Patients with severe psychotic disorders typically have small social networks containing disproportionately high numbers of relatives (Reference Cresswell, Kuipers and PowerCresswell et al, 1992). None the less, despite their increased reliance on family members for social contact, many patients do not have frequent contact with a relative (Reference Mitchell and BirleyMitchell & Birley, 1983). This is of concern given that patients' lack of contact with relatives is associated with increased psychiatric hospital use (Reference Becker, Thornicroft and LeeseBecker et al, 1997).
The theory that patients' isolation from relatives is attributable to patients' social withdrawal has gained widespread acceptance. Wasow (Reference Wasow1994), however, suggests an alternative explanation, that relatives avoid contact with patients because they find the situation distressing. The aim of the present study is to examine which characteristics predict frequent patient—relative contact, in particular whether relatives' experience, and the characteristics found in the literature to be associated with their distress, have a significant effect.
Predictors of relatives' experience
It has been demonstrated that a patient's illness may have an impact on several areas of family life (Reference Perring, Twigg and AtkinPerring et al, 1990), but it is unclear why some relatives are more adversely affected than others. Numerous potential influences have been investigated, including socio-demographic characteristics of patients and relatives, patients' clinical characteristics and characteristics of the patient—relative relationship, but generally findings are inconsistent, possibly reflecting differences in the conceptualisation and measurement of relatives' experience (Reference Maurin and Barmann BoydMaurin & Barmann Boyd, 1990). An exception is patients' symptom severity. Most studies have found it to be strongly related to their relatives' ‘burden’ (Reference BaronetBaronet, 1999), although a few have found no association (Reference Magliano, Fadden and MadianosMagliano et al, 1998). The specific symptoms that relatives find most distressing are not yet clear, however. Some studies have found negative symptoms to be more problematic, whereas others indicate that relatives have greater difficulty with positive symptoms (Reference Provencher and MueserProvencher & Mueser, 1997).
Aims
This study aims to identify predictors of frequent patient—relative contact. If relatives avoid frequent contact because they find the situation distressing, we anticipate that patients' symptom severity, shown in the literature to be associated with relatives' ‘burden’, will predict patient—relative contact frequency. We also anticipate that relatives who appraise caregiving more negatively and experience more psychological distress at baseline will be less likely to have frequent contact with the patient at 2-year follow-up.
METHOD
Sample
The sample was drawn from a multi-centre, randomised controlled trial of intensive case management for patients with severe psychotic disorders (UK700 Group, 1999). Patients met the following criteria:
-
(a) aged between 18 and 65 years;
-
(b) a diagnosis of psychotic disorder according to Research Diagnostic Criteria (Reference Spitzer, Endicott and RobinsSpitzer et al, 1978) established by a structured examination of case notes (Reference McGuffin, Farmer and HarveyMcGuffin et al, 1991);
-
(c) a minimum of two psychiatric hospital admissions, at least one in the preceding 2 years.
Patients with organic brain damage or a primary diagnosis of substance misuse were excluded. The sample was obtained by systematic review of community mental health team case-loads. Independent researchers collected information from case notes and interviews with patients, relatives and health professionals.
If the patient had face-to-face contact with a relative at least twice per week, their consent to approach the relative for interview was sought. Relatives included spouses and partners. Following baseline assessment, patients were randomised to 2 years of either standard or intensive case management. Assessments were repeated at 1- and at 2-year follow-up.
Instruments
Patients' clinical features
Disability in social functioning during the preceding month was measured using the 11-item World Health Organization (1988) adaptation of the Disability Assessment Schedule (DAS). Severity of psycho-pathology over the preceding week was assessed using the 65-item Comprehensive Psychiatric Rating Scale (CPRS; Reference Åsberg, Montgomery and PerrisÅsberg et al, 1978). The 10-item Montgomery-Åsberg Depression Rating Scale (MADRS; Reference Montgomery and ÅsbergMontgomery & Åsberg, 1979) was derived from the CPRS. Negative symptom severity during the same period was measured using the Scale for the Assessment of Negative Symptoms (SANS; Reference AndreasenAndreasen, 1989).
