Lifestyle and eating habits are key modifiable factors that people can change to decrease chronic disease risk. Poor diet, in particular, has been convincingly linked to the incidence of CVD and some forms of cancer( 1 , 2 ), which are responsible for most of the disease burdens in the majority of developed countries( Reference Allender, Peto and Scarborough 3 ).
Dietary recommendations promoting healthy dietary patterns including whole-grain foods, legumes, vegetables and fruit, and suggesting that the intake of full-fat dairy products, sweets and red meat be limited, are an emerging approach for the prevention of several diseases, and the Mediterranean-style diet embodies many of these recommendations( Reference Willett, Sacks and Trichopoulou 4 ). Indeed, in a recent meta-analysis, the Mediterranean eating pattern has turned out to be more effective than low-fat diets in inducing important long-term changes in cardiovascular risk factors and inflammatory markers( Reference Alain, Katja and Heiner 5 ).
Greater adherence to a Mediterranean-like dietary pattern, in particular, has been shown to be associated with improvement in health status( Reference Sofi, Abbate and Gensini 6 , Reference Sofi, Cesari and Abbate 7 ) as well as inversely associated with both premature( Reference Martinez-Gonzalez, Guillen-Grima and De Irala 8 ) and total mortality( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 9 , Reference McNaughton, Bates and Mishra 10 ). The latter effect has been observed in countries both inside( Reference Buckland, Agudo and Travier 11 ) and outside( Reference Lagiou, Trichopoulos and Sandin 12 – Reference Osler and Schroll 14 ) the Mediterranean basin, for instance, in Nordic countries( Reference Lagiou, Trichopoulos and Sandin 12 ), where we recently reported an inverse association with mortality both in elderly( Reference Tognon, Rothenberg and Eiben 15 , Reference Sjogren, Becker and Warensjo 16 ) and in middle-aged adults living in Sweden( Reference Tognon, Nilsson and Lissner 17 ).
Dietary patterns in the Mediterranean countries are changing rapidly, with an increased consumption of animal products and saturated fats and a decline in the intake of vegetable-based foodstuffs( Reference Martinez, Llull and Del Mar Bibiloni 18 – Reference Garcia-Closas, Berenguer and Gonzalez 20 ). On the other hand, Nordic populations have paradoxically increased their intakes of typical Mediterranean items such as fruit, vegetables and wine between 1970 and mid-2000( 21 – Reference Osler, Heitmann and Schroll 23 ).
The aim of the present study was to determine whether the Mediterranean Diet Score (MDS) was inversely associated with all-cause mortality as well as cardiovascular incidence and mortality in the Danish MONICA (MONItoring trends and determinants of Cardiovascular disease) population study.
Subjects and methods
Subjects and measures
In 1982, a sample of 4807 subjects was randomly selected from the Central Person Register of citizens born in 1922, 1932, 1942 and 1952 living in eleven municipalities in the Copenhagen County( Reference Hartz, Rupley and Rimm 24 ). Of these, 226 were of non-Danish origin. Among the 4581 invited, 3608 participated in a subsequent health examination in 1982–3( Reference Jensen and Jorgensen 25 ). The non-respondents have been described in detail elsewhere( Reference Heitmann 26 ). The present study was part of the Danish MONICA project, an international study conducted under the auspices of the WHO to monitor CVD trends and determinants. One subject was excluded due to missing BMI information at baseline and three subjects for missing blood test results. The cohort described here included 1849 subjects (948 women) with complete information on diet intake and anthropometry and 1348 subjects (701 women) who also had results for blood tests and blood pressure.
The participants filled in a questionnaire describing their highest grade of education or highest year of regular schooling classified into 0–7, 8–11 and ≥ 12 years, their cigarette smoking habits and their leisure time activity. The latter was categorised into four classes: inactive; light ( < 4 h/week); moderate (>4 h/week); energetic (>4 h/week).
