 (1.02-1.52) | 1.24 (1.05-1.46) | 1.23 (0.75-2.03) | 1.35 (0.88-2.08) | 1.31 (0.96-1.78) |
| Severity2: SMD (95% CI) | -0.30 (-0.55 to -0.05) | -0.35 (-0.66 to -0.04) | -0.48 (-1.01 to 0.04) | -0.51 (-1.45 to 0.44) | -0.22 (-0.55 to 0.10) |
| After termination | |||||
| Response1: RR (95% CI) | 1.61 (1.23-2.11) | 1.74 (1.12-2.69) | 1.52 (0.80-2.89) | 1.48 (1.02-2.17) | 1.39 (0.75-2.58) |
| Severity2: SMD (95% CI) | -0.58 (-1.78 to 0.63) | -0.58 (-1.78 to 0.63) | — | — | 0.00 (-0.34 to 0.34) |
| Combination v. psychotherapy | |||||
| Acute phase | |||||
| Response1: RR (95% CI) | 1.16 (1.03-1.30) | 1.17 (1.01-1.36) | 1.24 (0.94-1.65) | 1.18 (1.00-1.40) | 1.08 (0.84-1.38) |
| Severity2: SMD (95% CI) | -0.43 (-0.60 to -0.26) | -0.48 (-0.67 to -0.28) | -0.29 (-0.64 to 0.06) | -0.61 (-0.87 to -0.34) | -0.25 (-0.55 to 0.04) |
| After termination | |||||
| Response1: RR (95% CI) | 0.96 (0.79-1.16) | 0.91 (0.70-1.18) | 1.03 (0.73-1.44) | 1.00 (0.79-1.27) | 0.74 (0.46-1.19) |
| Severity2: SMD (95% CI) | 0.14 (-0.09 to 0.37) | 0.16 (-0.14 to 0.45) | 0.01 (-0.56 to 0.58) | 0.05 (-0.32 to 0.43) | 0.21 (-0.10 to 0.52) |
Patients with and without agoraphobia
We performed a meta-analysis of 13 studies that focused on patients with agoraphobia only. The results were very similar to the overall results, and overlapped substantially with the results of the only study that focused on patients without agoraphobia (Reference Barlow, Gorman and ShearBarlow et al, 2000) (Table 2).
When only those studies that were of higher quality in terms of allocation concealment, blinding, diagnostic accuracy, adequacy of psychotherapy or control of benzodiazepine co-intervention were included, the pooled estimates that were obtained were virtually identical to the overall results. Meta-regression analysis did not reveal any significant contribution of these quality variables, either individually or in combination, which suggests that the overall findings are robust.
DISCUSSION
Importance of the clinical problem in the context of previous reviews
There are a number of reasons why the clinical question concerning combined psychotherapy and antidepressant treatment is important. First, combination therapy is frequently provided in clinical practice, possibly because 30–50% of patients remain unimproved at the end of acute-phase treatment by either monotherapy. Second, it is now increasingly recognised that pharmacotherapy alone tends to result in substantial relapse rates not only when discontinued (Reference Mavissakalian and PerelMavissakalian & Perel, 2002), but even when maintained at adequate dosage (Reference Simon, Safren and OttoSimon et al, 2002), whereas psychotherapy is associated with fewer relapses in the short term, but may not always be able to prevent them in the long term (Reference Fava, Rafanelli and GrandiFava et al, 2001).
Several reviews of combination therapy can be found in the literature, but their conclusions have been variable, with some favouring the combination (Reference Mattick, Andrews and Hadzi-PavlovicMattick et al, 1990; Reference van Balkom, Bakker and Spinhovenvan Balkom et al, 1997), some favouring monotherapy (Reference Gould, Otto and PollackGould et al, 1995; Reference TaylorTaylor, 2000) and others drawing mixed or cautious conclusions (American Psychiatric Association, 1998; Reference Schmidt, Koselka, Woolaway-Bickel, Sammons and SchmidtSchmidt et al, 2001). Most of these reviews have been either unsystematic or narrative only (American Psychiatric Association, 1998; Reference TaylorTaylor, 2000; Reference Schmidt, Koselka, Woolaway-Bickel, Sammons and SchmidtSchmidt et al, 2001) and, where meta-analytical summary was undertaken, this did not focus on head-to-head comparisons (Reference Mattick, Andrews and Hadzi-PavlovicMattick et al, 1990; Reference Gould, Otto and PollackGould et al, 1995; Reference van Balkom, Bakker and Spinhovenvan Balkom et al, 1997), a practice that is known to be misleading (Reference Song, Altman and GlennySong et al, 2003).
Current findings
This systematic review demonstrated that combining psychotherapy and antidepressant treatment produced outcomes that were consistently superior to either treatment alone for the acute-phase treatment, in terms of both the response rates and the continuous outcomes measuring various aspects of the disorder. Taking the average response rates of 50–70% for single-modality treatments, the pooled RR of 1.2 for the combination therapy is equivalent to a value for the number needed to treat of between 7 and 10. During the acute-phase treatment, combination therapy resulted in more drop-outs due to side-effects than psychotherapy alone, and the number needed to harm was around 26.
