INTRODUCTION
Sickle cell disease (SCD) is a multisystem, inherited, and chronic blood disorder affecting over 300,000 births per year worldwide and is associated with early mortality and morbidity including stroke, sepsis, pain, and reduced quality of life.Reference Piel, Patil and Howes1 Sickle cell vaso-occlusive crises (VOC), characterized by severe bone pain, account for approximately 90% of acute health care visits for patients with SCD, usually in the setting of emergency departments (ED).Reference Ballas and Lusardi2, Reference Platt, Thorington and Brambilla3 While best practice management for VOC indicates that adequate analgesia should be provided within 30 minutes to achieve early resolution and facilitate early discharge, there are currently significant care gaps and delays in EDs to meet this target.Reference Rees, Olujohungbe and Parker4-7 Contributing factors to suboptimal care delivery for patients presenting with a VOC include ED crowding, negative health care provider’s attitudes, a lack of standardization of care, misperception of pain behaviours, gaps in provider experience, and patient factors such as opiate tolerance.Reference Adewoye, Nolan, McMahon, Ma and Steinberg8-Reference Tanabe, Hafner, Martinovich and Artz13
These gaps in care have prompted many SCD outpatient treatment centres in the United Kingdom, Caribbean, and United States to develop models for ambulatory short-stay units designed specifically to treat VOC.Reference Adewoye, Nolan, McMahon, Ma and Steinberg8-Reference Wright, Bareford and Wright10, Reference Benjamin, Swinson and Nagel14-Reference Ware, Hambleton, Ochaya and Serjeant17 Research has demonstrated that caring for patients with a VOC outside of an ED can result in improved pain control, fewer treatment delays, better patient satisfaction, and reduced costs. For example, a recent large cohort study in Maryland demonstrated a 20% lower admission rate for patients treated in a short-stay unit.Reference Lanzkron, Carroll and Hill15 Several examples of SCD short-stay units for the management of VOC have also demonstrated cost effectiveness, as compared with ED use, with the potential savings of up to $1000 USD per visit.Reference Adewoye, Nolan, McMahon, Ma and Steinberg8, Reference Chappidi, Alfonso, Bishai and Lanzkron9, Reference Benjamin, Swinson and Nagel14
In Canada, the prevalence of SCD is 3000–7000, with over 1000 residing within the Greater Toronto Area.18 Current provision of care for adult patients with SCD who experience VOC occurs predominantly in the ED, and a short-stay unit model has not been previously evaluated in Canada. Given the potential impact on the delivery of care for patients with SCD, we developed and examined the acceptability of an innovative model of care that incorporates a short-stay unit for the management of adult patients with SCD who experienced an uncomplicated VOC at the Women’s College Hospital in Toronto, Canada.
METHODS
Population and setting
Patients aged 18 years or older with a diagnosis of SCD between October 2014 and July 2016 who obtained follow-up at the Red Blood Cell Disorders (RBCD) Clinic at University Health Network (UHN) in Toronto, that houses the largest sickle-cell comprehensive care centre in Canada, were eligible for inclusion in the pilot study. SCD was defined by evidence of a clinically significant sickle cell genotype (Hb SS, Hb SB0, Hb SB+, and Hb SC) demonstrated using capillary electrophoresis. Patients were identified using a standard of care triage process that involved calling the RBCD clinic if they experienced pain concerning for VOC. Exclusion criteria included symptoms concerning for a complicated VOC, limited to neurologic symptoms, chest pain, severe abdominal pain, shortness of breath, priapism, and fever (>38.3°C/100.9°F).
Eligible patients were directed to the short-stay unit located within the existing acute ambulatory care unit (AACU) at the Women’s College Hospital in Toronto, Ontario. The AACU is open 24 hours a day Monday to Friday and staffed by a general internist, nurses, and a pharmacist. The unit provides urgent patient assessment for new medical conditions or exacerbations of chronic medical conditions and is resourced with rapid laboratory services, medical imaging, intravenous (IV) therapies, and oxygen supplementation.