Information regarding age at onset and duration of psychosis - months in psychiatric hospital since onset, months in psychiatric hospital and number of admissions to psychiatric hospital in the preceding 2 years, and parasuicide - was collected from case notes and hospital information systems. Two items from a slightly modified World Health Organization Life Chart (1992) were used to assess the course and severity of the patient's psychotic illness during the preceding 2 years.
Relatives' experience
Relatives' experience was conceptualised using the stress-appraisal-coping paradigm. Two components were assessed: appraisal of caregiving, measured using the Experience of Caregiving Inventory (ECI), and psychological distress, measured using the 12-item General Health Questionnaire (GHQ-12). The ECI (Szmukler et al, Reference Szmukler, Burgess and Herrman1996) is a 66-item self-report questionnaire developed specifically for use with relatives of patients with mental illness. Relatives rate the frequency with which they have thought about each item on a five-point Likert scale anchored at ‘never’ and ‘(nearly) always’. The time frame is the preceding 4 weeks. The ECI is divided into 52 items measuring negative appraisal and 14 measuring positive appraisal. The internal consistency and construct validity of the ECI are good (Reference Szmukler, Burgess and HerrmanSzmukler et al, 1996).
The GHQ-12 (Reference GoldbergGoldberg, 1978) is a widely used self-report questionnaire that measures psychological distress. Relatives rate the frequency with which they have experienced 12 indicators of psychological distress on a four-point scale. Again, the time frame is the preceding 4 weeks. Internal and test-retest reliability and validity coefficients (specificity and sensitivity) are satisfactory (Reference Goldberg and WilliamsGoldberg & Williams, 1988).
A straightforward, or ‘S-GHQ’, score was used in which the response ‘same as usual’ is taken to indicate the absence of distress. This is unlikely to be sensitive to feelings of resignation, however, and so an alternative method in which ‘same as usual’ on negative items indicates the presence of distress was, therefore, also used. This is the chronic, or ‘C-GHQ’, score. ‘Caseness’ was determined by applying a cut-off of 3/4 on the S-GHQ and 4/5 on the C-GHQ as recommended by Goldberg et al (Reference Goldberg, Gater and Sartorius1997).
Statistical methods
The representativeness of the sample was tested by comparing eligible patients who did not enter the trial with those who did, using chi-squared tests for categorical data and Mann-Whitney tests for non-normal continuous data.
Logistic regression analysis was used to test which patient characteristics predicted frequent patient-relative contact. To assist with interpretation, and because a linear relationship could not be assumed, continuous and whole number data were converted into categorical data. Patient characteristics were cross-tabulated with contact frequency and chi-squared tests were performed to test for a relationship. A significance value of less than 0.2 was considered indicative of an association requiring further investigation. Characteristics reaching this level of significance were entered into a forward logistic regression analysis. This logistic regression analysis was used to derive a series of adjusted odds ratios (and their 95% confidence intervals) of those characteristics that predicted frequent patient-relative contact (deemed significant at the 5% level).
The same procedure was then used to establish which relative characteristics at baseline were predictive of continued frequent contact at 2-year follow-up. Unlike in the previous analysis, a linear relationship with relatives' appraisal and psychological distress was hypothesised. To test the degree of association between these continuous variables and contact frequency, Mann-Whitney tests were used. The same significance value cut-off of 0.2 was applied.
RESULTS
Recruitment
A profile of the study is given in Fig. 1. Of the 890 patients identified as meeting the UK700 trial eligibility criteria 79% (708) entered. Patient refusal was the main reason for non-entry (21%). There were no significant age or gender differences between patients who entered the trial and patients who did not, but there was some indication that those who entered had been ill for longer (median duration=120 months v. 96 months; U=51899.00; P=0.04).
