Introduction
There is a large body of literature documenting the high prevalence of mood disorders in acute coronary syndromes (ACS)Reference Lichtman, Froelicher and Blumenthal 1 and their associations with poor therapeutic adherence, higher frequency of relapses, and increased mortality.Reference Carney and Freedland 2 , Reference Vaccarino, Badimon and Bremner 3 Mood disturbances may consist of major or minor depressive episodes, chronic depression, and demoralization.Reference Carney and Freedland 2 , Reference Rafanelli, Roncuzzi and Milaneschi 4 , Reference Kuhlmann, Arolt and Haverkamp 5 The latter is characterized by a sense of subjective incompetenceReference de Figueiredo and Frank 6 and it may co-occur with depression or be independent, as demoralization was found to be distinguishable from minor depressionReference Rafanelli, Roncuzzi and Finos 7 -Reference Rafanelli, Offidani, Gostoli and Roncuzzi 10and dysthymia.Reference Rafanelli, Milaneschi, Roncuzzi and Pancaldi 9 , Reference Rafanelli, Offidani, Gostoli and Roncuzzi 10 Key depressive symptoms, such as disturbances in mood, fatigue, cognitive complaints, poor quality of sleep or appetite, are common in ACS, and they substantially account for patients’ quality of life and functioning impairments.Reference Vaccarino, Badimon and Bremner 3 The hypothesis that certain clusters of symptoms could be more relevant for cardiac prognosis than others, in terms of “cardio-toxicity”Reference Rafanelli, Sirri, Grandi and Fava 11 has been supported by the recent position paper of the European Society of Cardiology,Reference Vaccarino, Badimon and Bremner 3 which recognizes that specific subtypes of depression (treatment-resistant, post-ACS, and somatic symptoms-related depression) might be more strongly associated with ACS risk than others, thus confirming that a qualitative evaluation of depression (and its subsequent treatment) would improve prognosis.
According to this clinical perspective, it is necessary to develop a broad and sensitive assessment of depression in cardiac units. It has been underlined that traditional psychiatric nosography alone, such as that reported in the Diagnostic and Statistical Manual of Mental Disorders (DSM), might not be able to provide sufficient clinical information.Reference Fava, Rafanelli and Tomba 12 The customary clinical taxonomy in psychiatry, in fact, does not take into consideration specific clinical features that may demarcate major prognostic and therapeutic differences among patients who otherwise would be misleadingly classified into the same diagnostic category or whose affective symptoms would eventually gone unrecognized.Reference Fava, Rafanelli and Tomba 12 It has been suggested that the assessment might take advantage from a clinimetric approach that reflects the clinical process underling decisions in practice, providing a framework for the reproduction and standardization of clinical intuitions.Reference Fava, Rafanelli and Tomba 12
The purpose of this study was to broaden the evaluation of depressive symptomatology in ACS patients by using a clinimetric approach in order to identify clinical phenomena such as symptom severity, timing of phenomena, and comorbid conditions relevant to cardiac disease. More specifically, the current investigation was aimed at identifying not only traditional psychiatric nosography (ie, major/minor depression and dysthymia), but also severity and longitudinal course of depressive symptomatology, as well as other qualitatively different psychological conditions, such as demoralization, type A behavior and psychological well-being.
Methods
Sample
Seven hundred and forty consecutive patients who suffered from a first episode of ACS (ie, acute myocardial infarction or unstable angina) were screened by the cardiologists at the Divisions of Cardiology of two hospitals in Northern Italy (Molinette Hospital in Turin and Maggiore Hospital in Bologna). Acute myocardial infarction was documented by cardiac symptoms (ie, presence of acute chest-, epigastric-, neck-, jaw-, or arm- pain, discomfort or pressure without apparent noncardiac source) and signs (ie, acute congestive heart failure or cardiogenic shock in the absence of non-CHD causes), associated with ECG findings (characteristic evolutionary ST-T changes or new Q waves) and/or cardiac biomarkers (blood measures of myocardial necrosis, specifically CK, CK-MB, CK-MBm, or troponin, cTn). Instable angina was acknowledged by cardiac symptoms (chest pain lasting less than 20 minutes) with likely ECG findings (ST-segment depression and abnormal T-wave) in absence of myocardial necrosis biomarkers. Among the initial 740 patients, 288 agreed to undergo the psychological assessment and thus were enrolled in the present study.
Study design
The whole sample (N = 288) was assessed at baseline for screening purposes related to a randomized controlled trial, the TREATED-ACS Study.Reference Rafanelli, Gostoli and Buzzichelli 13 The first 100 consecutive depressed (according to DSM-IV-TR) 14 and/or demoralized (according to Diagnostic Criteria for Psychosomatic Research—DCPR)Reference Fava, Freyberger and Bech 15 patients entered the trial and were reassessed at the end of the interventions sessions, and after 3, 6, 12, and 30 months. In this latter group, patients were randomly assigned to either a sequential combination of cognitive-behavioral therapy (CBT) and well-being therapy (WBT)Reference Fava 16 or to clinical management (CM), an active form of control in which specific psychological strategies were proscribed, albeit CM patients received the same amount of time and attention as CBT/WBT patients. The full study protocol and outcomes are detailed in a previous work.Reference Rafanelli, Gostoli and Buzzichelli 13 The sequential combination of CBT and WBT was associated with a greater significant improvement in depressive symptoms (from pre- to post-treatment) than that reported in CM, as indicated by a larger effect size. However, the superiority of CBT/WBT group faded starting from 3-month follow-up. In both groups, the improvement of depressive symptomatology persisted up to 30-month follow-up. Treatment was also related to a significant amelioration of biomarkers (platelet count, HDL, and D-dimer), whereas both groups showed similar frequencies of adverse cardiac events.Reference Rafanelli, Gostoli and Buzzichelli 13
The study was approved by the institutional review board of the ethics committees of Bologna (identifier: “Studio CE 09058,” AUSL Bologna) and Turin (identifier: “CPW28Y_002,” Comitato Etico Interaziendale A.O.U. San Giovanni Battista and A.O. “C.T.O. Maria Adelaide” Turin) and registered on ClinicalTrials.gov (identifier: NCT00998400). Written informed consent was secured from all of the patients for both the initial psychological evaluation and trial participation, after the procedures had been fully explained to them. The participants did not receive any compensation. All the procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Assessment
Baseline psychological evaluation was performed 1 month after the hospitalization for the ACS episode, in order to minimize the chance to detect transient ACS-related depressive symptomatology.Reference Fava and Sonino 17 Participants underwent detailed semistructured clinical interviews and observer-rated scales by a trained clinical psychologist and completed self-rating questionnaires for the assessment of subclinical psychological distress and well-being, as follows.
