1. Introduction
Pregnancy is a normal physiological process, yet complications that increase morbidity and mortality for the mother and baby occur in up to 20% of pregnancies [Reference Bernstein, VanBuren, DeCherney, Nathan, Laufer and Roman1]. The purpose of prenatal care is to ensure a successful pregnancy outcome when possible, including the delivery of a live, healthy fetus [Reference Bernstein, VanBuren, DeCherney, Nathan, Laufer and Roman1]. Prenatal care includes history taking, physical examinations, laboratory tests and prenatal ultrasound tests [Reference Bernstein, VanBuren, DeCherney, Nathan, Laufer and Roman1]. Prenatal care is an important predictor of outcomes for both mothers and babies [Reference Kelly, Danielsen, Golding, Anders, Gilbert and Zatzick2–Reference Swigonski, Skinner and Wolinsky4].
Women with psychiatric disorders are as likely as healthy mothers to become pregnant, and have an even higher rate of unplanned pregnancies [Reference DeCesaris5, Reference Oyserman, Mowbray, Meares and Firminger6]. Women with schizophrenia and affective disorders have increased risks for pregnancy complications [Reference Jablensky, Morgan, Zubrick, Bower and Yellachich7]. Several studies examined utilization of prenatal care in women with psychiatric disorders. Although most of these studies have found inadequate utilization of prenatal care in women with psychiatric disorders [Reference Lin, Chen and Lee8, Reference Nguyen, Faulkner, Frayne, Allen, Hauck and Rock9], others have not [Reference Vigod, Kurdyak, Dennis, Gruneir, Newman and Seeman10]. Poor compliance with prenatal care in women with psychiatric disorders has been associated with adverse perinatal outcomes, including preterm births, low birth weight and small for gestational age babies compared to controls [Reference Nguyen, Faulkner, Frayne, Allen, Hauck and Rock9, Reference Vigod, Kurdyak, Dennis, Gruneir, Newman and Seeman10]. Most of the previous studies have focused on severe mental illness, specifically schizophrenia, bipolar disorder and major depression. Although one study included a group of patients with non-psychotic mental illness [Reference Nguyen, Faulkner, Frayne, Allen, Hauck and Rock9], the group was too heterogenic (including 15 women with major depressive disorder.
5 women with anxiety disorders, 12 with emotionally unstable personality disorder, 3 with post-traumatic stress disorder, 2 with severe adjustment disorder and 1 with anorexia nervosa) to permit any clear conclusions regarding these disorders. In previous studies, prenatal care has largely been considered in terms of number of prenatal visits (NPV) and the time of initiation of prenatal care. Previous studies suggest that high NPV may be associated with increased risk for negative outcomes such as induction of labor and cesarean delivery possibly due to additional testing and unnecessary interventions [Reference Carter, Tuuli, Caughey, Odibo, Macones and Cahill11]. However, the issue of high NPV in women with psychiatric disorders has not been previously addressed. None of the previous studies included mothers with multiple gestation pregnancies (MGP), a high-risk subgroup which deserve special monitoring and treatment as part of prenatal care [Reference Ayres and Johnson12]. Moreover, to the best of our knowledge, compliance with laboratory prenatal tests in women with psychiatric disorders has not been previously examined. As laboratory studies such as infectious and genetic screening and metabolic studies (e.g., oral glucose tolerance test) are necessary in order to achieve to primary goal of prenatal care of ensuring successful pregnancy outcomes, our lack of knowledge in this regard is of major clinical concern. Finally, it is unknown whether psychiatric treatment during pregnancy can moderate the risk for non-compliance with prenatal care. To further address these issues, we conducted a retrospective cohort analysis of utilization of prenatal care in women with psychiatric disorders and healthy controls in the Tel-Aviv district of Clalit Health Services (CHS), the largest HMO in Israel, using data from 2004 to 2014.