The naturalistic follow-up of the randomised controlled trials that were included suggested that the combination therapy had a sustained advantage over antidepressant therapy. At 6–24 months after termination of treatment, the combined therapy still showed a number needed to treat of around 6 compared with antidepressant treatment alone. With regard to the comparison between the combination therapy and psychotherapy, there was no evidence of long-term benefit of the former compared with the latter. In this respect, it is interesting to note that, despite recent admonitions from several experts (Reference TaylorTaylor, 2000; Reference Schmidt, Koselka, Woolaway-Bickel, Sammons and SchmidtSchmidt et al, 2001; Reference Foa, Franklin and MoserFoa et al, 2002), the combination therapy was found to have no disadvantage in the long term.
Strengths and limitations
This systematic review has several major strengths. First, we performed systematic and comprehensive searches for relevant trials. We identified 23 randomised comparisons from 21 studies, whereas previous reviews included a maximum of 13 studies. Second, we applied the intention-to-treat principle when performing meta-analysis of dichotomous outcomes by counting all of the drop-outs as non-responders. This policy is especially pertinent in the context of the relative merits of the combination therapy over monotherapy in the long term, because we are interested in the number of patients doing well as a proportion of all those who started the acute-phase therapy, not just those who successfully completed it. Finally, the a priori planned heterogeneity and sensitivity analyses indicated that the results of the analyses were quite robust.
However, several potential limitations of this study must be acknowledged. First, the comparability of the treatment arms after termination of acute-phase and continuation treatments may be compromised by the naturalistic nature of the follow-up. Participants were usually free to seek further treatment between the termination of treatment and the follow-up assessments, and 30–77% of them received additional therapies. Unfortunately, inadequate reporting of additional therapies precluded further examination of this issue across studies. If the published studies had reported the number of patients who did well without further treatment, the interpretation of the relative merits of the combination therapy v. monotherapies would have been more straightforward. Second, funnel-plot analyses suggested the possibility of publication bias. However, the exclusion of outliers did not affect the pooled estimates. Third, we must point out that until recently there have been no widely accepted and validated rating scales for panic disorder, and that some of the studies that were included used the authors’ original scales. One study indicated that rating scales which have not been validated or standardised are more likely to report statistically significant findings (Reference Marshall, Lockwood and BradleyMarshall et al, 2000). Fourth, owing to this lack of accepted assessment methods for panic disorder, the definition of response (our primary outcome) had to be operationalised by a variety of measures. However, these overall results were corroborated by analyses that focused on specific aspects of the symptoms of panic disorder.
It must be noted that our review does not address the relative merits of combination therapy compared with sequential treatments. Given the present findings, some might argue for psychotherapy alone as first-line treatment, only considering combination therapy if psychotherapy fails. Although this appears to be a viable option, such a practice cannot be informed by the data available from these trials.
Clinical implications and future research
The current findings from the best available evidence suggest that either combined therapy or psychotherapy alone may be chosen as first-line treatment for panic disorder with or without agoraphobia. Treatment decisions may depend on the patient's preferences and values. Antidepressant pharmacotherapy alone is not to be recommended as first-line treatment where appropriate resources are available. Although none of the studies included in this review examined cost issues, economic consideration of the costs of years of medication compared with ‘one-off’ psychological treatment would also favour the use of psychotherapy (Reference Otto, Pollack and MakiOtto et al, 2000).
Several issues warrant further investigation. First, in the acute-phase treatment, if we adhere to the strict intention-to-treat principle, the response rates are only slightly above 50% for combination therapy and slightly below 50% for psychotherapy alone. Therefore additional strategies may be required to deal with partial and nonresponders to these therapies. Second, there are currently only limited data available on the effects of combining antidepressants with non-cognitive–behavioural therapies, such as psychodynamic and interpersonal therapies. In this review, the only available trial that involved psychodynamic therapy showed increased benefit when combined with antidepressants. This suggests the potential value of future trials designed to investigate this type of combination in the treatment of panic disorder.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Combined psychotherapy plus antidepressant therapy is more effective than either therapy alone for the acute-phase treatment of panic disorder with or without agoraphobia (number needed to treat 7–10). Combined therapy produces more drop-outs due to side-effects than psychotherapy alone (number needed to harm around 26).
-
▪ Combined therapy is as effective as psychotherapy and more effective than antidepressant pharmacotherapy after discontinuation of the acute-phase treatment (number needed to treat around 6).
-
▪ The evidence was most consistent for behavioural therapy and cognitive–behavioural therapy.
LIMITATIONS
-
▪ The comparability of the treatment arms after termination of the acute-phase and continuation treatments may be compromised by the naturalistic nature and inadequate reporting of the follow-up.
-
▪ Older studies did not use standardised assessment measures.
-
▪ This systematic review cannot address the relative merits of combination v. sequential treatments by psychotherapy and pharmacotherapy
Acknowledgements
This systematic review was conducted within the framework of the Cochrane Collaboration Depression, Anxiety and Neurosis Group, and we acknowledge their help and support. It was supported in part by a Health and Labour Sciences Research Grant (Research on Health and Technology Assessment) H13-018 from the Ministry of Health, Labour and Welfare, Japan.
T.A.F. has received research grants and/or fees for speaking from: Asahi Kasei, Astellas, Dai-Nippon, Eisai, Eli Lilly, GlaxoSmithKline, Janssen, Kyowa Hakko, Meiji, Organon, Tsumura and Yashitomi.









eLetters
No eLetters have been published for this article.