-
(a) The Structured Clinical Interview for DSM-IV-TR (SCID-I)Reference First, Spitzer, Gibbon and Williams 18 was used to identify depressive disorders. In order to qualify for a diagnosis of major depression, patients had to exhibit at least five (at least two for minor depression) out of nine symptoms, including either depressed mood or loss of interest and/or pleasure. 14 Minor depression was classified as “other specified depressive disorder, depressive episode with insufficient symptoms” (ie, characterized by insufficient number of symptoms to meet the criteria for major depressive disorder) in DSM-5. 19 As to dysthymia, which was relabeled to “persistent depressive disorder” in DSM-5, 19 patients had to report at least two additional depressive symptoms in addition to depressed mood for most of the day, for more days than not, and for at least 2 years. 14
-
(b) The Semistructured Interview based on the Diagnostic Criteria for Psychosomatic Research (SSI-DCPR)Reference Rafanelli, Roncuzzi and Finos 7 , Reference Fava, Freyberger and Bech 15 , Reference Porcelli and Sonino 20 was used to detect demoralization and Type A behavior. Diagnoses were formulated independently of DSM-IV-TR diagnostic findings. Items of the SSI-DCPR are scored through a dichotomous (ie, yes or no) response format and the interview contains skip instructions. The interview based on DCPR demonstrated high inter-rater reliability, with Cohen’s kappa for demoralization and Type A equal to 0.90 and 0.92, respectively.Reference Galeazzi, Ferrari, Mackinnon and Rigatelli 21 , Reference Guidi, Piolanti, Berrocal, Gostoli and Carrozzino 22
-
(c) The 20-item change version of Clinical Interview for Depression (CID)Reference Paykel 23 , Reference Guidi, Fava, Bech and Paykel 24 was selected to assess quality and severity of depressive symptoms. This dimensional observer-rated instrument represents an expanded version of the Hamilton Rating Scale for Depression.Reference Hamilton 25 , Reference Carrozzino, Patierno, Fava and Guidi 26 The interview covers 20 symptom areas and each item is rated on a 7-point Likert scale, with a score of 1 indicating the absence of symptoms and 7 severe debilitating manifestations, with specification of each anchor point based on the severity, frequency, and/or quality of symptoms. The higher the score, the worse the psychological condition. A score of 3 or above in each item was considered as the cut-off for the presence of the symptom, at least at a subclinical level. The scale encompasses a wide range of symptoms (such as irritability and phobic anxiety) compared to other scales and it is particularly suitable to assess subclinical symptoms of mood disorders.Reference Guidi, Fava, Bech and Paykel 24 One additional item concerning reactivity to social environment, selected from the full version of the CID, was included.
-
(d) The Symptom Questionnaire (SQ)Reference Kellner 27 , Reference Benasi, Fava and Rafanelli 28 constitutes a self-reported measure on subclinical psychological distress. It includes 92 items that yield 4 main scales, that is, depression, anxiety, hostility-irritability, and somatization. Each item has to be answered on a dichotomous format (ie, yes/true or no/false) and the higher the score, the higher the psychological distress.
-
(e) The psychological well-being (PWB) scales,Reference Ryff 29 , Reference Ryff 30 is a self-report 84-item questionnaire, for evaluating six inter-related areas of PWB and optimal functioning (ie, autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance). Items have to be rated on a 6-point Likert scale and higher scores correspond to greater PWB in each dimension.
Statistical analyses
Data were analyzed using SPSS 20.0 (SPSS Inc., Chicago, IL). Descriptive analyses were run for frequencies of specific depressive symptoms, as assessed by CID, and frequencies of DSM-IV-TR depressive disorders (ie, major/minor depression and dysthymia), DCPR demoralization, and type A behavior in the total sample. Chi-square test, applied to contingency tables, was used to compare the prevalence of DSM-IV-TR depressive disorders and DCPR demoralization with the frequencies of CID depressive symptoms. Multivariate analyses of variance using the general linear model were performed to test for associations between DSM-IV-TR depressive disorders, DCPR demoralization and average scores on dimensional psychological measures (SQ and PWB). Diagnoses formulated according to DSM-IV-TR and DCPR were examined separately.
By means of the GenLin command (indicating binomial as the probability distribution and logit as the link function to be used in the model), mixed-design repeated measures logistic regression was performed. This procedure allowed the evaluation of Time × Group allocation effect on multiple evaluations of CID depressive symptoms (ie, binary outcomes), including all the follow-up evaluations of each patient allocated to either the sequential combination of CBT and WBT or CM.
For all tests performed, the significance level was set at 0.05, two-tailed. In view of the exploratory nature of the investigation, adjustment for multiple testing was not performed.
Results
ACS patients’ characteristics
Patients’ response rate was 38.9% (N = 288 out of 740 ACS patients). Four hundred and fifty-two patients (35.4% females) refused to undergo the psychological assessment, mainly because of severe medical condition (35%), lack of interest (31%), or logistical problems (23.9%).