2. Method
2.1. Procedure
In this study we analyzed patient compliance with prenatal care using the computerized database of the CHS, the largest HMO in Israel. The Tel-Aviv district of the CHS includes about 310, 000 members, which represent about 40% of the district's population. The computerized database contains demographic data, number of visits to general practitioners and specialists, medical and psychiatric diagnoses, medications, laboratory tests, and results of ultrasound and imaging studies. The CHS database has been previously used in several studies (e.g., [Reference Birkenfeld, Dreiher, Weitzman and Cohen13–Reference Melamed, Horowitz, Elhayany and Vinker15]), and the validity of its diagnoses was found to be high [Reference Birkenfeld, Dreiher, Weitzman and Cohen13, Reference Rennert and Peterburg14]. Inclusions criteria were: (1) women, (2) at least 1 live birth from October 2004 to October 2014 (i.e., the study period). Exclusion criteria were: (1) Teenage mothers (<18 years-old), (2) women with intellectual disability, (3) women with substance use disorders.
The study was approved by the CHS Institutional Review Board (IRB). The information received by the authors did not include identifying personal information, and the IRB approved exemption from Informed Consent (retrospective data analysis).
2.2. Subjects
Included were 5395 women. The Study group consisted of 1043 women with psychiatric disorders of mean age 30.9 ± 5.2 years (range 18–41) who have had overall 1680 pregnancies (median 2.0 ± 0.9) during the study period. The Control group consisted of 4352 women without neurological or psychiatric disorders of mean age 27.8 ± 2.9 years (range 18–46), who have had overall 5765 pregnancies (median 1.0 ± 0.9) during the study period. The psychiatric diagnoses in the database were assigned by psychiatrists, neurologists and general practitioners according to the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) based on patient examination, coded for statistical purposes according to the 9th edition of the International Classification of Diseases (ICD-9, this is common practice in Israel). Neurological disorders were assigned by neurologists and general practitioners according to ICD-9. Diagnoses are active until cancelled by a physician seeing the patient who determines that they are no longer active. Psychiatric disorders included in the study were depressive disorders (major depressive disorder, dysthymic disorder, depressive disorder NOS), anxiety disorder (generalized anxiety disorder, panic with or without agoraphobia, social phobia), bipolar disorder 1 and 2, schizophrenia, and other psychotic disorders (delusional disorder, brief psychotic disorder, psychotic disorder NOS), using the appropriate codes from ICD-9. Psychiatric disorders codes excluded were all recorded disorders encompassed by the “Mental Disorders” section in ICD-9 (codes 290–319). Neurological disorders codes excluded were all diagnoses encompassed by the “Disease of the Nervous System” (ICD-9 codes 320–359).
The distribution of diagnoses in the study group was as follows (percentages refer to the study group): Depressive disorders (without anxiety disorders, Depression-only group), N = 395 (37.9%); Anxiety disorders (without depressive disorders, Anxiety-only group), N = 241, (23.1%); Depressive and Anxiety disorders (Depression & Anxiety group), N = 225 (21.6%); Bipolar disorder, N = 19 (1.8%); Schizophrenia, N = 70 (6.7%); and Other Psychotic disorders, N = 93 (8.9%). Data of the study group were first analyzed under the broader categories of depressive and anxiety disorders vs. schizophrenia and psychotic disorders, and then as separate diagnostic subgroups. The bipolar disorder subgroup was too small to attain statistical significance and was therefore not included in the analyses. For demographic data of subjects, see Table 1.