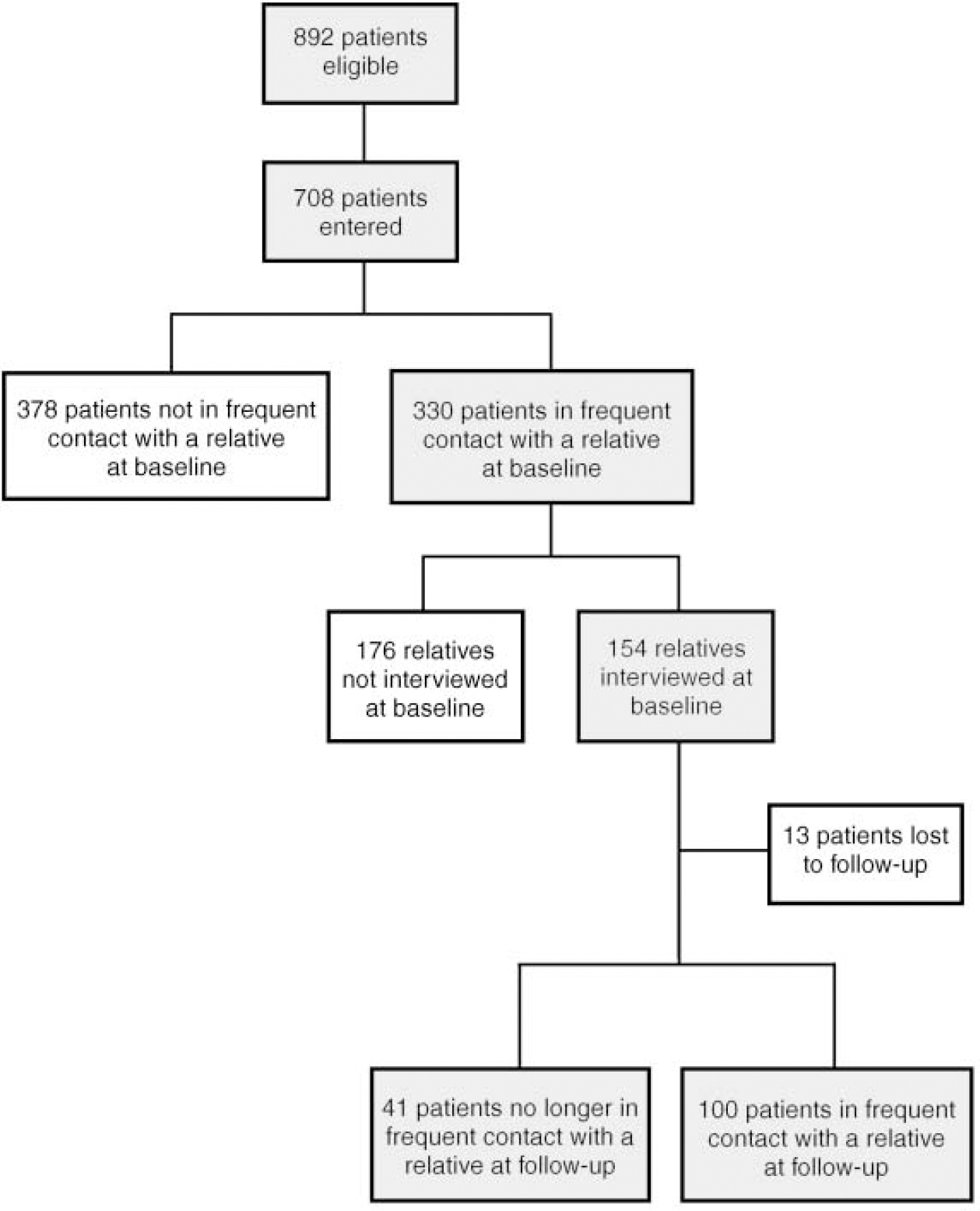
Fig. 1 Study profile.
At baseline almost half (47%) of patients were in frequent contact with a relative. An interview was conducted with 154 (47%) of these relatives. The remaining relatives were not interviewed, mainly because either the patient refused access (20%) or the relative refused to be interviewed (18%). The response rate, although low, is similar to that in other studies (Reference Stueve, Vine and StrueningStueve et al, 1997). At 2-year follow-up 65% of patients continued to have frequent contact with a relative. A small number of patients (8%) were lost to follow-up.