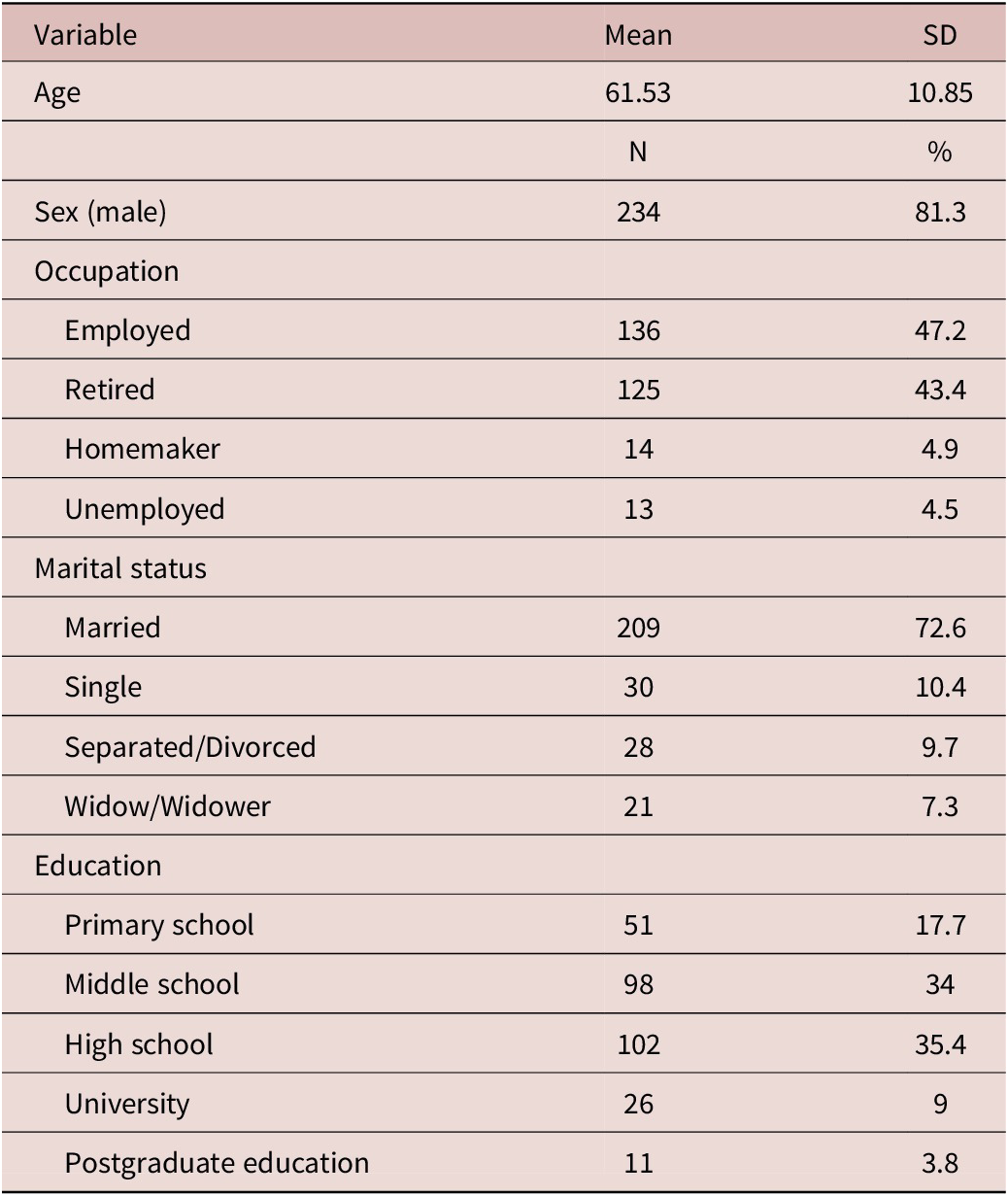
Descriptive sociodemographic characteristics of the study population are presented in Table 1. The sample included mainly men (81.3%) with a mean age of 61.53 years (SD = 10.85), ranging from 33 to 86 years. Most of the participants were employed (47.2%), married (72.6%) and had a high school diploma (35.4%).
Table 1. Sociodemographic Characteristics of the Patients with Acute Coronary Syndrome (ACS) (N = 288)
Relationship of DSM-IV-TR depressive disorders, DCPR demoralization, and type A behavior
Figure 1 describes the diagnostic profile of the sample (N = 288). One hundred and ten patients (38.2%) neither received a diagnosis of mood disturbance (ie, DSM-IV-TR depressive disorders or DCPR demoralization), nor satisfied criteria for type A behavior. Demoralization was the most frequently reported diagnosis (N = 123, 42.7% of the whole sample). Thirty-six (29.3% of demoralized patients) presented with demoralization alone, whereas 14 had comorbid type A behavior. The remaining 73 demoralized participants reported a comorbidity with mood disturbances according to DSM-IV-TR. As to DSM-IV-TR depressive disorders, minor depression was the most frequently reported mood disorder (N = 74, 25.7% of the whole sample). Ten (13.5% of patients with minor depression) presented with this diagnosis alone, whereas major depression (N = 8, 2.8% of the whole sample) and dysthymia (N = 4, 1.4% of the whole sample) were always diagnosed in comorbidity with demoralization, except one case of dysthymia. Eighty-one patients (28.1% of the whole sample) reported type A behavior and, among them, more than a half (N = 42, 14.6% of the whole sample) did not show any comorbid mood disturbance.