The historical control included patients with a diagnosis of SCD seen at the UHN ED between August 2009 and September 2012. Inclusion criteria were as follows: aged 18 years or older at the time of assessment, and assigned a discharge diagnosis code signifying a diagnosis of SCD, along with a sub-code consistent with VOC. Exclusion criteria were transfusion in the ED, absence of an SCD diagnosis based on clinic notes, and illegible handwriting in clinical documentation.
Design
This is a before-and-after pilot study to examine the acceptability of an ambulatory short-stay unit in Toronto, Canada, for the management of uncomplicated VOC in patients with SCD, as compared with a retrospective, historical control group managed in the ED.
Study protocol
A poster advertising the short-stay unit was displayed in the waiting room of the outpatient RBDC clinic that eligible patients attended, and pamphlets were also handed out at clinic visits during the pilot period. As part of routine care, patients of the RBCD clinic at UHN are instructed to contact a nurse practitioner at the clinic if they have pain that is difficult to control or concerning during daytime working hours. During the study period, all calls of this nature prompted the RBCD nurse to evaluate the inclusion and exclusion criteria to assess appropriateness for the short-stay unit. Eligible patients were directed to the short-stay unit for management of their uncomplicated VOC. Although the telephone line for triage was only available from 9 a.m. to 5 p.m. on weekdays, patients were permitted to present to the short-stay unit anytime during operating hours (24 hours from Monday to Friday) after triage. Once at the short-stay unit, patients were clinically assessed by nursing and medical staff trained in the management of uncomplicated VOC.
Data were collected from patients who provided consent to the study. If consent was not obtained, patients were still treated according to the standard of care at the short-stay unit but wer not included in the study. A local treatment protocol based on the British Committee for Standards in Haematology Guidelines for VOC management was utilized.Reference Rees, Olujohungbe and Parker4 This protocol was designed locally through iterative input by experts in the area of SCD, including physicians, pharmacy staff, and nursing staff. In addition to supportive clinical care and standard investigations for VOC, the protocol included treatment with supplemental oxygen, IV fluids, and a first opiate dose target within 30 minutes of arrival (see Supplementary Material). Consultation with a hematologist from the RBCD clinic was initiated upon patient arrival at the short-stay unit. Transfer to the local ED at UHN for admission under general internal medicine (GIM) would occur if patients developed any signs or symptoms suggestive of complications other than simple VOC or if their IV pain control requirement exceeded 72 hours. Patients were also transferred when the unit closed on Friday at midnight. Otherwise, they were discharged home if their pain decreased to a level that was manageable as an outpatient.
Data collection
The clinical course of the patients in the short-stay unit was documented according to local standards of care in patient charts. Relevant clinical data including times of triage, arrival, assessment and administration of pain control, sickle cell genotype, formulation and dose of pain medication, and pain scores throughout the stay were then transferred to a standardized data abstraction sheet by one of the investigators. Prior to discharge from the short-stay unit, patients were also asked to complete a short survey evaluating their experience. This included assessment of patients’ experience at and impressions of the short-stay unit according to several parameters on a five-point Likert scale with an option for qualitative feedback. Separate from the short-stay unit patients, a consecutive sample of outpatients with SCD attending routine clinical appointments at the RBCD clinic at UHN were asked to complete a survey about their knowledge of the short-stay unit and barriers for its use. Approximately 550 active adult patients with SCD were eligible to complete this survey form, but a minimum target of 10% was made a priori to accommodate the feasibility of distribution between June 1 and July 30, 2016. Lastly, retrospective data were collected from patient charts corresponding to presentations at the nearest ED (UHN) with ICD-10 codes for SCD (D57) from August 2009 to September 2012 to serve as the historical control group.
Outcome measures
The primary outcome was the time from patient arrival to administration of the first opiate dose. Secondary outcomes were total opiate dose per hour, pain scores on arrival, pain scores at set intervals, length of stay, and disposition status.