Sample characteristics
Baseline data showed a small preponderance of male patients (57%). Half of the patients were White (52%); most of those remaining were Black-Caribbean (28%). Only 12% were (living as) married. Patients' geographic mobility was relatively low, with only 25% having moved town or district since the onset of their illness. Thirty-three per cent lived alone and a similar proportion lived with family (32%). Patients living in hostel accommodation accounted for most of those living with people other than family (26%). Very few patients (8%) were employed, even though part-time and sheltered work were included. Almost half (49%) had a diagnosis of schizophrenia or schizoaffective disorder. For most, their illness had been lengthy (median=24 years; interquartile range=5-18 years) with considerable periods of time in psychiatric hospital (median=9 months; IQR=5-18 months). Patients' typical illness severity during the preceding 2 years was most commonly described as moderate (47%), although 24% were recovered. Half (52%) of patients had been episodically ill during the preceding 2 years and about two-thirds (37%) had been continuously ill.
Table 1 describes relatives' baseline characteristics. Their psychological distress was high, with 41% scoring above the caseness threshold on the S—GHQ. This contrasts with a community norm of 12% (Reference Goldberg, Kay and ThompsonGoldberg et al, 1976). Once feelings of resignation were taken into consideration, 64% were identified as potential ‘cases’.
Table 1 Characteristics of relatives at baseline (n=154)
| Missing data | Median (IQR) | n (%) | |
|---|---|---|---|
| Age | 50.0 (38-60) | ||
| Gender | |||
| Male | 51 (33.1) | ||
| Female | 103 (66.9) | ||
| Relationship to the patient | 1 (0.6%) | ||
| Parent | 68 (44.2) | ||
| Spouse/partner | 52 (33.8) | ||
| Adult child | 10 (6.5) | ||
| Sibling | 18 (11.7) | ||
| Other | 5 (3.2) | ||
| Living with the patient | 1 (0.6%) | 100 (64.9) | |
| Negative appraisal (ECI negative) | 21 (13.6%) | 79.0 (51-102) | |
| Positive appraisal (ECI positive) | 21 (13.6%) | 24.0 (16-33) | |
| Psychological distress (S—GHQ) | 13 (8.4%) | 3.0 (1-6) | |
| Potential psychiatric ‘cases’ | 63 (40.9) | ||
| Psychological distress (C—GHQ) | 13 (8.4%) | 6.0 (4-7) | |
| Potential psychiatric ‘cases’ | 99 (64.3) |
Patient characteristics predictive of frequent patient—relative contact at baseline
Of the 18 patient characteristics tested, 12 reached a significant level of 0.2 and were entered into a forward logistic regression analysis (age; gender; ethnicity; geographic mobility; diagnosis; duration of psychosis; months in psychiatric hospital since onset; history of parasuicide; current psychopathology; and, in the 2 years preceding entry, months in psychiatric hospital, severity of symptoms and course of illness). Missing data resulted in a sample size of 635.
The adjusted odds ratios of the six characteristics found to be significant predictors of frequent patient—relative contact at baseline are shown in Table 2. For patients aged 45 or older, the odds of frequent contact with a relative were about half those of patients aged under 25, and for female patients the odds of frequent contact with a relative were about twice those of males. For Asian patients the odds of frequent contact with a relative were around three times those of White patients, but there was no significant effect for other ethnic groups. Patients with a diagnosis of schizo-affective disorder or affective psychosis had slightly greater odds of frequent contact with a relative than patients with a diagnosis of schizophrenia, though the confidence interval for the latter only just avoided spanning unity. Patients with more than 18 months in hospital since the onset of their psychotic illness had around half the odds of frequent relative contact compared to those with less than 6 months. The odds of having frequent contact with a relative were also smaller for patients with a history of parasuicide.