Body weight was measured to the nearest 0·1 kg using a lever balance, with subjects dressed in light clothing or underwear. Height was measured without shoes to the nearest 1 cm. Weight change information after 11 years of follow-up was available for a subsample of 1348 subjects.
BMR (kcal/d) was calculated according to Schofield equations for subjects aged 30–59 years( Reference Schofield 27 ):
Food intake level (FIL) was then calculated based on the ratio of reported energy intake to BMR. Both systolic and diastolic blood pressures were measured with a London School of Hygiene sphygmomanometer, using one of the three different cuffs. Duplicate measurements were taken on the left arm after a minimum of 5 min of rest in a supine position. Means of duplicate measures were calculated and used in the analyses described below. Blood samples were drawn after a 12 h overnight fast. A commercial enzymatic method was used (Boehringer Mannheim) to measure the concentrations of total cholesterol, HDL-cholesterol and TAG (mmol/l) in the serum( Reference Heitmann 28 ). The total cholesterol:HDL-cholesterol ratio was calculated, and a value greater than 4 was arbitrarily chosen as a threshold of a risky lipid profile.
Dietary assessment
Information on diet was obtained by means of a four-page (A3 format) weighed 7 d food record. The front page contained instructions for correct completion of the diet records together with the average household weights of nineteen frequently consumed foods, e.g. the white of an egg and a slice of bread. For butter and liver pâté, three examples were given of typical amounts put on a slice of bread. On the next pages, 100 foods were listed in the following nine subgroups: dairy products; bread and cereal grains; fats; cold cuts, etc.; vegetables; fruit; meat (including poultry and fish); drinks; miscellaneous items. The last page included space to record foods that did not fit into any of the nine groups, such as mixed dishes, home-made salads and cakes.
The participants were also given thorough verbal instructions on how to fill out the food record. It was emphasised that the diet record be completed during a typical 7 d period including a minimum of non-habitual social activities. Food quantities were expressed in grams, estimated as accurately as possible or preferably weighed. The same trained dietitian manually checked and coded all food records into dietary components.
Definitions of food groups and of the Mediterranean Diet Score
To assess the association of diet and lifestyle factors with all-cause mortality, a version of the modified MDS( Reference Knoops, de Groot and Kromhout 29 ) adapted to the MONICA diet questionnaire was calculated. The score comprised eight positive or negative components: (1) ratio of (monounsaturated+polyunsaturated):saturated fats; (2) vegetables; (3) fruit; (4) cereal grains; (5) fish and fish products; (6) alcohol intake; (7) meat, meat products and eggs (negative); (8) dairy products (negative). As has been described previously( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 9 , Reference Knoops, de Groot and Kromhout 29 ), the intake of each component was adjusted to the daily energy intakes of 10·467 kJ (2500 kcal) for men and 8·374 kJ (2000 kcal) for women, in order to obtain energy-adjusted associations in all the analyses. As sex-specific median intakes were taken as cut-off points, the final score must be considered as a measure of relative adherence to the Mediterranean dietary pattern. A value of 1 was assigned to subjects whose consumption was higher than the sex-specific median and 0 to the others, with the exception of meat and dairy products, where the reverse rule was applied. The final score was obtained by summing these values, and it varied from 0 (low adherence) to 8 (high adherence). Food groups were defined based on two different procedures, from which two different scores were produced. The first procedure included the identification of all the possible food items that could be classified according to the above-mentioned food categories (vegetables, fruit, etc.), but excluding mixed dishes (score 1). The second procedure included food items classified into food groups as in score 1, but now including ingredients extrapolated from mixed dishes or recipes (score 2). Finally, a variant of score 2 was created, now including wine instead of total alcohol intake (score 3).