Statistical analysis
Descriptive statistics were performed for all relevant clinical data from the short-stay unit and used to summarize quantitative survey data. Comparison of clinical outcomes between the short-stay unit and local ED was performed by matching visits. Because of the limited availability of data, short-stay unit visits were matched for sex only to local ED visits at a one-to-four ratio, and age was included as an outcome variable. The analysis required the Wilcoxon signed-rank tests for continuous variables and McNemar test for discharge rates because of non-normally distributed data samples. Statistical analysis was performed using IBM SPSS Statistics, Version 23.
Ethical oversight
This study was completed by the investigators without the influence of any commercial sponsor and in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. The study was approved by the local research ethics boards at Women’s College Hospital and UHN.
RESULTS
Baseline demographics and clinical characteristics
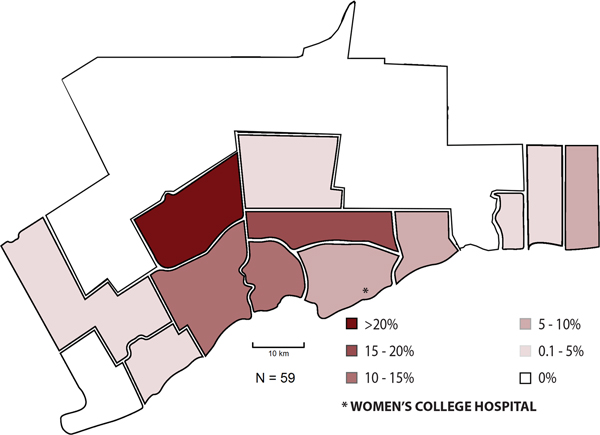
Baseline demographics and clinical characteristics of the short-stay unit patients are presented in Table 1. There were 21 patient visits during the study period corresponding to 12 unique patients. The mean age of the patients during these visits was 28.2±8.3 years, with a one-to-three male-to-female ratio. SS genotype patients accounted for 16 visits, SC patients for 4 visits and Sβ+ for 1 visit. On average, it took patients 110.4±87.9 minutes from telephone triage to presentation at the short-stay unit. Once there, patients were seen by an internist at a mean of 16.4±18.1 minutes and given their first opiate dose at a mean of 23.5±23.0 minutes. The mean total dose of oral (PO) morphine equivalent received per hour (46.7±47.0 mg/h) was driven up by one patient who attended the short-stay unit four times. However, the median remained high in this population at 25.1 mg/h. IV hydromorphone was the most commonly administered form of opiate. The average pain score at presentation was 8.3±1.3/10 and steadily decreased over time to 4.0±2.8/10 at 1080 minutes (Figure 1). The average length of stay was 28.7±21.2 hours, and 15.8% of visits required transfer to an internal medicine inpatient ward. Of the three patients who were transferred, two had persistent pain, and one showed clinical signs of an acute chest syndrome.
Figure 1. Mean pain scores with standard deviations of patients presenting with a VOC upon arrival at the short-stay unit and specified time intervals.
Table 1. Clinical and demographic data of short-stay unit patients

Patient experience
A patient satisfaction survey was completed for 85% of the visits to the short-stay unit. Sixty-seven percent of patients completing the survey had obtained treatment for a VOC at an ED more than three times in the past year. Satisfaction with care at the short-stay unit was ranked very highly overall and also with respect to specific aspects of care, with all the average ratings above four out of five on a five-point Likert scale with one exception. The convenience of location compared with a local ED was ranked 3.3/5 on average. Qualitative feedback primarily consisted of compliments to the organization of the short-stay unit and suggestions to open locations closer to where patients reside. Findings from other specific questions can be found in Table 2.
Table 2. Results of the short-stay unit patient satisfaction survey
ED=emergency department.