2.3. Measures of compliance
The Israeli Ministry of Health (IMH) recommends, in addition to visits to the gynecologist (the ideal number of which is not specified in the IMH recommendations), that routine prenatal care should include the following: screening for genetic diseases (pre-conception or early during pregnancy); complete blood count, blood type, fasting glucose levels, screening for syphilis and a urine chemistry and culture (immediately after the first prenatal visit and before week 12); several ultrasound tests during pregnancy (during first weeks and at the 1st and 2nd trimester); maternal serum markers (e.g., alpha-fetoprotein, aFP); and an oral glucose tolerance test (OGTT, weeks 24–28) [16]. Utilization of prenatal care was assessed in our study with regard to the following: number of prenatal visits (NPV); OGTT and aFP. NPV is the main measure that was assessed in previous studies. Laboratory tests such as aFP and OGTT are part of prenatal care [Reference Bernstein, VanBuren, DeCherney, Nathan, Laufer and Roman1], but have not been previously assessed. Compliance with prenatal ultrasound and genetic tests was considered but not assessed in our study because undergoing these tests via private clinics has become very popular in Israel, so a crucial percentage of the data regarding ultrasound tests was unavailable to us. Compliance with prenatal laboratory tests (i.e. aFP, OGTT) was assessed using dichotomous variables (having done the test or not). We defined compliance with prenatal care visits as NPV within 4–10, considering 4 as the minimum adequate NPV for even extreme prematurity (22-weeks’ gestation) according to the Kessner Index [Reference Kessner, Singer, Kalk and Schlesinger17], and 10 as an adequate NPV above which negative outcomes have been described in the literature [Reference Carter, Tuuli, Caughey, Odibo, Macones and Cahill11]. Because it is unclear what should be the minimal NPV for low risk women, we defined underutilization as absence of prenatal care visits (NPV = 0). Overutilization was examined using several criteria: (1) Exceeding 10 visits [Reference Carter, Tuuli, Caughey, Odibo, Macones and Cahill11]; (2) Exceeding the standard 14-visit schedule [18]; and (3) Exceeding 20 visits (more than once every two weeks considering a 40-week gestation).
Table 1 Demographic data of the subjects in our sample* (N = 5395).
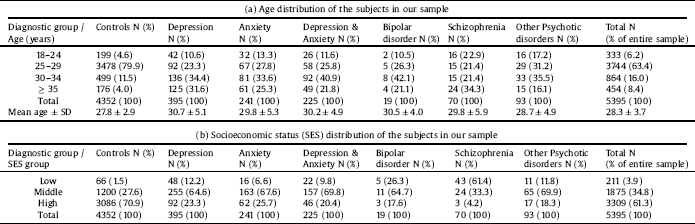
* Data refers to the first pregnancy of subjects in the database.
2.4. Age-group variable
The difference in mean age between the study and control groups was statistically significant (30.9 ± 5.2 vs. 27.8 ± 2.9, respectively, t = − 26.4, p < 0.001). Subjects' age was not normally distributed (Shapiro-Wilk tests' p < 0.001 for the study and control groups). Therefore, and based on the previous literature [Reference Chen and Lin19], we defined the age variable as categorical, assigning each subject to one the following groups: 18–24 years-old, 25–29 years-old, 30–34 years-old, and ≥35 years-old (see Table 1a), and considered 25–29 years-old mothers as the reference group. The categorical age-group variable was included in all further analyses in order to assure significance of findings beyond age differences.
2.5. Socioeconomic status (SES)-group variable
We defined a 3-level SES variable based on exemption from Social Security Tax (SST) and billing approval by the CHS. Exemption from payment of the SST in Israel is usually based on having a low income or documented disability, or otherwise belonging to specific populations of lower SES (e.g. new immigrants), and is considered a strong indication of a low SES. Additionally, the CHS allows some of its members to pay for healthcare services by means of direct billing of their bank account, which is usually an indication of higher SES. Based on these data, each patient was assigned to one of the following groups (Table 1b): High (no SST exemption, direct billing approved), Middle (no SST exemption, direct billing not approved) or Low SES (exemption of SST payment, regardless of billing approval). The modal category was middle SES (68.9%) for the study group and high SES for controls (71.3%), a statistically significant difference (χ2(2) = 1617.6, p < 0.001). The SES-group variable was included in all further analyses in order to assure significance of findings beyond SES differences.
2.6. Statistical analysis
SPSS ver. 22 (IBM Inc., Chicago, IL) was used for statistical analysis. Demographic data are presented as mean or median ± standard deviation as appropriate. Considering the nature of the data as repeated measures (pregnancies) with unbalanced design (the total number of pregnancies and the time intervals between them varies per subject), we conducted Generalized Estimating Equation (GEE) analyses of prenatal care utilization as criterion-derived dichotomous dependent variables (defined above). The diagnostic subgroup was the main independent, assessed once with and once without the effects of age, SES, and MGP, yielding crude and adjusted odds ratios compared to controls (cOR and aOR, respectively). The effects of diagnostically relevant psychopharmacological treatment (e.g. antipsychotics for schizophrenia) during pregnancy were analyzed separately. The models were conducted once with a broad 3-level diagnostic group variable (depressive and anxiety disorders, schizophrenia and psychotic disorders, and controls) and subsequently for specific diagnostic subgroups as appropriate.