Table 2 Patient characteristics predictive of frequent patient—relative contact at baseline (n=635)
| Odds ratio | 95% Confidence limits | ||
|---|---|---|---|
| Lower | Upper | ||
| Age | |||
| 18-24 years1 | |||
| 25-34 years | 0.78 | 0.45 | 1.38 |
| 35-44 years | 0.83 | 0.45 | 1.52 |
| 45-54 years | 0.43 | 0.22 | 0.85 |
| 55-66 years | 0.46 | 0.23 | 0.93 |
| Gender | |||
| Male1 | |||
| Female | 2.01 | 1.42 | 2.83 |
| Ethnicity2 | |||
| White1 | |||
| Black-Caribbean | 0.83 | 0.56 | 1.24 |
| Black-other | 0.91 | 0.52 | 1.58 |
| Asian | 3.14 | 1.20 | 8.16 |
| Other | 1.97 | 0.97 | 4.02 |
| Diagnosis | |||
| Schizophrenia1 | |||
| Schizoaffective disorder | 1.75 | 1.22 | 2.52 |
| Unspecified functional psychosis | 0.65 | 0.29 | 1.43 |
| Affective psychosis | 2.09 | 1.05 | 4.16 |
| Time in psychiatric hospital since onset | |||
| Less than 6 months1 | |||
| 6-11 months | 1.24 | 0.80 | 1.92 |
| 12-18 months | 1.01 | 0.60 | 1.71 |
| More than 18 months | 0.59 | 0.38 | 0.93 |
| Parasuicide | |||
| No1 | |||
| Yes | 0.67 | 0.47 | 0.96 |
The six characteristics predictive of frequent patient—relative contact having been identified, two subsequent questions arose. First, as 69% of patients in frequent contact with a relative were living with family, could these six characteristics be simply predictors of patient-relative co-residence? Second, which patient characteristics predicted contact frequency for patients who did not live with family? To address these issues two further sets of analyses using the baseline data were performed. The associations between each of the 18 patient characteristics and (a) patient-relative co-residence and (b) patient-relative contact frequency for the subgroup of patients who did not live with a relative were tested, using the same methods as before. The results are shown in Tables 3 and 4.
Table 3 Patient characteristics predictive of patient—relative co-residence at baseline (n=615)
| Odds ratio | 95% Confidence limits | ||
|---|---|---|---|
| Lower | Upper | ||
| Gender | |||
| Male1 | |||
| Female | 2.12 | 1.43 | 3.15 |
| Ethnicity2 | |||
| White1 | |||
| Black-Caribbean | 1.17 | 0.74 | 1.83 |
| Black-other | 1.42 | 0.76 | 2.65 |
| Asian | 3.97 | 1.51 | 10.46 |
| Other | 2.34 | 1.09 | 5.06 |
| Marital status | |||
| Single/widowhood1 | |||
| (Living as) married | 16.50 | 7.67 | 35.49 |
| Separated/divorced | 1.08 | 0.67 | 1.74 |
| Time in psychiatric hospital since onset | |||
| Less than 6 months1 | |||
| 6-11 months | 0.82 | 0.51 | 1.34 |
| 12-18 months | 0.74 | 0.41 | 1.33 |
| More than 18 months | 0.43 | 0.26 | 0.72 |
| Parasuicide | |||
| No1 | |||
| Yes | 0.50 | 0.33 | 0.75 |
Table 4 Patient characteristics predictive of frequent patient-relative contact at baseline for patients not living with family (n=448)
| Odds | 95% Confidence | ||
|---|---|---|---|
| ratio | limits | ||
| Lower | Upper | ||
| Age | |||
| 18-24 years1 | |||
| 25-34 years | 0.80 | 0.38 | 1.71 |
| 35-44 years | 0.68 | 0.31 | 1.51 |
| 45-54 years | 0.34 | 0.13 | 0.86 |
| 55-66 years | 0.35 | 0.13 | 0.92 |
| Diagnosis | |||
| Schizophrenia1 | |||
| Schizoaffective | 2.15 | 1.28 | 3.61 |
| Unspecified functional psychosis | 0.72 | 0.23 | 2.24 |
| Affective psychosis | 4.08 | 1.73 | 9.62 |
Five patient characteristics were found to predict patient-relative co-residence at baseline (Table 3). Four (gender, ethnicity, months in hospital since onset and a history of parasuicide) had been predictors of contact frequency. The fifth, marital status, had not been entered into the original regression analyses because (living as) married was synonymous with frequent contact. While (living as) married was also synonymous with patient-relative co-residence, it was included so that its effect could be adjusted for. The remaining two characteristics that predicted frequent contact in the original analysis (age and diagnosis) were the only characteristics found to predict frequent contact at baseline for the subsample of patients who did not live with family (Table 4).