Comparison with historical control
There were 602 visits to the local ED with diagnostic codes corresponding to SCD during the retrospective study period. However, availability of data, skewed sex trends regarding visits to the short-stay unit, and local ED populations restricted inclusion of most ED visits. It is also notable that 12 “super-user” patients accounted for more than one-half of these visits. After one was excluded because of incomplete data for the length of stay, 20 short-stay unit visits were matched to 80 ED visits and included in the analysis. All visits were from confirmed cases of SCD, but genotype data were not reliably available from the ED visits. A comparison revealed no difference in age (p=0.78) or pain score at presentation (p=0.72) between the two groups. Time to the first opiate dose was significantly lower in the short-stay unit (23.5 minutes), as compared with the ED (100.3 minutes, p<0.001). The mean length of stay in the short-stay unit (28.7 hours) was longer than that of the ED (7.9 hours); however, data on the total length of stay at UHN were unavailable as 30% of the patients in the historical control were transferred from the ED to other departments in the hospital. The mean total opiate dose received per hour was higher for patients in the short-stay unit (46.7 mg/h) than that of the ED (11.9 mg/h). The discharge rate was also higher for patients in the short-stay unit (84.2%) than those in the ED (69.7%). Further data comparing clinical outcomes from the short-stay unit to the ED can be found in Table 3.
Table 3. Comparison of clinical outcomes from the short-stay unit to historical emergency department control

SD=standard deviation.
Barriers
A survey distributed to the outpatient clinic population eligible for the short-stay unit had an 88% response rate (n=63) and revealed two major barriers to greater utilization of the short-stay unit. A lack of information regarding the short-stay unit (49.2%) was reported as the most prevalent barrier to its use, and travel distance (34.9%) was also a commonly reported concern. This survey also collected data on the region of residence within the Greater Toronto Area, revealing that only 5.1% of the patients resided in central Toronto, where the short-stay unit is located. The distribution of the eligible patient residence can be seen in Figure 2.
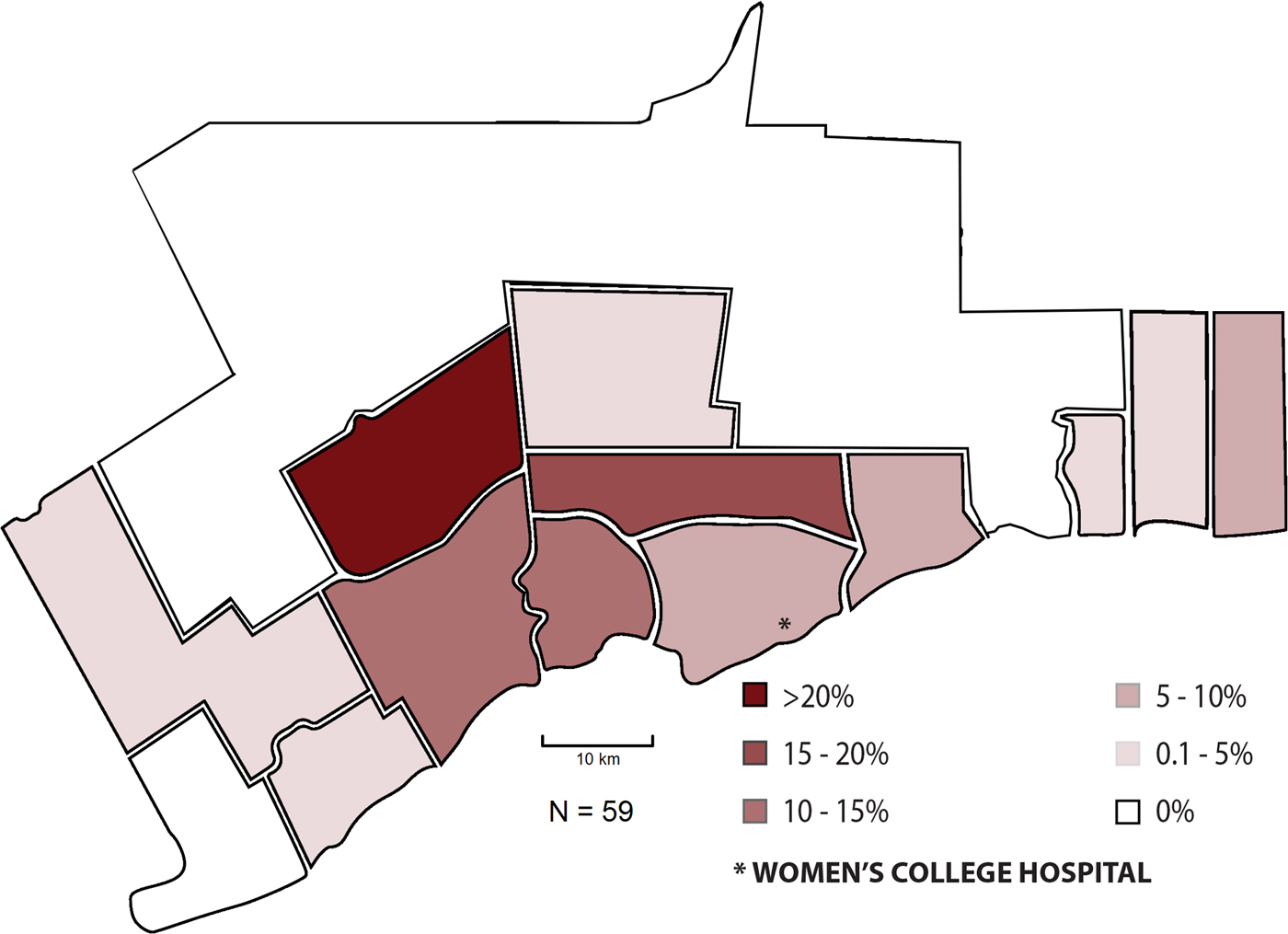
Figure 2. Geographic distribution of patients with SCD eligible for the short-stay unit in a scaled representation of the Greater Toronto Area.
DISCUSSION