3. Results
3.1. Oral glucose tolerance test (OGTT) (Table 2)
Women with depression and anxiety were more likely than controls to not comply with OGTT (cOR = 1.6, p < 0.0005, 95% CI = 1.4–1.8, aOR = 1.4, p < 0.0005, 95% CI = 1.1–1.6). The risk was higher for the depression-only group vs. controls (cOR = 1.6, p < 0.0005, 95% CI = 1.3–1.9, aOR = 1.4, p = 0.002, 95% CI = 1.1–1.7) than for the anxiety-only group vs. controls (cOR = 1.2, p=0.03, 95% CI = 1.0–1.6, aOR non-significant, p = 0.42). The depression & anxiety group had a nearly 2-fold increase in risk for non-compliance (cOR = 1.9, p=0.002, 95% CI = 1.3–3.2, aOR = 1.7, p < 0.0005, 95% CI = 1.3–2.1), similarly to women with schizophrenia (cOR = 2.0, p < 0.002, 95% CI = 1.3–3.2, aOR = 1.8, p=0.01, 95% CI = 1.1–2.9).
Age had no effect on the risk for non-compliance, except for a decreased risk in 30–34 years-old compared to 25–29 years-old (OR = 0.7, p=0.001, 95% CI = 0.5–0.8). Compared to women of high SES, women of middle SES were twice as likely to not comply with OGTT (aOR = 2.1, p < 0.0005, 95% CI = 1.9–2.4), with marginally-significant results for the low- vs. high-SES group (aOR = 1.3, p = 0.069, 95% CI = 1.0–1.8). The risk for non-compliance decreased in the second and third pregnancies of the subjects compared to their first (aOR = 0.3, p < 0.0005 for both). Women with MGP were 1.4 times more likely to not comply with OGTT (p < 0.0005, 95% CI = 1.2–1.6). Women who received psychopharmacological treatment during pregnancy were marginally less likely not to comply with OGTT compared to women who did not receive treatment (GEE OR = 0.82, p = 0.068, 95% CI = 0.67–1.01).
Table 2 Compliance with Oral Glucose Tolerance Test (OGTT) in our sample (N = 5395).
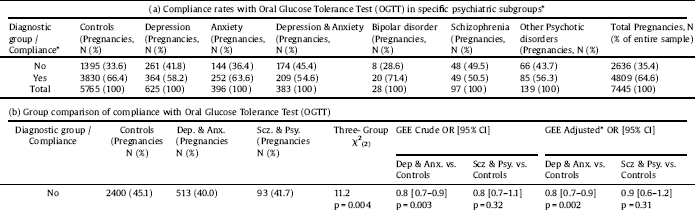
* See text for specific subgroup comparisons.
3.2. Serum alpha feto-protein test (aFP) (Table 3)
Women with depressive and anxiety disorders had lower risk for non-compliance with serum aFP than controls (cOR = 0.8, p = 0.003, 95% CI = 0.7–0.9, aOR = 0.7, p = 0.001, 95% CI = 0.6-0.9). Women of the depression-only group did not differ from controls, whereas patients of the anxiety-only group had significantly lower risk for non-compliance compared to controls (aOR = 0.6, p = 0.001, 95% CI = 0.5–0.8). The lower risk compared to controls was attenuated in the depression & anxiety group (aOR = 0.7, p = 0.044, 95% CI = 0.6–1.0). Women with schizophrenia and psychotic disorders did not differ from controls. The risk for non-compliance was the same for the second and third pregnancies of the subjects compared to their first, but was significantly higher for the fourth (aOR = 3.1, p < 0.0005, 95% CI = 1.8–5.2) and fifth pregnancy (aOR = 4.8, p = 0.015, 95% CI = 1.4–17.2). Age, SES and MGP had no significant effect. Women who received psychopharmacological treatment during pregnancy were more likely to comply with aFP compared to women who did not receive treatment (GEE OR = 1.4, p = 0.002, 95% CI = 1.1–1.7).
