Introduction
Extensive research has focused on the negative consequences of the COVID-19 pandemic on mental well-being. A number of studies have been especially investigating depressive, anxiety, and posttraumatic stress disorder (PTSD) symptoms arising in the wake of the pandemic and social distancing restrictions.Reference Cénat, Blais-Rochette and Kokou-Kpolou1 However, only little attention has been devoted to positive psychological changes that may develop in the aftermath of a stressful event. Beyond increasing the risk for psychiatric illness, traumatic events may also promote post-traumatic growth (PTG), which refers to thriving on traumatic circumstances while achieving greater appreciation of life and relationships, enhanced spirituality, increased awareness of personal strength, and identification of new possibilities in one’s life. As PTG is experienced by a large number of trauma survivors and associated with a beneficial effect on functioning,Reference Wu, Kaminga and Dai2 addressing the correlates of PTG might be as crucial as addressing those of PTSD.
Healthcare workers (HWs) have been shown to be at elevated risk for COVID-19-associated mental health issues, such as PTSD, depression, anxiety, and suicidal ideation (SI).Reference Pappa, Ntella, Giannakas, Giannakoulis, Papoutsi and Katsaounou3 While several sociodemographic and work-related factors were found to be associated with the propensity to develop mental health problems among HWs, a more comprehensive understanding still lacks the assessment of possible positive factors. A recent study, conducted during COVID-19 pandemic in a sample of US veterans, found that moderate to high levels of PTG were present in slightly less than a half of veterans, with markedly higher percentage among those with COVID-19-associated PTSD symptoms and a significant effect of some PTG dimensions in reducing the odd for SI.Reference Pietrzak, Tsai and Southwick4 In light of these findings, the present study analyzed data from a national sample of HWs gathered during the first wave of COVID-19 in Italy, aiming to evaluate (a) the prevalence of COVID-19-associated PTG among HW with and without COVID19-associated PTSD symptoms and (b) the association between PTG and SI during the first wave of the pandemic.
Methods
This is a cross-sectional, web-based survey study, conducted during the first wave of COVID-19 in Italy. Study procedures are extensively elucidated elsewhere.Reference Gesi, Cirnigliaro and Achilli5 Briefly, answers were collected between April 4 and May 13, 2020, the late phase of the first stay-at-home order in Italy. An invitation letter presenting the research and containing the link to the survey was sent to healthcare institutions, physicians’, and nurses’ associations and circulated through groups of health professionals on social networks and researchers’ direct contacts. Participants gave their informed consent to participate in this study and to have their personal, clinical, and demographic data used for research purposes. Their answers were collected anonymously. The study was conducted in accordance with the Declaration of Helsinki and all participants provided informed consent. The study protocol was approved by the Department of Psychiatry of the ASST Fatebenefratelli-Sacco of Milan as relevant institutional review board for low-risk studies (code: dsm 12–20).
Participants
The inclusion criterion was being an HW actively working in Italy during the pandemic. Any professionals involved in rehabilitation, diagnostic, and administrative activities were invited to participate.
Assessments
Post-traumatic growth
COVID-19-related PTG was assessed using the Posttraumatic Growth Inventory-Short Form (PTGI-SF)Reference Cann, Calhoun and Tedeschi6. One total score and 5 subscores including Appreciation of life, Relating to others, Personal strength, Spiritual change, and New possibilities were calculated. In proceeding with previous studies using the PTGI-SF,Reference Wu, Kaminga and Dai2, Reference Pietrzak, Tsai and Southwick4 item responses were also dichotomized based on moderate or greater endorsement. Endorsement at a moderate or greater level of both items composing each PTGI-SF domain was indicative of endorsement of the whole domain. Additional details regarding the Italian-validated version of PTGI-SF and chosen cut-offs are provided in the Supplementary Material.
COVID-19-related PTSD symptoms
Participants were invited to fill the Impact of Event Scale-Revised (IES-R) if they answered positively to a screening question (In the past month, did you significantly felt on guard/easily startled or detached from others/surrounding or disturbed by repeated/unwanted memories of the COVID-19 epidemic (or something you experienced because of it) or avoidant of situations that reminded you of it (or something you experienced because of it)? While the IES-R is not meant to be a diagnostic tool, a total score of 33 has been indicated as having good diagnostic sensitivity (0.91) and specificity (0.82) compared to a clinical diagnosis.Reference Creamer, Bell and Failla7 The Italian version has also shown optimal psychometric properties and validity.Reference Craparo, Faraci, Rotondo and Gori8
Suicidal ideation
SI was assessed using the Patient Health Questionnaire-9 (PHQ-9). A positive screen for SI was indicated by a response of “several days,” “more than half the days,” or “nearly every day” to the Item 9 (thoughts that you would be better off dead, or of hurting yourself in some way).
Statistical analysis
Descriptive statistics were used to assess frequencies of sociodemographic and clinical characteristics. A multivariable logistic regression analysis was used to examine the association between PTGI and SI, after adjustment for background characteristics and clinical features. Data were analyzed using the SPSS software program, version 27.0 (IBM Corp). All P-values are two-sided, and statistical significance was set at P < .05. Additional details regarding the PTGI-SF are provided in the Supplementary Material.