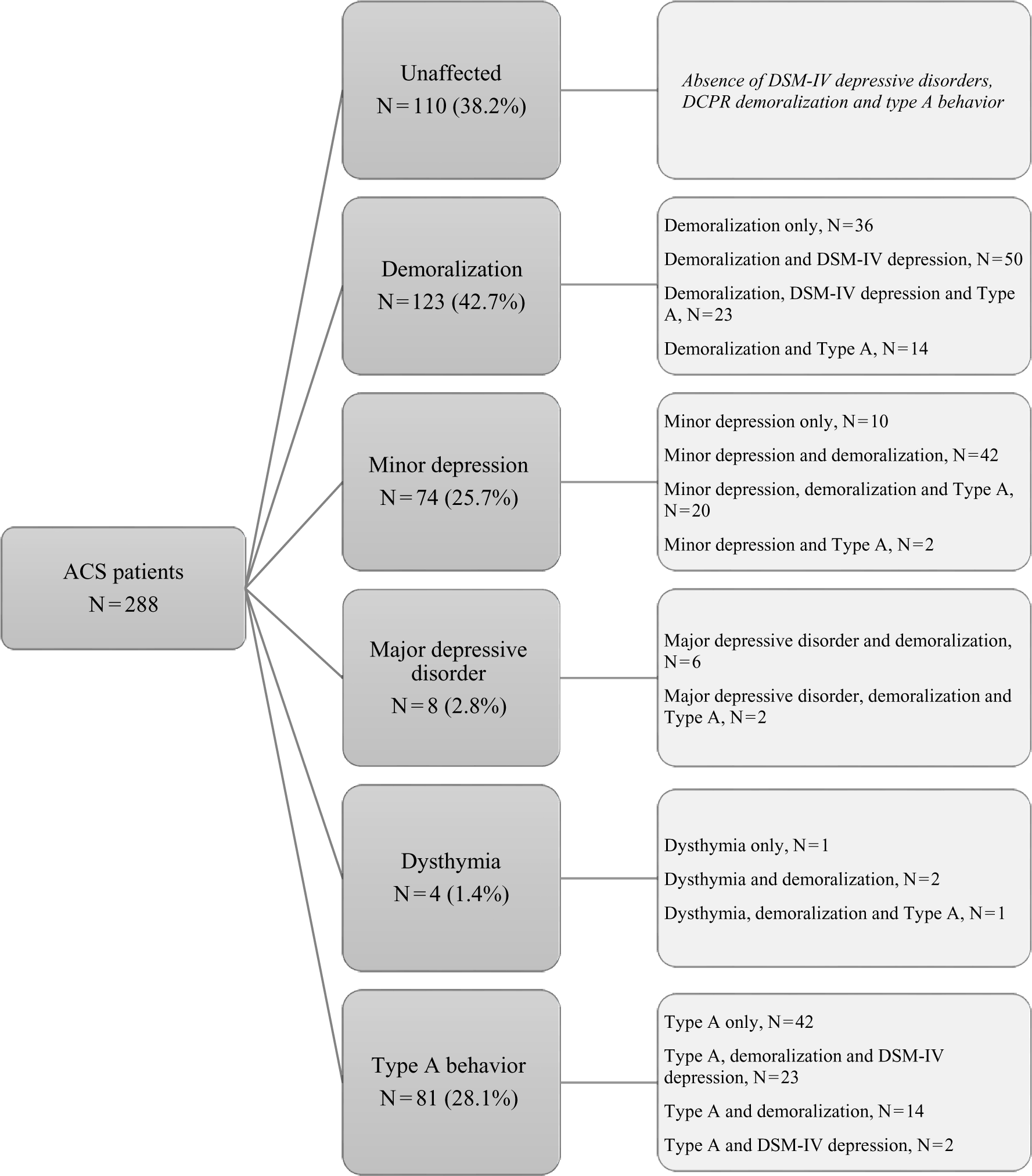
Figure 1. Prevalence of DSM-IV-TR depressive disorders (major depressive disorder, minor depression, and dysthymia), DCPR demoralization and Type A behavior in ACS patients. ACS, acute coronary syndrome; DCPR, diagnostic criteria for psychosomatic research.
If the assessment had relied uniquely on DSM-IV-TR, 70.1% of the patients would have been labeled as “unaffected,” with only 29.9% (N = 86) of the sample receiving a diagnosis of mood disorder, mainly minor depression. Instead, the joint use of the DCPR system allowed the identification of psychological distress in 58% (N = 167) of the sample.
As to past diagnoses, 41% of the sample (N = 118) reported to have a positive history of DSM-IV-TR depression, whereas 42% (N = 121) of DCPR demoralization.
Frequency of depressive symptoms in ACS patients
The frequencies of all CID items are presented in Table 2. The most common CID depressive symptoms in patients who suffered from a first episode of ACS were high environmental reactivity (59.4%, N = 171) and low energy and fatigue (50.7%, N = 146), followed by depressed mood (36.1%, N = 104) and somatic anxiety (35.4%, N = 102).
Table 2. Frequency of Depression-Related Symptoms (CID Items) in ACS Patients (N = 288) and their Associations with DSM-IV-TR Depressive Disorders (ie, Major Depression, Minor Depression, and Dysthymia) and DCPR Demoralization
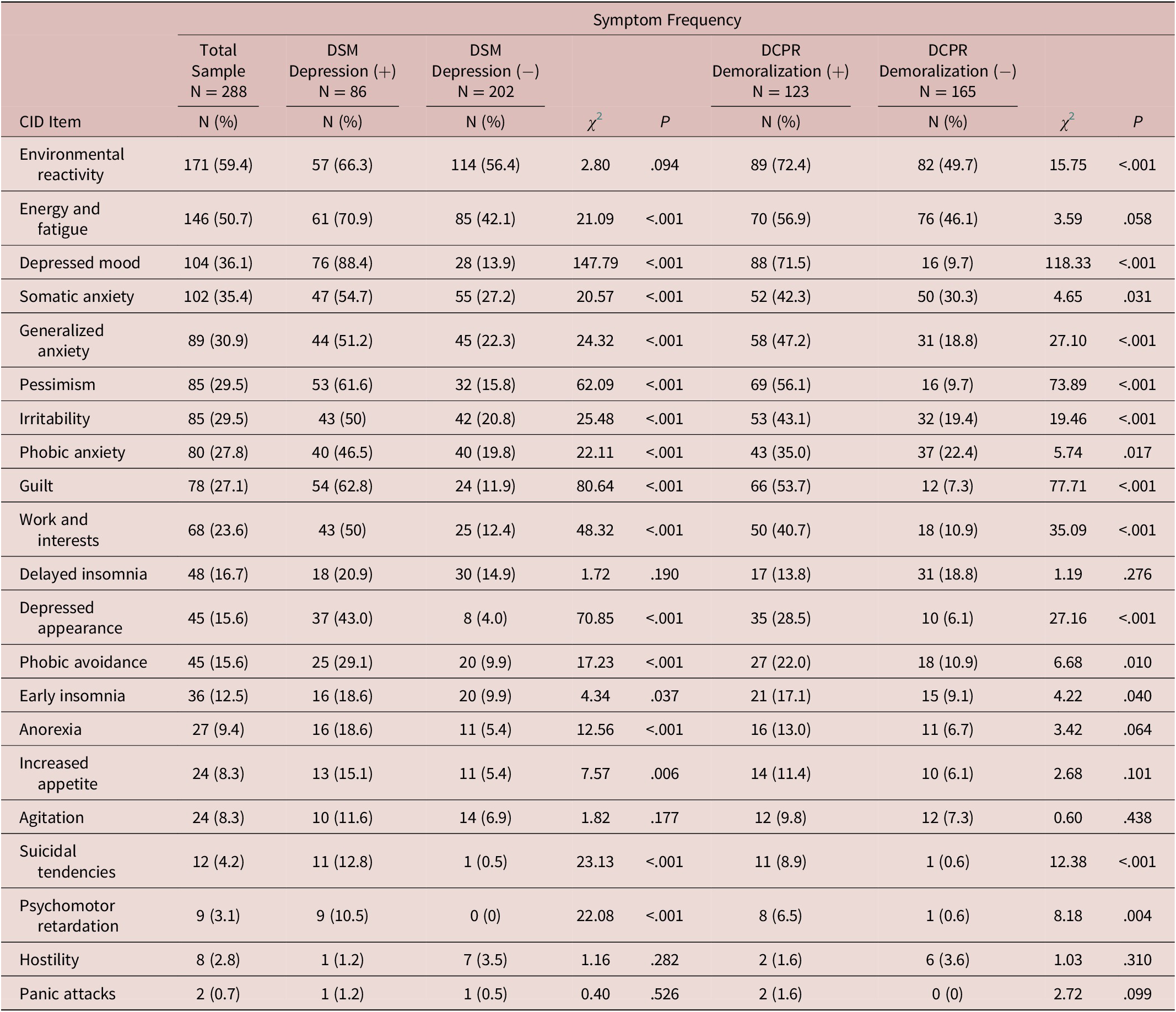
Abbreviations: ACS, acute coronary syndrome; CID, clinical interview for depression; DCPR, diagnostic criteria for psychosomatic research; DSM, diagnostic and statistical manual of mental disorders.