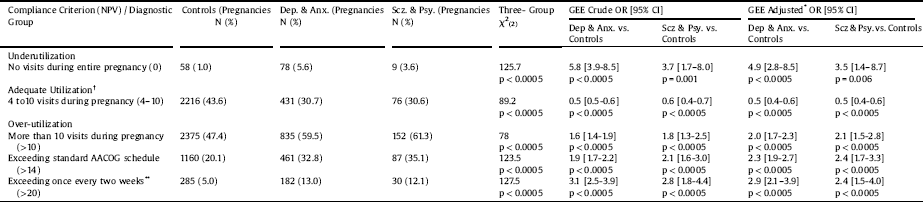
3.3. Number of prenatal visits (NPV) (Table 4)
Women with psychiatric disorders were more likely than controls to exhibit both under- and overutilization of prenatal care visits (Table 3). The risk for underutilization compared to controls was higher in the depression-only group (aOR = 4.8, p < 0.0005, 95% CI = 2.5–9.5) than in the anxiety-only group (aOR = 3.7, p < 0.0005, 95% CI = 1.9–7.4). The highest risk was found in the depression & anxiety group compared to controls (aOR = 6.5, p < 0.0005, 95% CI = 3.2–13.0), which was higher than that of women with other psychotic disorders compared to controls (aOR = 3.7, p < 0.0005, 95% CI = 1.9–7.4). The risk for underutilization in the schizophrenia group was marginally significant (cOR = 3.2, p=0.052, 95% CI = 1.0–10.3, aOR = 3.4, p = 0.07, 95% CI = 0.9-12.8). There was no statistically significant difference in the risk for underutilization in women who received psychopharmacological treatment during pregnancy (GEE OR p > 0.05).
The risk for over-utilization (NPV > 20) was higher in the anxiety-only group vs. controls (aOR = 3.2, p < 0.0005, 95% CI = 2.1–4.8) than in the depression-only group (aOR = 2.4, p < 0.0005, 95% CI = 1.7–3.5). The highest risk compared to controls was in the depression & anxiety group (aOR = 3.5, p < 0.0005, 95% CI = 2.4–5.3), which was higher than the risk in patients with schizophrenia (aOR = 3.3, p=0.002, 95% CI = 1.6–7.0) and other psychotic disorders (aOR = 1.9, p = 0.04, 95% CI = 1.0–3.5) compared to controls. The risk was higher in women who received psychopharmacological treatment during pregnancy (GEE OR = 2.2, p < 0.0005, 95% CI = 1.7–2.9).
In the analysis for adequate utilization, 18–24 year-old mothers were more likely than 25–29 years-old to adequately utilize prenatal care (aOR = 1.3, p = 0.017, 95% CI = 1.0–1.6). Regarding parity, the likelihood for adequate utilization increased with each consecutive pregnancy, rising from aOR = 1.6 in the second (p < 0.0005, 95% CI = 1.4–1.8) to aOR = 1.8 in the third (p < 0.0005, 95% CI = 1.5–2.3) and aOR = 3.1 (p < 0.0005, 95% CI = 1.9–5.0) in the fourth pregnancy. SES and MGP had no significant effect on NPV.
Table 3 Compliance with alpha-fetoprotein (aFP) in our sample* (N = 4823).
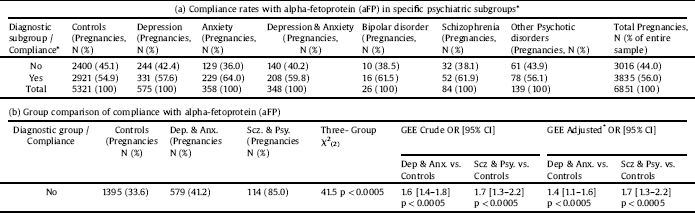
* See text for specific subgroup comparisons.
Table 4 Utilization of Prenatal Visits in Our Sample.