This pilot study demonstrated the acceptability of a short-stay unit for the management of low volumes of uncomplicated VOC in adult patients with SCD outside of the ED that was the first of its kind in Canada. The short-stay unit model provided faster access to a first dose of an opiate and higher discharge rates compared with the ED, suggesting improved quality of care. In addition, patient satisfaction was rated high. A lack of awareness and distance to the short-stay unit were major barriers to higher uptake. This model provides an example as to how to redesign the processes of care in Canada for the management of SCD-related VOC that have traditionally been managed in EDs.
Despite being repurposed for a patient population for which it was not originally designed to treat, the short-stay unit functioned smoothly in this study, as demonstrated by short times from presentation to assessment and initiation of pain control. These wait times are consistent with those of other North American examples involving dedicated SCD day hospitals, with 20 minutes reported by Benjamin et al.Reference Benjamin, Swinson and Nagel14 and 58 minutes by Lanzkron et al.Reference Lanzkron, Carroll and Hill15 The NIH, British Committee for Standards in Haematology, and Canadian consensus statement currently recommend administration of opiates within 30 minutes of presentation as the goal for the treatment of VOC.Reference Rees, Olujohungbe and Parker4, Reference Verhovsek and Simpson5, 7 With our short-stay unit model, this goal was achieved with an average time to first dose opiate of 23.5 minutes, four times shorter than in the ED (100.3 minutes).
Both mean and median doses of opiates utilized over the course of visits to the short-stay unit were high in this cohort, as compared with the historical control. Only pediatric data were available for comparison from other short-stay units, which reported substantially lower dose requirements at 0.25 mg/kg/day IV morphine equivalents.Reference Raphael, Kamdar, Beavers, Mahoney and Mueller16 Contributing to this was a small sample size, as well as repeat visits from patients with a high tolerance for opiates. Overnight stays up to 72 hours were also accommodated in this study. Other successful short-stay unit reports have demonstrated average lengths of stay from 5 hours to 5.7 consecutive day visits, but none included evening or overnight hours.Reference Adewoye, Nolan, McMahon, Ma and Steinberg8, Reference Benjamin, Swinson and Nagel14-Reference Raphael, Kamdar, Beavers, Mahoney and Mueller16 Because the length of stay was long and opiate doses were high in this study, it raises the concern of opiate withdrawal after discharge. Although it was reassuring that no short-stay unit patients returned within a month of discharge, prospective data on ED presentations were not included in this pilot study, so it is not known if patients presented to the ED with opiate withdrawal symptoms. Close outpatient follow-up after extended opiate use is recommended to address this issue.