Overall, DSM-IV-TR depressive disorders and DCPR demoralization were associated with a greater severity of symptoms, except for delayed insomnia, agitation, hostility, and panic attacks (Table 2). Significant associations of CID symptoms with DSM-IV-TR depressive disorders or with DCPR demoralization were found as well. In particular, low energy and fatigue (P < .001), as well as changes of appetite (anorexia: P < .001; increased appetite: P < .01), were uniquely associated with DSM-IV-TR depressive disorders. Environmental reactivity (P < .001) was exclusively associated with DCPR demoralization.
Associations between DSM-IV-TR depressive disorders and dimensional psychological variables
According to multivariate analyses of variance comparisons (Table 3), the presence of DSM-IV-TR depression (ie, major, minor depression, or dysthymia) was significantly associated with higher scores of psychological distress in all SQ scales (all P values < .001) and lower scores of PWB in all PWB dimensions (from P = .004 to P < .001), except for autonomy.
Table 3. Association of DSM-IV-TR Depressive Disorders (ie, Major Depression, Minor Depression, and Dysthymia) and DCPR Demoralization with Dimensional Psychological Measures (N = 288)
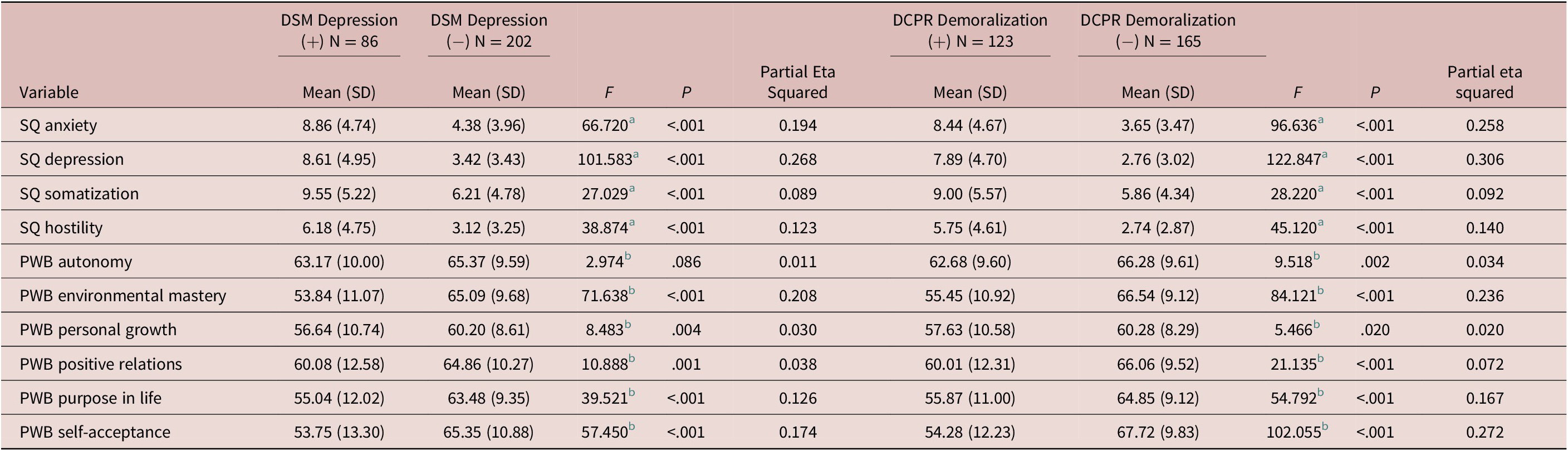
Note: (+) Disorder or syndrome present; (−) Disorder or syndrome absent.
Abbreviations: DCPR, diagnostic criteria for psychosomatic research; DSM, diagnostic and statistical manual of mental disorders; PWB, psychological well-being scales; SQ, symptom questionnaire.
a df = 1, 280.
b df = 1, 275.
Associations between DCPR demoralization and dimensional psychological variables
Concerning DCPR demoralization, multivariate analyses of variance indicated that the presence of this syndrome was significantly associated with higher scores in all SQ scales (all P values < .001), as well as with lower scores in all PWB dimensions (from P = .020 to P < .001) (Table 3).
Effects of CBT/WBT compared to CM on depression-related symptoms
Considering the first 100 depressed/demoralized consecutive patients who joined the TREATED-ACS Study and received the interventions, GenLin procedure showed that the interaction Time × Group allocation (either CBT/WBT or CM) was significant for guilt (Wald Chi-square = 12.05, df = 5, P < .05), pessimism (Wald Chi-square = 12.76, df = 5, P < .05), low energy/fatigue (Wald Chi-square = 14.45, df = 5, P < .05), somatic anxiety (Wald Chi-square = 11.61, df = 5, P < .05), and early insomnia (Wald Chi-square = 12.68, df = 5, P < .05) (Table 4).