4. Discussion
4.1. Laboratory prenatal tests
In this study, we examined compliance with prenatal care in women with and without psychiatric disorders. After adjusting for age, socioeconomic status, parity and multiple gestations, we found that women with psychiatric disorders had an increased risk for non-compliance with OGTT compared to controls. The risk for non-compliance was slightly increased in the anxiety-only group, higher in the depression-only group, and reached a two-fold increase in the schizophrenia and the depression & anxiety groups. The increased risk for non-compliance with OGTT is consistent with previous studies showing inadequate utilization of prenatal care in women with schizophrenia [Reference Lin, Chen and Lee8, Reference Nguyen, Faulkner, Frayne, Allen, Hauck and Rock9] and poor compliance with medical care in general in depressed patients [Reference DiMatteo, Lepper and Croghan20]. This may be due to higher prevalence of psychosocial risk factors such as lack of social support, unintended pregnancies, attitudes toward health professionals and financial difficulties [Reference Lin, Chen and Lee8]. In the current study we found that women of high SES were more likely to comply with OGTT than women of middle SES, with marginally significant results for low SES, but psychiatric disorders and SES contributed independently to the risk for non-compliance. In addition to psychosocial factors, psychiatric disorders may directly affect motivation for care [Reference Kelly, Danielsen, Golding, Anders, Gilbert and Zatzick2], which may lead to inadequate utilization of prenatal care [Reference Kalmuss and Fennelly21]. Anhedonia, a symptom of both depression and schizophrenia [Reference Pelizza and Ferrari22], seems particularly relevant in this regard. In a postpartum study of low-income women in New-York, the most common reasons given for inadequate utilization of prenatal care were: “feeling depressed and not up to going for care”, and “needing time and energy to deal with other problems” [Reference Kalmuss and Fennelly21].
Interestingly, in contrast to their lower compliance with OGTT, we found that women with schizophrenia and depression did not differ from controls in compliance with aFP. It may be that the difference in compliance between these tests lies in the mother's perception of their objective. Whereas oral glucose tolerance test may be perceived by mothers as merely concerning their own health (risk for diabetes), the term alpha-fetoprotein may alert mothers that the test is for the baby. The similar risk for non-compliance with aFP in women with schizophrenia and depression compared to controls may in fact represent an abnormally normal finding, stemming from increased anxiety for the fetus in women with psychiatric disorders. The fact that anxiety disorders were associated with greater compliance with aFP compared to controls further supports this hypothesis. In contrast, anxiety disorders contributed positively to the risk for non-compliance with OGTT. As discussed above, this may be understood in terms different behavioral responses of mothers to anxiety about their own health and the health of the fetus. The existing literature suggests that both healthcare avoidance and over-seeking of healthcare can result from health-related anxiety [Reference Abramowitz, Olatunji and Deacon23], depending in part on the degree to which one is preoccupied with worries about the potential consequences of not seeking medical care [Reference Salkovskis and Warwick24]. If one manages to suppress such thoughts, one avoids; if one ruminates over catastrophic consequences, one over-seeks [Reference Salkovskis and Warwick24]. It is arguably easier to dismiss concerns about one's own health than to disregard such concerns about the wellbeing of one's future baby. Indeed, the “fear of having a physically or mentally handicapped child” was found to be a major factor of anxiety in pregnancy [Reference Huizink, Mulder, Pascale, Roble de Medina, Visser and Buitelaar25]. This may explain why anxiety may lead to a pattern of low utilization of OGTT but high utilization of aFP.
4.2. Prenatal visits
After adjusting for possible confounders, we found that women with psychiatric disorders were more likely to exhibit both absence and very high utilization of prenatal care visits. These patterns may stem from similar factors of motivational deficits and health anxiety discussed above. Although the complete absence of prenatal care visits during pregnancy is arguably abnormal for any pregnant woman, we acknowledge that over-utilization may in some cases be due to objective demands of high-risk pregnancies. For instance, depression and anxiety have been associated with fetal growth retardation [Reference Bonari, Pinto, Ahn, Einarson, Steiner and Koren26] and preeclampsia [Reference Kurki, Hiilesmaa, Raitasalo, Mattila and Ylikorkala27], and schizophrenia has been associated with placental abnormalities, antepartum hemorrhages and fetal distress [Reference Jablensky, Morgan, Zubrick, Bower and Yellachich7] −complications that may necessitate more frequent prenatal visits. High utilization is therefore best seen in terms of a combination of the overall morbidity of the individual and over-utilization of prenatal care visits.