It is also notable that the relatively short length of stay seen in the historical control of this study was reflective only of time spent in the ED, rather than total time in the hospital that includes admission to inpatient wards in 30% of historical control visits. The short-stay unit cohort demonstrated an admission rate to GIM of 15%, which is within the range of reports from other day hospitals of 5%–57%.Reference Adewoye, Nolan, McMahon, Ma and Steinberg8, Reference Wright, Bareford and Wright10, Reference Benjamin, Swinson and Nagel14-Reference Ware, Hambleton, Ochaya and Serjeant17 The remaining discharged patients could significantly and positively impact ED utilization, if this model were to be successfully scaled to higher numbers.
The patient satisfaction survey completed at the short-stay unit demonstrated a very favourable experience for this cohort, as compared with emergency room visits. This indicates the successful mitigation in this pilot study of unfavourable factors common in the ED, such as crowding, a lack of standardization of care, misperception of pain behaviours, and gaps in provider experience. The only negative issue raised in the patient satisfaction survey was the location of the short-stay unit. The average time from triage to presentation was nearly two hours, which represents a prohibitive travel time for many patients experiencing severe pain. Geographic limitations are further highlighted in the demographic survey of eligible patients that showed that only 5.1% of subjects in this sample reside in the same region as the short-stay unit and that distances travelled are often >20 km.
We presented both quantitative and qualitative patient satisfaction data in this study. This allowed for unique insights into the effectiveness of the model, as well as barriers to its use, not previously reported for other short-stay units. Overnight stays of up to 72 hours were allowed using the existing infrastructure for short inpatient stays, representing a distinct feature and strength of this study. The main limitation of this study was low recruitment, resulting in a low power for statistical analysis. Ineffective advertisement to the eligible patient population and inconvenience of location contributed to infrequent utilization. Attempts were made to improve utilization through iterative attempts at raising awareness, including pamphlets, posters, and communication with ED physicians, but recruitment remained slow throughout the 20-month study period. Another limitation of this study was the historical control design, which did not account for confounding variables of differences in treatment between the study periods and differences in the patients’ presenting symptoms (complicated v. uncomplicated VOC) between the short-stay unit and ED. This factor, along with significantly different lengths of stay, limits the interpretation of the comparisons of outcome measures between the short-stay unit and historical control. It is also important to note that this model relied on existing infrastructure that may not be available to other centres, limiting reproducibility to other settings. However, we were able to utilize existing resources and design a model of care that was highly acceptable to patients with SCD, avoiding the use of emergency room settings.
Moving forward, engagement of health care centres outside of central Toronto with a higher density of SCD patients could be more effective in enrolling patients in a short-stay unit. Another consideration is to develop local infrastructure to establish more short-stay units for the treatment of VOC in the communities with the highest prevalence of SCD. Additionally, incorporating diversion of appropriate patients presenting to the ED that has been previously reported could enhance the feasibility of this model and demonstrate a significant impact on utilization.Reference Benjamin, Swinson and Nagel14 In future studies, prospective utilization of EDs should be examined to further explore reasons for low uptake of this model. It will also be important to evaluate the impact of a similar treatment protocol within the ED to determine how much impact can be attributed to the protocol, rather than the model of care.
CONCLUSIONS
This pilot represents a unique example of an acute care short-stay unit for the management of uncomplicated VOC in adult patients with SCD. We have demonstrated high patient satisfaction, acceptability, and improved quality of care provided with this model through the established metric of time to pain control administration. This model can be replicated in other acute care centres in Canada and other countries with populations with SCD to improve care delivery and patient satisfaction, but further studies are required to demonstrate feasibility and scalability to higher volumes.
Acknowledgements
The authors would like to thank the Women’s College Institute of Health Systems Solutions and Virtual Care (WIHV) for providing administrative support to conduct the study. The authors would also like to thank the nurse practitioners at UHN, Colleen Johnson and Kate Uchendu, for the recruitment of participants; Halysha Maloni for assistance with the figures; and Zachary Bouck for assistance with the statistical analysis. Finally, the authors are very grateful to the patients with SCD whose participation made this study possible.
Competing interests
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.