Table 4. Mixed-Design Repeated Measures Logistic Regressions on Multiple Evaluations of CID Depression-Related Symptoms (ie, Binary Outcomes), According to Group Allocation (CBT/WBT vs CM)
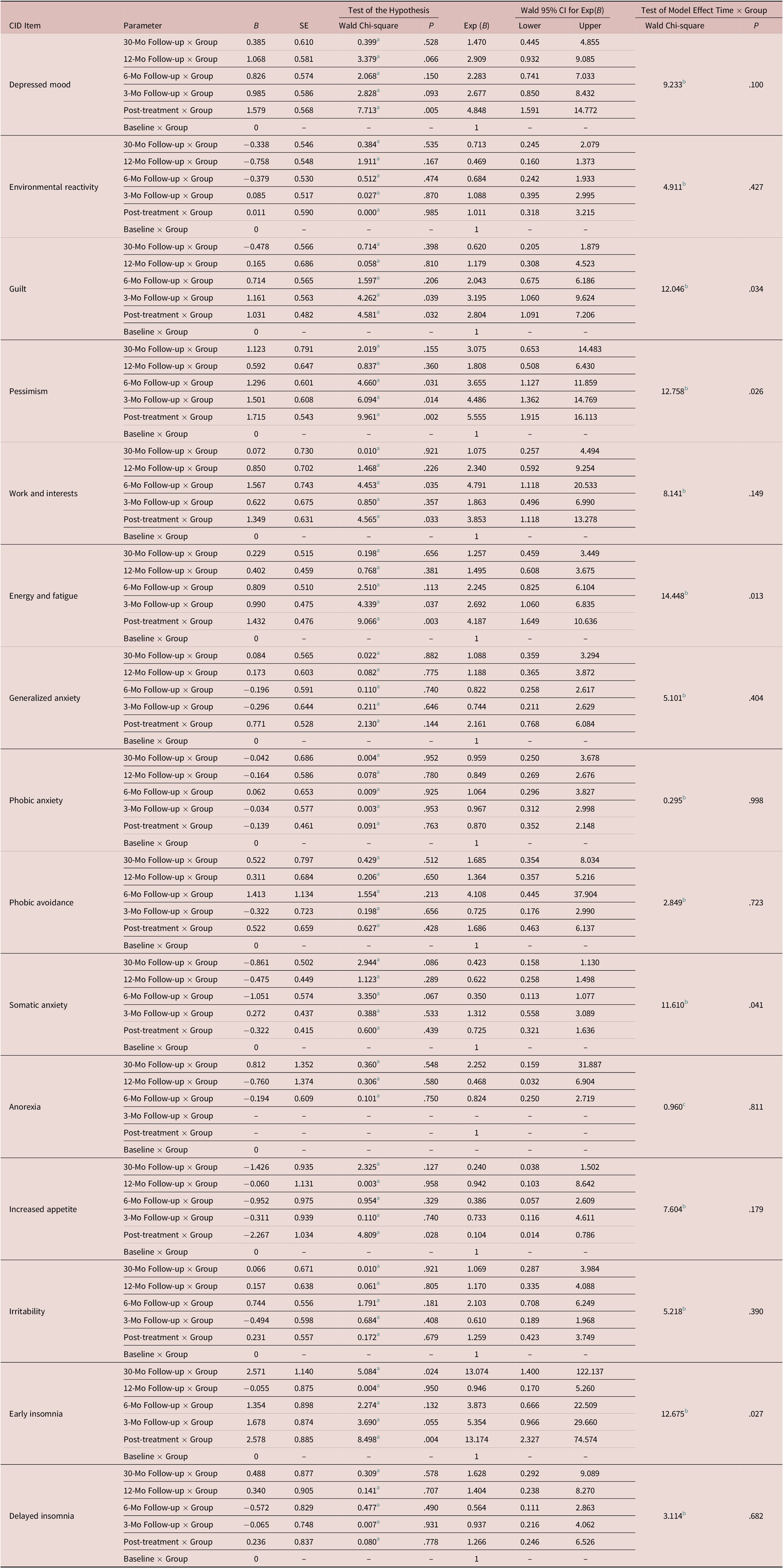
Abbreviations: CBT/WBT, sequential combination of cognitive-behavioral therapy and well-being therapy; CID, clinical interview for depression; CM, clinical management.
a df = 1;
b df = 5;
c df = 3.
Specifically, the sequential intervention (CBT/WBT) was significantly related to decreased feelings of guilt (Wald Chi-square = 4.58, df = 1, P < .05; Exp(B) = 2.80, 95%CI: 1.09-7.21) and pessimism (Wald Chi-square = 9.96, df = 1, P < .01; Exp(B) = 5.56, 95%CI: 1.92-16.11), from baseline to post-treatment (both P < .001), with benefits maintained up to 30-month follow-up. Moreover, CBT/WBT was significantly associated with a reduction of somatic depressive symptoms, such as low energy/fatigue (Wald Chi-square = 9.07, df = 1, P < .01; Exp(B) = 4.19, 95%CI: 1.65-10.64) and early insomnia (Wald Chi-square = 8.50, df = 1, P < .01; Exp(B) = 13.17, 95%CI: 2.33-74.57), from baseline to post-treatment (P < .001 and P = .011, respectively), with benefits maintained up to 12-month follow-up in the first case, and fluctuating over time in the case of insomnia (from 3- to 12-month follow-up: P > .05; 30-month follow-up: P = .016). The only exception was somatic anxiety, in which a significant reduction of symptoms was observed in CM group only between baseline and post-intervention (P = .031) with benefits maintained at subsequent follow-ups, except at 3-month follow-up.
Finally, as to depressed mood, no significant Time × Group interaction was found. Indeed, in both CBT/WBT and CM groups a significant decrease of depressed mood from baseline to post-treatment was found (P < .001 and P = .002, respectively), and maintained up to 30-month follow-up.
Discussion
Determination of depressive disorders according to DSM diagnostic criteria 14 is essentially based on the number of key depressive symptoms that are present, for example, at least five of a set of nine symptoms should be present (and one should be either depressed mood or loss of interest). However, setting a clinical threshold merely on the basis of these criteria may be problematic in ACS, particularly in the acute phase of illness,Reference Fava and Sonino 17 and may miss important clinical information. In this investigation, an innovative approach to the assessment of mood disturbances was attempted. Hospitalization carries a considerable amount of distress that tends to subside with dischargeReference Fava and Sonino 17; patients underwent psychological evaluation 1 month after the acute event. Further, the characteristics, quality and severity of each depressive symptom were assessed using a highly sensitive and accurate observer-rated scale, the CID.Reference Paykel 23 , Reference Guidi, Fava, Bech and Paykel 24 , Reference Carrozzino, Patierno, Fava and Guidi 26 Two additional related syndromes, demoralization and type A behavior,Reference Rafanelli, Roncuzzi and Finos 7 , Reference Lichtman, Froelicher and Blumenthal 1 Reference Kuhlmann, Arolt and Haverkamp 5 , Reference Porcelli and Sonino 20 were identified. Finally, self-rating measures of subclinical distress, the SQReference Kellner 27 , Reference Benasi, Fava and Rafanelli 28 and the PWB,Reference Ryff 29 , Reference Ryff 30 were included.