Endpoints
Information on all-cause mortality as well as on CVD or myocardial infarction (MI) incidence and mortality was retrieved from the National Patient Registry of Hospital Discharges, the Cause of Death Register and the Central Person Register. The subjects were followed until 8 July 2007 for an average of 14 years. Survival time was parameterised in terms of lifetime until death or censoring event in years, with left truncation at the age of entrance into the study being equal to baseline examination. Total CVD cases were identified based on codes 390–458 (ICD8) and I00–I99 (ICD10) and MI cases were identified based on codes 410 (ICD8) and I21 (ICD10), while stroke cases were identified based on codes 430–434+436 (ICD8) and I60–I64 (ICD10). Analyses on CVD, MI and stroke incidence (both fatal and non-fatal cases) and mortality were performed given that there was no CVD, MI or stroke at baseline.
Statistical analyses
The associations of the three above-mentioned diet scores with mortality were determined by means of Cox proportional hazards models, either adjusted only by age or adjusted for potential confounders such as sex, age, obesity, smoking status (two dummy variables were included, describing pack years greater than 0 but less than 30 and pack years greater than 30, keeping the ‘never smoked’ category as the reference), education (the lowest level v. higher levels) and physical activity (see the above-mentioned categories). The latter model was then considered the main model. Additionally, in order to determine possible pathways of effects, we performed some confirmatory analyses adjusting for blood pressure (systolic and diastolic, included as continuous variables), blood lipids (TAG, included as a continuous variable, and total cholesterol:HDL-cholesterol ratio >4) and weight change (including two dummy variables describing weight change >3 kg or < − 3 kg and keeping a weight change of 0 to ± 3 kg as the reference category). All-cause mortality as well as cause-specific incidence and mortality, i.e. total CVD, MI and stroke, were studied in association with the MDS.
Effect modification of exposure (MDS) by each covariate was tested in the main model by including interaction terms. Stratified estimates were calculated in case a significant interaction was found. The association of single components of the MDS was also tested separately, by including as exposure a variable describing an intake over the sex-specific medians (fat ratio, vegetables, fruit, cereal grains, fish and alcohol) or below the median (meat and dairy products). To reduce bias for changes in diet or lifestyle factors due to subclinical disease, the main model was also run after excluding the first 2 years of follow-up. In analyses, different versions of the MDS were included, and these were excluded one at a time, and also single components of these scores were tested (while keeping all other components) in order to determine whether any associations could be explained by a single component.
With the aim of determining the additive effects of an increasing number of risk factors such as ever been a smoker, having a low physical activity level (PAL) ( < 4 h/week) and obesity (BMI ≥ 30 kg/m2) and not consuming a Mediterranean-like diet (MDS ≤ 4), a new score was calculated, assigning an additional point for each of the above-mentioned risk factors. Different hazard ratios (HR) and 95 % CI describing the association (adjusted by sex) of each level of the score with all-cause mortality were calculated and depicted in a histogram.
A sensitivity analysis was performed, aiming to confirm the main results in a subsample of subjects who could be considered ‘adequate reporters’. The ratio of FIL:PAL was calculated. Adequate reporters were defined according to three different definitions based on increasingly stringent criteria, i.e. exclusion of the lowest 30 % (less stringent criterion) and of the lowest 50 % and of the lowest 65 % of the FIL:PAL ratio (most stringent criteria).
Statistical analyses were performed with SAS software (version 9.0; SAS Institute). All tests were considered significant if P< 0·05.
Bioethics
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki (1989) of the World Medical Association, and all procedures involving human subjects were approved by the Ethics Committee of the Medicine Faculty of the Copenhagen County. All subjects were informed of the aims and procedures of the study, and they gave their written consent.
Results
Cohort description
The population consisted of 948 women (51·3 %) and 901 men (48·7 %). Only a small number were obese (n 138, 7·5 %). A total of 476 (25·7 %) had never smoked cigarettes, while 303 (16·4 %) smoked more than thirty pack years. Finally, 241 subjects (13 %) abstained from any alcohol intake. Among the cardiovascular risk factors, 450 subjects (24·3 %) had high blood pressure (either systolic ≥ 140 mmHg or diastolic ≥ 90 mmHg), almost half of the population had either a total cholesterol:HDL-cholesterol ratio >4 (n 955, 51·6 %), while about a third had gained more than 3 kg at follow-up (n 666, 36·0 %).