Relative baseline characteristics predictive of continued frequent patient-relative contact at 2-year follow-up
Only three of the eight relative baseline characteristics were entered into the logistic regression analyses. The association between those remaining and continued frequent contact - in particular, relatives' appraisal (negative or positive) and psychological distress (before or after feelings of resignation were taken into consideration) - failed to reach the required 0.2 cut-off.
The regression analysis showed that patients were nearly three times more likely to remain in frequent contact with a relative at follow-up if the relative was aged over 60 at baseline compared to under 40 (Table 5). Similarly, patients were around three times more likely to remain in frequent contact with a relative if they had been living with a relative at baseline. The confidence intervals for both of these odds ratios were, however, fairly wide. The specific patient-relative relationship did not predict frequency of patient-relative contact at follow-up once other characteristics had been adjusted for.
Table 5 Relative baseline characteristics predictive of continued frequent patient-relative contact at follow-up (n=122)
| Odds | 95% Confidence | ||
|---|---|---|---|
| ratio | limits | ||
| Lower | Upper | ||
| Age | |||
| 17-39 years1 | |||
| 40-59 years | 2.34 | 0.89 | 6.13 |
| 60 years or older | 3.87 | 1.22 | 12.29 |
| Living with the patient | |||
| No1 | |||
| Yes | 4.21 | 1.78 | 9.93 |
DISCUSSION
This study establishes that half of patients with severe psychotic disorders do not have frequent contact with a relative and, consistent with previous studies (Reference Mitchell and BirleyMitchell & Birley, 1983), one-third have contact with a relative less than once a week. The theory that relatives avoid frequent contact with patients because they find the situation distressing was not supported, since neither patients' symptom severity nor relatives' experience predicted contact frequency. Nevertheless, before the theory can be rejected, other reasons for the lack of supporting evidence require consideration.
Study limitations
The theory tested in this study relied on two assumptions: first, that the characteristics identified in the literature as associated with ‘burden’ would be associated with experience as it was conceptualised in this study; second, that relatives' experience at baseline would be predictive of contact frequency 2 years later. Neither of these assumptions has been tested. Response bias is a further limitation. Arguably, patients and relatives experiencing difficulties may have been more reluctant to take part, thus biasing the sample in favour of those more likely to remain in contact. Although the anticipated characteristics did not predict contact frequency, several others were found to be important.
Demographic predictors of frequent contact
Female patients were more likely to live with, and thus have frequent contact with, a relative than were male patients. Initial comparisons suggest that this may simply reflect the living circumstances of the general population (Office for National Statistics, 1998); however, these gender differences in the general population are mainly attributable to differences in marital status and lone parenthood. In our study, these factors were adjusted for. The finding is unlikely to be explained by the theory that relatives avoid contact because they find the situation distressing, as evidence indicates that it is relatives of female patients who experience more distress (Reference Winefield and HarveyWinefield & Harvey, 1993).
Another characteristic found to predict patient-relative contact frequency through co-residence was ethnicity. Studies show that ‘White’ relatives experience greater difficulties than ‘minority’ relatives (Reference Horwitz and ReinhardHorwitz & Reinhard, 1995; Reference Stueve, Vine and StrueningStueve et al, 1997). However, most were conducted in the USA, where minority groups are typically ‘Black’ or ‘Hispanic’. That this study did not find differences between ‘White’ and ‘Black’ relatives may indicate that previous findings are culture-specific. Moreover, previous studies provide no information about the experience of ‘Asian’ relatives. ‘Asian’ households tend to be larger than ‘White’ or ‘Black’ households (Office for National Statistics, 1998), which may mean that support is more readily available and, consequently, individual relatives experience less distress. Alternatively, ‘Asian’ relatives may experience no less distress, but instead be more likely to consider providing care to a family member with mental illness to be their duty. Further research comparing experiences of caregiving and feelings of obligation across UK ethnic groups is needed in order to understand the effect of ethnicity on co-residence.
Patients' age was not associated with patient-relative co-residence, but it did predict frequent contact for patients who were not living with family. Older patients were less likely to have frequent contact with a relative than younger patients, which accords with Hirschberg's (Reference Hirschberg1985) finding that older patients have fewer social contacts generally. Relatives of younger patients may be more hopeful of recovery and, consequently, more likely to remain in frequent contact. Alternatively, since older patients' relationships have been exposed to more ‘risks’, they may simply have fewer relatives available to them. If this were true, however, it would be expected that age would also predict patient—relative co-residence, but it did not.