Based on DSM criteria only, less than one third of ACS patients (29.9%) received a diagnosis of mood disorder, mainly minor depression, whereas the DCPR system substantially increased the likelihood of identifying mood disturbances (58% of cases). Further, the most commonly reported symptoms, according to CID, were abnormal reactivity to social environment, low energy/fatigue, depressed mood, and somatic anxiety, with specific depressive somatic symptoms uniquely associated with DSM depression, whereas environmental reactivity with demoralization. Both depressed and demoralized patients reported significantly higher distress and lower well-being than their counterparts, except for autonomy scores, that were similar in depressed and nondepressed patients. The sequential combination of CBT and WBT was associated with a significant decrease in symptoms such as guilt, pessimism, fatigue, and early insomnia, as assessed by CID.
These findings provide further support to the incremental validity of the DCPR system in medical settings.Reference Guidi, Piolanti, Berrocal, Gostoli and Carrozzino 22 , Reference Gostoli, Montecchiarini and Urgese 31 Figure 1 illustrates the comprehensive assessment of mood disturbances that was performed in the present study on ACS patients. Our findings suggest a substantial overlap between depression and demoralization, as reported also in previous studies of medically ill patients,Reference Guidi, Fava and Picardi 32 , Reference Rafanelli, Guidi, Gostoli, Tomba, Porcelli and Grandi 33 even though depressed patients do not necessarily meet also the criteria for demoralization, and an important proportion of patients with demoralization do not meet diagnostic criteria for depression.Reference Rafanelli, Roncuzzi and Milaneschi 4 , Reference Rafanelli, Roncuzzi and Finos 7 , Reference Rafanelli, Offidani, Gostoli and Roncuzzi 10 , Reference Rafanelli, Guidi, Gostoli, Tomba, Porcelli and Grandi 33 , Reference Rafanelli, Gostoli, Roncuzzi and Sassone 34 Further, this study provides support to the distinctive clinical features of these two diagnostic entities. In line with prior research,Reference Guidi, Fava and Picardi 32 , Reference de Figueiredo 35 we found that specific somatic symptoms (such as fatigue and changes of appetite) are more likely to characterize depressed patients (and may act as “cardio-toxic” factors), whereas abnormal reactivity to social environment is more frequently related to demoralization.
Associations of demoralization with dimensional psychological measures provide further support to the incremental validity and clinical utility of the DCPR system.Reference Guidi, Piolanti, Berrocal, Gostoli and Carrozzino 22 Consistently with previous research,Reference Rafanelli, Roncuzzi and Milaneschi 4 , Reference Tecuta, Tomba, Grandi and Fava 36 , Reference Tecuta, Fava and Tomba 37 demoralization was found to be significantly associated with lower self-reported PWB and greater distress. PWB represents a neglected area in traditional psychiatric assessment, despite the growing literature supporting its buffering role in coping with stress and its favorable impact on disease course.Reference Ryff 30 , Reference Pressman and Cohen 38 PWB, indeed, was reported to be associated with reduced gene expression of conserved transcriptional response to adversity,Reference Frederickson, Grewen and Algoes 39 which is usually elicited by persistent stressReference Cole 40 and involved in the pathophysiology of cardiovascular diseases.Reference Nemeroff and Goldschmidt-Clermont 41
The DCPR interview allowed the detection of Type A behavior (TAB)Reference Fava, Freyberger and Bech 15 , Reference Friedman and Rosenman 42 in 28.1% of the sample, in line with other studies reporting the presence of TAB in about one third of patients with coronary heart disease.Reference Rafanelli, Roncuzzi and Finos 7 , Reference Sirri, Fava and Guidi 43 Moreover, similarly to previous studies,Reference Sirri, Fava and Guidi 43 the present investigation showed that Type A often occurs without a DSM diagnosis and it is more frequently associated with demoralization than with depression.
The Clinical Interview for DepressionReference Paykel 23 , Reference Guidi, Fava, Bech and Paykel 24 yielded the most frequently reported depressive symptoms characterizing patients suffering from ACS. Among these symptoms, reactivity to social environment, low physical energy, depressed mood and somatic anxiety, were the most common. Reactivity to social environment refers to variations of mood and symptomatology (ie, either improvement or worsening), as a reaction to environmental circumstances. This characteristic has been found to sensitively discriminate between different subgroups of depressed patients.Reference Paykel 44 -Reference Paykel, Klerman and Prusoff 46 It is also very common in patients with neurocirculatory astheniaReference Fava, Magelli and Savron 47 and cyclothymic disturbances.Reference Tomba, Rafanelli, Grandi, Guidi and Fava 48 Glass and ContradaReference Glass and Contrada 49 suggested that individuals who are prone to develop coronary diseases are more likely to display alternating coping patterns in challenging situations. Specifically, initial coping efforts could be manifested as behavioral hyper-reactivity (ie, Type A behavior and manic/hypomanic symptoms), which could be then followed by hypo-reactivity (including demoralization and depression) after repeated failure to assert control and/or attain relevant goals. These affective and behavioral transitions originally observed in individuals with Type A have been found to be similar to mood swings of bipolar patients,Reference Glass and Contrada 49 suggesting that in cardiac patients with type A behavior, depressive symptoms following a cardiovascular event may be part of a subsyndromal bipolar disorder.Reference Rafanelli, Sirri, Grandi and Fava 11 , Reference Dargél, Volant and Saha 50 This hypothesis seems to be supported by the findings of the present study, given the high rate of reactivity to social environment in ACS patients and the fact that almost half of patients with Type A behavior were also demoralized and/or depressed.