Energy-adjusted median values of each score component (Table 1) showed that the ratio of unsaturated:saturated fats was 1·1 (5th–95th percentiles: 0·8–1·6), indicating a similar level of consumption of each type of fat. Vegetable intake was higher than fruit intake, while the median intake for dairy products was almost 300 g/d. Median alcohol intake among users was about one standard unit and a half (15·5 g/d), while median wine intake was 2·5 g/d. The median reported daily energy intakes were 10 571·7 MJ (2525 kcal) in men and 7460·9 MJ (1782 kcal) in women. The ratio of energy intake:BMR was 1·4 (5th–95th percentiles: 0·8–2·1), indicating a good estimation of energy intake compared with the metabolic rate. The differences among the median values of the three scores were very small.
Table 1 Intake value of each food group included in the Mediterranean Diet Score, adjusted to 8·374 MJ (2000 kcal) in women and 10·467 MJ (2500 kcal) in men* (Medians with their 5th–95th percentiles)
FIL, food intake level.
* Energy intake and the ratio of energy intake:BMR are also reported.
Main analyses and effect modification
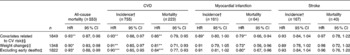
The association between the three different versions of the MDS (scores 1, 2 and 3) and all-cause mortality as well as CVD incidence and mortality was assessed (Table 2), adjusting for only age or for different potential confounders such as sex, age, BMI, education, physical activity and cigarette smoking (main model). Since no statistical interaction (P>0·05) with sex was found in relation to almost all outcomes, all analyses were conducted on men and women together, adjusting for sex.
Table 2 Survival analyses on the association between an increase in one unit of the three different versions of the Mediterranean Diet Score (scores 1, 2 and 3) and all-cause mortality as well as cardiovascular mortality and incidence (Hazard ratios (HR) and 95 % confidence intervals)

Values were significantly different: * P≤ 0·05, ** P≤ 0·01, *** P≤ 0·001.
† Fatal and non-fatal cases.
‡ Adjusted for sex, BMI, education, physical activity and cigarette smoking.
Results were, in general, in the direction of an inverse association between the three scores and all the outcomes, with the exception that the association between the MDS calculated excluding mixed dishes and recipes (score 1) did not reach statistical significance in either the main model or in the age-only-adjusted model. In contrast, the second version of the MDS, including the ingredients from mixed dishes and recipes (score 2), was inversely associated with all outcomes except with stroke incidence (HR 0·96; 95 % CI 0·86, 1·07) and mortality (HR 1·03; 95 % CI 0·82, 1·30). In the age-only-adjusted model, score 2 was significantly associated only with CVD incidence and MI mortality. Finally, score 2, recalculated to include wine instead of total alcohol intake (score 3), was significantly associated with all outcomes, but, again, not with stroke.
No effect modification was found when testing the interaction with potential confounders, with the exception of the association between the MDS and MI mortality, which was significant only at low PAL (moderate activity < 4 h/week) (score 3: HR 0·61; 95 % CI 0·43, 0·86; P for interaction: 0·04).
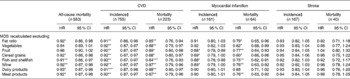
In order to determine possible pathways of effects in relation to the cardiovascular risk, the main model was further adjusted for blood lipids and blood pressure as well as for the latter plus weight change (Table 3). With the exception of MI incidence, which did not resist the adjustment for weight change (HR 0·91; 95 % CI 0·79, 1·05), the results obtained after these additional adjustments were in line with the previous ones (main model, Table 2) or slightly stronger. Finally, the exclusion of early deaths (i.e. subjects who died during the first 2 years of follow-up) did not materially change the results, with the exception, again, of MI incidence, where association with the score was only of borderline significance (HR 0·91; 95 % CI 0·81, 1·02).