Clinical predictors of frequent contact
The association between patient—relative co-residence (and thus contact frequency) and time in psychiatric hospital is consistent with the literature demonstrating that social networks containing fewer relatives are associated with patients' increased hospital use (Reference HorwitzHorwitz, 1978; Reference HirschbergHirschberg, 1985; Reference Holmes-Eber and RigerHolmes-Eber & Riger, 1990; Reference Becker, Thornicroft and LeeseBecker et al, 1997). It may be that relatives experience more distress if patients spend more time in hospital, and so avoid co-residence and frequent contact. However, as Horwitz (Reference Horwitz1978) asserts, living with a relative may mean that patients are less likely to need lengthy admissions or professionals may perceive the care that relatives provide to be an adequate alternative to hospitalisation. Unfortunately, the data from this study do not allow causality to be attributed. The problem of attributing causality is also pertinent to the association between parasuicide and patient—relative co-residence. It could be argued that relatives find patients' suicide attempts distressing, and so avoid living with them. Alternatively, patients may be less likely to attempt suicide if they live with a relative.
Patients' diagnosis was also associated with contact frequency. Patients who did not live with family were less likely to have frequent contact with a relative if they had schizophrenia than if they had affective or schizoaffective disorder. This may be because the relatives of patients with schizophrenia experience more distress than the relatives of patients with other diagnoses. It is also consistent with the alternative theory that patients' isolation is a consequence of their social withdrawal, since, arguably, social withdrawal is more characteristic of schizophrenia than psychoses with an affective component.
Baseline characteristics predictive of continued frequent contact
Of the relatives' characteristics tested, only co-residence with the patient at baseline and age significantly predicted continued frequent contact at 2-year follow-up. Arguably, as relatives get older they may learn to cope with the patient's illness more successfully, and thus experience less distress. Alternatively, as Greenberg (Reference Greenberg1995) has shown, the relationship between patients and their relatives becomes more reciprocal as relatives get older. A relative may be more likely to maintain frequent contact with a patient if they are relying on the patient for support or companionship.
This study is limited because cause and effect cannot be determined from these data. Moreover, many factors that may be significant determinants of patient—relative contact were not investigated, for example, the professional support that relatives receive. Nevertheless, this study elucidates some of the characteristics that indicate vulnerability to isolation and confirms that a lack of contact with relatives is associated with poorer patient outcomes.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Patients over the age of 45, who are male or suffering from schizophrenia are more vulnerable to isolation from relatives.
-
▪ A lack of frequent contact with relatives is associated with greater psychiatric hospital use and parasuicide.
-
▪ Many relatives experience considerable psychological distress, with two-fifths scoring above the caseness threshold on the General Health Questionnaire.
LIMITATIONS
-
▪ The pattern of patient—relative contact during the 2-year study period was not recorded.
-
▪ Half of eligible relatives were not interviewed because either the patient or relative refused.
-
▪ The assumption of an association between patient symptom severity and relatives' experience as measured in this study is untested.
ACKNOWLEDGEMENTS
The UK700 Group is a collaborative study team involving four clinical centres: Manchester Royal Infirmary: Tom Butler, Francis Creed, Janelle Fraser, Peter Huxley, Nicholas Tarrier and Theresa Tattan; Kings/Maudsley Hospital, London: Thomas Fahy, Catherine Gilvarry, Kwame McKenzie, Robin Murray, Jim Van Os and Elizabeth Walsh; St Mary's Hospital/St Charles' Hospital, London: John Green, Anna Higgit, Elizabeth van Horn, Donal Leddy, Patricia Thornton and Peter Tyrer; St George's Hospital, London: Robert Bale, Tom Burns, Matthew Fiander, Kate Harvey, Andy Kent and Chiara Samele; Centre for Health Economics, York: Sarah Byford and David Torgerson; London (Statistics): Simon Thompson (Royal Postgraduate Medical School) and Ian White (London School of Hygiene and Tropical Medicine).









eLetters
No eLetters have been published for this article.