4.3. Parity and multiple gestational pregnancies
Our study is the first to show that parity decreases the risk for non-compliance with OGTT. Further, our study is the first to show a significant increase in the likelihood for adequate utilization of prenatal care visits with each consecutive pregnancy of the mother. The fact that parity had no effect of aFP beyond the effects of age may be due to the greater emphasis that is put on the importance of aFP with increasing age. Regarding multiple gestation pregnancies, although we found an increased risk for non-compliance with regards to OGTT, but not to aFP and NPV. Further studies are needed in order to replicate and elucidate the effects of multiple gestation pregnancies on utilization of prenatal care.
4.4. Age and SES group differences
In our study, women with psychiatric disorders were on average 3.1 years older than controls, and were more likely to be assigned to middle or low SES categories. It should be noted that women with schizophrenia had also the highest rate of younger (18–24 years-old) mothers, which may point to unplanned pregnancies [Reference DeCesaris5, Reference Oyserman, Mowbray, Meares and Firminger6]. Age and SES variables were included in all analyses, and findings regarding compliance with prenatal care were significant beyond differences in these variables.
4.5. The effects of psychopharmacological treatment
Women who received psychopharmacological treatment were more likely to comply with aFP, and were marginally more compliant with OGTT. However, they were at risk for high utilization of prenatal visits. A possible explanation for these findings is that psychopharmacological treatment increases patient compliance, but also increases the likelihood that more rigorous prenatal visits will be requested either by the doctor or by the patient (or both) due to possible teratogenic risk that many psychiatric medications carry. Overall, it seems that psychiatric treatment during pregnancy increases patient compliance with prenatal care in women with psychiatric disorders, although more studies are clearly needed.
4.6. Strengths, limitations and conclusion
Our study adds to the existing literature in several ways. It is the first study to directly compare compliance with prenatal care in women suffering from several distinct groups of psychiatric disorders and controls in the same study, and the first to examine the effects of psychopharmacological treatment during pregnancy on compliance with prenatal care. Moreover, it is the first analysis of compliance with laboratory prenatal tests (i.e., OGTT and aFP) in women with psychiatric disorders. Unlike previous studies that either randomly selected one of the pregnancies or simply analyzed the first pregnancy, we employed GEE analysis with consecutive pregnancies as repeated measures. Unlike previous studies, multiple gestation pregnancies were taken into account in our analysis. Moreover, our study is the first to address the issue of both absent and very high utilization of prenatal care visits.
The current study has several limitations. First, the retrospective nature of our analysis precludes any definite conclusions regarding causality. Second, although some possible confounders and mediators were taken into account, such as age, socioeconomic status, multiple gestation pregnancies and previous pregnancies, data regarding other factors were not available to us and were thus not taken into account. These include partner support, maternal medical comorbidities obstetric and neonatal outcomes of previous pregnancies. These factors may limit the generalizability of our findings, and other studies are needed in order to confirm them. Moreover, our data sample did not include maternal and neonatal outcomes that would allow to directly correlate inadequate compliance and obstetric complications; however, this has been previously established in the previous literature. Finally, as in previous studies, the severity of psychiatric disorders and the differential impact of disorder onset (e.g. chronic prenatal morbidity versus perinatal exacerbation) were not available to us due to the retrospective nature of the data.
In conclusion, our finding suggest that women with psychiatric disorders exhibit low utilization of tests perceived for the wellbeing of the mother (i.e., OGTT) but high utilization of tests for the wellbeing of the fetus (i.e., aFP), and exhibit patterns of both absence and very high utilization of prenatal care visits. There is an increased risk for non-compliance with OGTT in women with depression and schizophrenia, but not anxiety. Women with anxiety are more compliant with aFP than controls, whereas women with depression and schizophrenia do not differ from controls in compliance with aFP. Women who receive psychopharmacological treatment during pregnancy are more likely to comply with aFP and may be more compliant with OGTT, and exhibit high utilization of prenatal visits. Healthcare professionals should be aware of the risks of both unusually-low and unusually-high utilization of prenatal care in women with psychiatric disorders and strive to improve compliance with psychiatric treatment in order to improve prenatal care utilization. Further studies are indicated.







Comments
No Comments have been published for this article.