Table 3 Survival analyses on the association between an increase in one unit of Mediterranean Diet Score 3 and all-cause mortality as well as cardiovascular (CV) mortality and incidence (Hazard ratios (HR) and 95 % confidence intervals)
Values were significantly different: * P≤ 0·05, ** P≤ 0·01, ***P≤ 0·001.
† Fatal and non-fatal cases.
‡ Adjusted for sex, BMI, education, physical activity and cigarette smoking.
§ Also adjusted for covariates potentially related to possible pathways of CV risk (i.e. blood pressure, TAG and total cholesterol:HDL-cholesterol ratio).
∥ Also adjusted for both covariates potentially related to possible pathways of CV risk and weight change.
Supplementary analyses
Table 4 summarises the results of a supplementary analysis, where the association of all endpoints with different versions of score 3 was determined. The alternative versions were created by excluding, one at a time, each single score component to check if any of these could explain alone the association of the score. The results show that the association was robust, and in the few cases where the association was not significant, a borderline association was found. The association of single MDS components (high or low intake according to median values) with all the endpoints investigated revealed only a few significant results (Table 5). The most robust one was found with high fruit intake, which was inversely associated with all-cause mortality (HR 0·74; 95 % CI 0·62, 0·88), CVD incidence (HR 0·86; 95 % CI 0·75, 1·00) and mortality (HR 0·72; 95 % CI 0·55, 0·94). Also, vegetables showed some significant associations with all-cause mortality (HR 0·81; 95 % CI 0·68, 0·96) as well as with MI incidence (HR 0·73; 95 % CI 0·54, 1·00) and mortality (HR 0·58; 95 % CI 0·35, 0·96).
Table 4 Sensitivity analyses excluding, one at a time, each level of Mediterranean Diet Score (MDS) 3† (Hazard ratios (HR) and 95 % confidence intervals)
Values were significantly different: * P≤ 0·05, ** P≤ 0·01, *** P≤ 0·001.
† All results were obtained from a Cox proportional hazards model, adjusted for sex, BMI, education, physical activity and cigarette smoking.
‡ Fatal and non-fatal cases.
Table 5 Survival analyses on the association between the intake of single food groups above or below the median and several outcomes related to all-cause mortality and cardiovascular incidence and mortality† (Hazard ratios (HR) and 95 % confidence intervals)
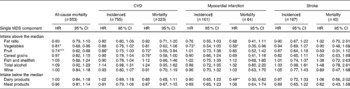
MDS, Mediterranean Diet Score.
Values were significantly different: * P≤ 0·05, ** P≤ 0·01, *** P≤ 0·001.
† All results were obtained from a Cox proportional hazards model, adjusted for sex, BMI, education, physical activity and cigarette smoking.
‡ Fatal and non-fatal cases.
The results of the sensitivity analyses, based on three different definitions of adequate diet reporters (>30 % FIL:PAL, >50 % and >65 %), showed that although score 3 was always inversely associated with both incidence and mortality, not all these analyses were statistically significant due to a highly reduced number of cases, especially when the most stringent criterion was applied (>65 % FIL:PAL). No large variations of these estimates were observed comparing these three analyses. Both all-cause mortality and CVD mortality were shown to be the strongest associations, since they were statistically significant no matter how adequate diet reporters were defined.
Mediterranean Diet Score and other lifestyle factors
Diet and lifestyle are strongly associated, and the level of the MDS was associated with smoking status, obesity and physical activity. We determined the cumulative effect of diet and lifestyle-related risk factors on mortality (not to be confused with a dose response to the number of levels of the MDS) by means of an additional score (Fig. 1). With increased number of risk factors (i.e. ever been a smoker, having a low physical activity level, being obese and not consuming a Mediterranean-like diet) the mortality risk increased linearly. In the highest risk category (three or four risk factors) the sex-adjusted association will all-cause mortality was strong and significant (HR 2·37; 95 % CI 1·50, 3·75; P for trend < 0·0001).