Results
Of the 948 participants, 931 completed both IES-R and PTGI, and were therefore included in the final sample. As the survey was circulated with the assistance of healthcare institutions, associations, and social networks, the response rate could not be calculated. The mean (SD) age was 45.1 (11.8) years, 592 (63.7%) were females, 441 (47.4%) were from Lombardy, and the remaining 489 (52.6%) were from other Italian regions. In total, 723 (77.7%) were physicians, 104 (11.2%) were nurses, and 103 (11.1%) were a mixed group mostly composed by midwives, rehabilitation personnel, and laboratory technicians. Table 1 shows the sociodemographic and clinical characteristics of all included participants. Regarding IES-R, 553 (58.3%) HWs reported a particularly stressful event. A total of 257 (27.6%) screened positive for COVID-19-associated PTSD symptoms. The median PTGI-SF score was 24.
Table 1. Sociodemographic, Pandemic, and Clinical Characteristics of the Sample and Results of Multivariate Regression Model Examining Their Association with Current Suicidal Ideation

Note: The table shows sociodemographic, pandemic, and clinical characteristics and ORs of suicidal ideation of each factor.
a P-values < 0.05.
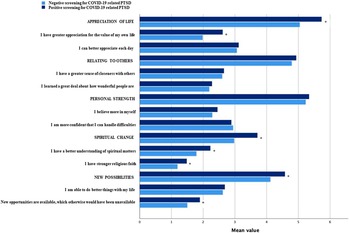
The most endorsed domain of PTGI-SF at a moderate or greater level was Appreciation of life (79.6%), the least endorsed was Spiritual change (41.7%) (Table 1). HWs who screened positive to COVID-19-associated PTSD symptoms scored higher than those who screened negative on the total and Spiritual change, Appreciation of life, and New possibilities domain scores of PTGI-SF (Figure 1).

Figure 1. Comparison between scores at the PTGI of subject with versus without PTSD. The figure shows the comparison between the mean scores in each PTGI-SF domain and subdomain of participants reporting COVID-19-related PTSD symptoms and those not showing PTSD symptoms.
A total of 100 HWs (10.8%) screened positive for SI as assessed through item 9 of the PHQ-9. After adjusting for background and pandemic-associated risk factors, COVID-19-associated improvements in Relating to others domain of PTGI-SF (odds ratio [OR]: .46; 95% confidence interval [CI], .25–.85) was independently associated with lower odds of SI (Table 1).
Discussion
The majority of HWs, mostly females and physicians, participating in this study in the wake of the first outbreak of COVID-19 in Italy, endorsed several dimensions of PTG at a moderate or greater level, the most prevalent being the domains of Appreciation of life (79.6%) and Personal strength (76.9%). This is consistent with 2 small studies reporting about PTG in samples of nurses facing COVID-19 pandemic, where the highest item mean scores were in the domains of Appreciation of life and Personal strength. Reference Cui, Wang, Wang, Ping, Wang and Chen9, Reference Peng, Zi, Yang, Li, Ying and He10 On the other hand, spiritual growth was found to be the PTGI-SF dimension with the lowest mean score, accordingly to recent data from literature.Reference Feingold, Hurtado and Feder11
Albeit concerns have been raised about the contribution of COVID-19 in suicide risk among HWs,Reference Rahman12, Reference Awan, Diwan and Aamir13 no studies evaluated whether PTG stemming from COVID-19 pandemic may exert a protective effect against SI. Greater improvement in Relating to others significantly reduced the odd of SI in our sample. This is consistent with the role of loneliness and lack of connectedness with others in enhancing the risk of suicideReference McClelland, Evans, Nowland, Ferguson and O’Connor14 and provides support to the implementation of interventions targeting PTG-driven relatedness with others to prevent and address SI among HWs. Notably, having a provisional PTSD diagnosis was not related to increased odds of SI, suggesting that such interventions could profitably be addressed to the whole population of HWs, independently from the presence of clinically significant PTSD symptoms. Somewhat in parallel, higher scores in Relating to others domain were not influenced by having a provisional PTSD diagnosis in the comparative analysis. This latter seems to confirm that PTG and PTSD does not develop one from another, nor are mutually exclusive, as they both represent different outcomes that may occur after exposure to a traumatic event.Reference Wu, Zhang, Liu, Zhou and Wei15 From this perspective, PTG may represent an independent target of intervention to promote post-traumatic adjustment and psychological well-being in populations exposed to traumas.
Conclusions
PTG may have a protective role against SI among HWs facing a global pandemic, especially when the dimension of relatedness to others is enhanced in the process of adjustment. Limitations of the study include the lack of information about the response rate of the survey, the use of self-report instruments, and the cross-sectional study design. Moreover, even though the presence of previous mental disorders was assessed as possible confounding factor (25.2% in our sample), the occurrence of psychopharmacological/psychological treatments was not assessed and might have biased the results. Lastly, since our data were collected in a relatively precocious phase of COVID-19, follow-up data on the long-lasting effects of the pandemic and the longitudinal course of PTG among HWs are needed. Studies replicating these findings and assessing changes in PTG and SI over time are warranted, as well as developing evidence-based interventions enhancing PTG and helping HWs to manage stressors during and beyond COVID-19 pandemic.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1092852923002493.
Acknowledgements
Fondazione Romeo ed Enrica Invernizzi.
Author contribution
Supervision: B.D.; Writing – original draft: G.C., F.L., F.A., C.G., M.B., M.D.M., M.C., R.C.; Conceptualization: F.L., C.G., M.D.M.; Data curation: F.L., C.G., M.D.M.; Formal analysis: F.L., C.G., M.D.M.; Writing – review & editing: R.C.
Financial support
No specific funding was received for this article.
Disclosure
The authors declare that they have no known competing financial or nonfinancial interests to disclose in relation to the present article.