Somatic manifestations of psychological distress, such as somatic symptoms of depression (ie, low energy and fatigue) and physical manifestations of anxiety (ie, sweating, shaking, muscle tension, and difficult breathing), were found to be extremely common in our sample. These data are in line with literature showing that approximately two thirds of patients with depression in medical settings—especially older adultsReference Hegeman, Kok, Van der Mast and Giltay 51—present with somatic symptoms,Reference Tylee and Gandhi 52 which could be interpreted as prodromal signs of mood disturbances and thus represent helpful indicators for the diagnostic process.Reference Benasi, Fava and Guidi 53 Compared to depression characterized by cognitive symptoms, depression with prevalent somatic symptoms seems to be more “cardio-toxic”Reference Rafanelli, Sirri, Grandi and Fava 11 since it may have worse health outcomes, such as reduced heart rate variability,Reference de Jonge, Mangano and Whooley 54 worse cardiovascular prognosisReference O’Neil, Sanderson and Oldenburg 55 and higher risk of all-cause mortality.Reference Rumsfeld and Ho 56 A meta-analysisReference de Miranda Azevedo, Roest, Hoen and De Jonge 57 showed that the severity of somatic symptoms of depression constituted a better predictor of mortality than affective and cognitive symptoms in patients with myocardial infarction. Recently, Iob et alReference Iob, Kirschbaum and Steptoe 58 prospectively examined a large cohort of adults aged over 50 years old and found that hair cortisol and plasma C-reactive protein exhibited stronger relationships with somatic rather than with cognitive/affective symptoms of depression, underlining the importance to consider symptom-specific effects in future studies on pathophysiological mechanisms.
On the same vein, somatic symptoms of anxiety have been identified as predictors of coronary heart diseaseReference Nabi, Hall and Koskenvuo 59 and contributors to disability in late life, particularly in the presence of depression,Reference Lenze, Rogers and Martire 60 , Reference Morin, Nelson, Bickford, Insel and Mackin 61 suggesting that the identification and treatment of these symptoms may improve functional outcomes among older depressed adults. Given the significant overlap of physical symptoms of medical disorders with somatic and anxiety symptoms of depression, it is necessary to disentangle the associations of these symptom clusters with functional impairment.Reference Galatzer-Levy and Bonanno 62 -Reference Morin, Galatzer-Levy, Maccallum and Bonanno 64 The use of the clinimetric approach for psychological assessment presented in the current study could be important to this purpose.
Furthermore, because of the clinimetric properties of the CID,Reference Guidi, Fava, Bech and Paykel 24 particularly discriminant validity and sensitivity to changes with treatment, we were able to detect which depressive symptoms may benefit more from a sequential combination of cognitive-behavioral techniques and strategies geared to euthymia. Indeed, CBT/WBT was found to be associated with significantly greater relief of guilt and pessimism, as well as with an amelioration of somatic symptoms of anxiety and quality of sleep. In the present study, the addition of sessions dedicated to the pursuit of euthymia (ie, WBT), that were aimed at promoting integration of psychic forces, a unifying outlook on life, and resistance to stress,Reference Fava and Bech 65 -Reference Guidi and Fava 67 proved their additional value on relieving depressive symptoms and promoting a balanced functioning. Indeed, sequential combination of treatments in depression was found to entail a lower likelihood of relapse.Reference Guidi and Fava 68
Both CBT/WBT and CM were associated with significant improvements of depressed mood. This finding supports the hypothesis that the presence of demoralization might help identify those patients with a heightened susceptibility to nonspecific elements of treatment (such as offering a healing setting, encouragement, and instilling hopes of improvement), which provide reduction of isolation and pave the ground for therapeutic alliance, enhancing the process of change.Reference Tomba, Tecuta, Guidi, Grandi and Rafanelli 69 CM, indeed, represents an active form of control that—unlike control conditions used in previous trialsReference Reavell, Hopkinson, Clarkesmith and Lane 70—allows discrimination of specific and nonspecific ingredients of the psychotherapeutic approach.Reference Fava, Guidi, Rafanelli and Rickels 71 , Reference Guidi, Brakemeier and Bockting 72
This investigation presents some limitations that should be mentioned, namely the lack of follow-up data on non-participantsReference Rafanelli, Gostoli and Buzzichelli 13 and the low rate of ACS patients who agreed to undergo the initial psychological assessment (38.9% of 740 ACS patients screened by the cardiologists), which—although it could mitigate the conclusion—is in line with participation rate reported elsewhereReference Hansen, Hanash, Rasmussen, Hansen and Birket-Smith 73 and reflects demographic characteristics of ACS patients in Italy (ie, prevalence of males and females).Reference De Luca, Marini and Gonzini 74 Despite these limitations, the present study has several strengths, such as the clinical homogeneity of the sample (ie, all participants had a first episode of ACS), the longitudinal and multicenter design, and the innovative, clinimetric approach to psychological assessment, which yielded new, important clinical insights into mood disturbances in ACS.
Conclusions
Expanding the assessment of mood disturbances from the identification of DSM depressive disorders to a broader number of related variables may yield important insights into the psychological state of patients with ACS. Assessing a wide spectrum of affective symptoms, detecting the presence of demoralization and type A behavior, and evaluating PWB and distress by dimensional self-rating tools, support the clinical relevance of subthreshold manifestations of psychological distress that would otherwise go unrecognized using the traditional taxonomy. Findings from this study indicate the clinical value of the clinimetric approach to the assessment of mood disturbances in ACS patients, which may allow subtyping of patients based on specific psychological profiles,Reference Guidi, Fava and Picardi 32 , Reference Rafanelli, Guidi, Gostoli, Tomba, Porcelli and Grandi 33 and provide therapeutic and prognostic indications.
Funding
This work was supported by a grant from the Compagnia di San Paolo di Torino (Italy) to C.R.
Disclosures
The authors declare that there is no conflict of interest.
Author Contributions
Conceptualization: S.G., G.A.F., C.R.; Data curation: S.G., C.R.; Formal analysis: S.G.; Funding acquisition: C.R.; Investigation: S.G., S.B., J.G., L.S., E.M.; Methodology: S.G., G.A.F., C.R.; Project administration: S.G., S.B., G.A.-D., C.R.; Resources: S.B., G.A.-D., C.R.; Supervision: R.R., G.A.-D., G.A.F., C.R.; Validation: G.A.F., C.R.; Visualization: S.G.; Writing—original draft: S.G., G.A.F., C.R.; Writing—review and editing: S.G., S.B., J.G., L.S., E.M., R.R., G.A.-D., G.A.F., C.R.