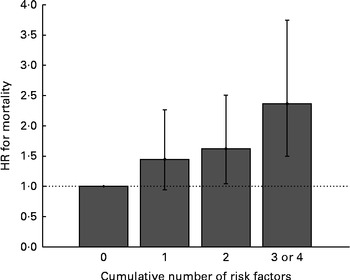
Fig. 1 Association between a cumulative number of risk factors related to both diet and lifestyle (including a modified Mediterranean Diet Score ≤ 4, ever being a smoker, low levels of physical activity and being obese) and all-cause mortality (adjusted by age). Values are hazard ratios (HR), with 95 % CI represented by vertical bars. P for trend < 0·0001. Cumulative number of risk factors: 0 – n 144 (HR 1); 1 – n 606 (HR 1·45, 95 % CI 0·93, 2·26); 2 – n 787 (HR 1·62, 95 % CI 1·05, 2·51); 3 or 4 – n 312 (HR 2·37, 95 % CI 1·50, 3·75).
Discussion
The present study shows that the MDS was inversely associated both with all-cause mortality and with cardiovascular incidence and mortality, but not with stroke incidence and mortality. All associations proved to be robust to the adjustment for several potential confounders (i.e. sex, BMI, education, physical activity and smoking status) as well as covariates potentially related to possible pathways of CV risk, such as blood pressure, blood lipids and, notably, weight change after 11 years of follow-up. Increasing the number of unhealthy dietary or lifestyle-related factors additively increased the mortality risk by more than two times compared with those with no risk factors, as suggested by previous studies( Reference Knoops, de Groot and Kromhout 29 , Reference van den Brandt 30 ). Fruit and vegetables were particularly relevant, as they attenuated the association of the diet score with some outcomes when excluded from score calculations.
Notably, only the MDS including ingredients from mixed dishes and recipes produced statistically significant results. It is not clear how ingredients have been treated in previous studies( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 9 , Reference Knoops, de Groot and Kromhout 29 , Reference Fung, Rexrode and Mantzoros 31 , Reference Trichopoulou, Costacou and Bamia 32 ). The present results imply that they should be included in the calculations of this score, because they allow for a more accurate depiction of a Mediterranean-like dietary pattern.
CVD prevention is of major public health importance, because of the negative impact of CVD on the quality of life( Reference Kahn, Robertson and Smith 33 ) and the expected increase in the number of deaths( 34 ). Lifestyle changes and particularly dietary interventions are cost-effective means for the prevention of CVD and the reduction of the social and economic burden of this condition( Reference Nishida, Uauy and Kumanyika 35 ).
Several studies( Reference Mitrou, Kipnis and Thiebaut 13 , Reference Knoops, de Groot and Kromhout 29 , Reference Trichopoulou, Costacou and Bamia 32 ) have shown associations between the adoption of a Mediterranean dietary pattern and the lower risk of overall mortality and death because of IHD and CVD in general. Particularly, the MDS has been shown to be inversely associated with mortality in Swedish elderly( Reference Tognon, Rothenberg and Eiben 15 ) and in middle-aged Swedes where an inverse association with cardiovascular mortality (excluding stroke) was found in women and an association with cancer mortality was found in men( Reference Tognon, Nilsson and Lissner 17 ). In the latter study, fruit intake was inversely associated with all-cause mortality in women. The results of the present study again suggest that fruit and vegetable intakes can have particular importance in the reduction of cardiovascular risk. A few years ago, a meta-analysis of prospective studies had calculated a CHD risk reduction of 4 % for each additional portion of fruit and vegetables consumed per day( Reference Dauchet, Amouyel and Hercberg 36 ). However, the exact mechanisms by which these food items reduce CV risk are still unclear( Reference Dauchet, Amouyel and Dallongeville 37 ).
We do not have a clear explanation as to why the MDS and its single components were not at all associated with stroke mortality, also when separately analysing haemorrhagic v. non-haemorrhagic cases as well as ischaemic v. non-ischaemic cases. However, a tendency towards an inverse association was found for stroke incidence. Some epidemiological studies have also examined the association between a MDS and the risk of stroke. Among these, some( Reference Fung, Rexrode and Mantzoros 31 , Reference Agnoli, Krogh and Grioni 38 , Reference Kastorini, Milionis and Kantas 39 ) found an inverse association, while others did not( Reference Tognon, Nilsson and Lissner 17 , Reference Gardener, Wright and Gu 40 ). Moreover, a recent paper has found an inverse association between adherence to a Mediterranean-like diet and total cerebrovascular disease( Reference Misirli, Benetou and Lagiou 41 ). Stroke mortality, in particular, could be more related to factors such as the use of anticoagulant therapy and the course of related infections, although the influence of the latter on stroke outcome is still debated( Reference Roquer, Cuadrado-Godia and Giralt-Steinthauer 42 ).
Comparing the methodology used in the present study with the one that we had applied previously to elderly Swedes (based on a refined version of the MDS( Reference Tognon, Rothenberg and Eiben 15 )), here a further score refinement was possible by adding the components of mixed dishes and recipes, which enabled us to identify the healthiest dietary pattern in relation to the health effects of a Mediterranean-like dietary pattern. Considering the alcohol component, in particular, one point should be noted. Based on the known U-shaped relationship between alcohol intake and CHD, previous studies using the MDS have given one point for moderate alcohol intakes ( < 50 g/d in men and 25 g/d in women) instead of negative scoring for high intakes( Reference Milaneschi, Bandinelli and Corsi 43 , Reference Romaguera, Guevara and Norat 44 ). However, since in our cohort only about 10 % of the subjects exceeded these thresholds, we decided to categorise alcohol intakes according to medians, as for the other food items.
The strengths of the present study include the adjustment of the analyses for several potential confounders as well as for covariates potentially related to possible pathways of cardiovascular risk such as blood pressure and lipids, our ability to examine effects on both MI and stroke, and the availability of a detailed food database based on a validated dietary assessment method that provided details of ingredients from mixed dishes and recipes. Additionally, there is almost 100 % follow-up for endpoints in the Danish registries as well as 100 % coverage of the Danish population( Reference Abildstrom, Torp-Pedersen and Madsen 45 ), which means a negligible loss to follow-up. However, some limitations must also be acknowledged, such as possible residual confounding due to physical activity, as well as the likelihood that diets could have been misreported. However, random misreporting would have resulted in attenuation and not inflation of the hazards, suggesting that the observed significant association is likely to be true.
In conclusion, the present Danish population study demonstrates that within a Nordic setting, a high MDS is associated with longer survival and with a reduction in cardiovascular mortality, particularly, MI. Fruit and vegetable intakes seem to be of particular importance in influencing the strength of this association. Thus, the study supports evidence that the Mediterranean diet may be beneficial to health even among populations outside the Mediterranean basin. This is of importance considering that in Europe this pattern is not so common any more among the young generation( 46 ).
Acknowledgements
The present study was supported by a grant from the Freja-programme from the Danish medical research foundation. We thank Kirsten Mehlig from the University of Gothenburg for the statistical advice. G. T. received salary support from the Swedish Council on Working Life and Social Research (FAS) EpiLife centre. The authors' responsibilities were as follows: G. T. performed the statistical analyses and wrote the paper; L. L. helped with the statistical analyses and their interpretation and provided comments on the manuscript; D. S. provided the dataset, helped with the statistical analyses and their interpretation and provided comments on the manuscript; K. Z. W. contributed to food group classification and provided comments on the manuscript; B. L. H. coordinated the research, helped with the statistical analyses and their interpretation and provided comments on the manuscript. All authors read and approved the final manuscript. The authors declare no conflicts of interest.








